Single-Vessel Versus Multivessel PCI in Patients with Acute Coronary Syndrome and Multivessel Coronary Artery Disease
Abstract
Introduction
Patients and methods
Patient population
Definitions and endpoints
Statistical analysis
Results
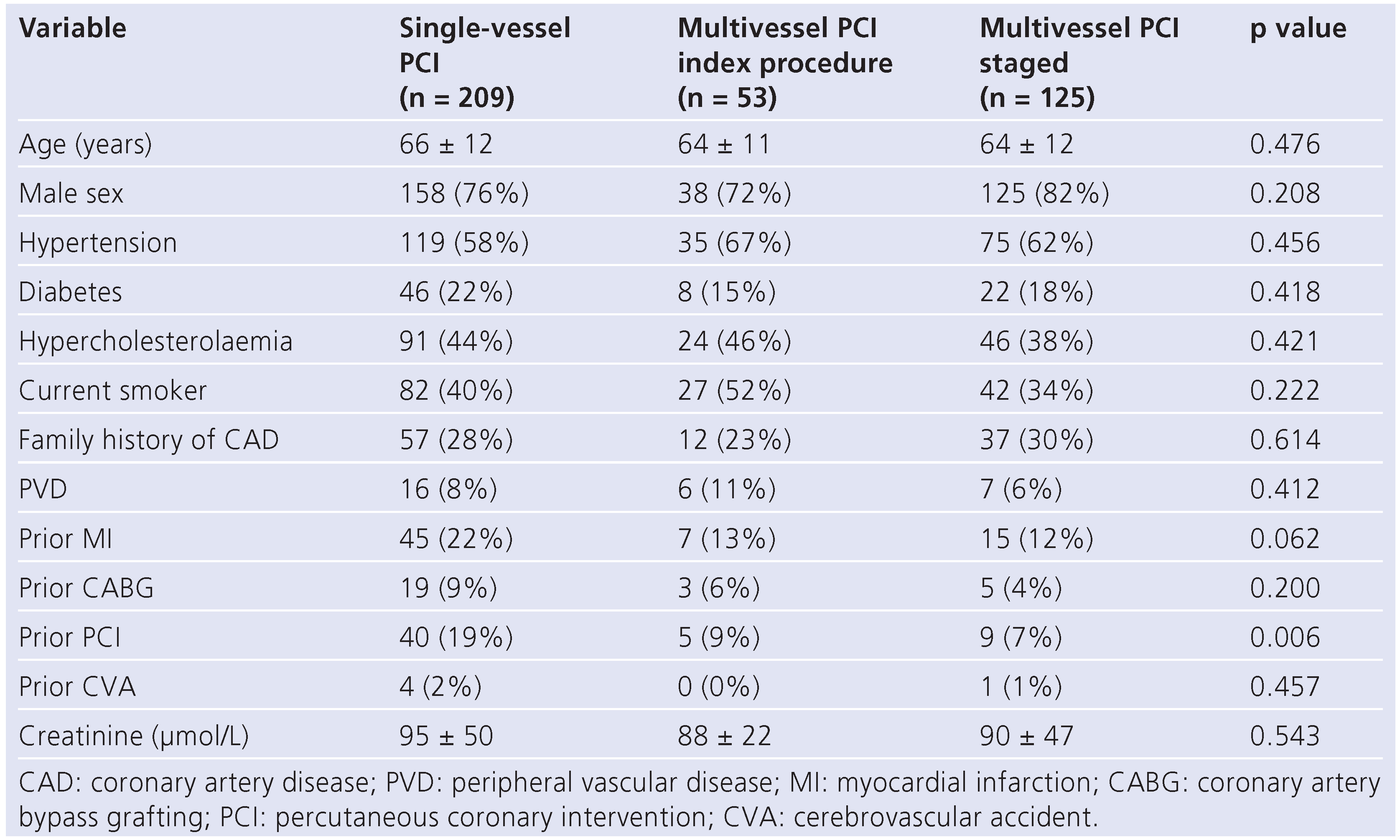
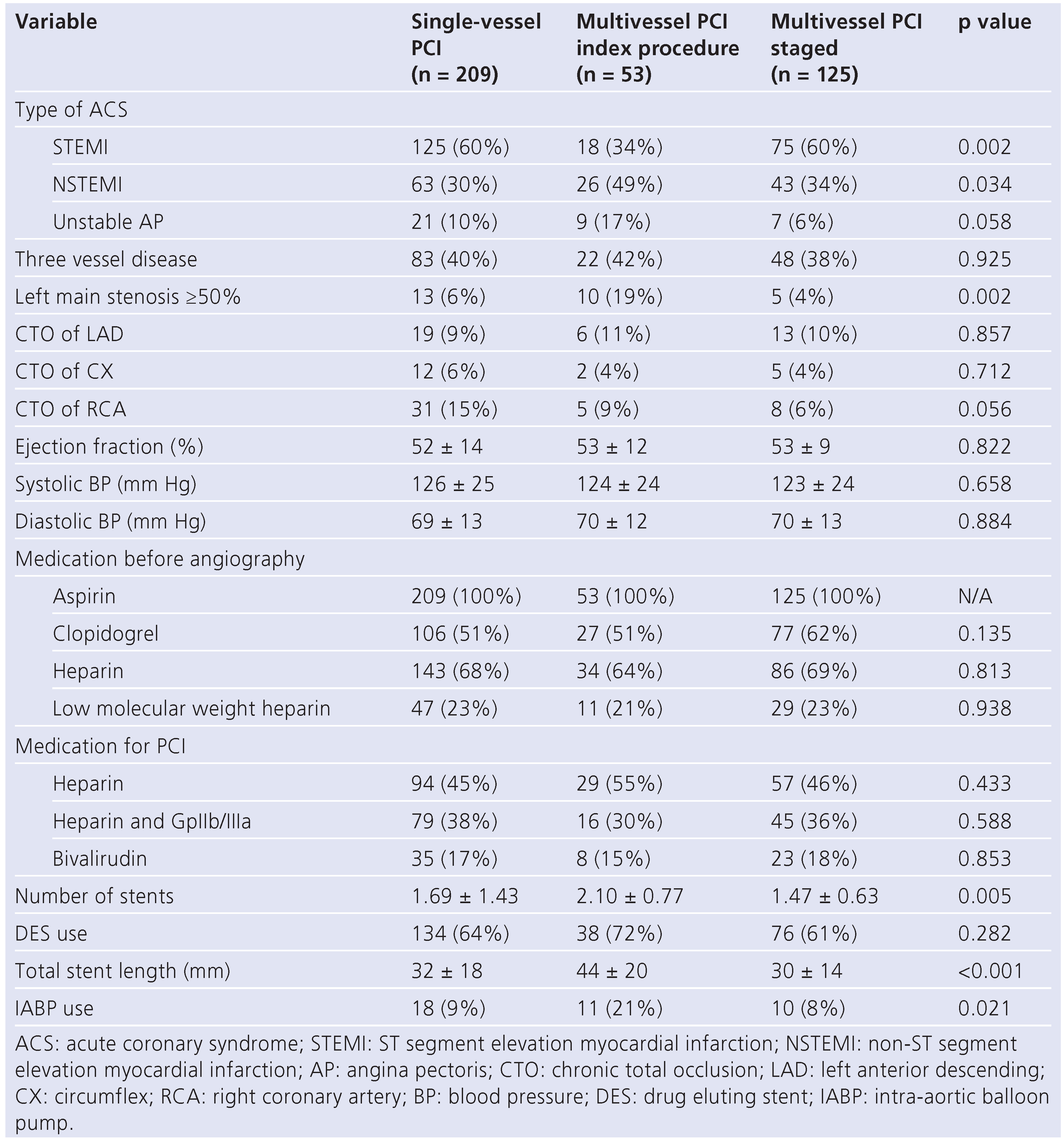
Patients and procedures
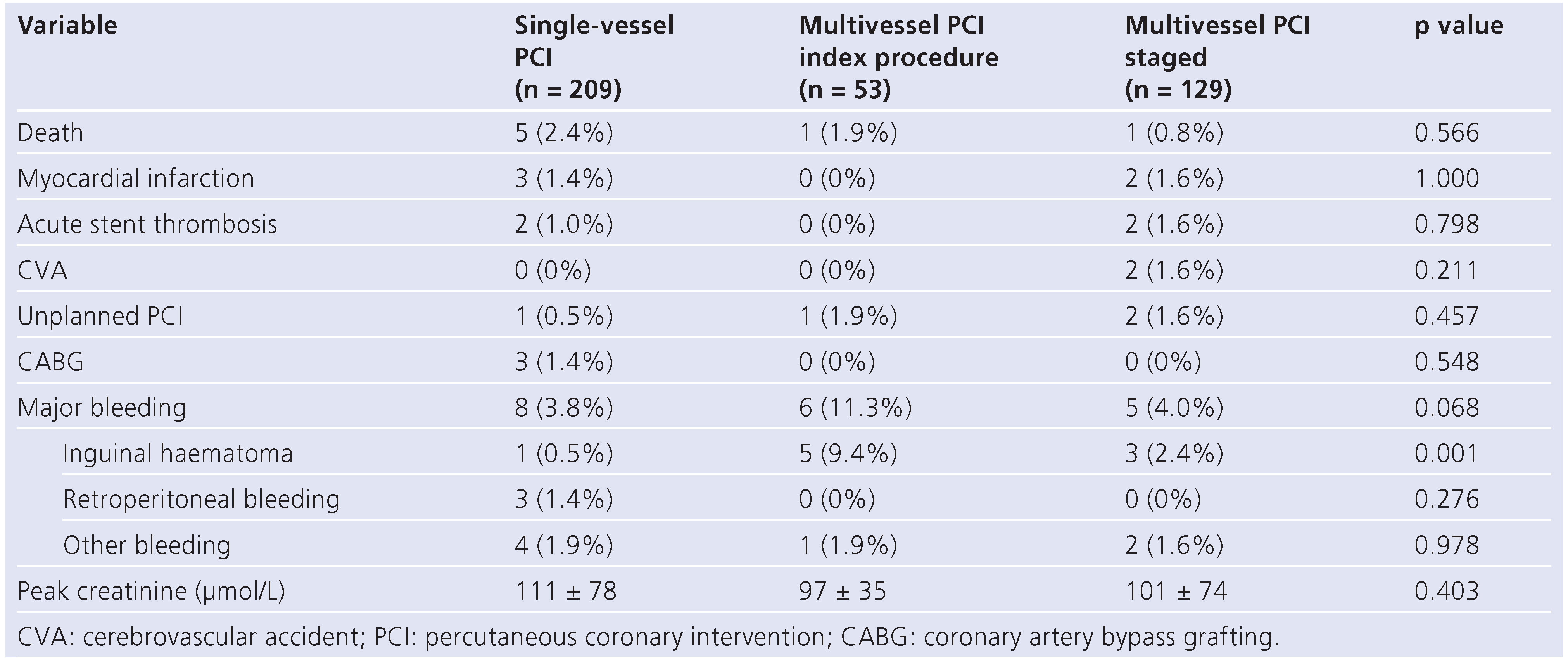
In-hospital outcome
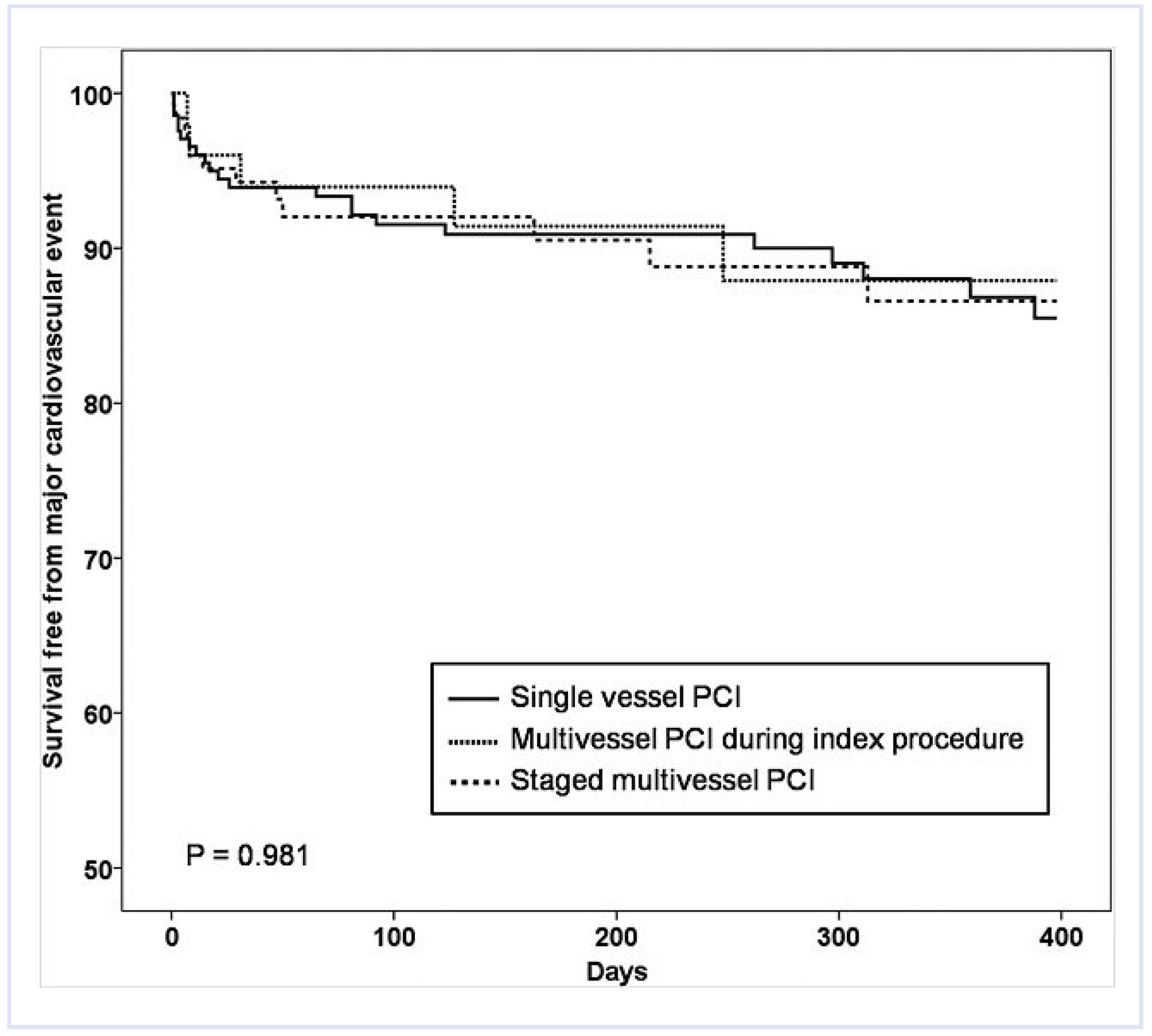
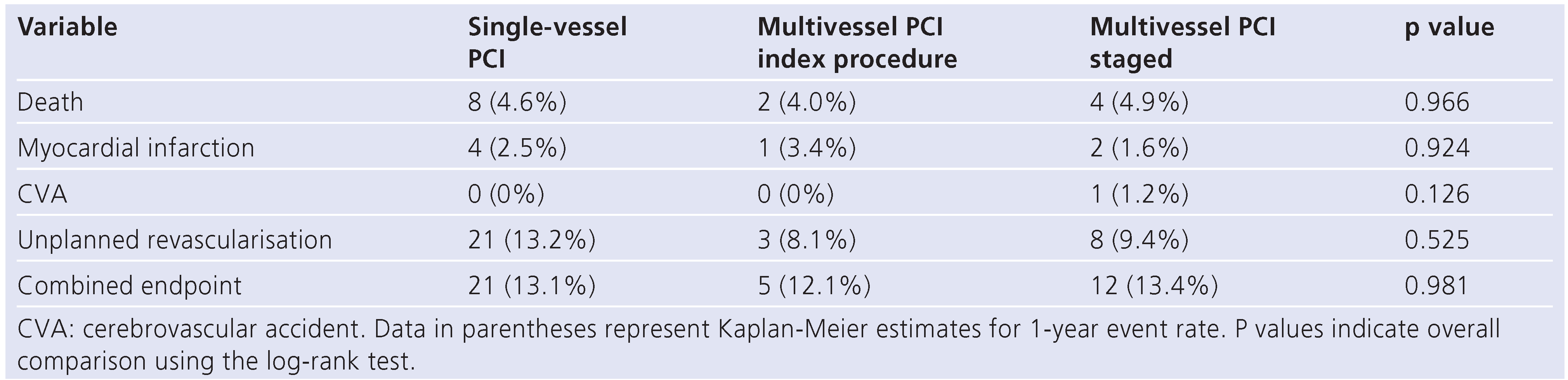
Long-term outcome
Discussion
Comparison to previous studies
Clinical relevance
Limitations
Conclusion
Funding/potential competing interests
References
- Sorajja, P.; Gersh, B.J.; Cox, D.A.; McLaughlin, M.G.; Zimetbaum, P.; Costantini, C.; et al. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J. 2007, 28, 1709–1716. [Google Scholar] [CrossRef] [PubMed]
- Timóteo, A.T.; Fiarresga, A.; Feliciano, J.; Ferreira, R.; Gonçalves, J.M.; Ferreira, L.; et al. Importance of complex additional stenosis after primary angioplasty for acute myocardial infarction in medium-term prognosis. Rev Port Cardiol. 2004, 23, 853–864. [Google Scholar]
- Tarantini, G.; Napodano, M.; Gasparetto, N.; Favaretto, E.; Marra, M.P.; Cacciavillani, L.; et al. Impact of multivessel coronary artery disease on early ischemic injury, late clinical outcome, and remodeling in patients with acute myocardial infarction treated by primary coronary angioplasty. Coron Artery Dis 2010, 21, 78–86. [Google Scholar] [CrossRef]
