Introduction
Cardiovascular disease is the most frequent cause of death in Switzerland [
1]. Currently, data on acute myocardial infarction (AMI) are available from a local registry on AMI [
2] and from the Federal Statistical Office’s (FSO) hospital statistics database (HOST) [
3]. Additionally, data on death caused by AMI are available from the FSO`s Cause of Death Statistics (CoD) [
4]. The HOST database keeps a record of all data on hospital discharges of AMI patients. Yet, HOST does not contain a complete set of data on AMI incidence in Switzerland. For its part, the CoD database does not provide information on case fatality nor does it differentiate between in- and out-of hospital deaths. The aim of this study was to estimate AMI incidence for Switzerland by combining data from the HOST and CoD databases. In addition, we aimed at estimating case fatality for both in-hospital and out-of-hospital deaths.
Methodology
The most recent data were taken from the FSO’s HOST and CoD databases (2004) [
3,
4]. Data were coded according to the International Classification of Disease (ICD) version 10. For HOST, data were coded in the hospitals where patients were discharged from, and then these codes were transferred to the HOST database. In 2004, hospital response rate was 100%.
In Switzerland all deaths are included in the CoD database. The number of deaths is based on data from the civil registry office where deaths are usually announced by family members of the deceased. The civil registry office obtains information on cause of death from the physician who verified the death. Based on this information, the primary cause of death is then coded by the FSO.
For data analysis, we used age groups as applied by the data provider (FSO) in standard morbidity and mortality tables on AMI, and as recommended by EUROCISS [
5]. In order to calculate rates, the 2004 data from the Swiss Census database were used [
6]. Age standardisation was calculated according to the European standard population [
7]. In order to prepare the data that would be used to estimate AMI incidence, and case fatality for both in- and out-of-hospital deaths due to AMI, we applied the following procedure (for definitions see
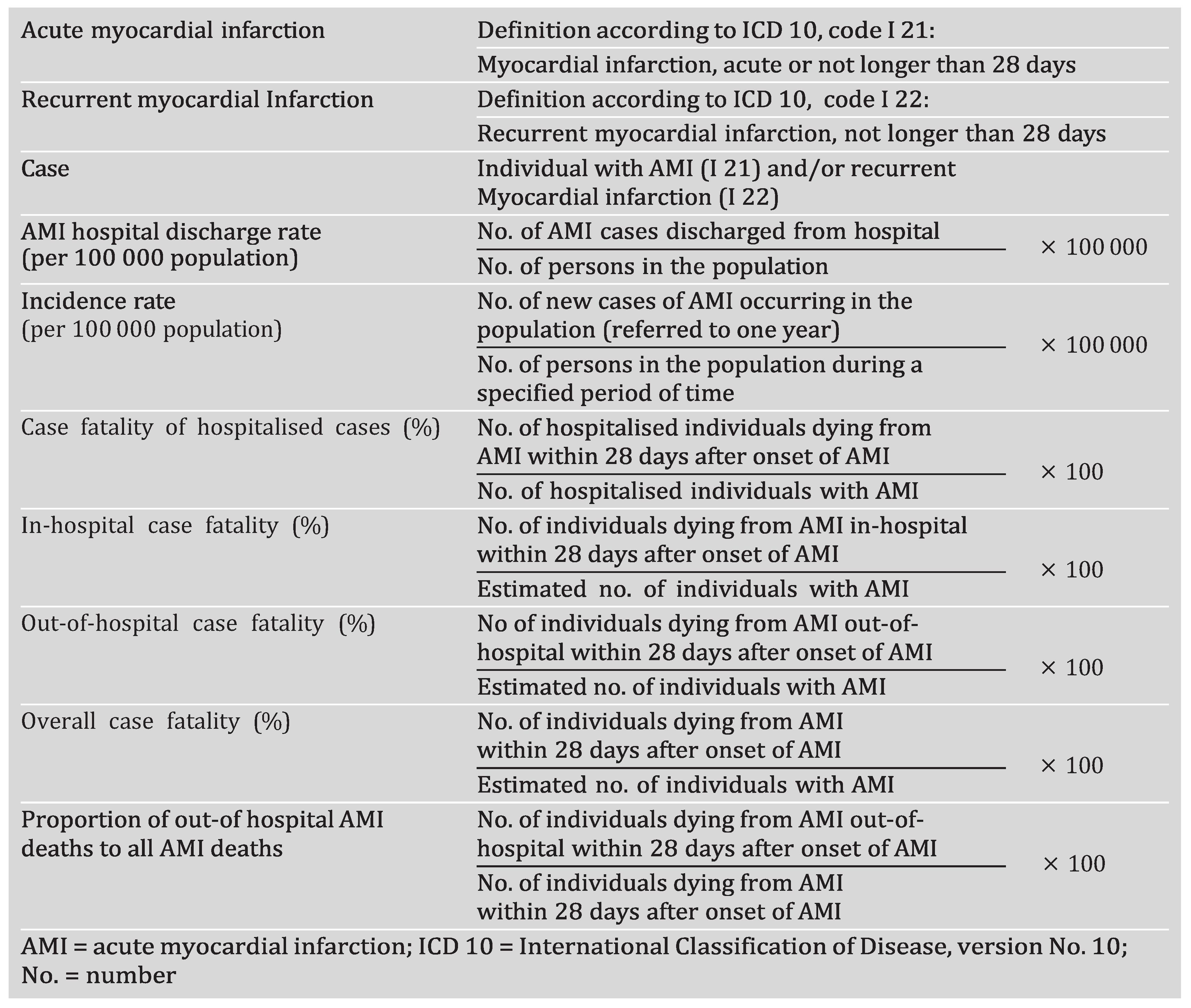
Table 1):
- -
From the HOST database, we selected all AMI cases (I 21 and I 22) documented in one of the first five diagnosis areas (cases A). If a patient was admitted to a district hospital (eg Regional Hospital) following an acute event and later transferred to a major hospital (ie University Hospital, Cantonal Hospital or Heart Centre), we used a connection code to identify a patient as being the same patient in the HOST database and thus counted him/her only once.
