Nutrition and Social Disadvantage as Risk Factors for Mortality Among School-Age Children: Regional Differences in Kazakhstan
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Socioeconomic and Dietary Indicators
2.2.1. Consumption of Major Food Groups
- kg per capita per year—bread and cereals, meat and meat products, fish and seafood, oils and fats, vegetables, fruits, potatoes, sugar and confectionery;
- liters per capita per year—milk and dairy products;
- pieces per capita per year—eggs.
2.2.2. Poverty Indicators
2.2.3. Gross Regional Product (GRP)
2.3. Handling of Missing Data
2.4. Regression Analysis
- −
- per capita consumption of major food groups;
- −
- proportion of the population with incomes below the subsistence minimum;
- −
- gross regional product;
- −
- calendar year of observation.
- −
- marginal R2—variance explained by fixed effects;
- −
- conditional R2—variance explained by fixed and random effects combined;
- −
- intraclass correlation coefficient (ICC)—proportion of between-region variance.
2.5. Statistical Analysis
3. Results
- “Diseases of the respiratory system” (ICD-10: J00–J99);
- “Diseases of the circulatory system” (ICD-10: I00–I99);
- “Congenital malformations, deformations and chromosomal abnormalities” (ICD-10: Q00–Q99);
- “Certain infectious and parasitic diseases” (ICD-10: A00–B99);
- “Endocrine, nutritional and metabolic diseases” (ICD-10: E00–E90);
