Discussion
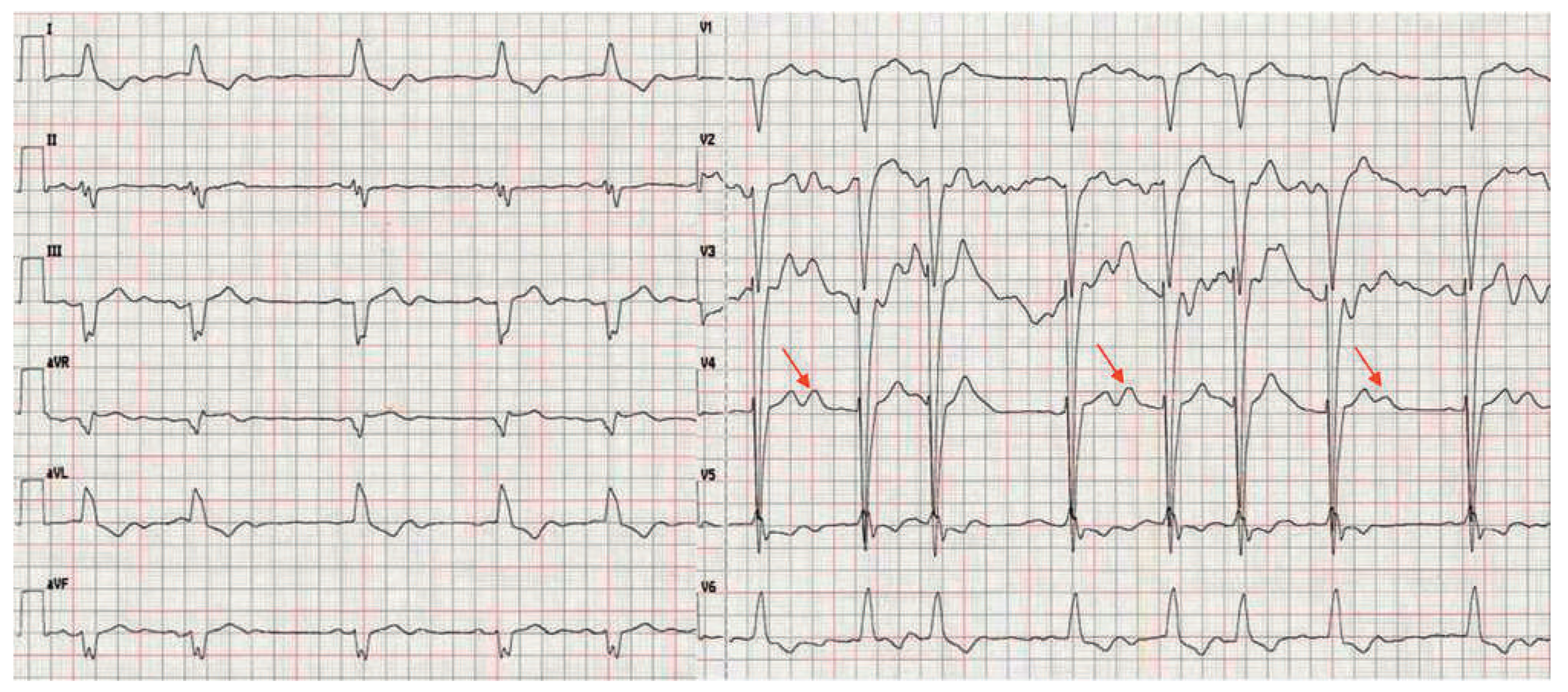
The ECG in figure 1 shows a relatively slow sinus rhythm with left bundle branch block and premature atrial beats. There are some artifacts on V2 and V3, but the “unusual waves” at the end of the T-waves (arrows), best seen in V4, are not artifacts as one could think at first glance. These waves are indeed part of the double peak T-waves, which are also called “notched T-waves” and result in a very long QT interval reaching 700 ms. Notched T-waves are clearly augmented with long R-R intervals after premature atrial beats.
