Summary
Since the first transradial percutaneous coronary intervention in 1992 by Kiemenij, this technique has been performed heterogeneously around the world with increasing interest due to recent reports in the literature. Indeed, this approach decreases access site complications and major bleeding and increases patient comfort. All patient subgroups benefit from this approach, especially in cases of acute coronary syndromes where the risk of bleeding is highest. In this review, we will address the debate between femoralists and radialists with regard to pre-RIVAL studies and including the RIVAL randomised trial. The aim of this literature review is to demonstrate that ignoring the transradial approach can no longer be justified.
Introduction
Vascular complications and bleeding related to femoral access represent a major cause of morbidity and mortality, especially in patients undergoing percutaneous coronary intervention (PCI). The transradial approach (TRA) virtually eliminates vascular complications. Indeed, the radial artery is superficial and easily compressed and thus bleeding is readily controlled. In addition it improves patient comfort and allows rapid mobilisation. Owing to its proven benefits in reducing bleeding complications and therefore its potential impact on morbidity and mortality, young interventionalists and experienced operators with a high volume of acute procedures should be trained in TRA for coronary procedures. In this manuscript, we discuss the recent randomised trial RIVAL and review the literature on TRA, considered by some operators as a simple alternative to transfemoral approach (TFA) and by a growing number of adepts as the default approach.
Historical perspective and worldwide penetration
The first percutaneous TRA for diagnostic coronary angiography was described by Campeau at the Montreal Heart Institute in 1989 who reported the first series of 100 patients [
1] and concluded that TRA may become as effective as and safer than the transbrachial approach, at that time the alternative to the transfemoral approach (TFA). In 1992 Kiemeneij and Laarman performed the first transradial (TR) percutaneous coronary angioplasty and, in 1993, the first coronary stenting by TRA. Nevertheless, despite the fact that the TRA for coronary procedures has gained progressive acceptance since its first introduction more than 20 years ago, it still accounts for less than 10% of all procedures worldwide. TRA is performed heterogeneously around the world, mainly in Europe, Canada and Asia where some high-volume operators perform more than 95% of coronary procedures by TRA. In the U.S. only 1.3% of PCI were performed by TRA in 2007, 4.3% in 2009 and this figure may now be over 10%. In Switzerland a minority of operators, mainly in the west of the country, use TRA as the default approach [
2,
3].
Allen’s test and plethysmography for patient selection
Since the introduction of TRA a dual-hand circulation assess has been recommended in order to avoid ischaemic hand complications due to radial artery occlusion following the procedure (incidence 3–10%). The most popular test is the Allen’s test, which is easy to use but remains subjective. The test is considered normal if hand recolouration occurs within ≤9 seconds. In 2004 Barbeau et al. [
4] showed in 1010 consecutive patients that a method combining pulse oxymetry and plethysmography is more accurate and objective than the Allen’s test (
Figure 1). Plethysmography type D (loss of the pulse trace without recovery within two minutes of radial artery compression) is the only method not recommended for TRA.
Advantages of TRA
TRA versus TFA: bleeding
Major advantages of TRA compared to TFA are the reduction of vascular complications and bleeding both representing major prognostic predictors after PCI. Two important meta-analysis of randomised trials compared TRA and TFA for diagnostic and therapeutic coronary procedures. The first published in 2004 by Agostoni et al. [
5] included 12 randomised trials performed between 1989 and 2003 with a total of 3224 patients. Results showed that TRA is associated with a significantly lower rate of entry site complications (0.3% vs. 2.8%, p <0.0001).
In 2009, Jolly et al. [
6] published a second metaanalysis of 23 randomised trials between 1994 and 2008 with a total of 7020 patients. In this analysis, only major bleeding (fatal bleeding, haemoglobin drop ≥3 g/dl, transfusion, need for surgery, intracranial haemorrhage) were considered. Again results were positive for TRA with a 73% decrease of major bleeding (0.05% vs. 2.3%, p <0.01) and a trend in MACE (death, myocardial infarction or stroke) reduction (2.5% vs. 3.8%, p = 0.058). Following coronary angiography and angioplasty, TRA reduced the absolute risk of major bleeding by 1.4% (p = 0.02) and 1.8% (p = 0.001) respectively. Fifty-six coronary angioplasties need to be performed by TRA to prevent one major bleeding event (number needed to treat [NNT] of 56). The most significant absolute risk reduction in major bleeding (3.1%, p = 0.001) was observed in cases of myocardial infarction with ST segment elevation (STEMI).
TRA versus TFA: impact on mortality in the pre-RIVAL era?