- -
In addition, from the HOST database, we extracted data on all AMI cases having a discharge code of 5, which meant that the AMI patient had died while in the hospital (cases Ad). For the calculation procedure, the remaining cases were called in-hospital survivors.
- -
From CoD, we identified all cases that died from AMI within 28 days after the onset of myocardial infarction (cases B).
Individuals who were discharged alive from hospital after AMI and died later within the same year were not considered as AMI cases in CoD but were coded as death from “chronic ischaemic heart disease” (according to I 25.2 and I 25.8) (
Table 1).
Calculation procedure
Using a prepared data set (see above) both AMI incidence and case fatality was determined by the following procedures (for definitions and procedure in brief see
Table 1):
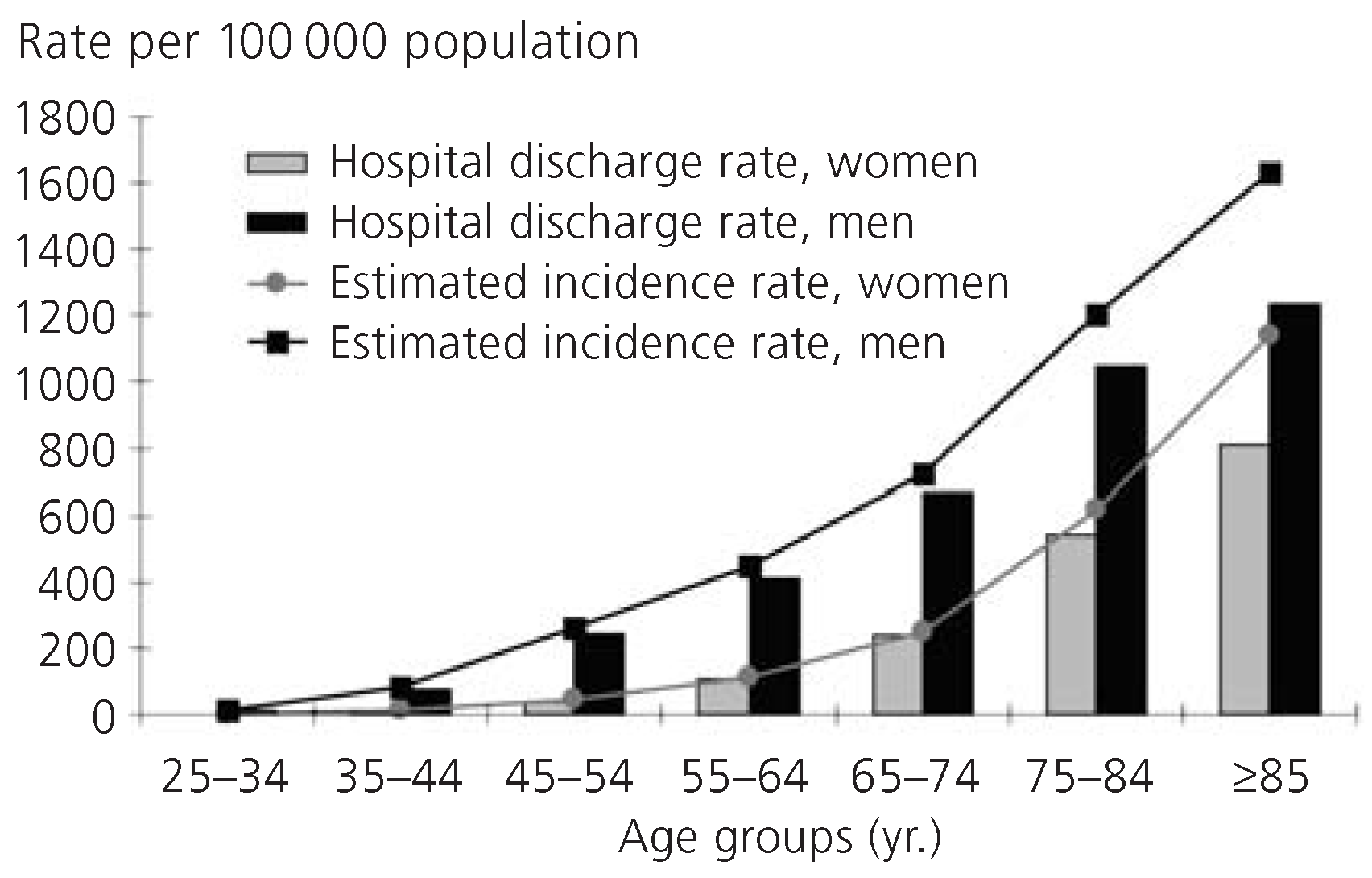
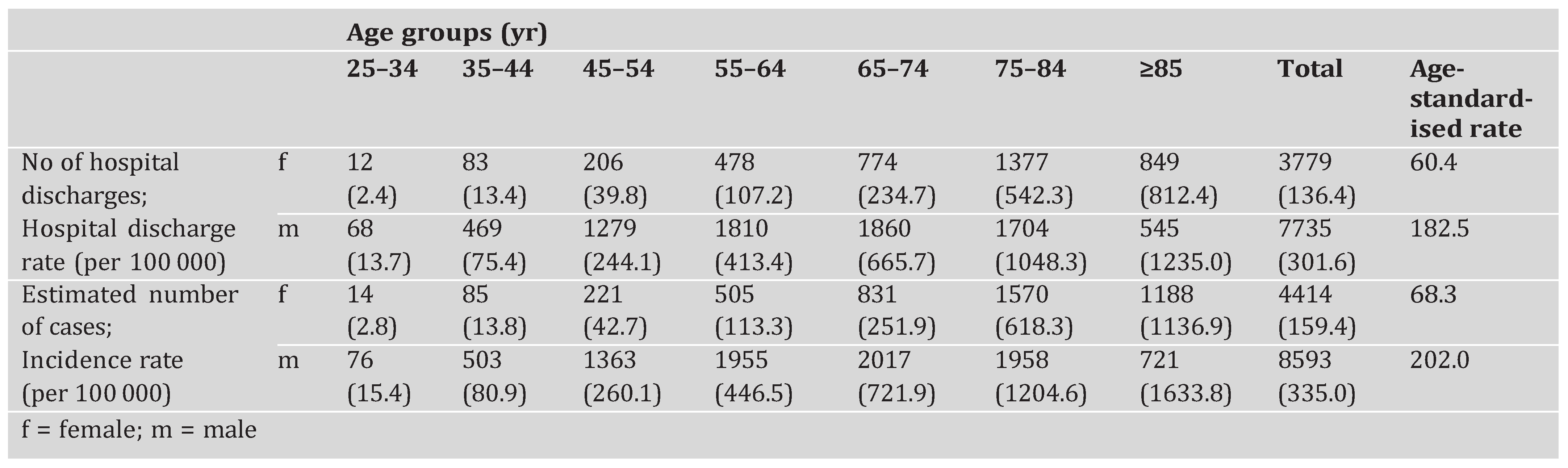
We first determined gender and age-specific rate for AMI patients discharged from the hospital (alive or dead) per 100,000 inhabitants ([cases A / population] × 100,000 = AMI discharge rate).
