Impact of a Cardiac Rehabilitation Programme on Exercise Capacity, Parameters of Left Ventricular Function and Health-Related Quality of Life in Chronic Heart Failure Patients
Abstract
Introduction
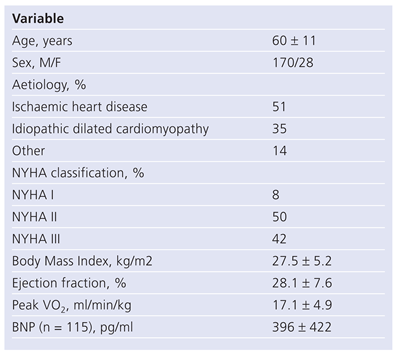
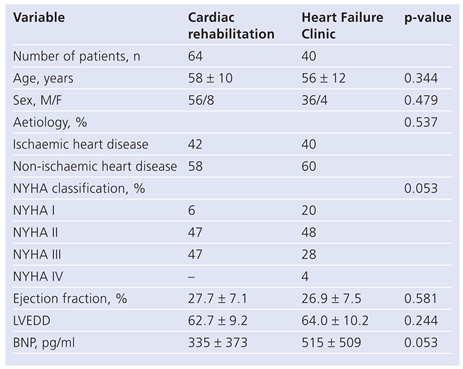
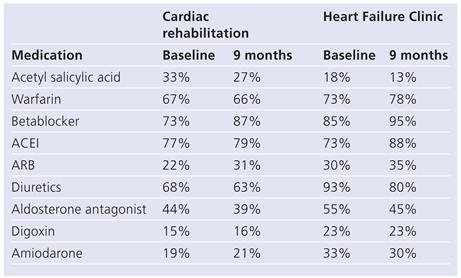
Methods
Cardiac rehabilitation programme
Exercise testing
Health-Related Quality of Life Assessment
Statistical analysis
Results
Exercise capacity
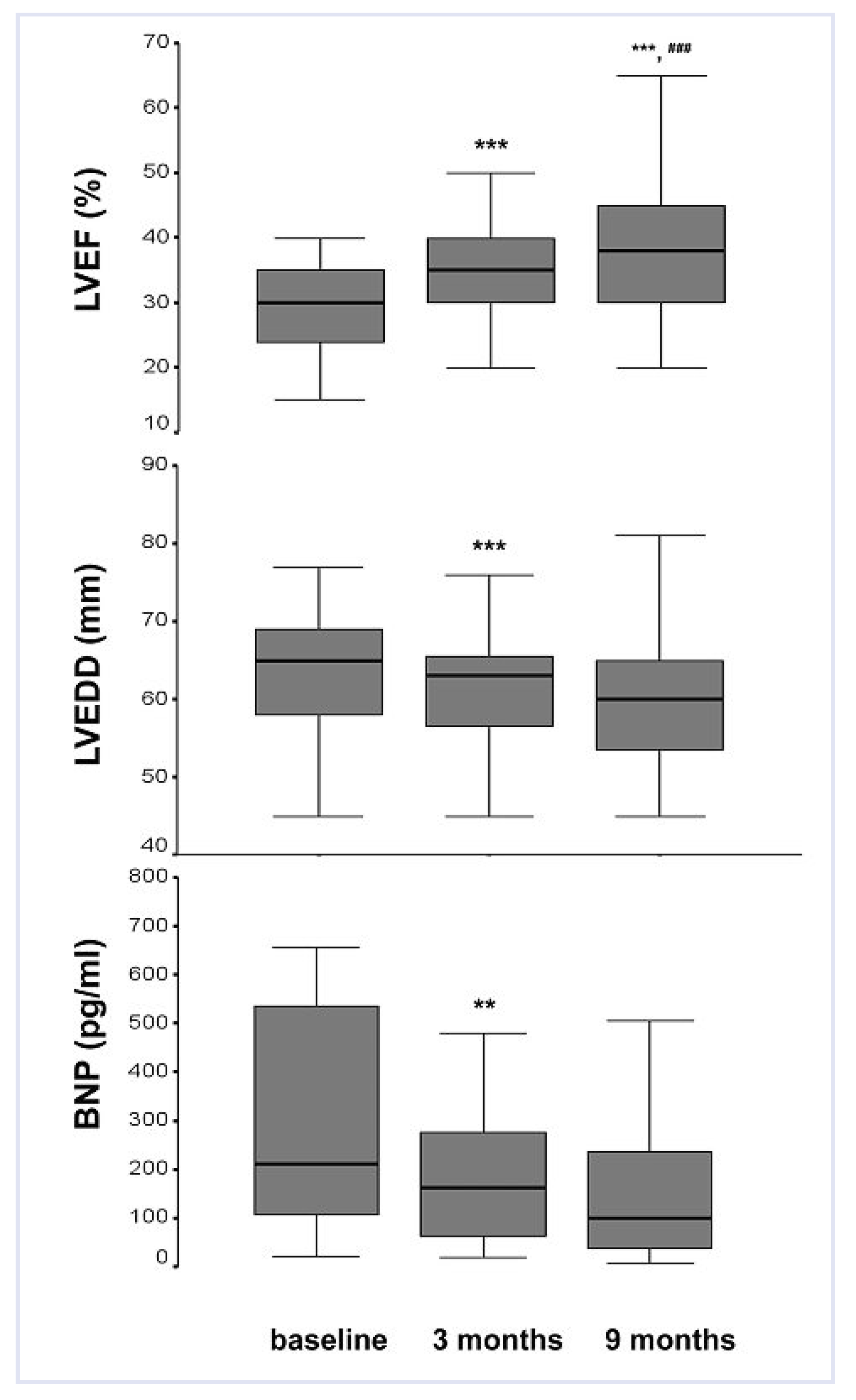
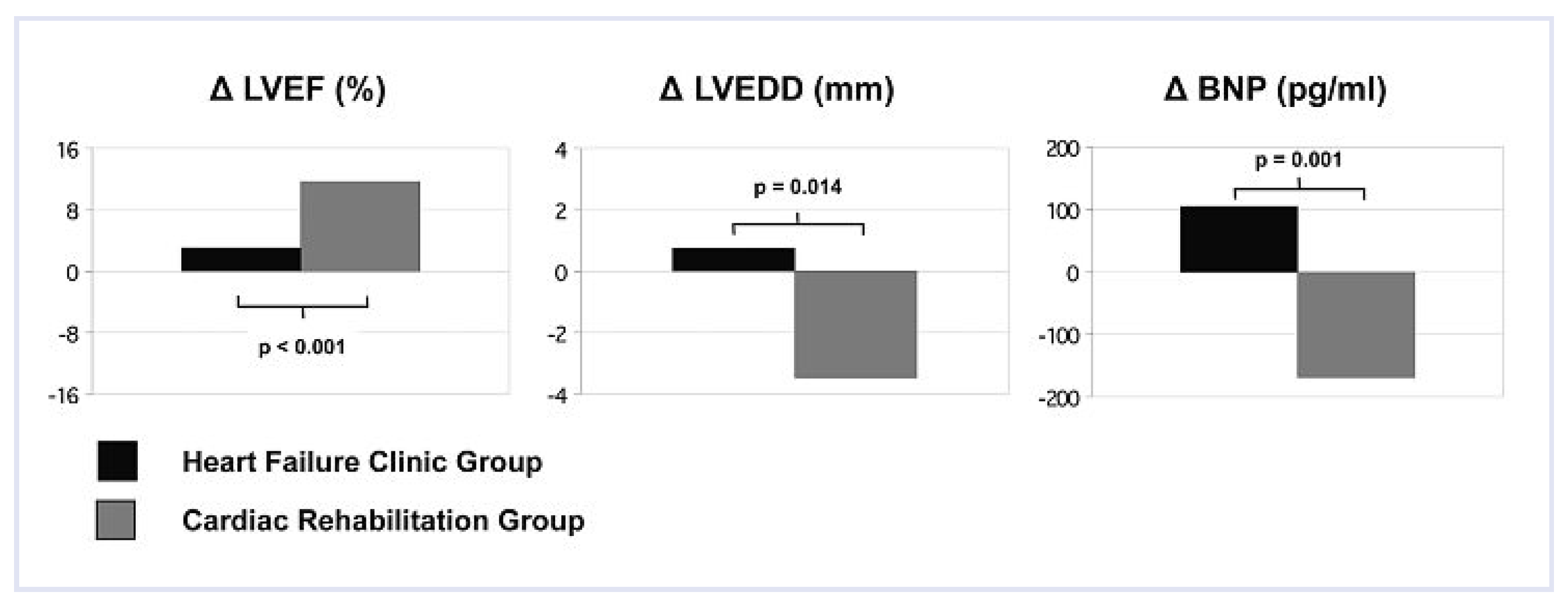
Left ventricular function, diameter and BNP
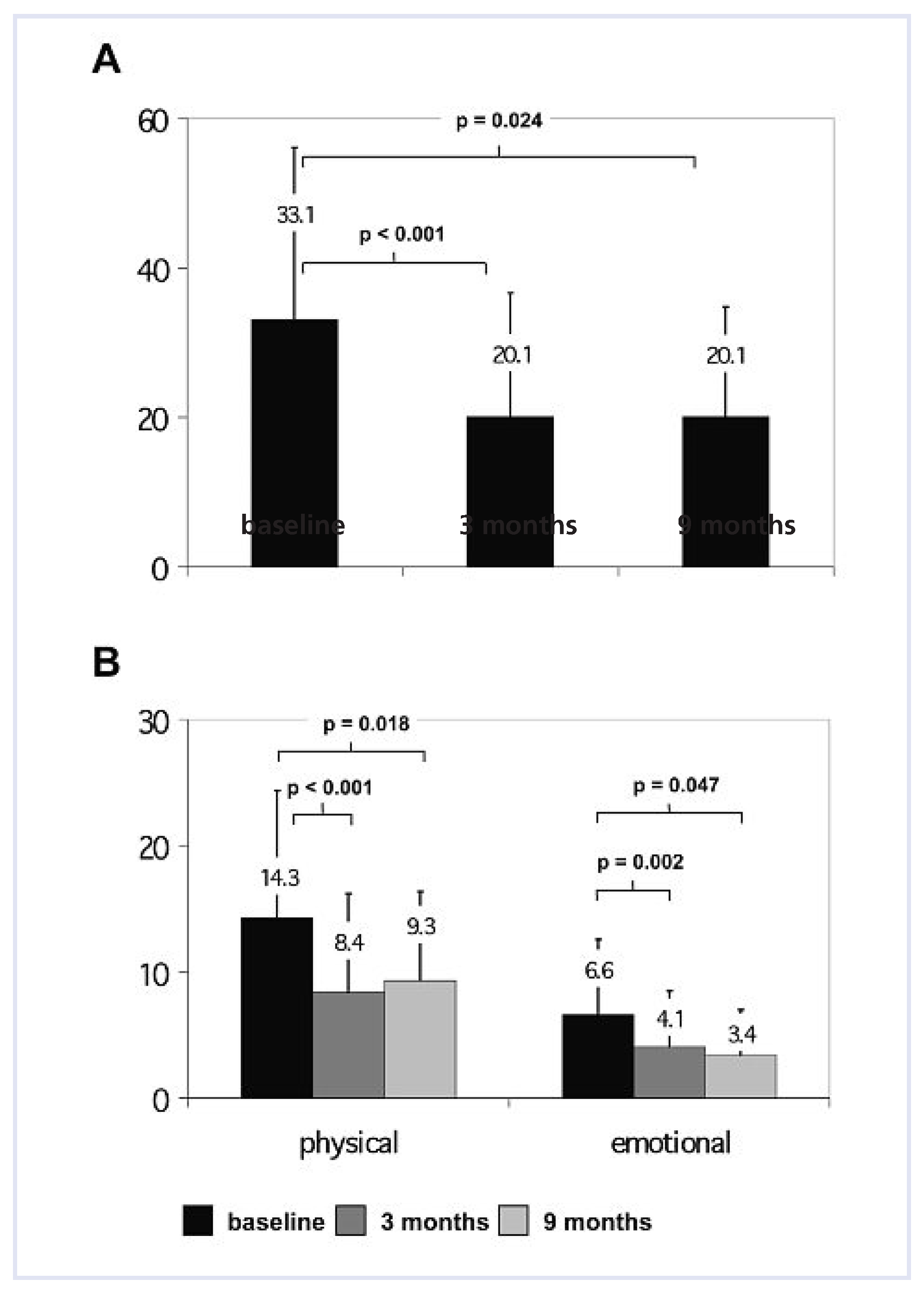
Health-Related Quality of Life
Discussion
Study limitations
Conclusion
Conflicts of Interest
References
- Hobbs, F.D.; Kenkre, J.E.; Roalfe, A.K.; Davis, R.C.; Hare, R.; Davies, M.K. Impact of heart failure and left ventricular systolic dysfunction on quality of life: A cross-sectional study comparing common chronic cardiac and medical disorders and a representative adult population. Eur Heart J. 2002, 23, 1867–1876. [Google Scholar] [CrossRef]
- Juenger, J.; Schellberg, D.; Kraemer, S.; Haunstetter, A.; Zugck, C.; Herzog, W.; et, al. Health related quality of life in patients with congestive heart failure: Comparison with other chronic diseases and relation to functional variables. Heart 2002, 87, 235–241. [Google Scholar] [CrossRef]
- Metra, M.; Ponikowski, P.; Dickstein, K.; McMurray, J.J.; Gavazzi, A.; Berghm, C.H.; et, al. Advanced chronic heart failure: A position statement from the Study Group on Advanced Heart Failure of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2007, 9, 684–694. [Google Scholar] [CrossRef] [PubMed]
- The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): A randomised trial. Lancet 1999, 353, 9–13. [CrossRef]