- Silber, S.; Albertsson, P.; Avilés, F.F.; Camici, P.G.; Colombo, A.; Hamm, C.; et al. Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Guidelines for Percutaneous Coronary Interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur Heart J 2005, 26, 804–847. [Google Scholar] [CrossRef]
- Smith, S.C.; Feldman, T.E.; Hirshfeld, J.W.; Jacobs, A.K.; Kern, M.J.; King, S.B., 3rd.; et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J Am Coll Cardiol 2006, 47, e1–e121. [Google Scholar]
- Palmer, N.D.; Causer, J.P.; Ramsdale, D.R.; Perry, R.A. Effect of completeness of revascularization on clinical outcome in patients with multivessel disease presenting with unstable angina who undergo percutaneous coronary intervention. J Invasive Cardiol. 2004, 16, 185–188. [Google Scholar]
- Shishehbor, M.H.; Topol, E.J.; Mukherjee, D.; Hu, T.; Cohen, D.J.; Stone, G.W.; et al. TARGET Investigators. Outcome of multivessel coronary intervention in the contemporary percutaneous revascularization era. Am J Cardiol. 2006, 97, 1585–1590. [Google Scholar] [CrossRef] [PubMed]
- Tsuiki, K.; Ohta, I.; Oguma, M.; Yamaguchi, S.; Tono-oka, I.; Yasui, S. Significant stenosis of coronary arteries in patients with single and multiple vessel diseases without previous myocardial infarction. Jpn Circ J. 1991, 55, 427–436. [Google Scholar] [CrossRef]
