Case report
A 70-year-old woman was addressed by her physician to the hospital for further investigation of a new deterioration of her general condition, fatigue and psychomotor alteration. The patient, known for resection of a gastric tumor in 2009, said that she had been feeling weak since 5 days, described a weight loss of 15 kg in 2 years and complained of a chronic costal pain and a tender right elbow. She had no family history of ischemic cardiomyopathy but she had additional cardio-vascular risk factors (hypertension, hypercholesterolemia and tobacco use) without a recent major psychological or physical stress. Systematic interrogation revealed no other symptom, especially no chest pain, dyspnea or other signs of cardiac failure.
Physical examination was unremarkable. Blood pressure was 112/63 mm Hg, with an irregular heart rate of 70 beats/min.
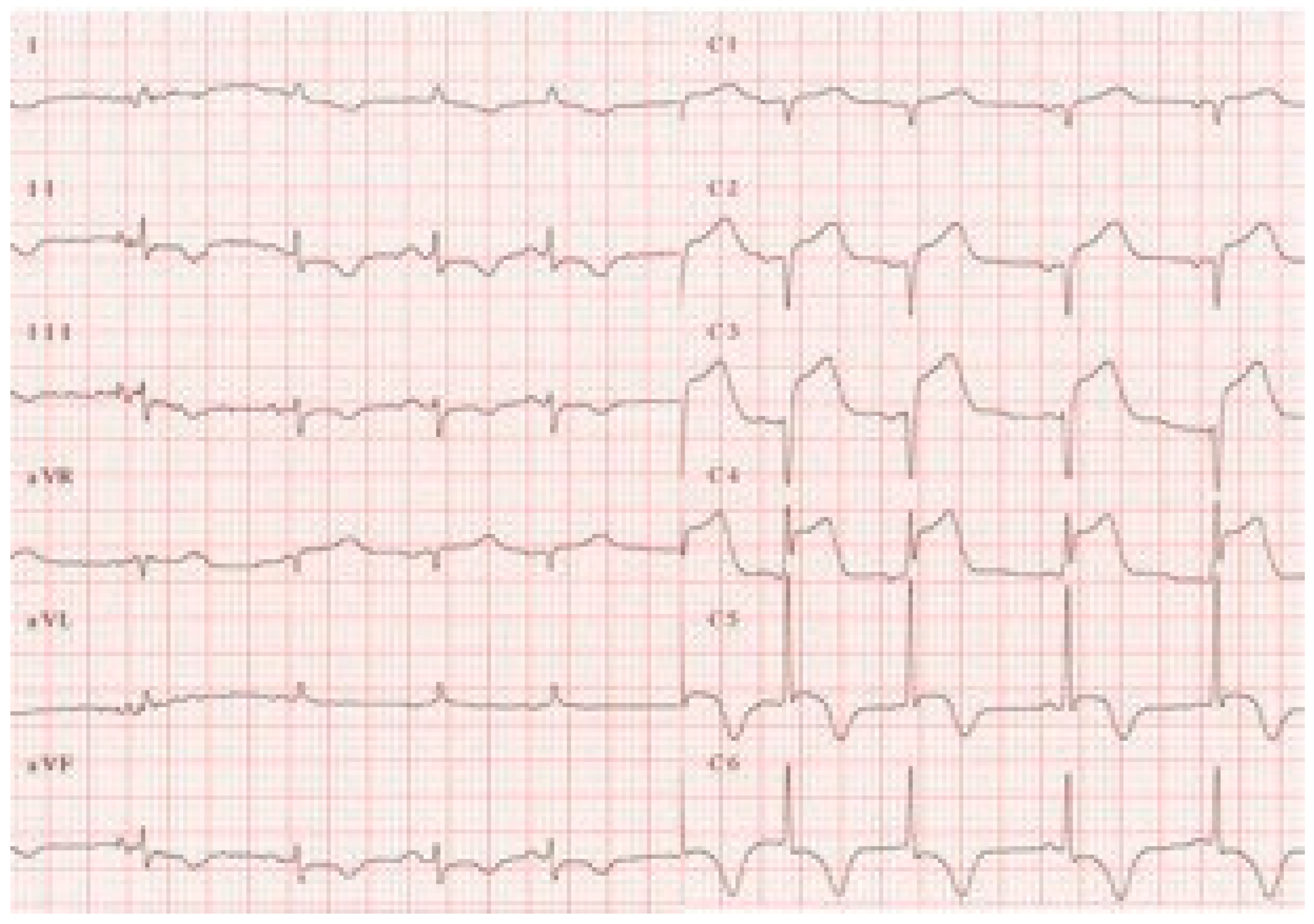
The resting ECG showed a sinus rhythm at 75/min, with 2 supraventricular extrasystoles, negative T waves in leads I, II, III, AVF and V3 to V6 with marked prolongation of QT interval (QTc: 0.62 sec) (
Figure 1). The biological exams revealed normal electrolytes and renal function and a slight increase in troponin (0.27 mcg/l) with normal total CK (63 U/l). Patient was treated for a NSTEMI, received aspirine 500 mg and clopidogrel 300 mg and was transferred in intensive care unit for monitoring.