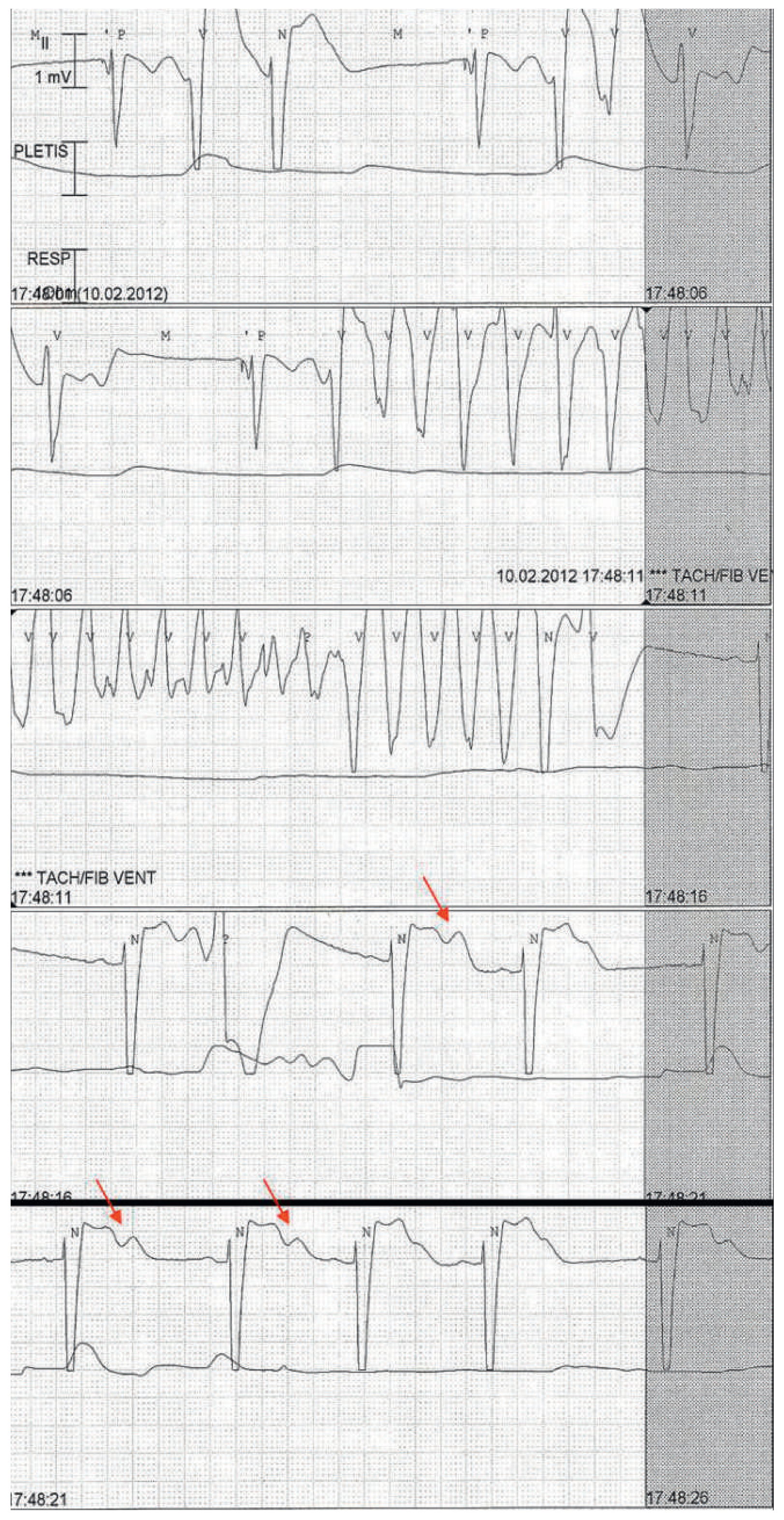
Shortly after admission the patient again had a pre-syncope. The ECG strip (
fig. 2) documented an episode of self-terminated torsade de pointes preceded by a long interval (1580 msec) ended with a paced beat (VVI 40 bpm). The serum potassium concentration was 3.3 mmol/l (3.5–5.0 mmol/l), the mag- nesium 0.60 mmol/l (0.65–1.05 mmol/l).
