Sudden Cardiac Arrest in the Region of Lausanne: A 5 years Consecutive Observational Study
Summary
Résumé
Introduction
Method
- Definitions
Results
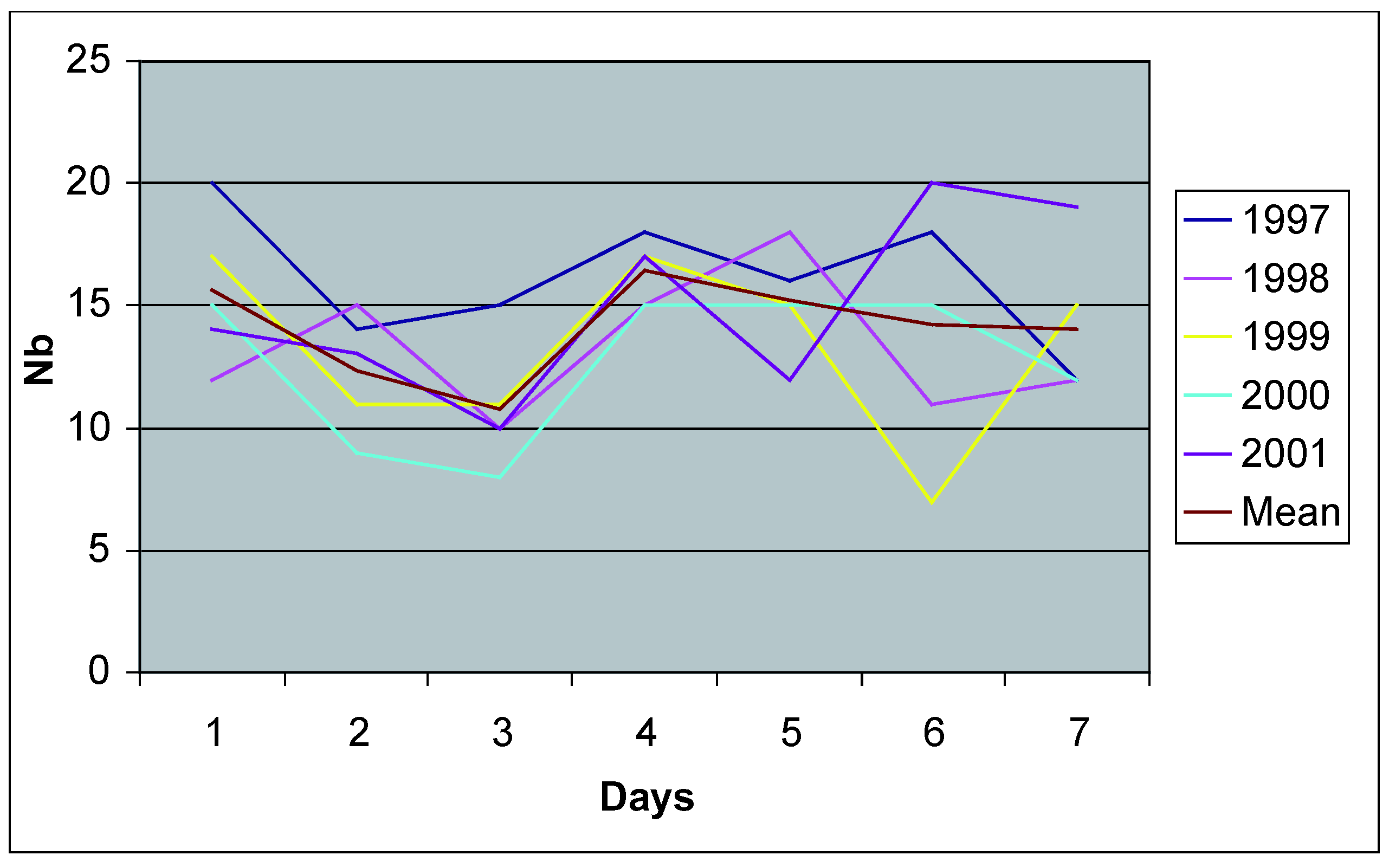
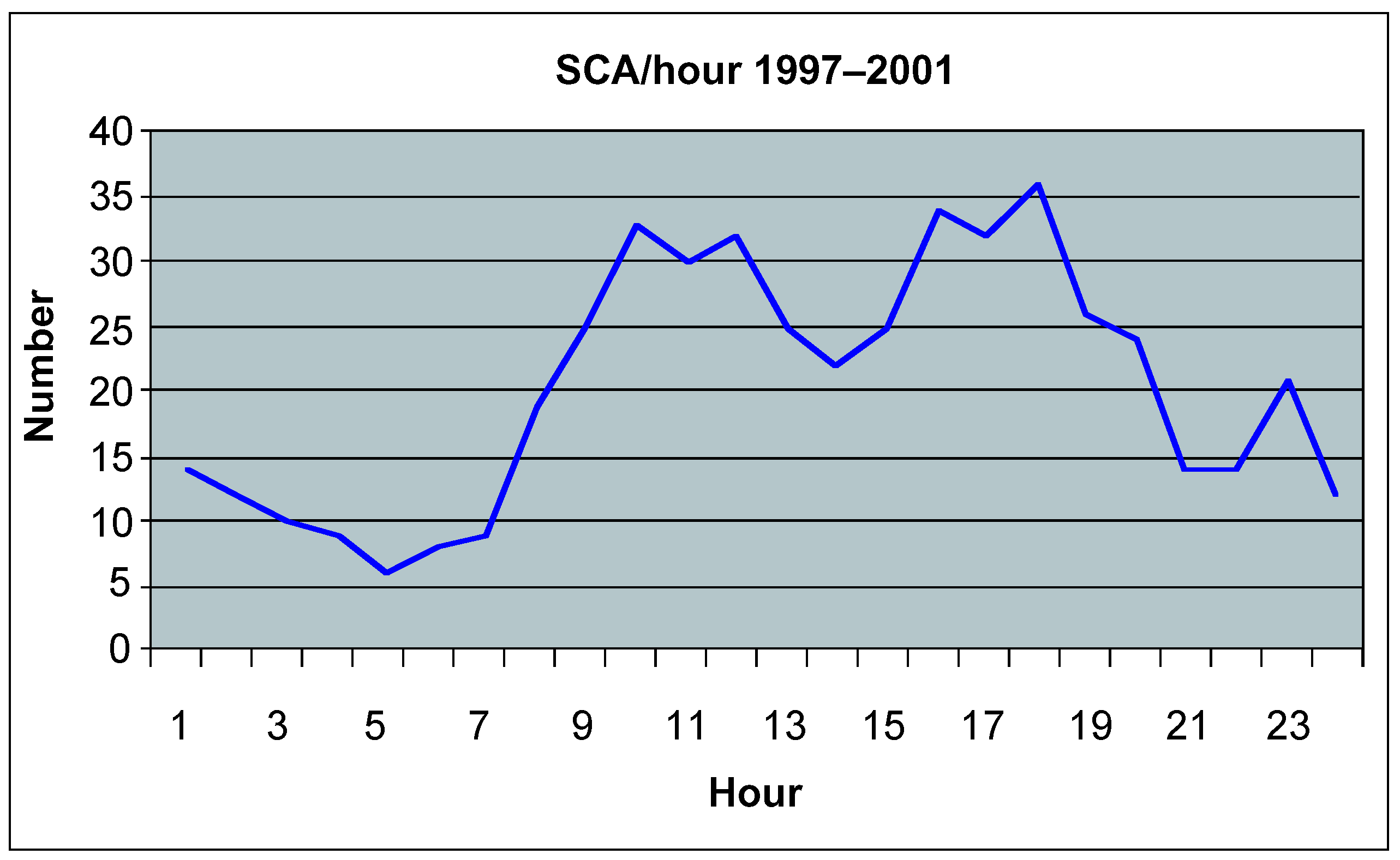
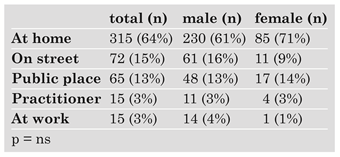
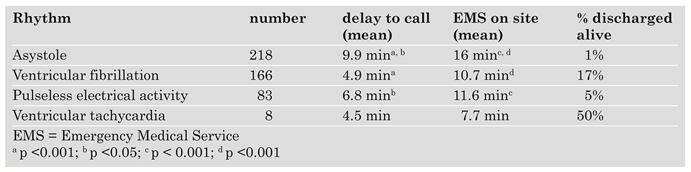
Distribution of the events
Clinical characteristics of survivors
Discussion
Conflicts of Interest
References
- Huikuri, H.V.; Castellanos, A.; Myerburg, R.J. Sudden death due to cardiac arrhythmias. N. Engl. J. Med. 2001, 345, 1473–1482. [Google Scholar] [CrossRef] [PubMed]
- Ganz, L. Primary prevention of sudden cardiac death. Curr. Cardiol. Rep. 2004, 6, 339–347. [Google Scholar] [CrossRef]
- Myerburg, R.J.; Castellanos, A. Emerging paradigms of the epidemiology and demographics of sudden cardiac arrest. Heart Rhythm. 2006, 3, 235–239. [Google Scholar] [CrossRef]
- De Torrente, A.; Scheidegger, D.; Von Planta, M.; Stauffer, J.C.; Jeker, K. Réanimation cardio-pulmonaire en Suisse: Le temps d’agir! Schweiz. Med. Wochenschr. 1990, 120, 1546–1548. [Google Scholar]
- Schoenenberger, R.A.; von Planta, M.; von Planta, I. Survival after failed-out-of-hospital resuscitation. Are further therapeutic efforts in the emergency department futile? Arch. Intern. Med. 1994, 154, 2433–2437. [Google Scholar] [CrossRef]
- Schoenenberger, R.; Sturmer, T.; von Panta, I.; von Planta, M. Prähospitale Reanimation in städtischen Verhältnissen – Ergebnisse und prognostische Entscheidungskriterien. Schweiz. Med. Wochenschr. 1995, 125, 573–580. [Google Scholar]
- Cummins, R.O.; Chamberlain, D.A.; Abramson, N.S.; Allen, M.; Baskett, P.J.; Becker, L.; et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: The utstein style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 1991, 84, 960–975. [Google Scholar] [CrossRef] [PubMed]
