Bridging Financial Inclusion and Health Equity in LMICs: Evidence from a Half-Century of Bibliometric Data
Highlights
- This research addresses the critical, yet understudied, link between financial inclusion and health equity, directly supporting the objectives of SDG 3 (Good Health and Well-being) and SDG 10 (Reduced Inequalities).
- It highlights how limited financial inclusion exacerbates health inequalities, particularly in low- and middle-income countries (LMICs), by restricting access to necessary care and increasing the burden of out-of-pocket healthcare spending.
- This is the first bibliometric analysis of this scope to examine eighty years of research at the intersection of financial inclusion and health equity, revealing a major gap where fewer than 0.3% of the extant literature has explored this area.
- The study establishes a foundational body of evidence and proposes a research agenda to guide future interdisciplinary work on utilizing financial instruments to promote equitable health outcomes.
- Policymakers and health professionals should integrate financial inclusion strategies—such as digital finance, microinsurance, and mobile money—into broader health equity frameworks.
- Researchers are encouraged to adopt interdisciplinary approaches and develop common metrics that correlate financial inclusion indicators directly with health equity outcomes.
Abstract
1. Introduction
2. Materials and Methods
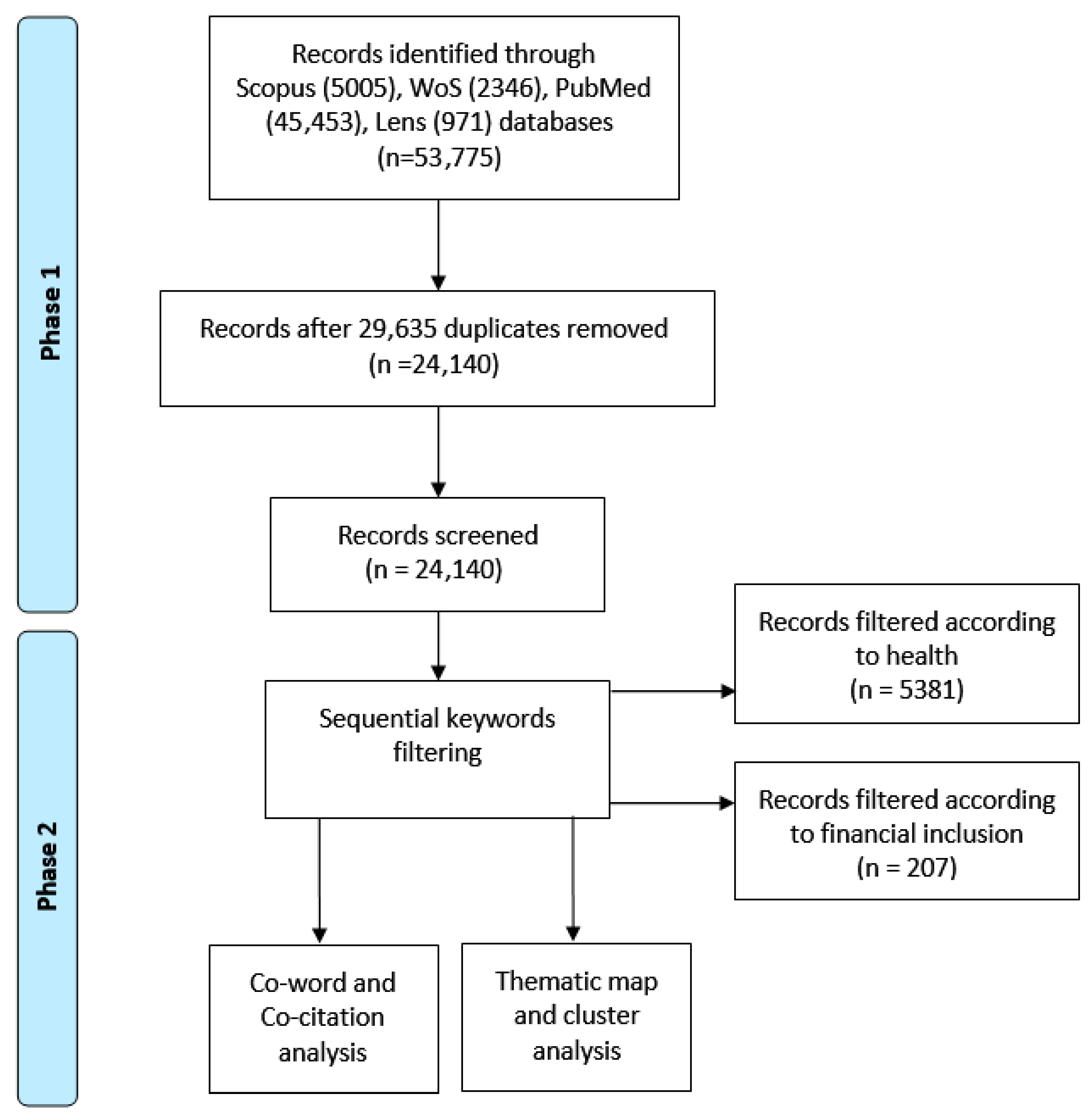
2.1. Search Strategy and Data Collection
2.2. Screening and Refinement for Thematic Analysis
- Title/Abstract Screening: Two reviewers independently screened titles and abstracts against the inclusion criterion: the study had to discuss a financial inclusion mechanism (e.g., savings, credit, insurance, digital payment) in relation to a health outcome, behavior, or access issue.
- Full-Text Eligibility Assessment: The full texts of the 24,140 records were assessed. Studies were excluded if they (i) addressed financial access but without a clear link to health; (ii) discussed health disparities without a financial inclusion dimension; (iii) were non-empirical commentaries/editorials. From an initial pool of 24,140 articles, a sequential keyword filtration was applied. Filtering for ‘financial inclusion’ yielded 207 articles. A subsequent filter for ‘health’ within the initial subset yielded 5381 articles. To identify the most impactful works at the intersection for qualitative synthesis, the ten articles from this final set with the highest citation counts (n = 10) were isolated. This stringent filtering process—from 24,140 to a core intersection of 5381 articles—quantitatively underscores the paper’s central finding: the Financial Inclusion-Health Equity (FI-HE) nexus is profoundly under-studied, with most literature treating the domains in isolation.
2.3. Bibliometric Analysis Framework
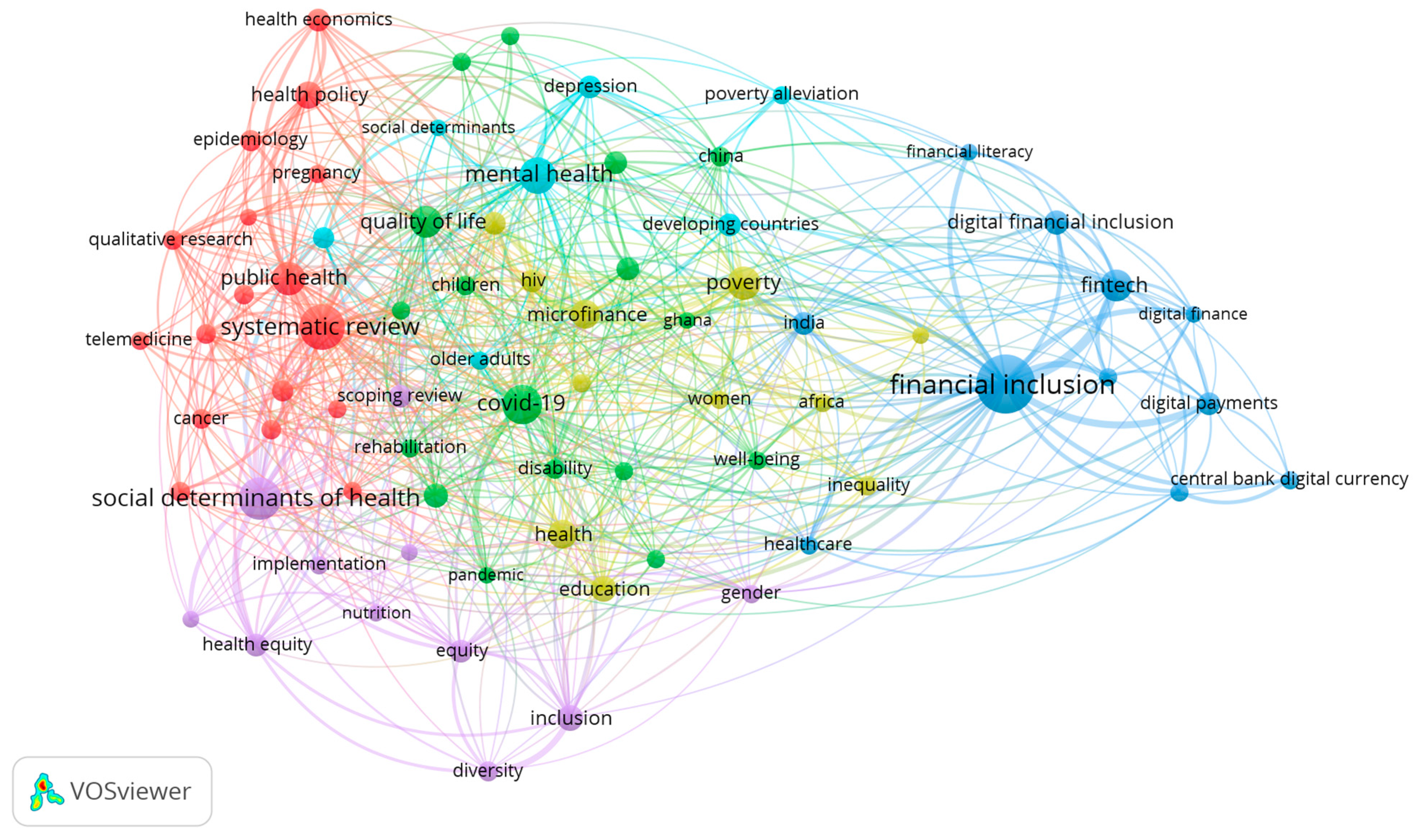
- Co-word Analysis: A network using both Author Keywords and KeyWords Plus as units of analysis was constructed. A minimum occurrence threshold was applied to ensure meaningful connections. The resulting network was visualized and thematically clustered using VOSviewer’s LinLog/modularity normalization method.