Figure 1.
ECG showing a sinus bradycardia (40–60 bpm) with left bundle branch block and frequent premature atrial beats (in precordial leads). The T-waves, best seen in V4, are unusual with a double component (arrows) varying in amplitude inversely with the preceding cycle length. The abnormal. T-waves result in a prolonged QT interval reaching 700 ms.
Figure 1.
ECG showing a sinus bradycardia (40–60 bpm) with left bundle branch block and frequent premature atrial beats (in precordial leads). The T-waves, best seen in V4, are unusual with a double component (arrows) varying in amplitude inversely with the preceding cycle length. The abnormal. T-waves result in a prolonged QT interval reaching 700 ms.
Figure 2.
ECG strip showing an episode of pause-dependent self-terminated torsade de pointes. The torsade is preceded by a pause (1580 ms) and a paced beat (VVI 40). Note also in the last 2 lines the pause-dependent notched T-waves (arrows) and a ventricular premature beat arising from the second component of the T-wave.
Figure 2.
ECG strip showing an episode of pause-dependent self-terminated torsade de pointes. The torsade is preceded by a pause (1580 ms) and a paced beat (VVI 40). Note also in the last 2 lines the pause-dependent notched T-waves (arrows) and a ventricular premature beat arising from the second component of the T-wave.
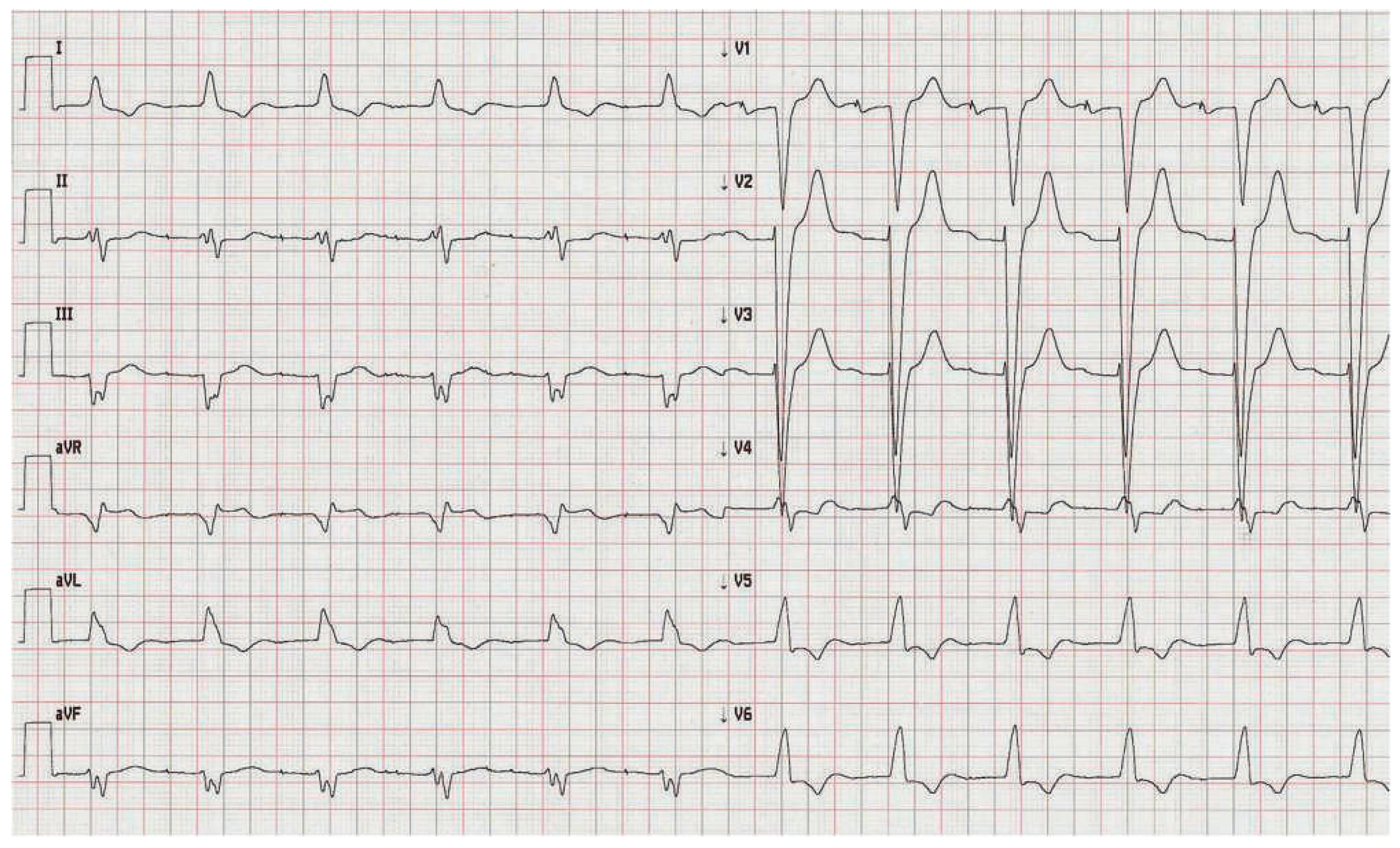
The pacemaker was reprogrammed in DDD 70 bpm, an infu- sion of magnesium sulphate was administered, and potassium was replaced. Moreover, we optimised treatment of heart failure, and withdrew haloperidol. Clinical conditions of the patient progressively improved, and heart rhythm stabilisation was achieved. 48 hours after admission the ECG (
fig. 3) showed the disappearance of the notched T-waves and the shortening of the QT interval to 500 ms.
Figure 3.
ECG showing the evolution of the T-wave morphology and the QT interval 48 hours later. The pacemaker has been programmed in DDD 70 bpm with AV hysteresis resulting in atrial paced rhythm with slightly prolonged AV interval (240 ms) and left bundle branch block. Note the disappearance of the notched T-waves with shortening of the QT interval to 500 ms.