- Idris, A.H.; Becker, L.B.; Ornato, J.P.; Hedges, J.R.; Bircher, N.G.; Chandra, N.C.; et al. Utstein-Style guidelines for uniform reporting of Laboratory CPR Research: A Statement for Healthcare Professionals From a Task Force of the American Heart Association, the American College of Emergency Physicians, the American College of Cardiology, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, the Institute of Critical Care Medicine, the Safar Center for Resuscitation Research, and the Society for Academic Emergency Medicine. Circulation 1996, 94, 2324–2336. [Google Scholar]
- de Vreede-Swagemakers, J.J.M.; Gorgels, A.P.M.; Dubois-Arbouw, W.I.; van Ree, J.W.; Daemen, M.J.A.P.; Houben, L.G.E.; etal., *!!! REPLACE !!!*. Out-ofhospital cardiac arrest in the 1990s: A population-based study in the Maastricht area on incidence, characteristics and survival. J. Am. Coll. Cardiol. 1997, 30, 1500–1505. [Google Scholar] [CrossRef] [PubMed]
- de Vreede-Swagemakers, J.J.M.; Gorgels, A.P.M.; DuboisArbouw, W.I.; Dalstra, J.; Daemen, M.J.A.P.; van Ree, J.W.; etal., *!!! REPLACE !!!*. Circumstances and causes of out-of-hospital cardiac arrest in sudden death survivors. Heart 1998, 79, 356–361. [Google Scholar] [CrossRef]
- Priori, S.G.; Aliot, E.; Blomstrom-Lundqvist, C.; Bossaert, L.; Breithardt, G.; Brugada, P.; et al. Task Force on sudden cardiac death of the European Society of Cardiology. Eur. Heart J. 2001, 16, 1374–1450. [Google Scholar] [CrossRef]
- Engdahl, J.; Holmberg, M.; Karlson, B.W.; Luepker, R.; Herlitz, J. The epidemiology of out-of-hospital “sudden” cardiac arrest. Resuscitation 2002, 52, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Norris RM, on behalf of the UK Heart Attack Study (UKHAS) Collaborative Group. Circumstances of out of hospital cardiac arrest in patients with ischaemic heart disease. Heart 2005, 91, 1537–1540. [Google Scholar] [CrossRef] [PubMed]