A few hours later, she became somewhat confused and less alert. After stimulation she reported no chest pain and no other symptoms. An electrocardiogram performed at that time revealed ST-segment elevation in precordial leads V1–V5 (
Figure 2), followed by ventricular tachycardia suggestive of “torsade de pointes” (
Figure 3) and cardio-respiratory arrest.
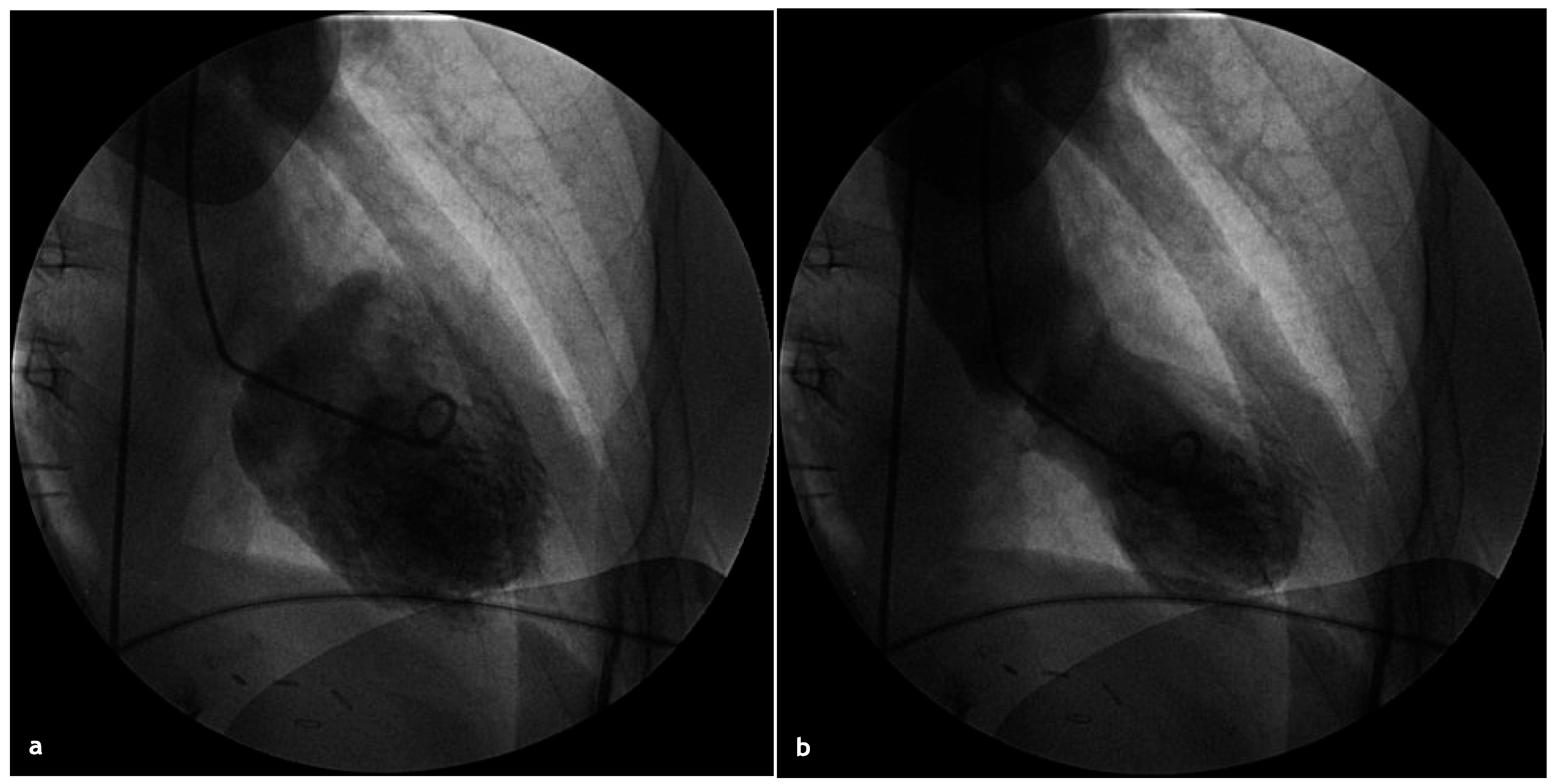
After successful CPR (patient received 3 direct current shocks, intravenous magnesium and intravenous beta-blocker before restoration of a sinus rhythm), the patient was transferred to the University Hospital for urgent angiography, which demonstrated no significant coronary artery lesions. The left ventriculography showed the typical image of an apical ballooning (
Figure 4).
The echocardiography confirmed the extensive apical akinesia and the severe hypokinesia of the other walls sparing the basal segments with an EF of 20% and revealed the presence of an apical thrombus. The treatment of aspirine and clopidogrel was stopped and anticoagulation with acenocoumarol was started. Beta-blocker was maintained and ACE-inhibitor as well as loop diurectics introduced. An echocardiography, performed 1 week later, showed a improvement of the EF from 20 to 33% and a partial resolution of the thrombus. The patient achieved good cerebral recovery without neurological deficit and was discharged in a rehabilitation unit. Follow-up echocardiography at 2 months confirmed a complete recovery of the left ventricular systolic function. ECG also gradually normalizes, but slower than the left ventricular wall motion abnormalities.
Discussion
This case fullfils the criteria of Tako-Tsubo cardiomyopathy proposed by Tschuchihashi in 2001 and revised by Gianni [