- Hjalmarson, A.; Goldstein, S.; Fagerberg, B.; Wedel, H.; Waagstein, F.; Kjekshus, J.; et, al. Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: The Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group. JAMA 2000, 283, 1295–1302. [Google Scholar] [CrossRef] [PubMed]
- Packer, M.; Coats, A.J.; Fowler, M.B.; Katus, H.A.; Krum, H.; Mohacsi, P.; et, al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001, 344, 1651–1658. [Google Scholar] [CrossRef]
- Smits, J.M.; Vanhaecke, J.; Haverich, A.; de Vries, E.; Smith, M.; Rutgrink, E.; et al. Three-year survival rates for all consecutive heart-only and lungonly transplants performed in Eurotransplant, 1997–1999. Clin Transpl. 2003, 89–100. [Google Scholar]
- Taylor, D.O.; Edwards, L.B.; Aurora, P.; Christie, J.D.; Dobbels, F.; Kirk, R.; et al. Registry of the International Society for Heart and Lung Transplantation: Twenty-fifth official adult heart transplant report—2008. J Heart Lung Transplant. 2008, 27, 943–956. [Google Scholar] [CrossRef]
- Swedberg, K.; Cleland, J.; Dargie, H.; Drexler, H.; Follath, F.; Komajda, M.; et al. Guidelines for the diagnosis and treatment of chronic heart failure: Executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J. 2005, 26, 1115–1140. [Google Scholar] [CrossRef]
- Pina, I.L.; Apstein, C.S.; Balady, G.J.; Belardinelli, R.; Chaitman, B.R.; Duscha, B.D.; et al. Exercise and heart failure: A statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation 2003, 107, 1210–1225. [Google Scholar] [CrossRef]
- Grady, K.L.; Dracup, K.; Kennedy, G.; Moser, D.K.; Piano, M.; Stevenson, L.W.; et al. Team management of patients with heart failure: A statement for healthcare professionals from The Cardiovascular Nursing Council of the American Heart Association. Circulation 2000, 102, 2443–2456. [Google Scholar] [CrossRef] [PubMed]