In multiple studies major bleeding events have been shown to be independently associated with a marked increase of the risk of death and ischaemic events in patients with acute coronary syndrome (ACS) [
7,
8]. Moreover, vascular complications and the need for transfusion have been implicated in excess deaths after PCI [
9,
10]. The MORTAL study [
11] retrospectively examined the association between access site, transfusion and outcomes in more than 32 000 consecutive patients undergoing PCI in British Columbia and concluded that by reducing vascular access site complications, TRA led to a 50% reduction in transfusion rate (1.4% vs. 2.8%), a relative reduction in 30-day mortality of 29% and one-year mortality of 17%, which corresponds to an approximately 1% absolute risk reduction at one year. The RIVIERA study [
12], a large prospective international registry (7962 patients), showed that TRA is associated with a significant reduction in PCIrelated mortality or myocardial infarction. Similar results are found in the PREVAIL study, a multicentre Italian registry [
13]. The subgroup of STEMI patients was examined in a meta-analysis by Vorobcsuk et al. [
14] and included 12 studies (5 randomised and 7 nonrandomised trials) with a total of 3324 STEMI patients. This meta-analysis showed that TRA significantly reduced major bleeding (0.77% vs. 2.61%, p = 0.0001); a composite endpoint of death, myocardial infarction or stroke (3.65% vs. 6.55%, p = 0.001); and mortality (2.04% vs. 3.06%, p = 0.01) compared to TFA in the setting of STEMI. All these studies have the inherent limitations of retrospective analyses of non-randomised data from registries and observational studies or small randomised trials.
Which subgroup of patients can benefit from this technique?
All patients will benefit from the TRA, but especially populations at high risk of vascular complications i.e., elderly patients, over and underweight patients, women, patients with high blood pressure, anticoagulation therapy, chronic renal disease or with an ACS/STEMI.
Elderly patients
Advanced age is a risk factor for vascular complications. TRA may sometimes be technically more demanding because of the more common vascular tortuosity and calcification in an elderly population. OCTOPLUS [
15], a multicentre randomised comparison of TRA versus TFA in 377 octogenarians showed a significant reduction of vascular complications (1.6% vs. 6.5%, p = 0.029), defined as complications requiring surgery, transfusion, discharge delay or related to limb ischaemia. With the exception of one radial haematoma without consequences, all vascular complications occurred in patients treated with TFA. Interestingly, a similar crossover rate from one approach to the other was observed (8.9% for TRA vs. 8.1% for TFA, p = NS).
A more recently published study [
16] of 307 patients aged 75 years or more again showed a lower major complication rate (bleeding requiring surgery or transfusion, stroke) following TRA compared to TFA (0% vs. 3.2%, p <0.001).
Women
Women represent a high-risk population for bleeding. Since the radial artery is often smaller in women, interventionalists may sometimes be restricted to 5 French (F) guiding catheters to perform a PCI, instead of the traditional 6F, which permits more complex techniques (bifurcation lesions, atherectomy, aspiration devices). Hydrophilic Sheathless Eaucath catheters (Asahi Intecc, Japan) are an attractive alternative, allowing the use of a 6F-guiding catheter without sheath (the outer diameter [2.16 mm] is smaller than a 5F [2.29 mm] sheath).
In 2007 Pristipino et al. analysed the gender influence with respect to bleeding during percutaneous coronary procedures in more than 2900 patients [
17] in a prospective registry. Among 838 women (33% of TRA) no major bleeding occurred after TRA compared to 4.1% after TFA (p = 0.0008). Minor bleeding events were also less frequent after TRA (6.3% vs. 39.4%, p = 0.00001). On multivariate analysis, female gender was among the independent predictors of major bleeding with an odds ratio (OR) of 4.5 (95% CI 2.2 to 9.0). The other independent predictors of major bleeding were TFA (OR 27.4, 95% confidence interval [CI] 3.8 to 199.9), glycoprotein IIb/IIIa inhibitors use (OR 5.6, 95% CI 2.7 to 11.9), age >70 years (OR 2.4, 95% CI 1.2 to 4.8), and ACS (OR 2.4, 95% CI 1.1 to 5.0).
Obese patients
Vascular complications after TFA for either coronary angiography or angioplasty are more frequent in this high risk population because of puncture and haemostasis difficulties and delay in haematoma detection.
The TROP registry [
18], a prospective non-randomised multicentre European registry of 555 obese patients (BMI >35 kg/m
2), showed that TRA significantly reduced vascular complications delaying hospital discharge and/or transfusion (0.8% vs. 5.1% for the TFA, p = 0.0009) and/or haematomas (1.8% vs. 10.2%, p <0.0001). Procedural time and hospital stay were significantly shorter in the TRA group with a high success rate (96%).
TRA versus TFA: primary PCI
The advantages of TRA are greater in primary PCI for STEMI when the risk of bleeding is highest in relation to aggressive anticoagulation and antiplatelet therapies. Importantly, several studies showed that radial access remains beneficial for STEMI patients, where rapid reperfusion is critical [
19].