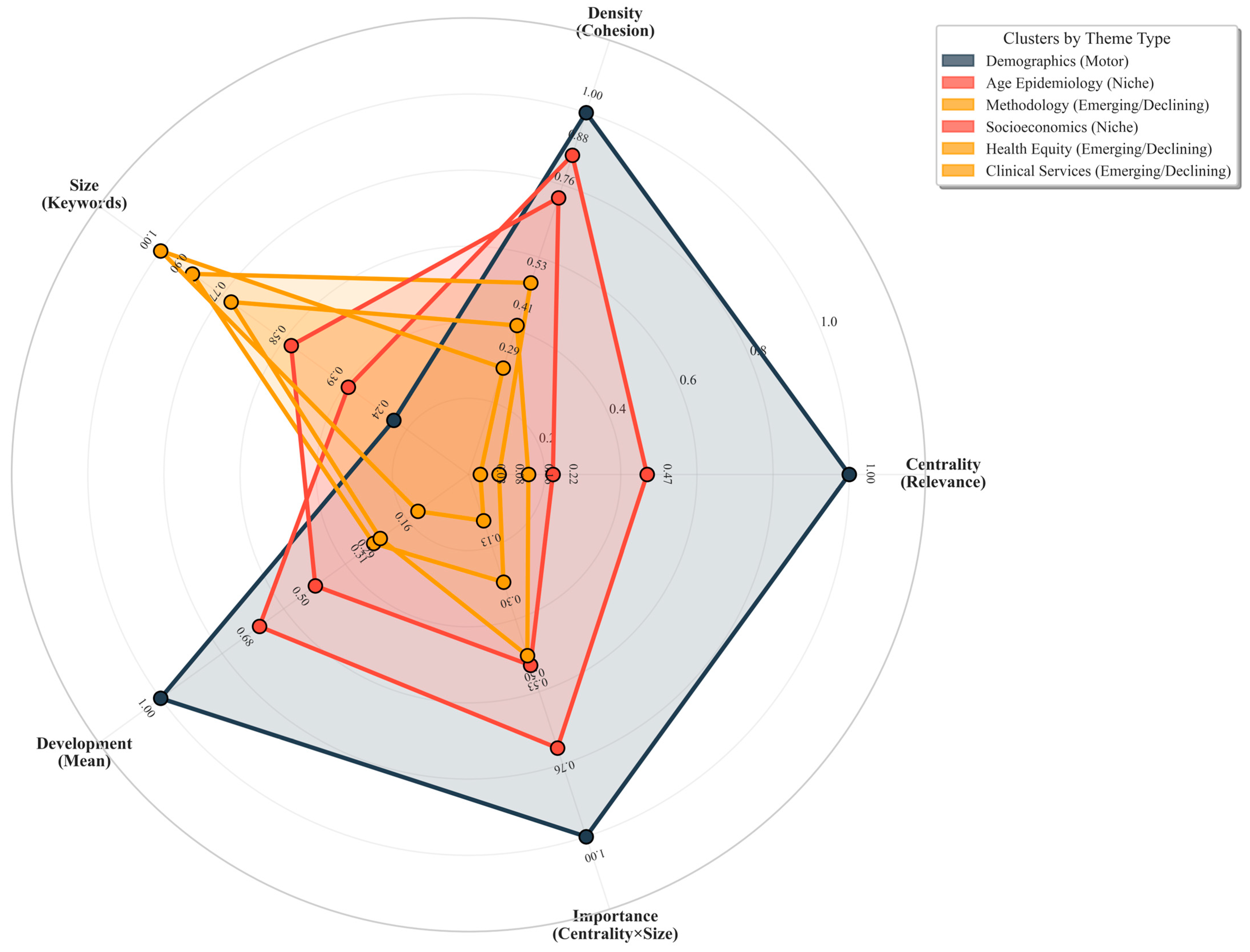
- Thematic Map Analysis: Based on the co-word network clusters, themes were categorized into four types—motor, niche, emerging, and basic—according to their centrality (relevance to the broader field) and density (internal development) metrics.
3. Results
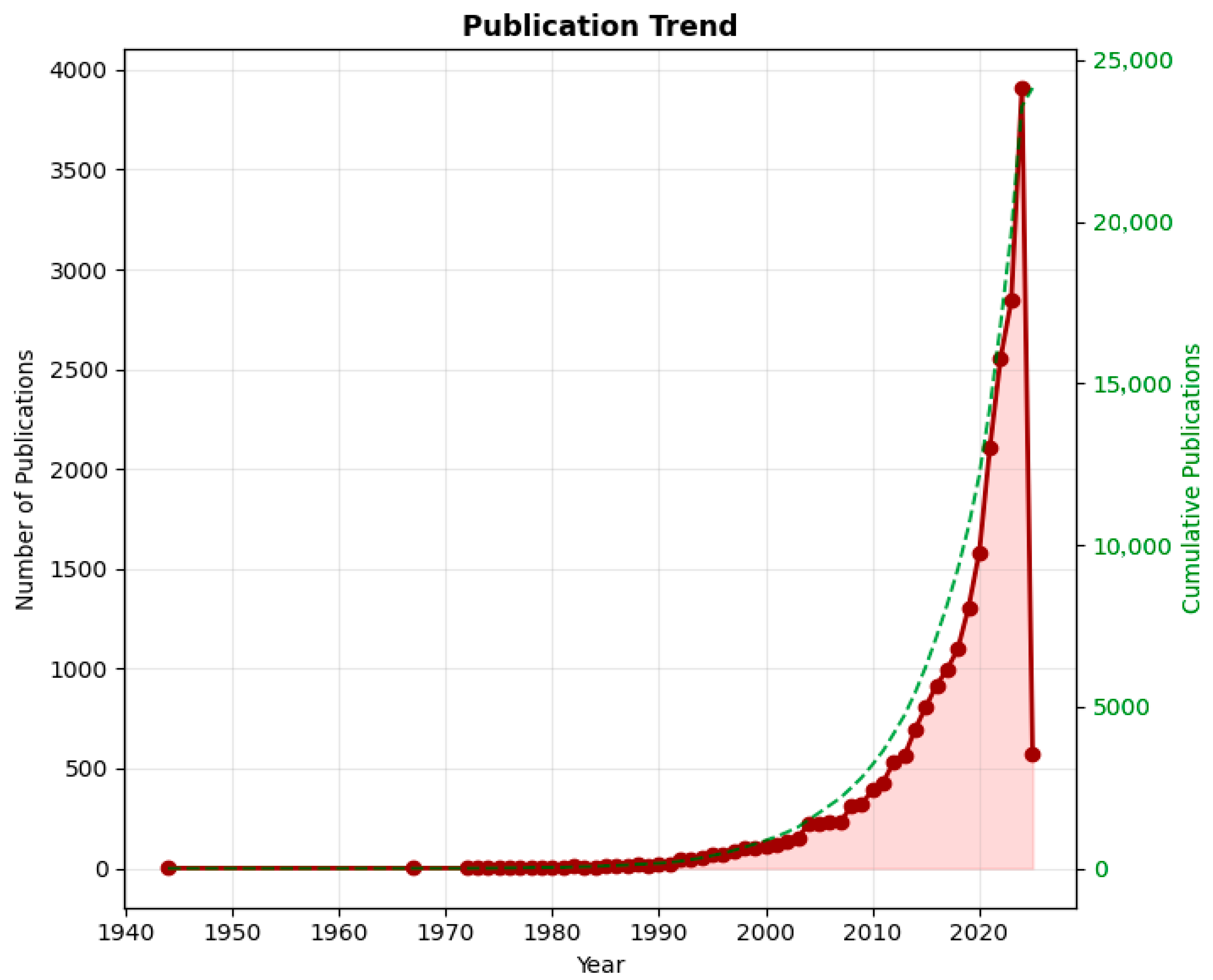
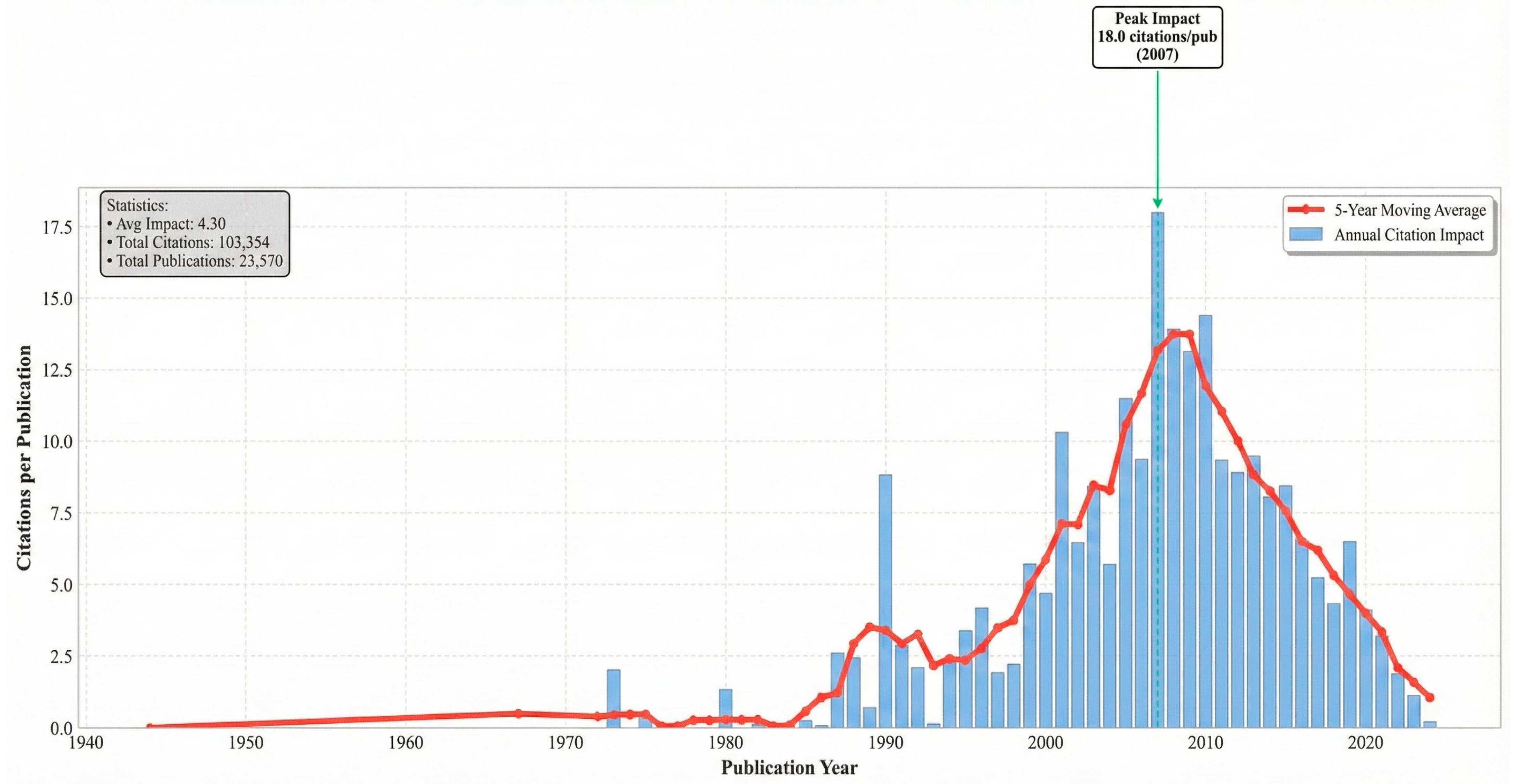
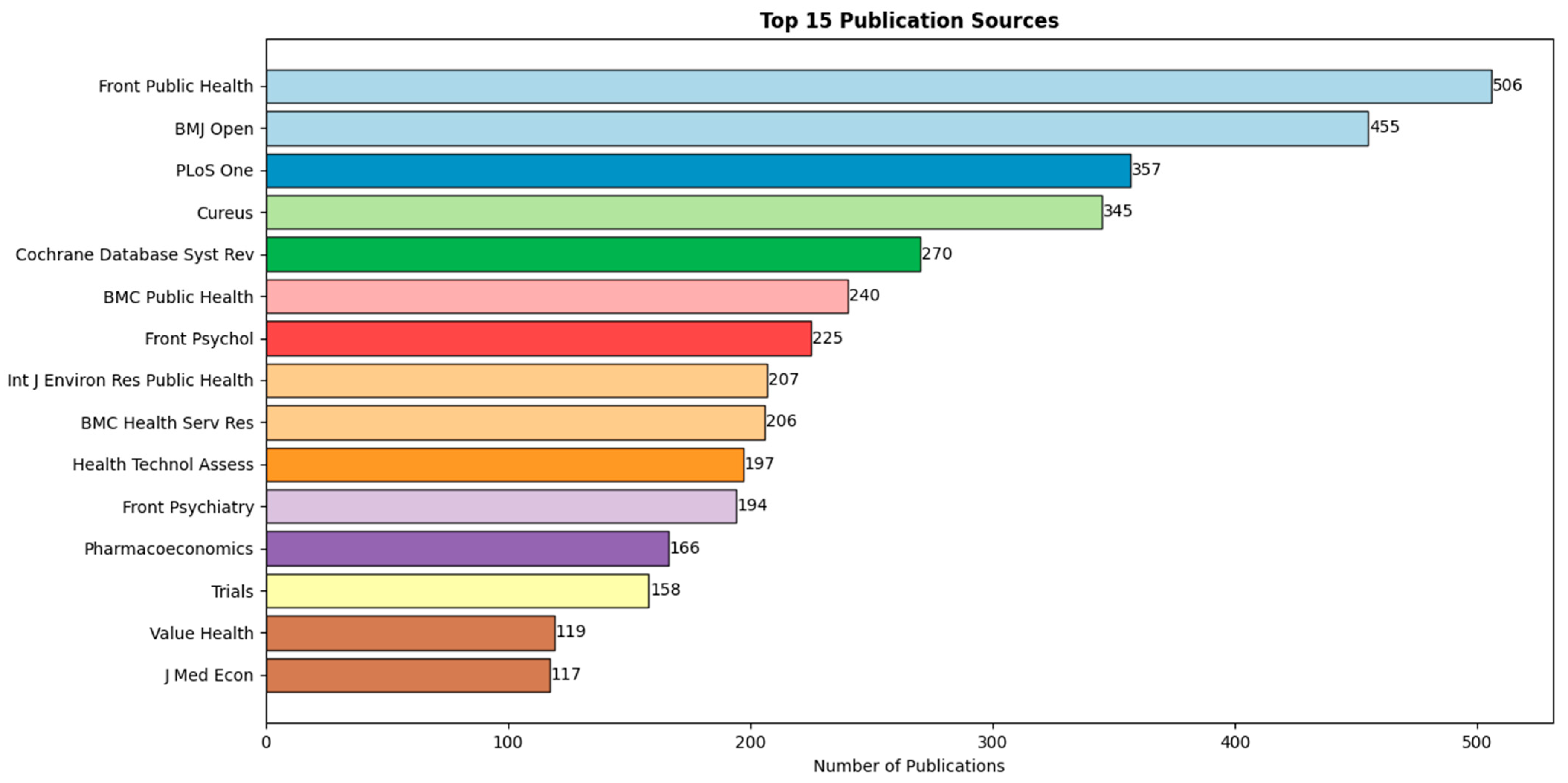
3.1. Research Landscape (Addressing RQ1)
3.2. Conceptual Structure (Addressing RQ2 & RQ3)
4. Discussion
4.1. Methodological Considerations
4.2. Key Findings and Interpretation
4.3. The Equity Blind Spot
4.4. A Path Forward
- Interdisciplinary research should move beyond descriptive mapping to clarify the causal pathways through which specific financial instruments affect equity metrics. This requires adopting robust experimental and quasi-experimental methods from development economics [89] within equity-focused evaluation frameworks [90]. For example, studies could investigate how microinsurance uptake influences health-seeking behavior for chronic diseases among rural women or how digital savings platforms affect maternal health outcomes in urban informal settlements.
- Research must examine how fintech innovations can be intentionally harnessed within equitable health financing architectures. This involves learning from integrated systems like Kenya’s mobile money infrastructure to design ‘health-smart’ financial products [90] and India’s Aadhaar-linked welfare and health schemes [91]. Research should also investigate how financial resources are strategically allocated within health systems to improve equity [92,93], ensuring that digital tools do not exacerbate existing disparities in access.
