Introduction
Paradoxical embolism is a rare entity and refers to the entry of a venous thrombus into the systemic circulation through a right-to-left shunt, most commonly through a patent-foramen ovale (PFO). Usually, paradoxical embolism remains a speculative diagnosis, because only rarely can the passage of venous thrombus from the right to the left atrium be documented. However, in the presence of a deep venous thrombosis or pulmonary embolism (PE), an abnormal communication between the venous and the systemic circulation, and with clinical, angiographic or pathologic evidence of systemic embolism, the diagnosis of paradoxical embolism may be retained [
1].
Occasionally, the thrombus may be observed in transition from the right to the left cardiac chambers, especially straddling through a PFO, and this condition is better known as impending paradoxical embolism (IPDE). Prior to the advent of echocardiography or multislice-computer-tomography (MSCT), IPDE was usually only discovered during post-mortem examination [
2].
Very rarely does a patient present with high-risk PE, an acute ischaemic stroke and a large IPDE and in that case, the optimal therapeutic strategy is still unknown and debated. The high haemodynamic instability mandating for a prompt medical decision and the absolute contraindications of the usual treatment (thrombolysis or surgical embolectomy) make the management of this kind of situation very challenging.
We report the case of a patient presenting this complex clinical picture (high-risk PE, an acute ischaemic stroke and a large IPDE) while having an absolute contraindication for systemic thrombolysis or cardiac surgery. The discussion will be centered on current endovascular options in this setting.
Case report
A 72-year-old female renal transplant recipient was admitted because of generalised weakness and lowgrade fever. Two months earlier, pulmonary nocardiosis with cerebral, cutaneous and pericardial involvement was diagnosed, and she has been on antibiotic therapy with ceftriaxone and ciprofloxacine since. Two weeks after hospital admission, the patient developed a sudden decline of consciousness with respiratory and haemodynamic collapse requiring endotracheal intubation and vasopressor support. Arterial blood gas assessment revealed a severe mixed acidosis with a pH at 6.99, a PCO2 of 11 kPa (83 mm Hg), lactate 7 mmol/l with bicarbonate at 18.8 mmol/l and a PO2 of 14.5 kPa (109 mm Hg) on an inspired fraction oxygen of 0.70. The electrocardiogram showed a new right bundle branch block and an SI/QIII pattern. A contrast-enhanced CT-scan of the head and thorax confirmed the clinical suspicion of a high-risk PE by showing a central bilateral pulmonary embolism and also a thrombotic occlusion of the left middle cerebral artery. Trans-thoracic echocardiography (TTE) detected a severely dilated and dysfunctioning right ventricle and a floating thrombus in the right atrium (RA), close to the entry of inferior vena cava (IVC), without an obvious point of attachment. The haemodynamic and ventilatory status continued to deteriorate rapidly with the patient requiring a high dose of vasopressors.
Due to the intracranial bleeding risk in this patient with multiple nocardiosis-associated cerebral cysts and concomitant acute ischaemic stroke, both systemic thrombolytic treatment and surgery were deemed to be contraindicated. In the light of a rapid deterioration of the haemodynamic status, it was decided to attempt a percutaneous pulmonary thrombectomy. The procedure was performed in compliance with our institutional protocol investigating safety and efficacy of rheolytic thrombectomy (AngioJet™, Possis Medical, Minneapolis, MN, USA) in massive PE (Clinical Trial No. NCT00780767), and the relatives of the patient gave informed consent.