- Schweiger, M.J.; Stanek, E.; Iwakoshi, K.; Hafer, J.G.; Jacob, A.; Tullner, W.; et al. Comparison of visual estimate with digital caliper measurement of coronary artery stenosis. Cathet Cardiovasc Diagn. 1987, 13, 239–244. [Google Scholar]
- Leaman, D.M.; Brower, R.W.; Meester, G.T.; Serruys, P.; van den Brand, M. Coronary artery atherosclerosis: severity of the disease, severity of angina pectoris and compromised left ventricular function. Circulation. 1981, 63, 285–299. [Google Scholar] [CrossRef]
- Austen, W.G.; Edwards, J.E.; Frye, R.L.; Gensini, G.G.; Gott, V.L.; Griffith, L.S.; et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975, 51, 5–40. [Google Scholar] [CrossRef] [PubMed]
- Serruys, P.W.; Unger, F.; van Hout, B.A.; van den Brand, M.J.; van Herwerden, L.A.; van Es, G.A.; et al. The ARTS study (Arterial Revascularization Therapies Study). Semin Interv Cardiol. 1999, 4, 209–219. [Google Scholar]
- Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J. 2000, 21, 1502–1513. [CrossRef]
- Katritsis, D.G.; Ioannidis, J.P.A. Percutaneous Coronary Intervention Versus Conservative Therapy in Nonacute Coronary Artery Disease: A Meta-Analysis. Circulation 2005, 111, 2906–2912. [Google Scholar] [CrossRef]
