Atrial Arrhythmia in the Intensive Care Unit
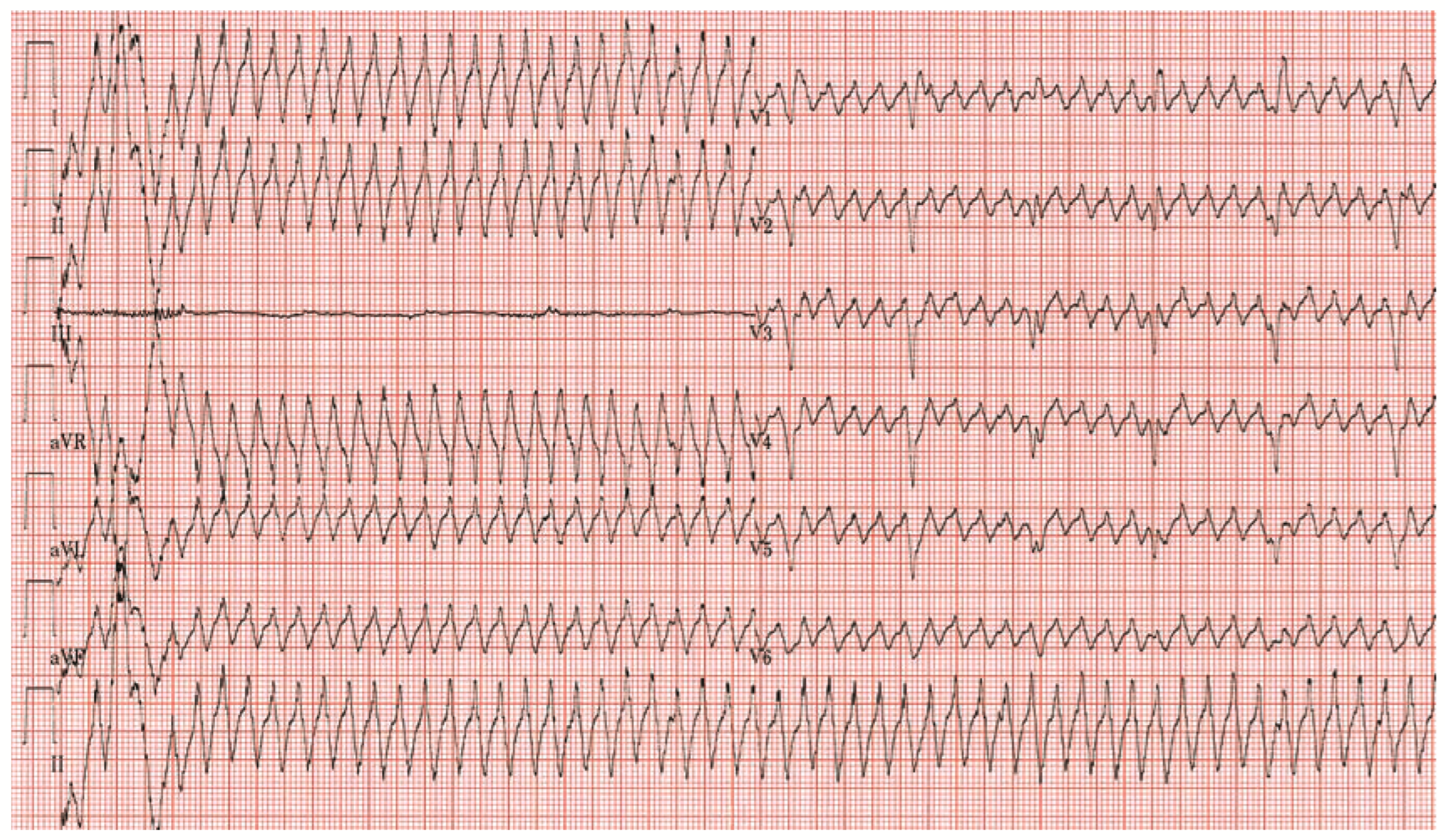
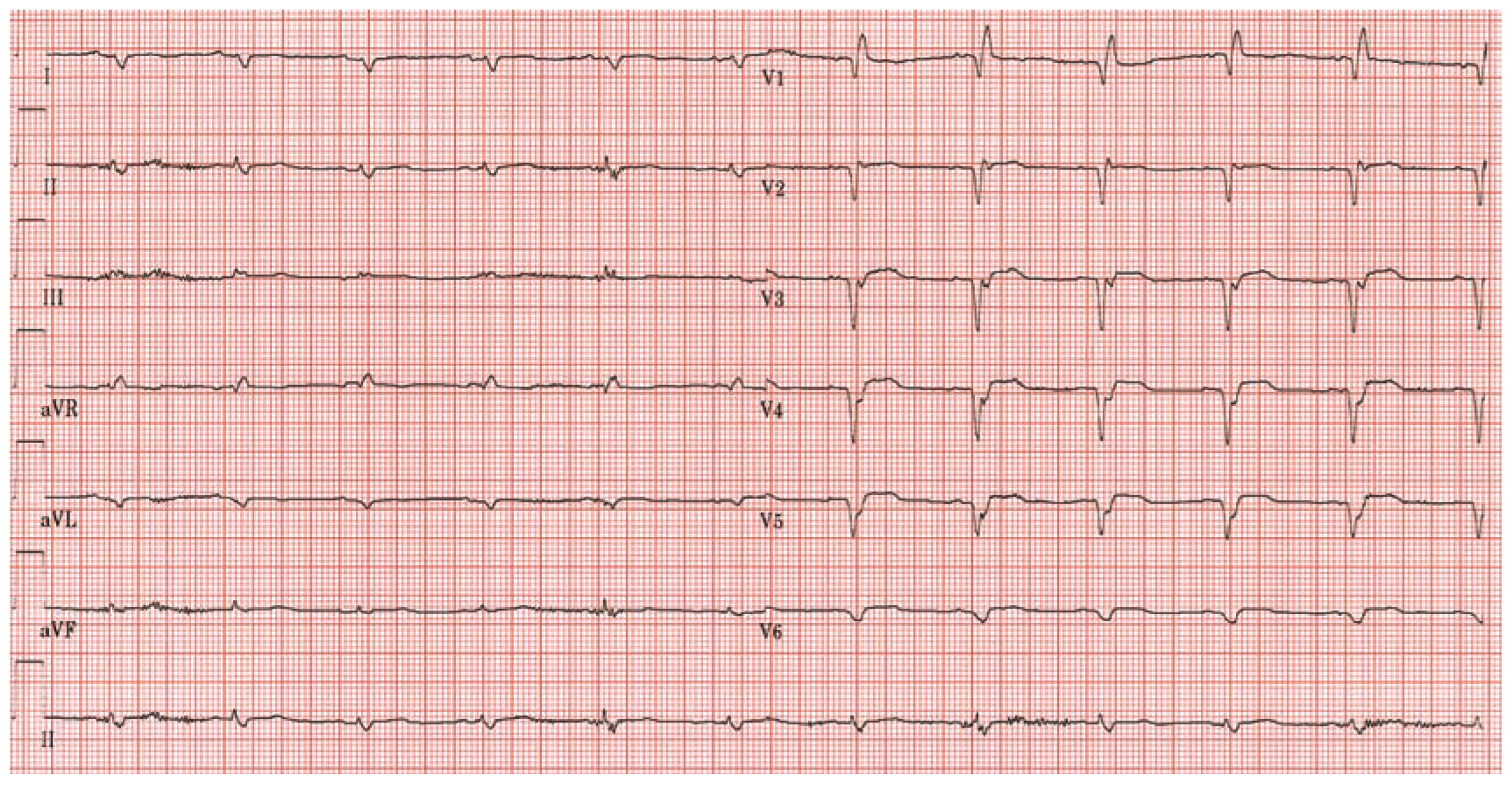
Case report
Explanatory answers
References
- Graansma, C.; Liu, T.T.; Tobe, S.W. A simple solution to pseudoarrhythmia during continuous renal replacement therapy. CANNT J 2004, 14, 24–5. [Google Scholar] [PubMed]
- Vanerio, G. Tremor as a cause of pseudoatrial flutter. Am. J. Geriatr. Cardiol. 2007, 16, 106–8. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, L.; Turner, D.R. Parkinson’s tremor mimicking ventricular tachycardia. Age Ageing 2005, 34, 410–1. [Google Scholar] [CrossRef] [PubMed]
- Austin, S.M.; Flach, S.D.; Gaines, C.M. Atrial flutter simulated by a portable compact disk player. Mayo. Clin. Proc. 2007, 82, 383–4. [Google Scholar] [CrossRef] [PubMed]
- Knight, B.P.; Pelosi, F.; Michaud, G.F.; Strickberger, S.A.; Morady, F. Clinical consequences of electrocardiographic artifact mimicking ventricular tachycardia. N. Engl. J. Med. 1999, 341, 1270–4. [Google Scholar] [CrossRef] [PubMed]
© 2008 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Ritter, S.; Maggiorini, M. Atrial Arrhythmia in the Intensive Care Unit. Cardiovasc. Med. 2008, 11, 64. https://doi.org/10.4414/cvm.2008.01309
Ritter S, Maggiorini M. Atrial Arrhythmia in the Intensive Care Unit. Cardiovascular Medicine. 2008; 11(2):64. https://doi.org/10.4414/cvm.2008.01309
Chicago/Turabian StyleRitter, Simon, and Marco Maggiorini. 2008. "Atrial Arrhythmia in the Intensive Care Unit" Cardiovascular Medicine 11, no. 2: 64. https://doi.org/10.4414/cvm.2008.01309
APA StyleRitter, S., & Maggiorini, M. (2008). Atrial Arrhythmia in the Intensive Care Unit. Cardiovascular Medicine, 11(2), 64. https://doi.org/10.4414/cvm.2008.01309