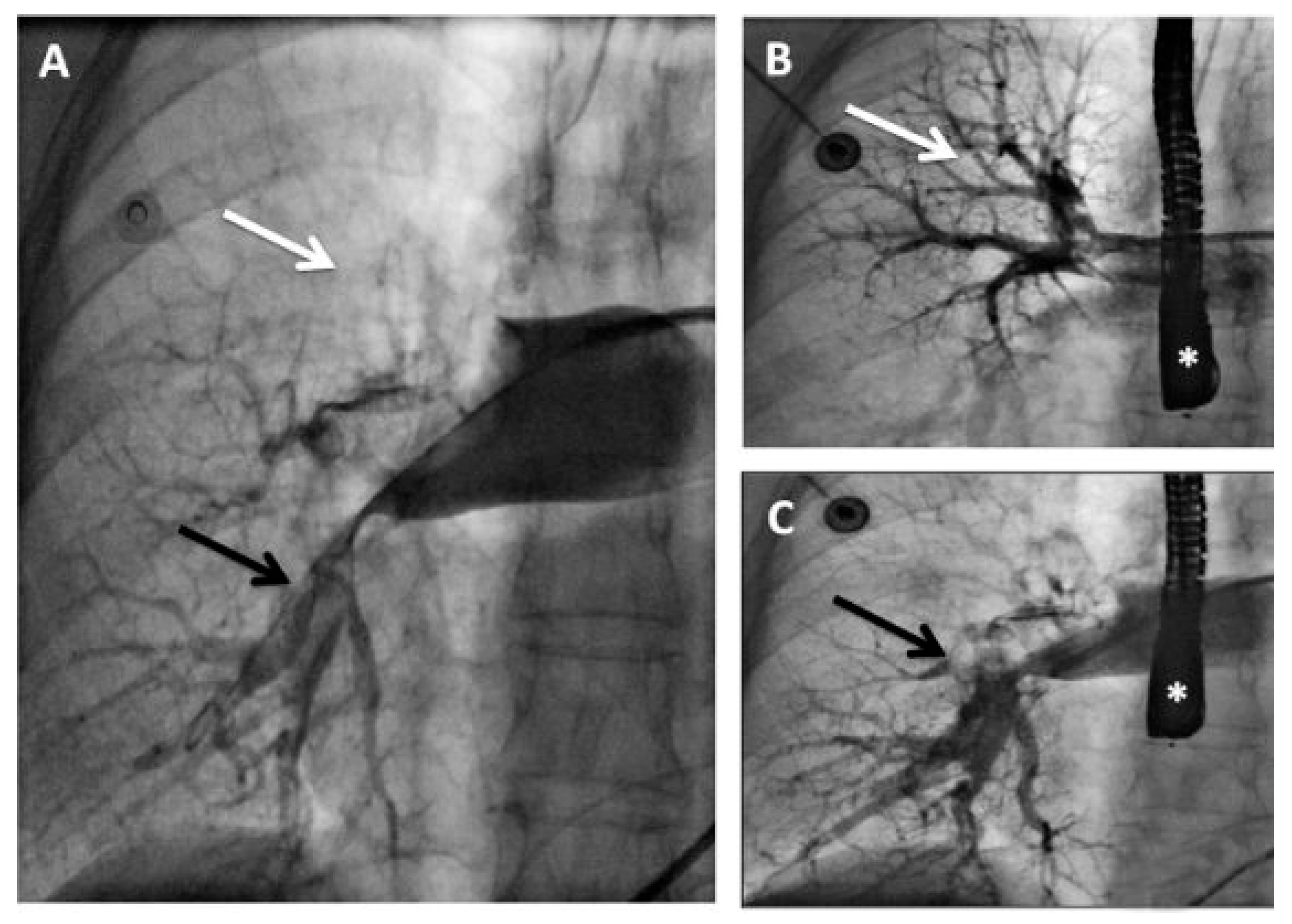
The intended strategy was to first perform rheolytic thrombectomy at the level of the IVC/RA and subsequently in the pulmonary arteries without administration of systemic or local fibrinolytics. However, the inferior cavography performed at the beginning of the procedure showed that the thrombus was not at the IVC/RA transition as suspected, but that it was lodged into the RA at the level of the
fossa ovalis (
Figure 1). Associating this imaging with the clinical presentation of a combined ischaemic stroke and massive PE, the presence of an IPDE was suspected. At that moment, the rheolytic thrombectomy was performed only at the pulmonary level and a trans-oesophageal echocardiography (TEE) was scheduled to confirm the presence of an IPDE.
Two venous retrograde approaches (6 and 8 F sheaths) were inserted in the common femoral vein. Using a 8 F Multipurpose guiding catheter and a 6 F long diagnostic Judkins right catheter (i.e., telescoping technique), a soft tip guide wire was gently advanced firstly in the right atrium, then in the right ventricle and finally in the right pulmonary artery. At that moment, a selective pulmonary angiography confirmed the presence of a massive PE and while preparing the AngioJet™ catheter, a temporary pacemaker was positioned in the right ventricle. Finally, the Angiojet system was advanced through the 8 Fr guiding catheter and activated (max. 20 s) inside the pulmonary occlusion. During the thrombectomy procedure, the TEE confirmed the presence of a large serpentine thrombus in the right atrium floating through the PFO into the left atrium (
Figure 2).