- “Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified” (ICD-10: R00–R99).
4. Discussion
4.1. Role of Diet and Food Security
4.2. Poverty as a Social Determinant
4.3. Regional Disparities in Child Mortality Within Countries
4.4. Comparison with the Findings of the Present Study
4.5. Limitations
4.6. Key Points
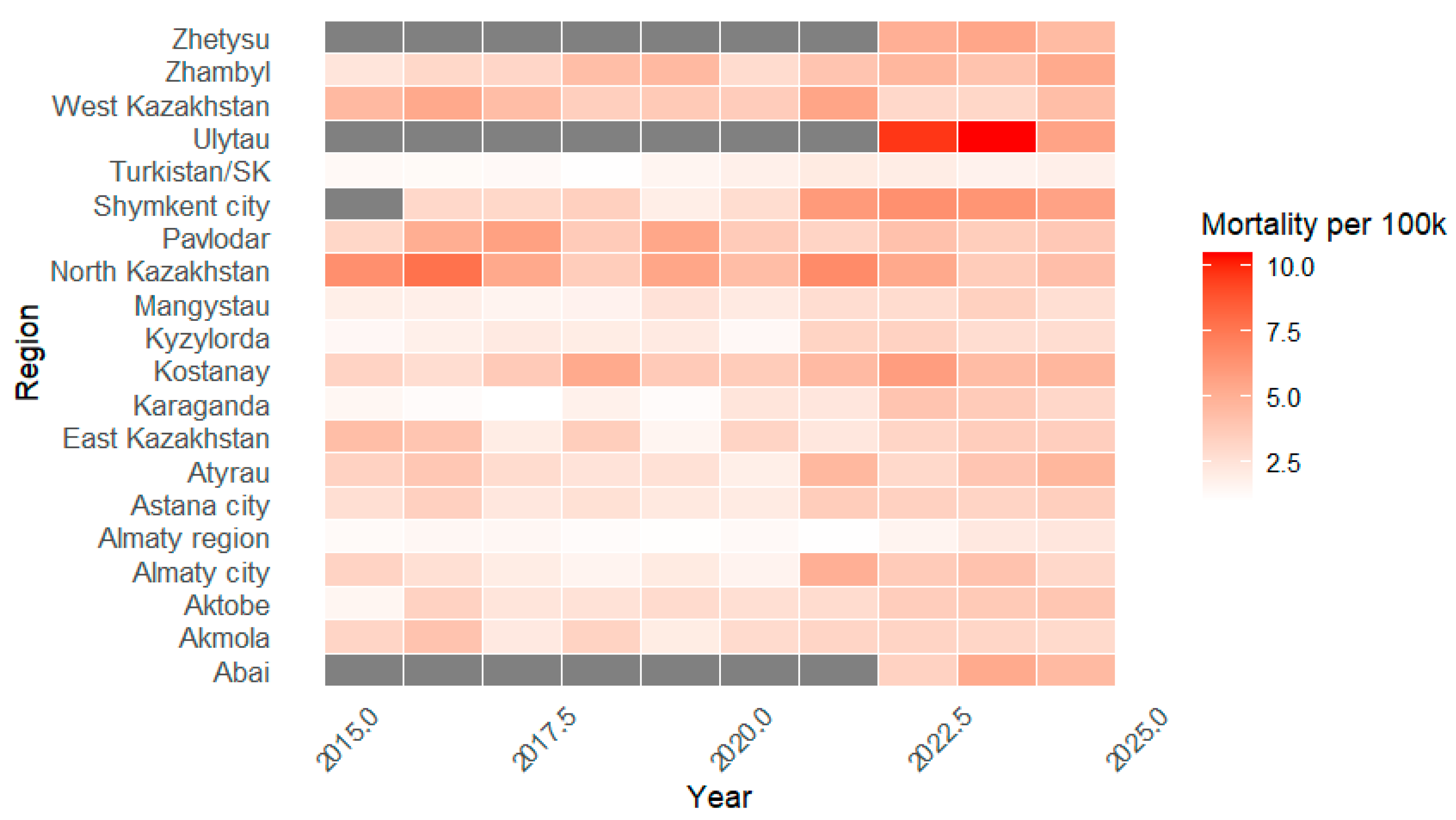
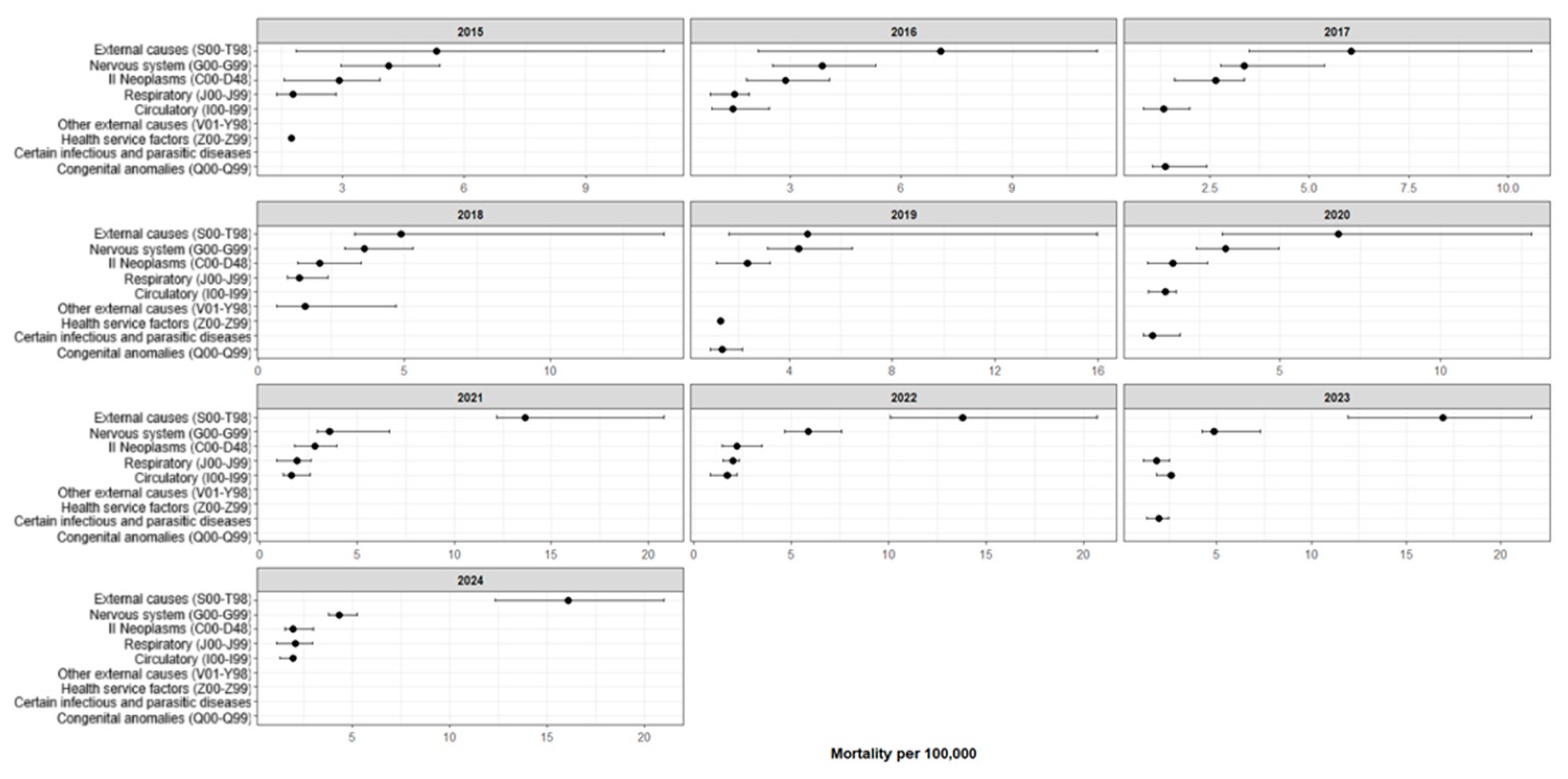
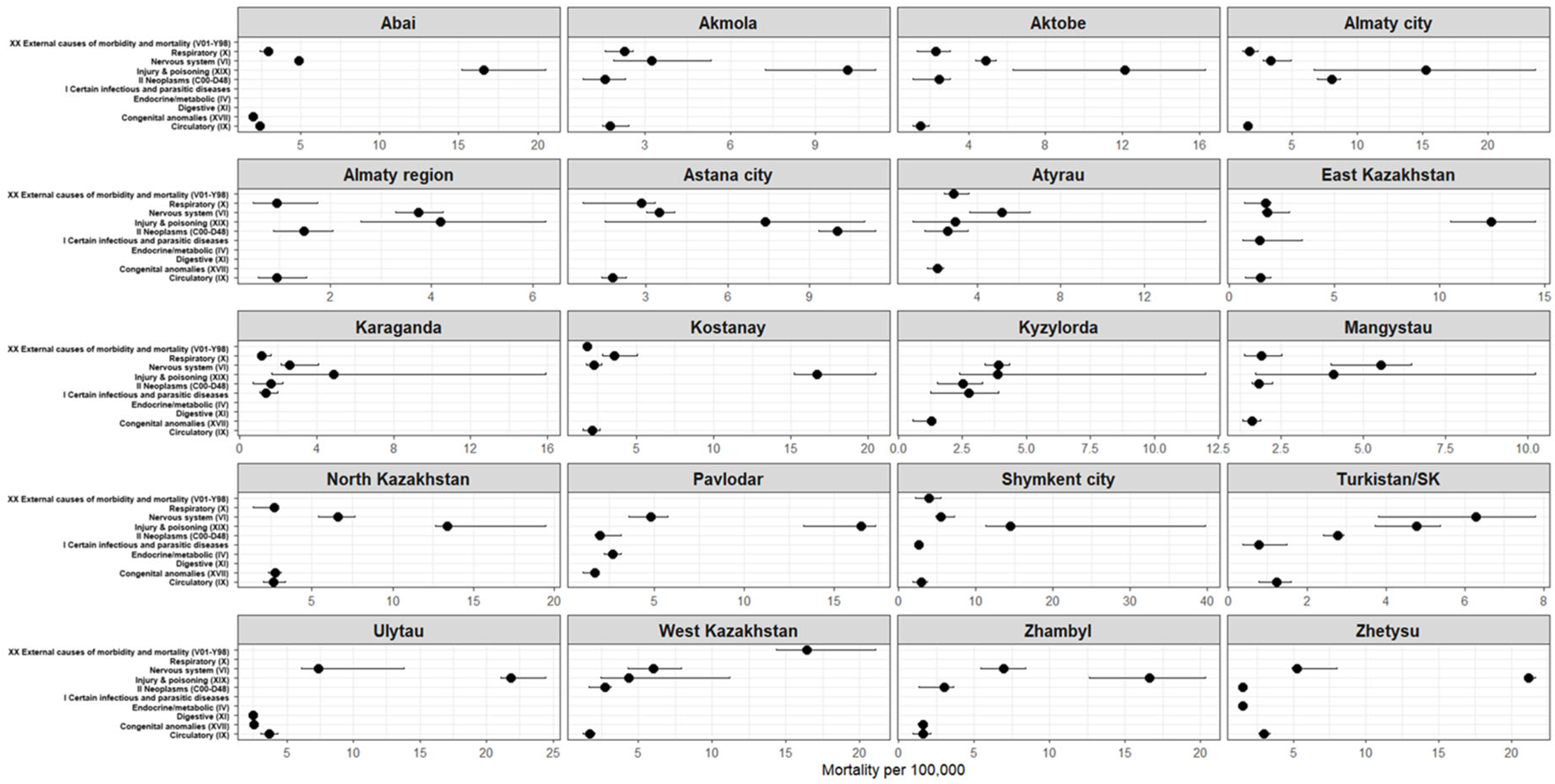
- Between 2015 and 2024, mortality among children aged 6–17 years in Kazakhstan remained relatively low, but showed considerable variation across regions and calendar years, with no clear linear trend towards either increase or decrease.