- Policy-Relevant Research and Monitoring should develop integrated monitoring frameworks that explicitly link financial inclusion indicators—such as those from the Global Findex [9]—with health equity outcomes, building on established tools like WHO’s health inequality monitoring framework [94]. This requires embracing insights from economics on evaluating trade-offs and policy options in public health [95] to provide policymakers with actionable evidence on which financial inclusion levers most effectively reduce disparities in healthcare access, financial risk protection, and health status for disadvantaged populations in LMICs.
4.5. Emerging Research Avenues
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2020. Available online: https://www.who.int/health-topics/social-determinants-of-health (accessed on 1 December 2024).
- Shrivastava, S.R.; Shrivastava, P.S.; Ramasamy, J. Moving Toward the Universal Health Coverage: A Strategy to Expedite Health Equity. J. Med. Soc. 2016, 30, 70–71. [Google Scholar] [CrossRef]
- Sadare, O.; Williams, M.; Simon, L. Implementation of the Health Equity Impact Assessment (HEIA) Tool in a Local Public Health Setting: Challenges, Facilitators, and Impacts. Can. J. Public Health 2020, 111, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Muinde, J.V.S.; Prince, R.J. A New Universalism? Universal Health Coverage and Debates about Rights, Solidarity and Inequality in Kenya. Soc. Sci. Med. 2023, 319, 115258. [Google Scholar] [CrossRef]
- Shady, K.; Phillips, S.; Newman, S. Barriers and Facilitators to Healthcare Access in Adults with Intellectual and Developmental Disorders and Communication Difficulties: An Integrative Review. Rev. J. Autism Dev. Disord. 2024, 11, 39–51. [Google Scholar] [CrossRef]
- World Bank. Global Financial Development Report 2023; The World Bank: Washington, DC, USA, 2023. Available online: https://www.worldbank.org/en/publication/gfdr (accessed on 15 November 2024).
- Chitimira, H.; Warikandwa, T.V. Financial Inclusion as an Enabler of United Nations Sustainable Development Goals in the Twenty-First Century: An Introduction. In Financial Inclusion and Digital Transformation Regulatory Practices in Sub-Saharan Africa; Ius Gentium: Cham, Switzerland, 2023; pp. 1–22. [Google Scholar]
- Baheti, S.S.; Verma, D.; Amarnath, D.D. Understanding Evolution, Development, and Transitioning of Digital Financial Inclusion: A Bibliometric Study. In Transforming the Financial Landscape with ICTs; IGI Global: Hershey, PA, USA, 2024; pp. 76–93. [Google Scholar]
- Demirgüç-Kunt, A.; Klapper, L.; Singer, D.; Ansar, S. The Global Findex Database 2017: Measuring Financial Inclusion and the Fintech Revolution; The World Bank: Washington, DC, USA, 2018. [Google Scholar]
- Yao, J.S.; Kibu, O.D.; Asahngwa, C.; Ngo, N.V.; Ngwa, W.; Jasmin, H.M.; Tchoupa, A.M.; Nkem, M.P.; Nana, T.J.; Nji, M.A.M. A Scoping Review on the Availability and Utilization of Essential Opioid Analgesics in Sub-Saharan Africa. Am. J. Surg. 2023, 226, 409–421. [Google Scholar] [CrossRef]
- Bayked, E.M.; Toleha, H.N.; Kebede, S.Z.; Workneh, B.D.; Kahissay, M.H. The Impact of Community-Based Health Insurance on Universal Health Coverage in Ethiopia: A Systematic Review and Meta-Analysis. Glob. Health Action 2023, 16, 2189764. [Google Scholar] [CrossRef]
- Daliri, D.B.; Aninanya, G.A.; Laari, T.T.; Abagye, N.; Dei-Asamoa, R.; Afaya, A. Exploring the Barriers to Mental Health Service Utilization in the Bolgatanga Municipality: The Perspectives of Family Caregivers, Service Providers, and Mental Health Administrators. BMC Health Serv. Res. 2024, 24, 278. [Google Scholar] [CrossRef]
- Sule, F.A.; Uthman, O.A.; Olamijuwon, E.O.; Ichegbo, N.K.; Mgbachi, I.C.; Okusanya, B.; Ojo, T.; Gholbzouri, K.; Odukoya, O.O.; Adu, C. Examining Vulnerability and Resilience in Maternal, Newborn and Child Health through a Gender Lens in Low-Income and Middle-Income Countries: A Scoping Review. BMJ Glob. Health 2022, 7, e007426. [Google Scholar] [CrossRef] [PubMed]
- Oyekanmi, O. Digital Gender Inclusion and Women’s Economic Empowerment in Ethiopia and Nigeria. In African Women in the Fourth Industrial Revolution: Change, Policies, and Approaches; Muthuki, J., Mhlanga, D., Eds.; Springer: Cham, Switzerland, 2024; pp. 144–153. [Google Scholar]
- Khatib, M.E.; Hamidi, S.; Marqab, R.A. Digital Disruption and Big Data in Healthcare—Opportunities and Challenges. Clinicoecon. Outcomes Res. 2022, 14, 537–547. [Google Scholar] [CrossRef]
- Patel, V.; Saxena, S.; Lund, C.; Thornicroft, G.; Baingana, F.; Bolton, P.; Chisholm, D.; Collins, P.Y.; Cooper, J.L.; Eaton, J.; et al. The Lancet Commission on Global Mental Health and Sustainable Development. Lancet 2018, 392, 1553–1598. [Google Scholar] [CrossRef]
- Sen, A. Development as Freedom; Alfred A. Knopf: New York, NY, USA, 1999. [Google Scholar]
- World Health Organization. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008; Available online: https://www.who.int/publications/i/item/9789241563703 (accessed on 13 August 2024).
- Senyo, P.K.; Karanasios, S.; Agbloyor, K.E.; Choudrie, J. Government-Led Digital Transformation in FinTech Ecosystems. J. Strateg. Inf. Syst. 2024, 33, 101849. [Google Scholar] [CrossRef]
- Mongeon, P.; Paul-Hus, A. The Journal Coverage of Web of Science and Scopus: A Comparative Analysis. Scientometrics 2016, 106, 213–228. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L. Software Survey: VOSviewer, a Computer Program for Bibliometric Mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef] [PubMed]
- Costello, A.; Abbas, M.; Allen, A.; Ball, S.; Bell, S.; Bellamy, R.; Friel, S.; Groce, N.; Johnson, A.; Kett, M.; et al. Managing the Health Effects of Climate Change. Lancet 2009, 373, 1693–1733. [Google Scholar] [CrossRef]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The Operation of the Century: Total Hip Replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Zimlichman, E.; Henderson, D.; Tamir, O.; Franz, C.; Song, P.; Yamin, C.K.; Keohane, C.; Denham, C.R.; Bates, D.W. Health Care-Associated Infections: A Meta-Analysis of Costs and Financial Impact on the US Health Care System. JAMA Intern. Med. 2013, 173, 2039–2046. [Google Scholar] [CrossRef]
- Zhang, W.; Nuki, G.; Moskowitz, R.W.; Abramson, S.; Altman, R.D.; Arden, N.K.; Bierma-Zeinstra, S.; Brandt, K.D.; Croft, P.; Doherty, M.; et al. OARSI Recommendations for the Management of Hip and Knee Osteoarthritis. Part III: Changes in Evidence Following Systematic Cumulative Update of Research Published through January 2009. Osteoarthr. Cartil. 2010, 18, 476–499. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.E.; Hillman, C.H.; Castelli, D.; Etnier, J.L.; Lee, S.; Tomporowski, P.; Lambourne, K.; Szabo-Reed, A.N. Physical Activity, Fitness, Cognitive Function, and Academic Achievement in Children: A Systematic Review. Med. Sci. Sports Exerc. 2016, 48, 1197–1222. [Google Scholar] [CrossRef]
- Babitsch, B.; Gohl, D.; von Lengerke, T. Re-Revisiting Andersen’s Behavioral Model of Health Services Use: A Systematic Review of Studies from 1998–2011. GMS Psycho-Soc. Med. 2012, 9, Doc11. [Google Scholar]
- Lund, C.; Breen, A.; Flisher, A.J.; Kakuma, R.; Corrigall, J.; Joska, J.A.; Swartz, L.; Patel, V. Poverty and Common Mental Disorders in Low and Middle Income Countries: A Systematic Review. Soc. Sci. Med. 2010, 71, 517–528. [Google Scholar] [CrossRef]
- Munro, S.A.; Lewin, S.A.; Smith, H.J.; Engel, M.E.; Fretheim, A.; Volmink, J. Patient Adherence to Tuberculosis Treatment: A Systematic Review of Qualitative Research. PLoS Med. 2007, 4, e238. [Google Scholar] [CrossRef]
- Theorell, T.; Hammarström, A.; Aronsson, G.; Träskman Bendz, L.; Grape, T.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Hall, C. A Systematic Review Including Meta-Analysis of Work Environment and Depressive Symptoms. BMC Public Health 2015, 15, 738. [Google Scholar] [CrossRef]
- Hout, M. Social and Economic Returns to College Education in the United States. Annu. Rev. Sociol. 2012, 38, 379–400. [Google Scholar] [CrossRef]