- Elliott, W.J. Cyclic and circadian variations in cardiovascular events. Am. J. Hypertens. 2001, 14, S291–5. [Google Scholar] [CrossRef]
- Witte, D.R.; Grobbee, D.E.; Bots, M.L.; Hoes, A.W. A meta-analysis of excess cardiac mortality on monday. Eur. J. Epidemiol. 2005, 20, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Straus, S.M.J.M.; Bleumink, G.S.; Dieleman, J.P.; van der Lei, J.; Stricker, B.H.C.; Sturkenboom, M.C.J.M. The incidence of sudden cardiac death in the general population. J. Clin. Epidemiol. 2004, 57, 98–102. [Google Scholar] [CrossRef]
- Herlitz, J.; Castren, M.; Friberg, H.; Nolan, J.; Skrifvars, M.; Sunde, K.; et al. Post resuscitation care. What are the therapeutic alternatives and what do we know? Resuscitation 2006, 69, 15–22. [Google Scholar] [CrossRef]
- Roine, R.O.; Kajaste, S.; Kaste, M. Neuropsychological sequelae of cardiac arrest. JAMA 1993, 269, 237–242. [Google Scholar] [CrossRef]
- Bunch, T.J.; Hammill, S.C.; White, R.D. Outcomes after ventricular fibrillation out-of-hospital cardiac arrest: Expanding the chain of survival. Mayo Clin. Proc. 2005, 80, 774–782. [Google Scholar] [CrossRef]
- Saner, H.; Borner Rodriguez, E.; Kummer-Bangerter, A.; Schüppel, R.; von Planta, M. Quality of life in long-term survivors of out-of-hospital cardiac arrest. Resuscitation 2002, 53, 7–13. [Google Scholar] [CrossRef]
- Zipes, D.P.; Wellens, H.J.J. Sudden cardiac death. Circulation 1998, 98, 2334–2351. [Google Scholar] [CrossRef] [PubMed]
- Wellens, H.J.J.; Gorgels, A.P.; de Munter, H. Sudden death in the community. J. Cardiovasc. Electrophysiol. 2003, 14, S104–7. [Google Scholar] [CrossRef] [PubMed]