- Hannan, E.L.; Racz, M.J.; McCallister, B.D.; Ryan, T.J.; Arani, D.T.; Isom, O.W.; et al. A comparison of three-year survival after coronary artery bypass graft surgery and percutaneous transluminal coronary angioplasty. J Am Coll Cardiol 1999, 33, 63–72. [Google Scholar] [CrossRef]
- Mauri, L.; Silbaugh, T.S.; Garg, P.; Wolf, R.E.; Zelevinsky, K.; Lovett, A.; et al. Drug-eluting or bare-metal stents for acute myocardial infarction. N Engl J Med 2008, 359, 1330–1342. [Google Scholar] [CrossRef]
- Kastrati, A.; Dibra, A.; Spaulding, C.; Laarman, G.J.; Menichelli, M.; Valgimigli, M.; et al. Meta-analysis of randomized trials on drug-eluting stents vs. bare-metal stents in patients with acute myocardial infarction. Eur Heart J 2007, 28, 2706–2713. [Google Scholar] [CrossRef] [PubMed]
- Brener, S.J.; Milford-Beland, S.; Roe, M.T.; Bhatt, D.L.; Weintraub, W.S.; Brindis, R.G. American College of Cardiology National Cardiovascular Database Registry. Culprit-only or multivessel revascularization in patients with acute coronary syndromes: an American College of Cardiology National Cardiovascular Database Registry report. Am Heart J. 2008, 155, 140–146. [Google Scholar] [CrossRef]
- Kong, J.A.; Chou, E.T.; Minutello, M.; Wong, S.C.; Hong, M.K. Safety of single versus multi-vessel angioplasty for patients with acute myocardial infarction and multi-vessel coronary artery disease: report from the New York State Angioplasty Registry. Coronary Artery Disease 2006, 17, 71–75. [Google Scholar] [CrossRef]