- Bellis, M.A.; Hughes, K.; Ford, K.; Ramos Rodriguez, G.; Sethi, D.; Passmore, J. Life Course Health Consequences and Associated Annual Costs of Adverse Childhood Experiences across Europe and North America: A Systematic Review and Meta-Analysis. Lancet Public Health 2019, 4, e517–e528. [Google Scholar] [CrossRef] [PubMed]
- Gomez, L.E.; Bernet, P. Diversity Improves Performance and Outcomes. J. Natl. Med. Assoc. 2019, 111, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Sabel, C.F.; Zeitlin, J. Learning from Difference: The New Architecture of Experimentalist Governance in the EU. Eur. Law J. 2008, 14, 271–327. [Google Scholar] [CrossRef]
- Alomari, M.; Aladi, I. Financial Inclusion and Market-Based Performance: Empirical Evidence from Syrian Banks. J. Financ. Econ. Policy 2023, 16, 60–79. [Google Scholar] [CrossRef]
- Acharya, S.; Swadimath, U.C. Digital Financial Inclusion and Economic Empowerment of Farmers in India. In Utilizing Technology for Sustainable Resource Management Solutions; IGI Global: Hershey, PA, USA, 2024; pp. 295–308. [Google Scholar]
- Kraiwanit, T.; Limna, P.; Wattanasin, P. Digital Wallet Dynamics: Perspectives on Potential Worldcoin Adoption Factors in a Developing Country’s FinTech Sector. J. Open Innov. Technol. Mark. Complex. 2024, 10, 100287. [Google Scholar] [CrossRef]
- Kodom, M.; Osarfo, D.; Quartey, P. Digital Financial Inclusion and Women’s Economic Empowerment in Northern Ghana: The Experience of Rural Women in the Shea Value Chain. In Sustainable Development Goals Series; Springer: Cham, Switzerland, 2024; pp. 179–200. [Google Scholar]
- Suhrab, M.; Chen, P.; Ullah, A. Digital Financial Inclusion and Income Inequality Nexus: Can Technology Innovation and Infrastructure Development Help in Achieving Sustainable Development Goals? Technol. Soc. 2024, 76, 102411. [Google Scholar] [CrossRef]
- Oluwafemi, E.; Esebre, S.D.; Abijo, I.; Timothy, A.M.; Babayemi, T.D.; Makinde, E.O.; Fatoki, I.E. Harnessing Artificial Intelligence to Optimize Financial Technologies for Achieving Sustainable Development Goals. World J. Adv. Res. Rev. 2024, 23, 616–625. [Google Scholar] [CrossRef]
- Leon, F.M. The Effect of Self-Efficacy Financial Mediation on Factors Affecting Financial Inclusion in Small Businesses in West Jakarta. J. Ekon. 2020, 11, 29–42. [Google Scholar] [CrossRef]
- Antonijević, M.; Ljumović, I.; Ivanović, Ž. Is There a Gender Gap in Financial Inclusion Worldwide? J. Women’s Entrep. Educ. 2022, 2022, 79–96. [Google Scholar]
- Callon, M.; Courtial, J.P.; Laville, F. Co-Word Analysis as a Tool for Describing the Network of Interactions between Basic and Technological Research: The Case of Polymer Chemistry. Scientometrics 1991, 22, 155–205. [Google Scholar] [CrossRef]
- Balasubramanian, P.; Ibanez, M.; Sahoo, S. Does Women’s Economic Empowerment Promote Human Development in Low- and Middle-Income Countries? A Meta-Analysis. World Dev. 2024, 175, 106588. [Google Scholar] [CrossRef]
- Al-Hanawi, M.K.; Al Rahahleh, N. Mitigating Role of Financial Inclusion on Medical Expenses in Saudi Arabia. Cost Eff. Resour. Alloc. 2024, 22, 2. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, C.; Alem, A.; Chisholm, D. Moving Towards Universal Health Coverage for Mental Disorders in Ethiopia. Int. J. Ment. Health Syst. 2019, 13, 11. [Google Scholar] [CrossRef] [PubMed]
- Acheampong, A.O.; Tetteh, G.K. Does Financial Inclusion Matter to Population Health? Insight from a Global Dataset. Soc. Indic. Res. 2024, 172, 1005–1040. [Google Scholar] [CrossRef]
- Rush, K.L.; Seaton, C.; Pesut, B. Rural Use of Health Service and Telemedicine During COVID-19: The Role of Access and eHealth Literacy. Health Inform. J. 2021, 27, 14604582211020064. [Google Scholar] [CrossRef]
- Adel, N. The Impact of Digital Literacy and Technology Adoption on Financial Inclusion in Africa, Asia, and Latin America. Heliyon 2024, 10, e40951. [Google Scholar] [CrossRef]
- Bollaert, H.; Lopez-de-Silanes, F.; Schwienbacher, A. Fintech and Access to Finance. J. Corp. Finance 2021, 68, 101941. [Google Scholar] [CrossRef]
- Tan, B.J. Central Bank Digital Currency and Financial Inclusion. J. Macroecon. 2024, 81, 103620. [Google Scholar] [CrossRef]
- Corbet, S.; Cumming, D.; Glatzer, Z.; Johan, S. Understanding the Rapid Development of CBDC in Emerging Economies. Financ. Res. Lett. 2024, 70, 106226. [Google Scholar] [CrossRef]
- Gyasi, R.M.; Adam, A.M.; Phillips, D.R. Financial Inclusion, Health-Seeking Behavior, and Health Outcomes Among Older Adults in Ghana. Res. Aging 2019, 41, 794–820. [Google Scholar] [CrossRef]
- Koomson, I.; Abdul-Mumuni, A.; Abbam, A. Effect of Financial Inclusion on Out-of-Pocket Health Expenditure: Empirics from Ghana. Eur. J. Health Econ. 2021, 22, 1411–1425. [Google Scholar] [CrossRef] [PubMed]
- Alhanawi, M.K.; Chirwa, G.C.; Kamninga, T.M.; Manja, L.P. Effects of Financial Inclusion on Access to Emergency Funds for Healthcare in the Kingdom of Saudi Arabia. J. Multidiscip. Healthc. 2020, 13, 1157–1167. [Google Scholar] [CrossRef]
- Banerjee, R.; Maruta, A.A.; Donato, R. Does Higher Financial Inclusion Lead to Better Health Outcomes? Evidence from Developing and Transitional Economies. Econ. Transit. Inst. Change 2023, 31, 363–401. [Google Scholar] [CrossRef]
- Wirajing, M.A.K.; Haruna, A.; Nchofoung, T.N. Financial Inclusion and Healthcare in Africa: Examining the Moderating Role of Education. Rev. Dev. Econ. 2024, 28, 97–127. [Google Scholar] [CrossRef]
- Naveenan, R.V.; Liew, C.Y.; Kijkasiwat, P. Nexus between Financial Inclusion, Digital Inclusion, and Health Outcomes: Evidence from Developing Economies. Soc. Indic. Res. 2024, 174, 367–408. [Google Scholar] [CrossRef]
- Ajide, F.; Osinubi, T.; Ojeyinka, T.; Kudaisi, B.V. The Interactive Effects of Financial Inclusion and Women Political Empowerment on Health Outcomes in Africa. In The Role of Female Leaders in Achieving the Sustainable Development Goals; IGI Global: Hershey, PA, USA, 2024; pp. 136–159. [Google Scholar] [CrossRef]
- Nyamugira, A.B.; Flessa, S.; Richter, A. Health Insurance Uptake, Poverty and Financial Inclusion in the Democratic Republic of Congo. Sustain. Dev. 2024, 32, 3293–3312. [Google Scholar] [CrossRef]
- Saraswati, P.W. Corrigendum: Saving More Lives on Time: Strategic Policy Implementation and Financial Inclusion for Safe Abortion in Indonesia during COVID-19 and Beyond. Front. Glob. Women’s Health 2023, 4, 1129026. [Google Scholar] [CrossRef]
- Carmichael, A.E.; Lennon, N.H.; Qualters, J.R. Analysis of Social Determinants of Health and Individual Factors Found in Health Equity Frameworks: Applications to Injury Research. J. Saf. Res. 2023, 87, 508–518. [Google Scholar] [CrossRef]
- Kapalu, C.L.; Wilkes, C.D. Toward Promotion of Health Equity in Pediatric Disorders of Gut–Brain Interaction: A Call to Action. Clin. Pract. Pediatr. Psychol. 2023, 11, 449–464. [Google Scholar] [CrossRef]
- Cook, N.E.; Kissinger-Knox, A.; Iverson, I.A.; Liu, B.C.; Gaudet, C.E.; Norman, M.A.; Iverson, G.L. Social Determinants of Health and Health Equity in the Diagnosis and Management of Pediatric Mild Traumatic Brain Injury: A Content Analysis of Research Underlying Clinical Guidelines. J. Neurotrauma 2023, 40, 1977–1989. [Google Scholar] [CrossRef]
- Osae, S.P.; Chastain, D.B.; Young, H.N. Pharmacist Role in Addressing Health Disparities—Part 2: Strategies to Move Toward Health Equity. J. Am. Coll. Clin. Pharm. 2022, 5, 541–550. [Google Scholar] [CrossRef]
- Macintyre, A.K.; Shipton, D.; Sarica, S.; Scobie, G.; Craig, N.; McCartney, G. Assessing the Effects of Population-Level Political, Economic and Social Exposures, Interventions and Policies on Inclusive Economy Outcomes for Health Equity in High-Income Countries: A Systematic Review of Reviews. Syst. Rev. 2024, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Coulter, N.; Monarch, I.; Konda, S. Software Engineering as Seen through Its Research Literature: A Study in Co-Word Analysis. J. Am. Soc. Inf. Sci. 1998, 49, 1206–1223. [Google Scholar] [CrossRef]