We then estimated AMI incidence rate as follows: total number of in-hospital survivors (calculated by data from the HOST database) plus the total number of AMI deaths (CoD database), divided by gender and age-specific population per 100,000 ([cases A − cases Ad + cases B] / population × 100,000 = AMI incidence rate).
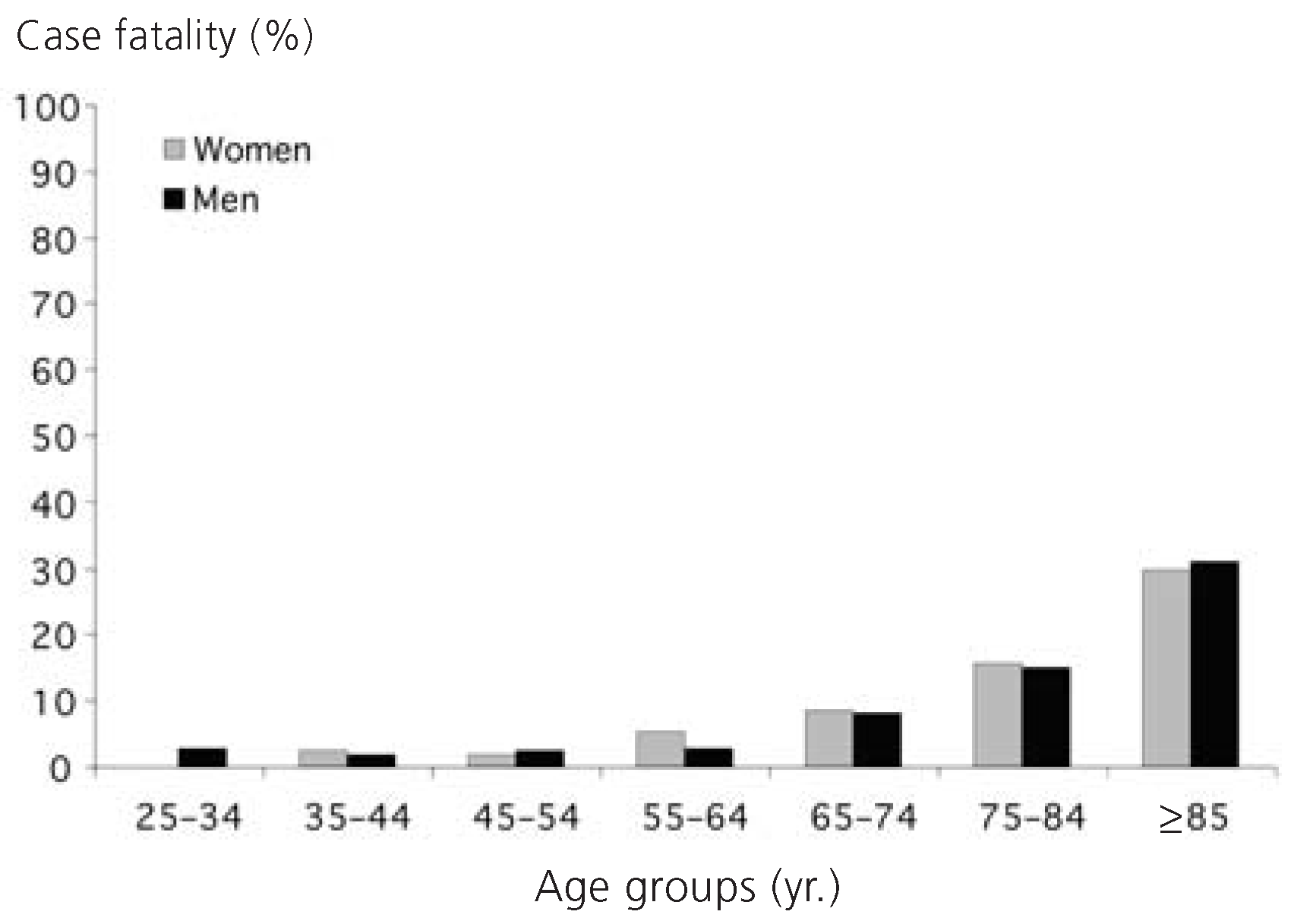
The case fatality of hospitalised patients was calculated as follows: total number of AMI patients who died from AMI while in the hospital (cases Ad) divided by the total number of AMI patients discharged from the hospital (cases A) (cases Ad / cases A × 100 = 28-day case fatality of hospitalised cases).