- Khattab, A.A.; Abdel-Wahab, M.; Röther, C.; Liska, B.; Toelg, R.; Kassner, G.; et al. Multi-vessel stenting during primary percutaneous coronary intervention for acute myocardial infarction. A single-center experience. Clin Res Cardiol. 97, 32–38. [CrossRef] [PubMed]
- Qarawani, D.; Nahir, M.; Abboud, M.; Hazanov, Y.; Hasin, Y. Culprit only versus complete coronary revascularization during primary PCI. Int J Cardiol 2008, 123, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Roe, M.T.; Cura, F.A.; Joski, P.S.; Garcia, E.; Guetta, V.; Kereiakes, D.J.; et al. Initial Experience With Multivessel Percutaneous Coronary Intervention During Mechanical Reperfusion for Acute Myocardial Infarction. Am J Cardiol 2001, 88, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Corpus, R.A.; House, J.A.; Marso, S.P.; Grantham, J.A.; Huber, K.C., Jr.; Laster, S.B.; et al. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J. 2004, 148, 493–500. [Google Scholar] [CrossRef]
- Rigattieri, S.; Biondi-Zoccai, G.; Silvestri, P.; Di Russo, C.; Musto, C.; Ferraiuolo, G.; et al. Management of multivessel coronary disease after ST elevation myocardial infarction treated by primary angioplasty. J Interv Cardiol. 2008, 21, 1–7. [Google Scholar] [CrossRef]