- Oke, G.I.; Nsofor, I.; Abubakar, B.; Lucero-Prisno, D.E.; Sunday, A.P.; Dibia, E.O. Experience of People Living with Leprosy at Leprosy Settlements in Nigeria. Public Health Chall. 2024, 3, e171. [Google Scholar] [CrossRef] [PubMed]
- Song, A. Financial Sustainability of Microfinance Institutions in Sub-Saharan Africa: Challenges and Solutions. Res. Beacon 2024, 18, 13–24. [Google Scholar] [CrossRef]
- Banerjee, A.V.; Duflo, E. Poor Economics: A Radical Rethinking of the Way to Fight Global Poverty; PublicAffairs: New York, NY, USA, 2011. [Google Scholar]
- Suri, T.; Jack, W. The Long-Run Poverty and Gender Impacts of Mobile Money. Science 2016, 354, 1288–1292. [Google Scholar] [CrossRef]
- Aria, M.; Cuccurullo, C. Bibliometrix: An R-tool for Comprehensive Science Mapping Analysis. J. Informetr. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Zupic, I.; Čater, T. Bibliometric Methods in Management and Organization. Organ. Res. Methods 2015, 18, 429–472. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Boyce, T.; Goldblatt, P.; Morrison, J. Health Equity in England: The Marmot Review 10 Years on; The Health Foundation: London, UK, 2020. [Google Scholar]
- Kuhn, T.S. The Structure of Scientific Revolutions, 2nd ed.; University of Chicago Press: Chicago, IL, USA, 1962. [Google Scholar]
- Levine, R.; Zervos, S. Financial Inclusion and Economic Growth. J. Econ. Perspect. 2016, 30, 67–88. [Google Scholar]
- Dror, D.M. Health Microinsurance Programs in Developing Countries. In Encyclopedia of Health Economics; Culyer, A.J., Ed.; Elsevier: Amsterdam, The Netherlands, 2014; pp. 412–421. [Google Scholar] [CrossRef]
- Bobek, J.; Braunegger-Kallinger, G.; Winkler, P. Social Protection and Health: Links Between Social Protection Measures and Health Equity. Präv. Gesundheitsf. 2019, 14, 214–220. [Google Scholar] [CrossRef]
- Santos Salas, A.; Bassah, N.; Pujadas Botey, A.; Robson, P.; Beranek, J.; Iyiola, I. Interventions to Improve Access to Cancer Care in Underserved Populations in High Income Countries: A Systematic Review. Oncol. Rev. 2024, 18, 1427441. [Google Scholar] [CrossRef]
- Ryan, G.K.; Nwefoh, E.; Eaton, J. Partnership for the Implementation of Mental Health Policy in Nigeria: A Case Study of the Comprehensive Community Mental Health Programme in Benue State. Int. J. Ment. Health Syst. 2020, 14, 17. [Google Scholar] [CrossRef]
- Silva, F.N.S.; Sousa, M.E.C.; Lourenço, C.E.; Paiva, A.V.P.; Monteiro, T.C.; Grimaldi, M.R.M. Discrimination and Access to Healthcare for People with Disabilities: An Integrative Literature Review. Aquichan 2024, 24, e2434. [Google Scholar] [CrossRef]
- Wood, S.M.; Alston, L.; Chapman, A.; Lenehan, J.; Versace, V.L. Barriers and Facilitators to Women’s Access to Sexual and Reproductive Health Services in Rural Australia: A Systematic Review. BMC Health Serv. Res. 2024, 24, 1221. [Google Scholar] [CrossRef]
- Mugisha, N.; Uwishema, O.; Noureddine, R.; Ghanem, L.; Manoel, A.Z.; Shariff, S. Utilization of Mobile Surgical Units to Address Surgical Needs in Remote African Communities: A Narrative Review. BMC Surg. 2024, 24, 304. [Google Scholar] [CrossRef]
- Pei, X.; Wang, B.; Yang, X.; Feng, W.; Sun, Y.; Wang, H. Analysis of the Changing Trend of Economic Burden of Patients with Chronic Diseases under the Integrated Medical and Health Service System. BMC Public Health 2023, 23, 731. [Google Scholar] [CrossRef]
- Farmer, P.E.; Nizeye, B.; Stulac, S.; Keshavjee, S. Structural Violence and Clinical Medicine. PLoS Med. 2006, 3, e449. [Google Scholar] [CrossRef]
- Gentilini, U.; Almenfi, M.; Orton, I.; Dale, P. Social Protection and Jobs Responses to COVID-19: A Real-Time Review of Country Measures; The World Bank: Washington, DC, USA, 2020. [Google Scholar]
- Karlan, D.; Appel, J. Failing in the Field: What We Can Learn When Field Research Goes Wrong; Princeton University Press: Princeton, NJ, USA, 2016. [Google Scholar]
- O’Donnell, O.; van Doorslaer, E.; Wagstaff, A.; Lindelow, M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation; The World Bank: Washington, DC, USA, 2008. [Google Scholar]
- Drèze, J.; Khera, R. Recent Social Security Initiatives in India. World Dev. 2017, 98, 555–572. [Google Scholar] [CrossRef]
- Jack, W.; Suri, T. Risk Sharing and Transactions Costs: Evidence from Kenya’s Mobile Money Revolution. Am. Econ. Rev. 2014, 104, 183–223. [Google Scholar] [CrossRef]
- Tandon, A. Privacy and Reproductive Health: Curtailing Rights and Choices. Socio-Legal Rev. 2021, 17, 136. [Google Scholar] [CrossRef]
- Hosseinpoor, A.R.; Bergen, N. Health Inequality Monitoring: A Practical Application of Population Health Monitoring. In Population Health Monitoring: Climbing the Information Pyramid; Springer: Cham, Switzerland, 2018; pp. 121–137. [Google Scholar] [CrossRef]
- Green, T.; Venkataramani, A.S. Trade-Offs and Policy Options—Using Insights from Economics to Inform Public Health Policy. N. Engl. J. Med. 2022, 386, 1094–1097. [Google Scholar] [CrossRef]
- Dupas, P.; Robinson, J. Why Don’t the Poor Save More? Evidence from Health Savings Experiments. Am. Econ. Rev. 2013, 103, 1138–1171. [Google Scholar] [CrossRef]
- Msheik, L.; Barakat, M.; Jaber, J. Challenges Facing Telemedicine in Low Income Countries. Electron. J. Med. Dent. Stud. 2023, 4, em0141. [Google Scholar] [CrossRef]
- Kabeer, N. Gender Equality and Women’s Empowerment: A Critical Analysis of the Third Millennium Development Goal. Gend. Dev. 2005, 13, 13–24. [Google Scholar] [CrossRef]
- Malki, I.; Ghalib, A.; Kaousar, R. The Impact of Microfinance on Entrepreneurship and Welfare Among Women Borrowers in Rural Pakistan. World Dev. Perspect. 2024, 35, 100616. [Google Scholar] [CrossRef]
- Chirambo, D. Enhancing Climate Change Resilience Through Microfinance: Redefining the Climate Finance Paradigm to Promote Inclusive Growth in Africa. J. Dev. Soc. 2017, 33, 147–170. [Google Scholar] [CrossRef]
| Ref. No. | Reference Title | Total Citation | TC Per Year |
|---|---|---|---|
| [22] | Costello, A.; Abbas, M.; Allen, A.; Ball, S.; Bell, S.; Bellamy, R.; Friel, S.; Groce, N.; Johnson, A.; Kett, M.; et al. Managing the health effects of climate change. Lancet 2009, 373, 1693–1733. | 2095 | 26.18 |
| [23] | Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. | 1993 | 24.91 |
| [24] | Zimlichman, E.; Henderson, D.; Tamir, O.; Franz, C.; Song, P.; Yamin, C.K.; Keohane, C.; Denham, C.R.; Bates, D.W. Health care-associated infections: A meta-analysis of costs and financial impact on the US health care system. JAMA Intern. Med. 2013, 173, 2039–2046. | 1441 | 18.01 |
| [25] | Zhang, W.; Nuki, G.; Moskowitz, R.W.; Abramson, S.; Altman, R.D.; Arden, N.K.; Bierma-Zeinstra, S.; Brandt, K.D.; Croft, P.; Doherty, M.; et al. OARSI recommendations for the management of hip and knee osteoarthritis. Part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthr. Cartil. 2010, 18, 476–499. | 1355 | 16.93 |
| [26] | Donnelly, J.E.; Hillman, C.H.; Castelli, D.; Etnier, J.L.; Lee, S.; Tomporowski, P.; Lambourne, K.; Szabo-Reed, A.N. Physical activity, fitness, cognitive function, and academic achievement in children: A systematic review. Med. Sci. Sports Exerc. 2016, 48, 1197–1222. | 1174 | 14.67 |
| [27] | Babitsch, B.; Gohl, D.; von Lengerke, T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: A systematic review of studies from 1998–2011. GMS Psycho-Soc. Med. 2012, 9, Doc11. | 881 | 11.01 |
| [28] | Lund, C.; Breen, A.; Flisher, A.J.; Kakuma, R.; Corrigall, J.; Joska, J.A.; Swartz, L.; Patel, V. Poverty and common mental disorders in low and middle income countries: A systematic review. Soc. Sci. Med. 2010, 71, 517–528. | 851 | 10.63 |
| [29] | Munro, S.A.; Lewin, S.A.; Smith, H.J.; Engel, M.E.; Fretheim, A.; Volmink, J. Patient adherence to tuberculosis treatment: A systematic review of qualitative research. PLoS Med. 2007, 4, e238. | 740 | 9.25 |
| [30] | Theorell, T.; Hammarström, A.; Aronsson, G.; Träskman Bendz, L.; Grape, T.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Hall, C. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 2015, 15, 738. | 714 | 8.92 |
| [31] | Hout, M. Social and economic returns to college education in the United States. Annu. Rev. Sociol. 2012, 38, 379–400. | 663 | 8.28 |