The Vorobcsuk et al. [
14] meta-analysis showed significant benefits in using TRA compared to TFA in 3324 STEMI patients with respect to major bleeding, a composite endpoint of death, myocardial infarction or stroke and also mortality (2.04% vs. 3.06%, p = 0.01). Procedural and reperfusion times were similar between the two groups confirming the safety of TRA in this setting. Likewise, in the prospective study of Arzamendi et al. [
20] of 489 pts with STEMI, TRA is associated with a fourfold reduction in major bleeding events (4.2% vs. 16.8%, p <0.001) without compromising revascularisation time and with a significant decrease in major adverse cardiac events (cardiac death, myocardial infarction or target vessel revascularisation) at 12 months (2.9% vs. 14.3%, p <0.001) compared to TFA.
RIVAL, the contemporary randomised study
The RIVAL trial, the largest randomised multicentre comparison between TRA and TFA in patients with ACS, was recently published [
21] and provides contemporary data. This trial, with 7021 patients included between June 2006 and November 2010 in 32 countries, demonstrated that while the two approaches had similar overall safety (primary outcome: composite of death, myocardial infarction, stroke, or non-CABG major bleeding at 30 days; 3.7% for TRA vs. 4.0% for TFA, p = 0.50) and efficacy (PCI success rates, 95.4% for TRA vs. 95.2% for TFA, p = 0.83), the TRA for coronary angiography and PCI significantly reduced major vascular complications (1.4% vs. 3.7%, p <0.0001) by decreasing the incidence of large haematoma (1.2% vs. 3.0%, p <0.0001) and pseudo-aneurysm requiring closure (0.2% vs. 0.6%, p = 0.006).
Table 1.
Definitionofmajorbleeding.
Table 1.
Definitionofmajorbleeding.
This study has caused some controversy among the interventional community. Firstly, and surprisingly, there was no significant difference in major bleeding between the two approaches (0.7% in TRA vs. 0.9% in TFA, p = 0.23). Indeed, the rate of major bleeding was extremely low in the TFA group, lower than that reported in previous studies, probably because experienced and high-volume operators participated in this study and because of the improvement of contemporary material. Notably, in this trial involving ACS patients, two thirds of the major bleeding events were not related to vascular access site but were from gastrointestinal, intracranial and pericardial origins. These bleeding sources are not expected to be influenced by the vascular approach. A final consideration is the rigorous definition used for major bleeding (table 1). In a post-hoc analysis, when the bleeding definition from the ACUITY trial [
22] was used, the rate of major bleeding was then significantly less with TRA than TFA (p <0.0001).
The subgroup analyses, with their inherent limitations, suggest that TRA PCI lowered the primary composite endpoint in STEMI PCI (3.1% vs. 5.2%, p = 0.026) and also in centres with operators performing >146 radial PCI/year (1.6% vs. 3.2%, p = 0.015). They also suggest a benefit for TRA over TFA for access site crossover, major vascular complications and the composite of death, myocardial infarction and stroke (1.3% vs. 2.7%, p = 0.027) at centres with a high proportion of TRA PCI. On the other hand, there was no significant interaction with femoral versus radial access (p = 0.75) when the primary outcome was analysed with respect to TFA experience.
The most striking result in favour of TRA in the subgroup analyses was the reduction in mortality for PCI in STEMI patients (1.3% vs. 3.2%, p = 0.006). Finally, more patients preferred their subsequent procedure to be performed by TRA (90.2% of patients after TRA vs. 50.7% of patients after TFA, p <0.0001); although this preference could be biased as most patients did not experience the other approach, it corresponds to our own experience. Patient preference could be a drive for change in the centres performing only or mainly TFA.
Disadvantages and limitations of TRA
Despite its various advantages, TRA is not embraced by the whole interventional community. Highly experienced TFA operators are reluctant to retrain in TRA. Indubitably, anatomical variations in the arm or subclavian tortuosity may represent a real challenge especially during the learning curve and result in longer procedural time and more radiation. With experience these technical challenges can be largely overcome. In the Tip and Tricks manuscript [
23] we hope to share our experience in order to facilitate your learning curve.
Indeed longer procedural time and higher radiation exposure during coronary angiogram and/or PCI are reported after TRA compared to TFA [
6,
24]. As shown by the meta-analysis of Jolly, procedural time in TRA is influenced by the operator’s expertise (+4.8 min, 95% CI 3.7–5.8 min for nonradial experts and +1.7 min, 95% CI 0.7–2.6 min for radial experts). Fluoroscopy time was also longer after TRA than TFA (+0.4 minutes, 95% CI 0.3–0.5 min, p <0.001). Interestingly in the contemporary trial RIVAL, procedural time was similar between TRA and TFA but there was a significant difference in fluoroscopy time in favour of TFA (9.8 min [5.8–15.0] for TRA versus 8.0 min [4.5–13.0] for TFA, p <0.0001). This might be partially explained by the more frequent necessity to control wire progression by fluoroscopy in the arm or at the level of subclavian tortuosity than in the aorto-iliac segment when TFA is performed. Indeed, once the guiding catheter is cannulated in the coronary ostium, procedural time and radiation exposure should be similar between TRA and TFA in the vast majority of cases. With respect to procedural time and radiation exposure, crossover to TFA should be considered in cases of complex anatomy.