- Gwadry-Sridhar, F.H.; Flintoft, V.; Lee, D.S.; Lee, H.; Guyatt, G.H. A systematic review and meta-analysis of studies comparing readmission rates and mortality rates in patients with heart failure. Arch Intern Med. 2004, 164, 2315–2320. [Google Scholar] [CrossRef] [PubMed]
- McAlister, F.A.; Lawson, F.M.; Teo, K.K.; Armstrong, P.W. A systematic review of randomized trials of disease management programs in heart failure. Am J Med. 2001, 110, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Davos, C.; Francis, D.P.; Coats, A.J. Exercise training metaanalysis of trials in patients with chronic heart failure (ExTraMATCH). BMJ 2004, 328, 189. [Google Scholar] [CrossRef]
- Rees, K.; Taylor, R.S.; Singh, S.; Coats, A.J.; Ebrahim, S. Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev. 2004, CD003331. [Google Scholar]
- Guyatt, G.H.; Sullivan, M.J.; Thompson, P.J.; Fallen, E.L.; Pugsley, S.O.; Taylor, D.W.; et al. The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985, 132, 919–923. [Google Scholar]
- Haykowsky, M.J.; Liang, Y.; Pechter, D.; Jones, L.W.; McAlister, F.A.; Clark, A.M. A meta-analysis of the effect of exercise training on left ventricular remodeling in heart failure patients: The benefit depends on the type of training performed. J Am Coll Cardiol. 2007, 49, 2329–2336. [Google Scholar] [CrossRef]
- Braith, R.W.; Welsch, M.A.; Feigenbaum, M.S.; Kluess, H.A.; Pepine, C.J. Neuroendocrine activation in heart failure is modified by endurance exercise training. J Am Coll Cardiol. 1999, 34, 1170–1175. [Google Scholar] [CrossRef]
- Hambrecht, R.; Gielen, S.; Linke, A.; Fiehn, E.; Yu, J.; Walther, C.; et al. Effects of exercise training on left ventricular function and peripheral resistance in patients with chronic heart failure: A randomized trial. JAMA 2000, 283, 3095–3101. [Google Scholar] [CrossRef]