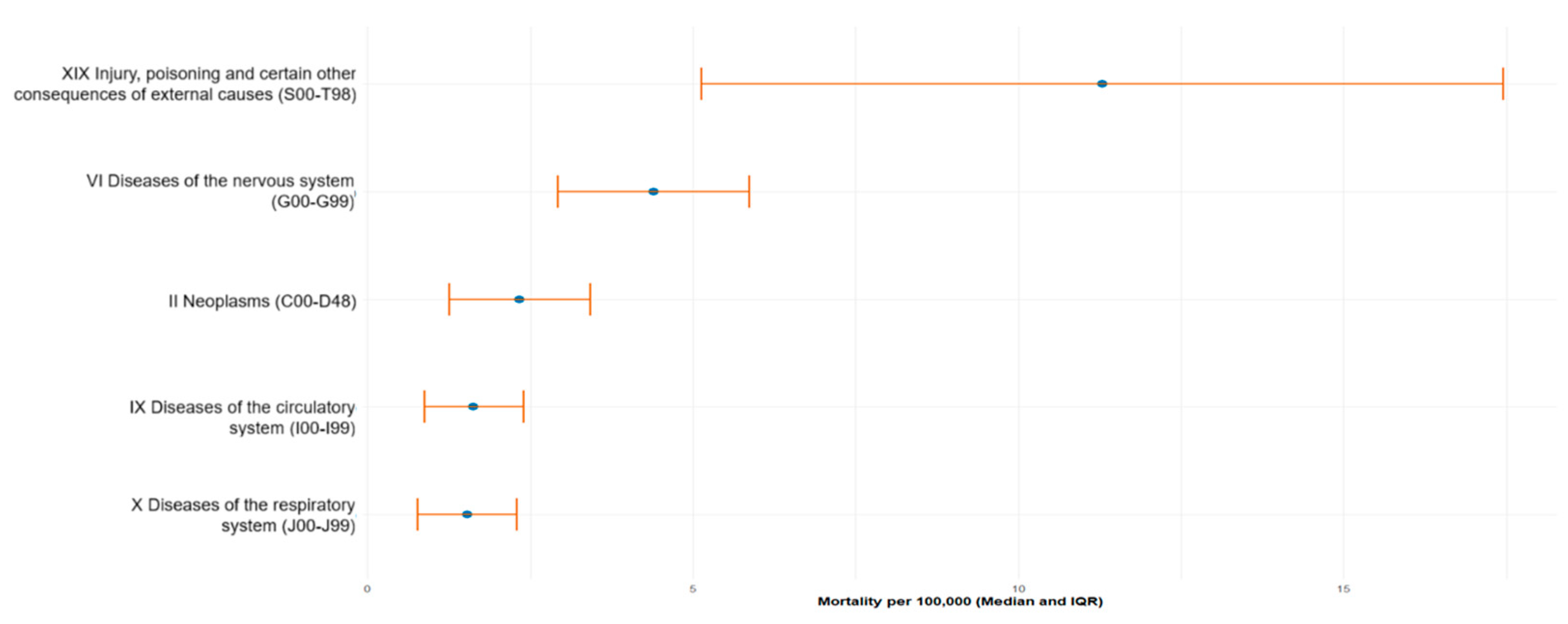
- Across the entire study period, the leading contributors to school-age mortality were Injury, poisoning and certain other consequences of external causes (ICD-10: S00–T98), followed by diseases of the nervous system, neoplasms, circulatory diseases and respiratory diseases; the overall cause pattern was stable over time and largely similar between regions.
