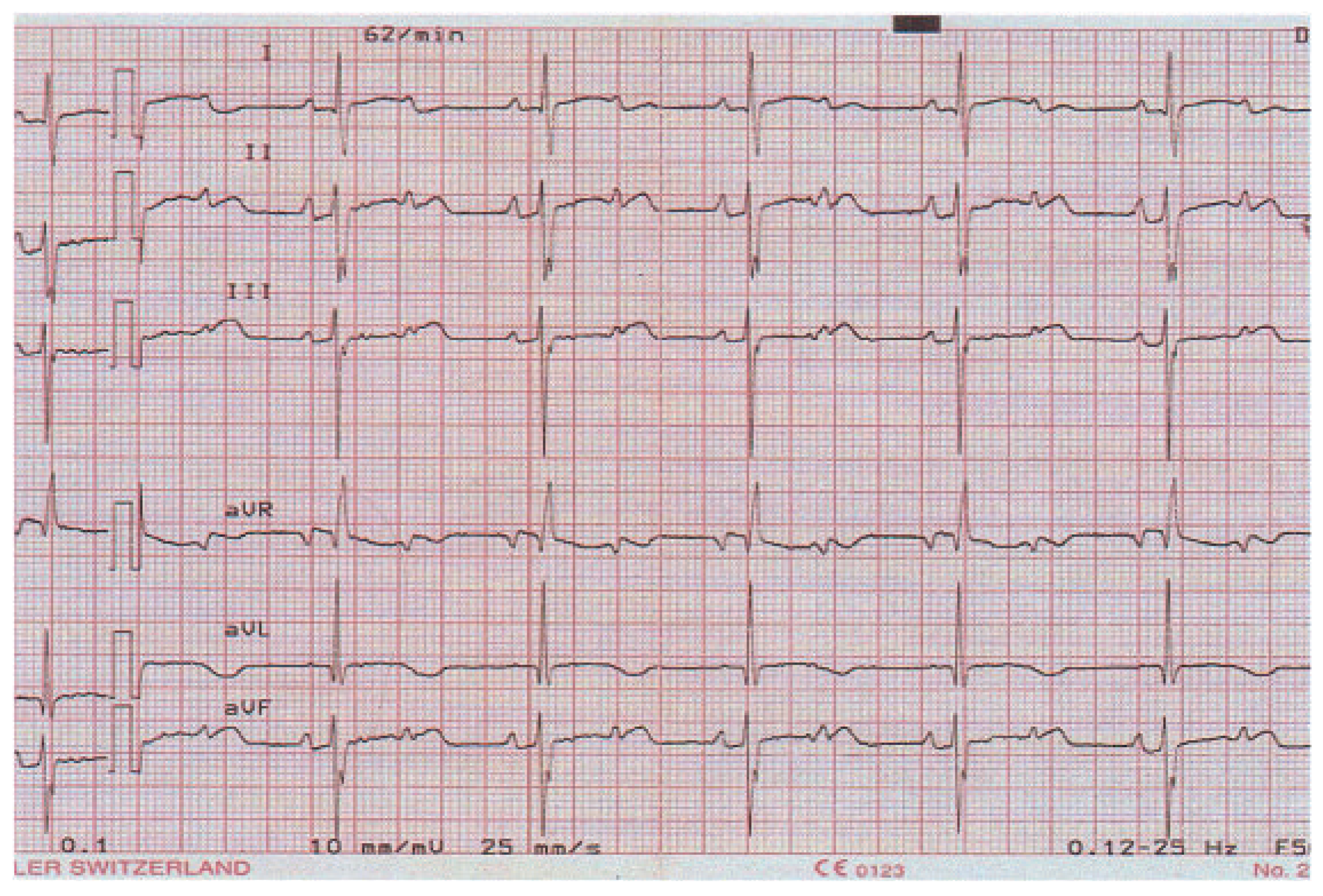
Neonatal Bradycardia
Case presentation
Question
Discussion
Conflicts of Interest
References
- Trippel, D.L.; Parsons, M.K.; Gillette, P.C. Infants with long QT syndrome and 2:1 atrioventricular block. Am. Heart J. 1995, 130, 1130–1134. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.C.; Acharfi, S.; Wu, M.F.; et al. A novel SCN5A mutation manifests as a malignant form of long QT syndrome with perinatal onset of tachycardia/bradycardia. Cardiovasc. Res. 2004, 64, 268–278. [Google Scholar] [CrossRef] [PubMed]
- Tomek, V.; Skovranek, J.; Gebauer, R.A. Prenatal diagnosis and management of fetal long QT syndrome. Pediatr. Cardiol. 2009, 30, 194–196. [Google Scholar] [CrossRef] [PubMed]
© 2010 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Navarini, S.; Pavlovic, M.; Schwick, N.; Pfammatter, J.-P. Neonatal Bradycardia. Cardiovasc. Med. 2010, 13, 141. https://doi.org/10.4414/cvm.2010.01495
Navarini S, Pavlovic M, Schwick N, Pfammatter J-P. Neonatal Bradycardia. Cardiovascular Medicine. 2010; 13(4):141. https://doi.org/10.4414/cvm.2010.01495
Chicago/Turabian StyleNavarini, Susanne, Mladen Pavlovic, Nicola Schwick, and Jean-Pierre Pfammatter. 2010. "Neonatal Bradycardia" Cardiovascular Medicine 13, no. 4: 141. https://doi.org/10.4414/cvm.2010.01495
APA StyleNavarini, S., Pavlovic, M., Schwick, N., & Pfammatter, J.-P. (2010). Neonatal Bradycardia. Cardiovascular Medicine, 13(4), 141. https://doi.org/10.4414/cvm.2010.01495