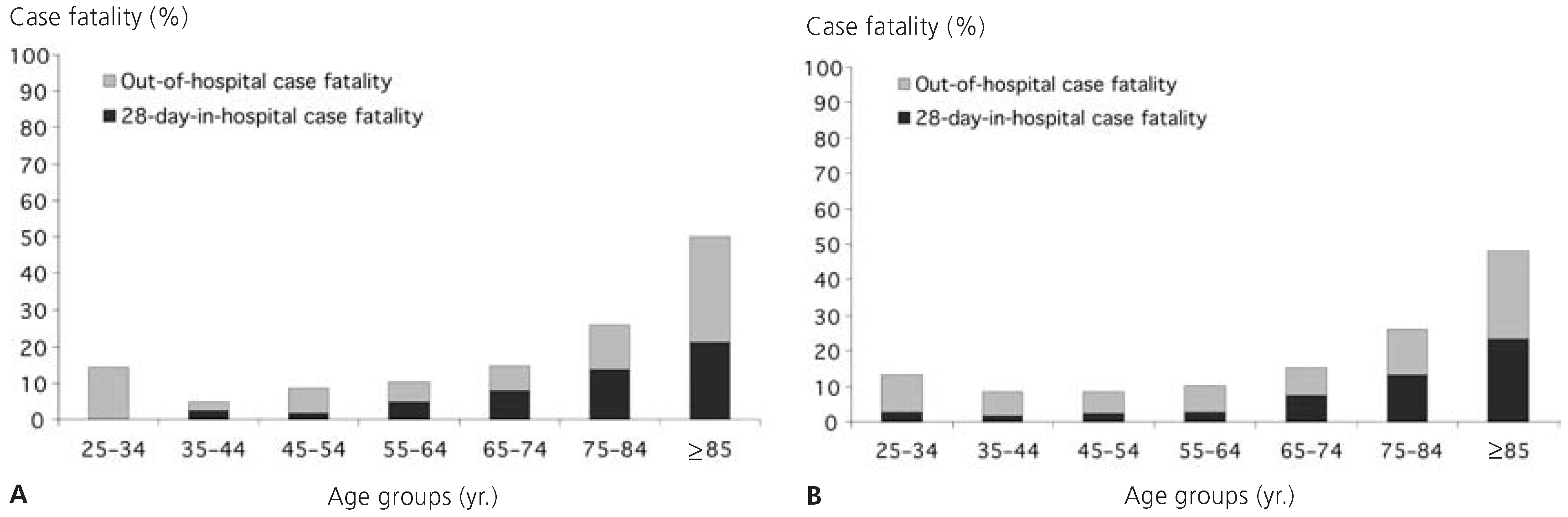
We then calculated the in-hospital case fatality: total number of patients who died due to AMI inside the hospital divided by the total number of estimated AMI events (cases Ad / estimated AMI events × 100 = in-hospital case fatality).
Out-of-hospital case fatality was calculated as follows: total number of deaths due to AMI reported in the CoD database minus total number in-hospital deaths due to AMI reported in the HOST database divided by the total number of estimated AMI events ([cases B − cases Ad] / estimated AMI events × 100 = out-of hospital case fatality).
The overall case fatality was calculated by dividing total of deaths reported in CoD database by the total number of estimated AMI events (cases B / estimated AMI events × 100,000 = overall case fatality).
The proportion of out-of-hospital AMI deaths to the total number of AMI deaths was calculated as follows: total number of deaths due to AMI reported in the CoD database minus the total number of in-hospital AMI deaths reported in the HOST database, divided by the total number of AMI deaths reported in the CoD database ([cases B − cases Ad] / cases B × 100 = Proportion of out-of-hospital AMI deaths to all AMI deaths).