- Han, Y.L.; Wang, B.; Wang, X.Z.; Li, Y.; Wang, S.L.; Jing, Q.M.; et al. Comparative effects of percutaneous coronary intervention for infarct-related artery only or for both infarct- and non-infarctrelated arteries in patients with ST-elevation myocardial infarction and multi-vessel disease. Chin Med J. 2008, 121, 2384–2387. [Google Scholar] [CrossRef]
- Hannan, E.L.; Samadashvili, Z.; Walford, G.; Holmes, D.R.; Jacobs, A.K.; Stamato, N.J.; et al. Culprit Vessel Percutaneous Coronary Intervention Versus Multivessel and Staged Percutaneous Coronary Intervention for ST-Segment Elevation Myocardial Infarction Patients With Multivessel Disease. J Am Coll Cardiol Intv. 2010, 3, 22–31. [Google Scholar] [CrossRef]
- Widimsky, P.; Holmes, D.R. How to treat patients with ST-elevation acute myocardial infarction and multi-vessel disease? Eur Heart J. 2011, 32, 396–403. [Google Scholar] [CrossRef]
- Mohamad, T.; Bernal, J.M.; Kondur, A.; Hari, P.; Nelson, K.; Niraj, A.; et al. Coronary Revascularization Strategy for ST Elevation Myocardial Infarction with Multivessel Disease: Experience and Results at 1-Year Follow-Up. Am J Ther. 2010. [Epub ahead of print]. [Google Scholar]
- Jaski, B.E.; Cohen, J.D.; Trausch, J.; Marsh, D.G.; Bail, G.R.; Overlie, P.A.; et al. Outcome of urgent percutaneous transluminal coronary angioplasty in acute myocardial infarction: comparison of single-vessel versus multivessel coronary artery disease. Am Heart J. 1992, 124, 1427–1433. [Google Scholar] [CrossRef]