- Myerburg, R.J.; Velez, M.; Rosenberg, D.G.; Fenster, J.; Castellanos, A. Automatic external defibrillators for prevention of out-of-hospital sudden death: Effectiveness of the automatic external defibrillator. J. Cardiovasc. Electrophysiol. 2003, 14, S108–116. [Google Scholar] [CrossRef]
- Müller, D.; Agrawal, R.; Arntz, H.R. How sudden is sudden cardiac death? Circulation. 2006, 114, 1146–1150. [Google Scholar] [CrossRef]
- Capucci, A.; Aschieri, D.; Piepoli, M.F.; Bardy, G.H.; Iconomu, E.; Arvedi, M. Tripling survival from sudden cardiac arrest via early defibrillation without traditional education in cardiopulmonary resuscitation. Circulation 2002, 106, 1065–1070. [Google Scholar] [CrossRef] [PubMed]

 |
 |
 |
© 2008 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Praz, L.; Fishman, D.; Yersin, B.; Moeschler, O.; Schläpfer, J. Sudden Cardiac Arrest in the Region of Lausanne: A 5 years Consecutive Observational Study. Cardiovasc. Med. 2008, 11, 55. https://doi.org/10.4414/cvm.2008.01303
Praz L, Fishman D, Yersin B, Moeschler O, Schläpfer J. Sudden Cardiac Arrest in the Region of Lausanne: A 5 years Consecutive Observational Study. Cardiovascular Medicine. 2008; 11(2):55. https://doi.org/10.4414/cvm.2008.01303
Chicago/Turabian StylePraz, Laurent, Daniel Fishman, Bertrand Yersin, Olivier Moeschler, and Jürg Schläpfer. 2008. "Sudden Cardiac Arrest in the Region of Lausanne: A 5 years Consecutive Observational Study" Cardiovascular Medicine 11, no. 2: 55. https://doi.org/10.4414/cvm.2008.01303
APA StylePraz, L., Fishman, D., Yersin, B., Moeschler, O., & Schläpfer, J. (2008). Sudden Cardiac Arrest in the Region of Lausanne: A 5 years Consecutive Observational Study. Cardiovascular Medicine, 11(2), 55. https://doi.org/10.4414/cvm.2008.01303