- Although mortality levels differed between regions, the contribution of geography was minimal (ICC < 1%), indicating weak regional heterogeneity. The highest mortality rates from external causes were observed in Ulytau, Zhetysu, Zhambyl, Pavlodar and Kostanay regions.
- Poverty levels and gross regional product (GRP) per capita were low and relatively stable across all regions, whereas dietary indicators varied substantially. However, in multivariable models none of the socioeconomic or dietary predictors showed a statistically significant association with mortality among children aged 6–17 years (all p > 0.05).
- Residual autocorrelation and heteroscedasticity pointed to the panel nature of the data and likely non-linear temporal dynamics, resulting in low explanatory power of the models (marginal R2 = 1.7%) and underscoring the limitations of simple linear mixed-effects specifications for this outcome.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Navarro-Jimenez, E.; Saturno-Hernández, P.; Jaramillo-Mejía, M.; Clemente-Suárez, V.J. Amenable Mortality in Children under 5: An Indicator for Identifying Inequalities in Healthcare Delivery: A Review. Children 2024, 11, 764. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Villavicencio, F.; Yeung, D.; Perin, J.; Lopez, G.; Strong, K.L.; Black, R.E. National, Regional, and Global Causes of Mortality in 5–19-Year-Olds from 2000 to 2019: A Systematic Analysis. Lancet Glob. Health 2022, 10, e337–e347. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Estimates. World Health Organization Website. Available online: https://www.who.int/data/global-health-estimates (accessed on 4 December 2025).
- GBD 2019 Adolescent Mortality Collaborators. Global, Regional, and National Mortality Among Young People Aged 10–24 Years, 1950–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2021, 398, 1593–1618. [Google Scholar] [CrossRef]
- Zakharov, M.V.; Fedulova, M.V.; Pigolkin, Y.I. Sudden Death in School-Aged Children at Physical Exercise: Forensic Diagnosis. Sud.-Med. Ekspert. 2021, 64, 64–67. (In Russian) [Google Scholar] [CrossRef]
- Miller, T.L.; Neri, D.; Extein, J.; Somarriba, G.; Strickman-Stein, N. Nutrition in Pediatric Cardiomyopathy. Prog. Pediatr. Cardiol. 2007, 24, 59–71. [Google Scholar] [CrossRef]
- Dasgupta, S.; Aly, A.M. Dilated Cardiomyopathy Induced by Chronic Starvation and Selenium Deficiency. Case Rep. Pediatr. 2016, 2016, 8305895. [Google Scholar] [CrossRef]
- Shimada, B.K.; Alfulaij, N.; Seale, L.A. The Impact of Selenium Deficiency on Cardiovascular Function. Int. J. Mol. Sci. 2021, 22, 10713. [Google Scholar] [CrossRef]
- Benstoem, C.; Goetzenich, A.; Kraemer, S.; Borosch, S.; Manzanares, W.; Hardy, G.; Stoppe, C. Selenium and Its Supplementation in Cardiovascular Disease—What Do We Know? Nutrients 2015, 7, 3094–3118. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific Opinion on Dietary Reference Values for Selenium. EFSA J. 2014, 12, 3846. [CrossRef]
- Speakman, A.; Kaul, A.; Chin, C.; Xanthakos, S.; Mouzaki, M. Malnutrition-Related Cardiomyopathy in a Pediatric Patient with Autism Spectrum Disorder. JPGN Rep. 2025, 6, 39–42. [Google Scholar] [CrossRef] [PubMed]
- World Bank. Poverty and Shared Prosperity 2022: Correcting Course; World Bank: Washington, DC, USA, 2022. Available online: https://www.worldbank.org/en/publication/poverty-and-shared-prosperity (accessed on 13 November 2025).