| [32] | Bellis, M.A.; Hughes, K.; Ford, K.; Ramos Rodriguez, G.; Sethi, D.; Passmore, J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: A systematic review and meta-analysis. Lancet Public Health 2019, 4, e517–e528. | 642 | 8.02 |
| [33] | Gomez, L.E.; Bernet, P. Diversity improves performance and outcomes. J. Natl. Med. Assoc. 2019, 111, 383–392. | 619 | 7.73 |
| [34] | Sabel, C.F.; Zeitlin, J. Learning from difference: The new architecture of experimentalist governance in the EU. Eur. Law J. 2008, 14, 271–327. | 615 | 7.68 |
| Journal | Publications | Ratio (%) |
|---|---|---|
| Front. Public Health | 506 | 2.1 |
| BMJ Open | 455 | 1.88 |
| PLoS One | 357 | 1.48 |
| Cureus | 345 | 1.43 |
| Cochrane Database Syst Rev | 270 | 1.12 |
| BMC Public Health | 240 | 0.99 |
| Front. Psychol. | 225 | 0.93 |
| Int. J. Environ Res. Public Health | 207 | 0.86 |
| BMC Health Serv. Res. | 206 | 0.85 |
| Subject Area | Number Article | Ratio |
|---|---|---|
| Health/Medical | 10,381 | 59.24% |
| Technology/Digital | 3275 | 18.69% |
| Finance/Economics | 1626 | 9.28% |
| Social Sciences | 839 | 4.79% |
| Business/Management | 482 | 2.75% |
| Education | 444 | 2.53% |
| Policy/Governance | 226 | 1.29% |
| Research Methodology | 134 | 0.76% |
| Public Health | 118 | 0.67% |
| Ref. No. | Paper Title | Total Citations | IF | Abstract of the Article |
|---|---|---|---|---|
| [53] | Gyasi, R.M.; Adam, A.M.; Phillips, D.R. Financial Inclusion, Health-Seeking Behavior, and Health Outcomes Among Older Adults in Ghana. Res. Aging 2019, 41, 794–820. https://doi.org/10.1177/0164027519846604 | 51 | 1.8 | This study examines the associations between financial inclusion, health-seeking behavior, and health-related outcomes in older persons in Ghana. we estimated regression models of self-rated health (SRH), psychological distress (PD), and health-care use (HCU) on a variable representing compositional characteristics of financial inclusion. |
| [54] | Koomson, I., Abdul-Mumuni, A., & Abbam, A. 2021. Effect of financial inclusion on out-of-pocket health expenditure: Empirics from Ghana. European Journal of Health Economics, 22(9):14111425. https://doi.org/10.1007/s10198-021-01320-1 | 34 | 6.1 | This study examines the link between financial inclusion and out-of-pocket health expenditure in Ghana. It finds that increased financial inclusion is associated with higher out-of-pocket health spending, especially among female-headed and urban households. The study suggests that scaling up financial inclusion can facilitate better health outcomes by enabling households to invest in health. |
| [55] | Alhanawi, M. K., Chirwa, G. C., Kamninga, T. M., & Manja, L. P. 2020. Effects of financial inclusion on access to emergency funds for healthcare in the Kingdom of Saudi Arabia. Journal of Multidisciplinary Healthcare,13:11571167. https://doi.org/10.2147/JMDH.S277357 | 15 | 4.6 | This research investigates the effects of financial inclusion on access to emergency funds for healthcare in Saudi Arabia. It reveals that financially included individuals have a higher probability of accessing emergency funds and borrowing for medical purposes, particularly among low-income groups. The study underscores the need for policies that promote financial inclusion to enhance healthcare access. |
| [56] | Banerjee, R., Maruta, A. A., & Donato, R. 2023. Does higher financial inclusion lead to better health outcomes? Evidence from developing and transitional economies. Economics of Transition and Institutional Change, 31(2): 363–401. https://doi.org/10.1111/ecot.12341 | 9 | 1.7 | This research analyzes the impact of financial inclusion on life expectancy and infant mortality in developing and transitional economies. It finds that financial inclusion improves health outcomes, particularly in societies with higher poverty and income inequality. The study emphasizes the role of financial inclusion in enhancing health capital and risk management. |
| [57] | Wirajing, M. A. K., Haruna, A., & Nchofoung, T. N. 2024. Financial inclusion and healthcare in Africa: Examining the moderating role of education. Review of Development Economics, 28(1): 97–127. https://doi.org/10.1111/rode.13043 | 3 | 3.2 | This study investigates the effect of financial inclusion on healthcare in Africa, with a focus on the moderating role of education. It finds that financial inclusion enhances healthcare outcomes, particularly when combined with education and technology diffusion. The study suggests that financial literacy programs can improve healthcare in Africa. |
| [58] | Naveenan, R. V., Liew, C. Y., & Kijkasiwat, P. 2024. Nexus between financial inclusion, digital inclusion, and health outcomes: Evidence from developing economies. Social Indicators Research, 174(1): 367–408. https://doi.org/10.1007/s11205-024-03391-y | 2 | 6.3 | This research explores the nexus between financial inclusion, digital inclusion, and health outcomes in developing economies. It finds that digital inclusion moderates the impact of financial inclusion on health outcomes. The study suggests that policies promoting both financial and digital inclusion can enhance health indices in emerging markets. |
| [47] | Acheampong, A. O., & Tetteh, G. K. 2024. Does financial inclusion matter to population health? Insight from a global dataset. Social Indicators Research, 172(3): 1005–1040. https://doi.org/10.1007/s11205-024-03341-8 | 0 | 6.3 | This global study investigates the relationship between financial inclusion and population health across 121 countries. It finds that financial inclusion improves health outcomes, especially in countries with lower income inequality and higher ICT penetration. The study highlights the importance of financial inclusion policies in promoting population health. |
| [59] | Ajide, F., Osinubi, T., Ojeyinka, T., & Kudaisi, B. V. 2024. The interactive effects of financial inclusion and women political empowerment on health outcomes in Africa. In The Role of Female Leaders in Achieving the Sustainable Development Goals: 136–159. https://doi.org/10.4018/979-8-3693-1834-8.ch008 | 0 | N. A | This study examines the interactive effects of financial inclusion and women’s political empowerment on health outcomes in Africa. It finds that financial inclusion strengthens women’s political empowerment, leading to better health outcomes. The study highlights the role of financial inclusion in achieving Sustainable Development Goal 3 (SDG-3). |
| [60] | Nyamugira, A. B., Flessa, S., & Richter, A. 2024. Health insurance uptake, poverty and financial inclusion in the Democratic Republic of Congo. Sustainable Development, 32(4): 3293–3312. https://doi.org/10.1002/sd.2841 | 0 | 17.3 | This research estimates the prevalence of health insurance coverage in the Democratic Republic of Congo and its association with financial inclusion. It finds that financial inclusion, proxied by bank account ownership, is strongly associated with higher health insurance coverage. The study recommends policies to improve financial inclusion to enhance health insurance uptake. |
| [61] | Saraswati, P. W. 2023. Corrigendum: Saving more lives on time: Strategic policy implementation and financial inclusion for safe abortion in Indonesia during COVID-19 and beyond. Frontiers in Global Women’s Health, 4: 1129026. https://doi.org/10.3389/fgwh.2023.1129026 | 0 | 3.7 | This corrigendum corrects errors in a previous study on financial inclusion and safe abortion services in Indonesia. The original study highlights the importance of financial inclusion in providing safe abortion services, particularly through partnerships with the nonprofit private sector. The study underscores the role of financial inclusion in improving women’s health outcomes. |
| Ref. No. | Paper Title | Total Citation | CiteScore | Abstract of the Article |
|---|---|---|---|---|