Discussion
To our knowledge, this was the first estimation of AMI incidence for Switzerland based on both the HOST and CoD database. We found that the estimated AMI incidence rate exceeded the number of cases discharged from hospital with AMI as reported by HOST database indicating that the estimated AMI incidence rate is closer to the actual AMI incidence rate. Out-of-hospital AMI deaths accounted for 65% on average of total AMI deaths. Compared 2004, data on hospital discharge rates and estimated incidence rates of the years 2001 to 2003 showed marginal differences (
Figure 4).
In order to estimate AMI incidence rate, we needed to identify all patients who were discharged from the hospital alive as well as those who died from AMI either inside or outside the hospital. Nevertheless, there are still cases that are clearly not reported in the HOST or CoD databases. For example, these could be patients suffering from a silent myocardial infarction, and/or exhibiting a false-negative diagnosis of AMI. It has been reported that around 20% of all AMI patients experience silent AMI or acute myocardial infarction with atypical symptoms [
8,
9]. Because non-fatal myocardial infarction occurring out of hospital was registered neither in HOST nor CoD database, a further underestimation of AMI incidence could be assumed. Moreover, death certificates do not always indicate AMI as the respective cause of death: in the case of sudden death, for example, where not enough time is available for use of diagnostic tools to justify diagnosis of AMI. Other potential causes of death in which AMI is supposedly the cause of death such as malign rhythm disorders or pulmonary embolism often remain unidentified. For cases where the cause of death is uncertain, there is no obligation to perform an autopsy in Switzerland. This may confound the estimated AMI incidence and case fatality.
In our study, coding of AMI deaths was based on a clinical diagnosis which does mean definite AMI. Contrary, an epidemiological definition could comprise not only definitive clinical diagnosis of AMI but also possible AMI or coronary death and thus, result in different findings. In the German MONICA project, for example, overall 28-day case fatality of hospitalised patients was 28% when an epidemiological definition for AMI and/or AMI death was applied using the diagnostic criteria “definite AMI” and “possible AMI” or “coronary death”. However, if AMI cases were diagnosed on the basis of a clinical definition alone (definite AMI), 28-day case fatality dropped to 13.5% [
10]. According to our calculation procedure, an average of 65% of deaths due to AMI occurred outside of the hospital. A similar prevalence for out-of-hospital AMI deaths has been reported by Löwel et al. [
11]: About two thirds of deaths due to definite AMI and/or possible coronary deaths occurred before patients reached the hospital. Kalusche et al. [
12] stated that two-thirds of the pre-hospital deaths occurred within the first hour after onset of symptoms leading up to an AMI.
Because it was not possible to validate HOST and CoD data with data from the patients’ medical history and/or autopsy findings in our study, clinical definition of AMI may result in missing AMI data and very early deaths due to AMI. Therefore, estimated AMI incidence rate and/or case fatality determined for Switzerland hold an underestimation compared to a calculation procedure based on a broader definition of AMI.
Comparison of the estimated AMI incidence and case fatality in Switzerland with morbidity data from other European countries is problematic because of use of different data sources (
eg hospital discharge records, surveys, and registries; application of different coding practices) and lack of harmonised data (
eg use of different AMI definitions; different standardisation of morbidity rates) [
5].
In conclusion, our analysis provided a closer estimate of AMI incidence rate and case fatality of hospitalised patients in Switzerland than known from HOST taken as a single database. Nevertheless, because of methodological limitations, an uncertain number of AMI cases and cases of very early deaths due to AMI remain unrecorded. Therefore, the estimated AMI incidence rate as demonstrated still does not represent the actual AMI incidence rate for Switzerland. In order to obtain the actual overall AMI incidence rate, personal identification numbers would have to be used to link the data in the HOST database with the data in the CoD database as was successfully performed in Sweden [
13]. As an alternative, a probabilistic record linkage method could be applied to combine both HOST and CoD databases by using date of birth, sex and zip code [
13]. Due to lack of identification numbers in the FSO’s CoD database and because of strong data protection restrictions, it was not possible to link data from the HOST and CoD databases. Yet, to get more comprehensive data on AMI incidence rate, it is important for AMI diagnosis to be based on a broader definition than a clinical one.