- Chulanova, Z.; Brimbetova, N.; Satybaldin, A.; Zhanegizova, A. Poverty in Kazakhstan Regions: Assessment of the Impact of Key Indicators on Differences in Its Level. Sustainability 2024, 16, 6752. [Google Scholar] [CrossRef]
- Kagoye, S.; Konje, E.T.; Todd, J.; Mangya, K.; Urassa, M.; Maiga, A.; Marston, M.; Boerma, T. Levels, Trends, and Inequalities in Mortality among Adolescents Aged 5–19 Years in Tanzania: Evidence from the Magu Health and Demographic Surveillance System, 1995–2022. J. Glob. Health 2024, 14, 04124. [Google Scholar] [CrossRef] [PubMed]
- Faruk, M.O.; Zahangir, M.S.; Akhter, S.; Prome, J.F.; Akter, N.; Tasnim, J. A Review of the Impact of Socio-Economic, Demographic and Cultural Factors on Child Mortality. Discov. Public Health 2025, 22, 141. [Google Scholar] [CrossRef]
- Christian, P.; Smith, E.R. Adolescent Undernutrition: Global Burden, Physiology, and Nutritional Risks. Ann. Nutr. Metab. 2018, 72, 316–328. [Google Scholar] [CrossRef] [PubMed]
- Anand, S.S.; Hawkes, C.; de Souza, R.J.; Mente, A.; Dehghan, M.; Nugent, R.; Zulyniak, M.A.; Weis, T.; Bernstein, A.M.; Krauss, R.M.; et al. Food Consumption and Its Impact on Cardiovascular Disease: Importance of Solutions Focused on the Globalized Food System. A Report from the Workshop Convened by the World Heart Federation. J. Am. Coll. Cardiol. 2015, 66, 1590–1614. [Google Scholar] [CrossRef]
- Espinoza-Salas, S.; Gonzalez-Arias, M. Nutrition: Micronutrient Intake, Imbalances, and Interventions. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK597352/ (accessed on 13 November 2025).
- Jo, U.; Park, K. Carbohydrate Intake and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Studies. Nutrients 2023, 15, 1740. [Google Scholar] [CrossRef]
- World Health Organization. Social Determinants of Health; World Health Organization: Geneva, Switzerland. Available online: https://www.who.int/health-topics/social-determinants-of-health (accessed on 13 November 2025).
- Marmot, M.; Wilkinson, R.G. (Eds.) Social Determinants of Health, 2nd ed.; Oxford University Press: Oxford, UK, 2005. [Google Scholar] [CrossRef]
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health; Social Determinants of Health Discussion Paper 2 (Policy and Practice); World Health Organization: Geneva, Switzerland, 2010. Available online: https://apps.who.int/iris/handle/10665/44489 (accessed on 13 November 2025).
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO); World Bank Group. Levels and Trends in Child Malnutrition: UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2023 Edition; World Health Organization: Geneva, Switzerland, 2023. Available online: https://iris.who.int/server/api/core/bitstreams/ccd825e2-e6d0-4101-bedd-8189355dcd81/content (accessed on 13 November 2025).
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and Child Nutrition Study Group. Maternal and Child Undernutrition and Overweight in Low-Income and Middle-Income Countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- World Health Organization. Poverty and Health. World Health Organization Website. 2019. Available online: https://iris.who.int/server/api/core/bitstreams/5b9620a5-43b2-4a70-ad25-3c824b79aded/content (accessed on 13 November 2025).
- United Nations Development Programme (UNDP). Human Development Report 2021/2022: Uncertain Times, Unsettled Lives—Shaping Our Future in a Transforming World; United Nations Development Programme: New York, NY, USA, 2022; Available online: https://hdr.undp.org (accessed on 13 November 2025).
- Yoshikawa, H.; Aber, J.L.; Beardslee, W.R. The Effects of Poverty on the Mental, Emotional, and Behavioral Health of Children and Youth. Am. Psychol. 2012, 67, 272–284. [Google Scholar] [CrossRef]
- Siddiqui, F.; Salam, R.A.; Lassi, Z.S.; Das, J.K. The Intertwined Relationship Between Malnutrition and Poverty. Front. Public Health 2020, 8, 453. [Google Scholar] [CrossRef]
- Nandy, S.; Irving, M.; Gordon, D.; Subramanian, S.V.; Smith, G.D. Poverty, Child Undernutrition and Morbidity: New Evidence from India. Bull World Health Organ. 2005, 83, 210–216. [Google Scholar] [PubMed]
- Government of the Republic of Kazakhstan. Education in Kazakhstan; GOV.KZ—Unified Platform of Internet Resources of Government Agencies. Available online: https://www.gov.kz/article/128171?lang=ru (accessed on 4 December 2025). (In Russian)
- World Health Organization (WHO). Adolescent Health. Available online: https://www.who.int/health-topics/adolescent-health (accessed on 13 November 2025).