| [62] | Carmichael, A.E.; Lennon, N.H.; Qualters, J.R. Analysis of social determinants of health and individual factors found in health equity frameworks: Applications to injury research. J. Saf. Res. 2023, 87, 508–518. https://doi.org/10.1016/j.jsr.2023.10.001 | 1 | 6.9 | Introduction: This research evaluated existing health equity frameworks as they relate to social determinants of health (SDOHs) and individual factors that may impact injury outcomes and identify gaps in coverage using the Healthy People (HP) 2030 key domains. Methods: The study used a list of health equity frameworks sourced from previous literature. SDOHs and individual factors from each framework were identified and categorized into the Healthy People 2030 domains. Five injury topic areas were used as examples for how SDOHs and individual factors can be compared to injury topic-specific health disparities to identify health equity frameworks to apply to injury research. Results: The study identified 59 SDOHs and individual factors from the list of 33 health equity frameworks |
| [63] | Kapalu, C.L.; Wilkes, C.D. Toward Promotion of Health Equity in Pediatric Disorders of Gut–Brain Interaction: A Call to Action. Clin. Pract. Pediatr. Psychol. 2023, 11, 449–464. https://doi.org/10.1037/cpp0000507 | 1 | 2.2 | There has been increased attention to health equity, or the opportunity to obtain one’s health potential without disadvantage caused by discriminatory social systems, in recent years. The social determinants of health (SDoH), including economic stability, educational access and quality, healthcare access and quality, neighborhood and built environment, and social and community context, are the social, political, and systems-level factors that contribute to health inequities. In this commentary, the authors will review the ways in which structural and systemic racism impact health, discuss what is known about SDoH in pediatric DGBIs and propose a call to action for pediatric psychologists to promote health equity via research, clinical work, teaching, and advocacy. |
| [64] | Cook, N.E.; Kissinger-Knox, A.; Iverson, I.A.; Liu, B.C.; Gaudet, C.E.; Norman, M.A.; Iverson, G.L. Social Determinants of Health and Health Equity in the Diagnosis and Management of Pediatric Mild Traumatic Brain Injury: A Content Analysis of Research Underlying Clinical Guidelines. J. Neurotrauma 2023, 40, 1977–1989. https://doi.org/10.1089/neu.2023.0021 | 6 | 8.9 | A content analysis of the literature underlying the Centers for Disease Control and Prevention (CDC) Guideline on the Diagnosis and Management of Mild Traumatic Brain Injury Among Children (i.e., the ‘‘Guideline’’) was conducted to determine the extent to which social determinants of health (SDoH) were examined or addressed. The systematic review forming the basis for the Guideline included 37 studies addressing diagnosis, prognosis, and treatment/rehabilitation. We examined those studies to identify SDoH domains derived from the U.S. Department of Health and Human Services’ Healthy People 2020 and 2030 websites. |
| [65] | Osae, S.P.; Chastain, D.B.; Young, H.N. Pharmacist role in addressing health disparities—Part 2: Strategies to move toward health equity. JACCP J. Am. Coll. Clin. Pharm. 2022, 5, 541–550. https://doi.org/10.1002/jac5.1594 | 10 | 2.6 | Health disparities or extreme gaps of health across different groups of people result in poor outcomes for many Americans today. Pharmacists have an important role in addressing health disparities across many populations. Contextualizing root causes of gaps in health care and outcomes and identifying potential solutions to address those root causes are important initial steps clinical pharmacists can take to combat health disparities. PubMed and Web of Science were searched to identify articles published from inception until 9 May 2021. |
| [66] | Macintyre, A.K.; Shipton, D.; Sarica, S.; Scobie, G.; Craig, N.; McCartney, G. Assessing the effects of population-level political, economic and social exposures, interventions and policies on inclusive economy outcomes for health equity in high-income countries: A systematic review of reviews. Syst. Rev. 2024, 13, 1. https://doi.org/10.1186/s13643-023-02429-5 | 0 | 11.0 | A fairer economy is increasingly recognised as crucial for tackling widening social, economic and health inequalities within society. However, which actions have been evaluated for their impact on inclusive economy outcomes is yet unknown. Objective: Identify the effects of political, economic and social exposures, interventions and policies on inclusive economy (IE) outcomes in high-income countries, by systematically reviewing the review-level evidence. We conducted a review of reviews; searching databases (May 2020) EconLit, Web of Science, Sociological Abstracts, ASSIA, International Bibliography of the Social Sciences, Public Health Database, Embase and MEDLINE; and registries PROSPERO, Campbell Collaboration and EPPI Centre (February 2021) |
| Cluster | Top 3 Keywords | Betweenness Centrality (Top Node) | PageRank (Top Node) | Centrality | Cluster Frequency | Interpretation |
|---|---|---|---|---|---|---|
| 1. Foundational Health Demographics | Human, Female, Humans | 1000.00 (human) | 0.030 (human) | 0.8235 | 6 | Core demographic bridge concepts—Basic human identifiers serve as primary interdisciplinary connectors with maximum network centrality, linking diverse health research areas through common participant characteristics. |
| 2. Age-Specific Health Epidemiology | Aged, Middle Aged, Child | 386.27 (aged) | 0.0125 (aged) | 0.3862 | 22 | Life stage health specialization—Focused research on age-specific health issues with strong bridging between pediatric, adult, and geriatric medicine, showing moderate interdisciplinary connectivity. |
| 3. Health Research Methodology | Sensitivity Analysis, Awareness, Body Mass | 24.76 (sensitivity analysis) | 0.0010 | 0.0661 | 1338 | Methodological and behavioral studies—Quantitative research techniques and health behavior investigations forming a large but specialized cluster with limited cross-theme connectivity. |
| 4. Socioeconomic Health Determinants | Health Insurance, Education, Income | 132.72 (health insurance) | 0.0047 (health insurance) | 0.1825 | 101 | Financial and educational health influences—Research examining how economic resources and education impact health outcomes, showing moderate bridging capacity between financial and health domains. |
| 5. Health Equity & Chronic Conditions | Health Equity, Obesity, Anxiety | 42.37 (health equity) | 0.0017 (health equity) | 0.1295 | 487 | Disparities in chronic disease burden—Studies addressing health inequities in the context of obesity, mental health, and other chronic conditions, with emerging interdisciplinary connections. |
| 6. Clinical Health Services | Infection Risk, Children, Electronic Medical Record | 7.33 (infection risk) | 0.00036 | 0.0256 | 3065 | Clinical operations and pediatric care—Largest cluster focused on healthcare delivery, infection control, and pediatric health services, highly specialized with minimal cross-theme bridging. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Nazha, H.M.; Alomari, M.; Darwich, M.A. Bridging Financial Inclusion and Health Equity in LMICs: Evidence from a Half-Century of Bibliometric Data. Int. J. Environ. Res. Public Health 2026, 23, 96. https://doi.org/10.3390/ijerph23010096
Nazha HM, Alomari M, Darwich MA. Bridging Financial Inclusion and Health Equity in LMICs: Evidence from a Half-Century of Bibliometric Data. International Journal of Environmental Research and Public Health. 2026; 23(1):96. https://doi.org/10.3390/ijerph23010096
Chicago/Turabian StyleNazha, Hasan Mhd, Masah Alomari, and Mhd Ayham Darwich. 2026. "Bridging Financial Inclusion and Health Equity in LMICs: Evidence from a Half-Century of Bibliometric Data" International Journal of Environmental Research and Public Health 23, no. 1: 96. https://doi.org/10.3390/ijerph23010096
APA StyleNazha, H. M., Alomari, M., & Darwich, M. A. (2026). Bridging Financial Inclusion and Health Equity in LMICs: Evidence from a Half-Century of Bibliometric Data. International Journal of Environmental Research and Public Health, 23(1), 96. https://doi.org/10.3390/ijerph23010096