- Katritsis, D.G.; Meier, B. Percutaneous Coronary Intervention for Stable Coronary Artery Disease. J Am Coll Cardiol 2008, 52, 889–893. [Google Scholar] [CrossRef]

© 2011 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Quarella, M.; Toggweiler, S.; Müller, D.J.; Wyss, C.A.; Corti, R.; Lüscher, T.F. Single-Vessel Versus Multivessel PCI in Patients with Acute Coronary Syndrome and Multivessel Coronary Artery Disease. Cardiovasc. Med. 2011, 14, 141. https://doi.org/10.4414/cvm.2011.01593
Quarella M, Toggweiler S, Müller DJ, Wyss CA, Corti R, Lüscher TF. Single-Vessel Versus Multivessel PCI in Patients with Acute Coronary Syndrome and Multivessel Coronary Artery Disease. Cardiovascular Medicine. 2011; 14(5):141. https://doi.org/10.4414/cvm.2011.01593
Chicago/Turabian StyleQuarella, Marino, Stefan Toggweiler, Dominic J. Müller, Christophe A. Wyss, Roberto Corti, and Thomas F. Lüscher. 2011. "Single-Vessel Versus Multivessel PCI in Patients with Acute Coronary Syndrome and Multivessel Coronary Artery Disease" Cardiovascular Medicine 14, no. 5: 141. https://doi.org/10.4414/cvm.2011.01593
APA StyleQuarella, M., Toggweiler, S., Müller, D. J., Wyss, C. A., Corti, R., & Lüscher, T. F. (2011). Single-Vessel Versus Multivessel PCI in Patients with Acute Coronary Syndrome and Multivessel Coronary Artery Disease. Cardiovascular Medicine, 14(5), 141. https://doi.org/10.4414/cvm.2011.01593