The percutaneous AngioJet™ rheolytic thrombectomy was rapidly and successfully performed at the pulmonary level (
Figure 3), and the procedure was interrupted immediately when the haemodynamic condition of the patient had improved with elevation of systemic pressure permitting a diminishing dose of vasopressors. Due to the estimated high risk of dislodgement or fragmentation with subsequent systemic embolisation, the thrombus at the level of the PFO was not approached. The patient left the cardiac catheterisation laboratory under full heparin anticoagulation with stable haemodynamic conditions. Over a few hours, a progressive weaning from the vasopressor was possible and a second TEE performed 12 h following the procedure confirmed the improvement of the right ventricular function in the absence of residual intra-atrial thrombus. Without any further neurologic deterioration, the patient could be extubated on day 7 and she could be discharged from the hospital on day 60 with only mild neurological
sequelae. At 12 months, she was still doing well without relapse on oral anticoagulation.
Discussion
The first case of IPDE diagnosed by echocardiography was made by Nellessen et al. in 1985 [
3] and since then the observation of entrapped embolus through a PFO has become more common [
4]. As known from a recent meta-analysis by Myers et al., there have been 174 patients presenting with IPDE reported in the medical literature between 1964 and 2009 [
5].
The clinical presentation of an IPDE may be an isolated PE in half of the patients, a combined presentation of PE and paradoxical embolism in up to 40% of cases, and in the remaining cases an isolated paradoxical embolism [
5,
6]. In the subgroup of patients presenting with systemic and pulmonary embolism, only few cases have presented with a high-risk PE [
7] (i.e., pulmonary embolism with haemodynamic instability).
Impending paradoxical embolism associating with an acute ischaemic stroke and a high-risk PE is a very challenging situation because the recent stroke event may contraindicate the systemic thrombolysis and the massive PE-related mortality, without this treatment, remains prohibitive (i.e., up to 30%) [
8].
The International Cooperative Pulmonary Embolism registry confirms that timely performed treatment of patients with PE, especially in the presence of associated haemodynamic instability, may greatly impact outcomes [
9]. Furthermore, it is admitted that the presence of a PFO in patients presenting with PE is an independent predictor of in-hospital mortality, suggesting that a prompt and aggressive treatment, especially in those patients with associated IPDE, should be proposed [
10].
In high-risk PE, systemic fibrinolysis is recommended as first-line treatment [
11], however, this therapy is associated with a risk of up to 22% of major bleeding [
9]. Accordingly, as in our case, about one third of patients suffering from high-risk PE may not be candidates for thrombolytic therapy because of absolute or relative contraindications [
12]. Surgical embolectomy is the alternative treatment modality of massive PE especially in case of associated IPDE. However, it carries a substantial morbidity and mortality risk (30–50%) and may not be performed in case of major haemodynamic instability [
13]. Furthermore, extracorporal circulation requires a high degree of perioperative anticoagulation and therefore may not be applicable in patients at risk of high bleeding.
For all these reasons, new therapeutic approaches with percutaneous thrombectomy devices may be particularly useful in this kind of situation when lytics and surgery are not possible or are unavailable. There are currently various types of catheter for percutaneous mechanical thrombectomy in case of massive PE [
14]. One of them is the AngioJet™ Rheolytic Thrombectomy (Possis Medical, Minneapolis, MN), which is a device specially designed to remove intravascular thrombus from coronary and peripheral arteries. This system uses a high-speed saline jet delivered at high pressure that fragments the thrombus and, due to the Bernoulli Effect, produces a vacuum phenomenon for clot aspiration and extraction. In 1997, Koning et al. [
15] were the first to use the AngioJet™ catheter with success in a patient with high-risk PE and contraindications to thrombolytic therapy. Since then, several case reports and small retrospectives studies followed [
16,
17]. From the available clinical data, percutaneous thrombectomy with AngioJet™ was technically successful in >90% of cases and achieved significant angiographic and haemodynamic improvement in most of the cases [
16,
17].
Since only few reports have described patients presenting with high-risk PE, stroke and IPDE, there is no consensus on how these patients should be managed [
5]. With this case, it has been illustrated that percutaneous thrombectomy with the AngioJet™ system can be a life-saving intervention in this very challenging situation. This new technique seems relatively safe and effective and could be considered, in the near future, as a first-line therapy in patients with contraindication to thrombolytic therapy [
14].
Indeed, a randomised study of systemic thrombolysis versus modern percutaneous thrombectomy is needed to determine the optimal treatment of patients presenting with massive PE with or without IPDE, but until then the optimal therapeutic strategy should be chosen on a per patient basis.