In TRA literature, the rate of access site crossover remains higher in TRA than TFA. In the 19 randomised trials with crossover data available included in the meta-analysis of Jolly et al. [
6], the mean rate of access site crossover was 5.9% for TRA (range 0 to 23%) and 1.4% in TFA (range 0 to 8.1%). The more recent RIVAL study [
21] showed similar crossover rates (7.6% vs. 2.2%). In this last study, the reasons for changing the access site were mainly radial spasm, subclavian tortuosity and radial artery loop. Subclavian tortuosity is—in our experience—the most difficult technical challenge to overcome, especially when a RCA PCI is required. One of the rare studies showing a similar crossover rate [
15] targeted elderly patients suggesting that tortuosity and atherosclerosis on the ilio-femoral axes also represent a technical challenge in this population.
Based on the assessment of the ulnopalmar arterial arches with pulse oxymetry and plethysmography, only 1.5% (2% of men and 0.3% of woman with a plethysmography type D) were turned down for TRA by either right or left access in a large series from Quebec [
4]. In an Internet survey on transradial practice among more than 1000 interventional cardiologists, 23% answered that they do not assess dual hand circulation before procedures [
25]. We believe this is not recommended especially for the less experienced as the risk of radial occlusion might be higher during the learning curve. Even though radial occlusion is asymptomatic in the vast majority of cases, hand ischaemia represents an avoidable complication that should never happen.
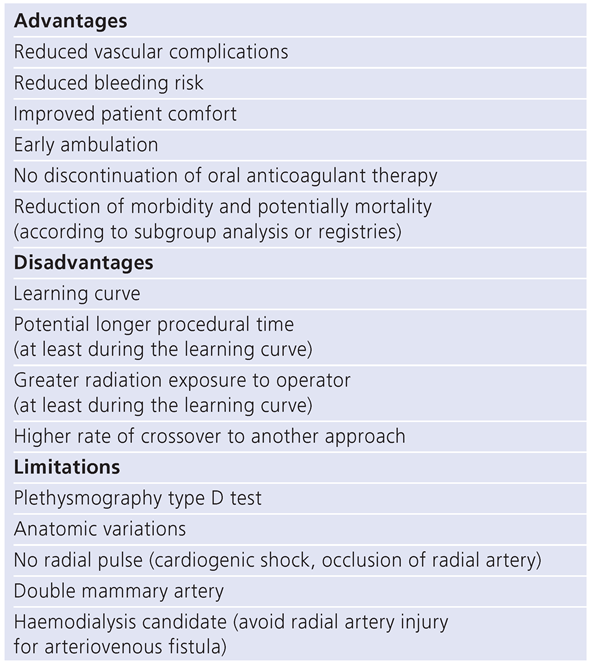
TRA is not the preferred approach in specific situations such as patients with double mammary bypass grafts. In this clinical setting TRA is technically feasible through the right access, but it can be a real challenge with an increased risk of complications. Therefore the benefit/risk ratio is unfavourable. TFA should also be the approach of choice in patients with cardiogenic shock without a palpable radial pulse or patients at risk of needing haemodialysis when the radial artery must be preserved for a potential arteriovenous fistula. Complex PCI, such as for chronic total occlusion, are feasible by TRA, but operators should be highly experienced with TRA. However TFA remains an excellent approach in complex procedures. Advantages, disadvantages and limitations of TRA are summarised in table 2.
Table 2.
Advantages, disadvantagesandlimitationsoftransradialapproach.
Table 2.
Advantages, disadvantagesandlimitationsoftransradialapproach.
Conclusion
Several studies, meta-analysis and the recent randomised trial RIVAL showed a dramatic decrease in access site complications with TRA compared to TFA. By reducing vascular complications and major bleeding, TRA has a potential impact on morbidity and probably on mortality after coronary angioplasty, especially for STEMI patients. Further studies are required to confirm these hypotheses. This technique considerably improves patient comfort and allows rapid mobilisation. Even if the learning curve is longer compared to TFA, the success rate of a TR procedure is similar to that obtained with TFA. Owing to its obvious benefits, there is no longer any justification to ignore the transradial approach and patient preference will definitely contribute to motivating the femoralist to make the leap into the transradial world.