1] in 2006: new ST segment elevation or depression or T wave inversion on the ECG, transient akinesis or dyskinesis of the apical or midventricular segments in association with regional wall motion abnormalities that extend beyond the distribution of a single epicardial coronary vessel on the echocardiography, absence of evidence of obstructive coronary artery disease and absence of a recent significant head trauma, intracranial bleeding, pheochromocytoma or hypertrophic cardiomyopathy. Its presentation is somewhat atypical by the absence of a provocative emotional or physical stress and the absence of chest pain or dyspnea, but this pattern is not unusual as described in our recently published observation of 31 patients [
2]. QTc prolongation is usual, and was present in 77% of the patients in the previous study [
2]. The mechanism is unknown, but is linked to exaggerated sympathetic stimulation, either directly by the autonomic innervation of the heart, or indirectly by circulating catecholamines [
3].
Sudden cardiac death in Tako-Tsubo cardiomyopathy is rare, but has been described [
4] and we personnally observed 3 cases including this case report. The mechanism of the arythmia is often difficult to record. In our 2 previous patients, VF was present at the time of diagnosis and successfully treated by electrical cardioversion. There are 2 previous observation of QT prolongation degenerating in “torsade de pointes” and ventricular fibrillation as a cause of cardiac arrest in Tako-Tsubo cardiomyopathy [
5,
6]. In the second published case, genetic testing failed to identify any known mutation predisposing to prolongation of the QT interval and malignant ventricular arythmia.
In summary, QT prolongation is a classical feature of Tako-Tsubo cardiomyopathy. Even if the prognosis of this condition is generally good, sudden cardiac death has been observed and some case reports, including this one, suggest that “torsade de pointes” could be the cause of the malignant arythmia.