- Passino, C.; Severino, S.; Poletti, R.; Piepoli, M.F.; Mammini, C.; Clerico, A.; et al. Aerobic training decreases B-type natriuretic peptide expression and adrenergic activation in patients with heart failure. JAm Coll Cardiol. 2006, 47, 1835–1839. [Google Scholar] [CrossRef]
- Conraads, V.M.; Beckers, P.; Vaes, J.; Martin, M.; Van Hoof, V.; De Maeyer, C.; et al. Combined endurance/resistance training reduces NT-proBNP levels in patients with chronic heart failure. Eur Heart J. 2004, 25, 1797–1805. [Google Scholar] [CrossRef] [PubMed]
- Arad, M.; Adler, Y.; Koren-Morag, N.; Natanzon, S.; Sela, B.A.; Ben Dov, I.; et al. Exercise training in advanced heart failure patients: Discordance between improved exercise tolerance and unchanged NT-proBNP levels. Int J Cardiol. 2007. [Google Scholar] [CrossRef]
- Jonsdottir, S.; Andersen, K.K.; Sigurosson, A.F.; Sigurosson, S.B. The effect of physical training in chronic heart failure. Eur J Heart Fail. 2006, 8, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Anand, I.S.; Fisher, L.D.; Chiang, Y.T.; Latini, R.; Masson, S.; Maggioni, A.P.; et al. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (ValHeFT). Circulation. 2003, 107, 1278–1283. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Ferrer, M.; Gandek, B.; Ware JEJr Aaronson, N.K.; Mosconi, P.; et al. Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004, 13, 283–298. [Google Scholar] [CrossRef]
- Lewis, E.F.; Johnson, P.A.; Johnson, W.; Collins, C.; Griffin, L.; Stevenson, L.W. Preferences for quality of life or survival expressed by patients with heart failure. J Heart Lung Transplant. 2001, 20, 1016–1024. [Google Scholar] [CrossRef]
- Leidy, N.K.; Rentz, A.M.; Zyczynski, T.M. Evaluating Health-related quality-of-life outcomes in patients with congestive heart failure. A review of recent randomised controlled trials. Pharmacoeconomics 1999, 15, 19–46. [Google Scholar] [CrossRef]