Figure 3.
ECG showing the evolution of the T-wave morphology and the QT interval 48 hours later. The pacemaker has been programmed in DDD 70 bpm with AV hysteresis resulting in atrial paced rhythm with slightly prolonged AV interval (240 ms) and left bundle branch block. Note the disappearance of the notched T-waves with shortening of the QT interval to 500 ms.
This case illustrates an example of acquired long QT syndrome complicated by torsade de pointes. Long QT interval was caused by a combination of electrolyte abnormalities (hypokalaemia and hypomagnesaemia), drugs (haloperidol and amiodarone), underlying decompensated heart failure and pauses due to relative bradycardia with premature atrial beats. As illustrated in
figure 1, the T-waves are very abnormal with two components (notched T-waves, arrows). The second component represents early after-depolarisation that can lead to ventricular ectopic beats and can degenerate into torsade de pointes, the polymorphic ventricular tachycardia typically associated with long QT syndrome [
1]. Tor sade de pointes is usually self-terminated leading to syncope, as in our case, but may degenerate into fatal ventricular fibrillation. In acquired long QT syndrome, torsade is typically pause-dependent, as a long cycle increases early after-depolarisation (increasing the notched T-wave) creating the basis for ventricular arrhythmia as depicted in
figure 2 (arrows) [
1]. It is, therefore, important to avoid long cycles, which was achieved in our case increasing the rate of the pacemaker.
In conditions associated with prolonged QT interval, the absolute length of the QT interval and the distortion of the T-wave (as in our case), particularly when accompanied by ventricular ectopic beats on the terminal component of the T-wave, represent signs of imminent danger for developing malignant ventricular arrhythmias and deserve, therefore, close rhythm monitoring [
2].