- van Tol, B.A.; Huijsmans, R.J.; Kroon, D.W.; Schothorst, M.; Kwakkel, G. Effects of exercise training on cardiac performance, exercise capacity and quality of life in patients with heart failure: A meta-analysis. Eur J Heart Fail. 2006, 8, 841–850. [Google Scholar] [CrossRef]
 |
 |
 |
 |
© 2010 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Schmid, J.-P.; Blatter-Bühler, P.; Gaillet, R.; Binder, R.K.; Schmid, R.W.; Mohacsi, P.; Saner, H. Impact of a Cardiac Rehabilitation Programme on Exercise Capacity, Parameters of Left Ventricular Function and Health-Related Quality of Life in Chronic Heart Failure Patients. Cardiovasc. Med. 2010, 13, 86. https://doi.org/10.4414/cvm.2010.01486
Schmid J-P, Blatter-Bühler P, Gaillet R, Binder RK, Schmid RW, Mohacsi P, Saner H. Impact of a Cardiac Rehabilitation Programme on Exercise Capacity, Parameters of Left Ventricular Function and Health-Related Quality of Life in Chronic Heart Failure Patients. Cardiovascular Medicine. 2010; 13(3):86. https://doi.org/10.4414/cvm.2010.01486
Chicago/Turabian StyleSchmid, Jean-Paul, Patricia Blatter-Bühler, Raymond Gaillet, Ronald K. Binder, Raphaela Walker Schmid, Paul Mohacsi, and Hugo Saner. 2010. "Impact of a Cardiac Rehabilitation Programme on Exercise Capacity, Parameters of Left Ventricular Function and Health-Related Quality of Life in Chronic Heart Failure Patients" Cardiovascular Medicine 13, no. 3: 86. https://doi.org/10.4414/cvm.2010.01486
APA StyleSchmid, J.-P., Blatter-Bühler, P., Gaillet, R., Binder, R. K., Schmid, R. W., Mohacsi, P., & Saner, H. (2010). Impact of a Cardiac Rehabilitation Programme on Exercise Capacity, Parameters of Left Ventricular Function and Health-Related Quality of Life in Chronic Heart Failure Patients. Cardiovascular Medicine, 13(3), 86. https://doi.org/10.4414/cvm.2010.01486