- United Nations Children’s Fund (UNICEF). Child and Youth Mortality Age 5–24 Years. UNICEF Data, 2025. Available online: https://data.unicef.org/topic/child-survival/child-and-youth-mortality-age-5-24/ (accessed on 13 November 2025).
- World Health Organization (WHO). Older Children and Young Adolescent Mortality (5 to 14 Years). World Health Organization: Geneva, Switzerland, 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/older-children-and-young-adolescent-mortality-(5-to-14-years) (accessed on 4 December 2025).
- World Health Organization (WHO). Children: Improving Survival and Well-Being. Fact Sheet. World Health Organization: Geneva, Switzerland, 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality (accessed on 13 November 2025).
- United Nations Children’s Fund (UNICEF). Feeding Profit: How Food Environments Are Failing Children—Data Tables. UNICEF: New York, NY, USA, 2025. Available online: https://data.unicef.org/wp-content/uploads/2025/09/CNR-2025-Feeding-Profit-Data-Tables-English-FINAL.pdf (accessed on 17 December 2025).
- Choedon, T.; Brennan, E.; Joe, W.; Lelijveld, N.; Huse, O.; Zorbas, C.; Backholer, K.; Murira, Z.; Wrottesley, S.V.; Sethi, V. Nutritional Status of School-Age Children (5–19 Years) in South Asia: A Scoping Review. Matern. Child Nutr. 2024, 20, e13607. [Google Scholar] [CrossRef]
- Miropolskaia, K.Y.; Kochubei, A.V.; Vershinina, M.G.; Cherniakhovskii, O.B. Pishchevye Predpochteniya Detei Shkol’nogo Vozrasta [Food Preferences of School-Age Children]. Russ. Pediatr. J. 2024, 27, 367–372. (In Russian) [Google Scholar] [CrossRef]
- Punuh, M.I.; Rahayu, H.A.; Mandagi, C. Energy Intake, Household Food Security and Stunting in Toddlers at the Health Center of Molibagu, South Bolaang Mongondow Regency. Int. J. Community Med. Public Health 2025, 12, 2460–2464. [Google Scholar] [CrossRef]
- Islam, B.; Ibrahim, T.I.; Wang, T.; Wu, M.; Qing, J. Current Trends in Household Food Security, Dietary Diversity and Stunting among Children under Five Years in Asia: A Systematic Review. J. Glob. Health 2025, 15, 04049. [Google Scholar] [CrossRef] [PubMed]
- Carbone, A.S.; Roscioli, F.; Mazziotta, M. Urban Food Insecurity and Child Undernutrition in Luanda, Angola. Front. Public Health 2025, 13, 1604713. [Google Scholar] [CrossRef]
- Bureau of National Statistics. Food Consumption in Households of the Republic of Kazakhstan (II Quarter 2024); Bureau of National Statistics of the Agency for Strategic Planning and Reforms of the Republic of Kazakhstan: Astana, Kazakhstan, 2024. Available online: https://stat.gov.kz/ru/industries/labor-and-income/stat-life/publications/184040/ (accessed on 13 November 2025). (In Russian)
- Eurostat. Eurostat Main Page; Eurostat: Luxembourg, 2025. Available online: https://ec.europa.eu/eurostat/web/main/home (accessed on 13 November 2025).
- Dokova, K.G.; Pancheva, R.Z.; Usheva, N.V.; Haralanova, G.A.; Nikolova, S.S.; Kostadinova, T.I.; Rodrigues, C.E.; Singh, J.; Illner, A.-K.; Aleksandrova, K. Nutrition Transition in Europe: East–West Dimensions in the Last 30 Years—A Narrative Review. Front. Nutr. 2022, 9, 919112. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.X.; Samake, Y.; Tolo, O.; Treleaven, E.; Poudiougou, B.; Whidden, C.; Johnson, A.; Kayentao, K.; Boettiger, D.C. Mortality among 5 to 19-year-olds in rural Mali. PLOS Glob. Public Health 2025, 5, e0004172. [Google Scholar] [CrossRef] [PubMed]
- Alabi, O.; Doctor, H.V.; Afenyadu, G.Y.; Findley, S.E. Spatial Analysis of Under-Five Mortality Clustering in Northern Nigeria: Nahuche Health and Demographic Surveillance System. Int. J. Trop. Dis. Health 2016, 15, 1–17. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Study 2019 (GBD 2019) Results. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 4 December 2025).
- Ogunniyi, A.I.; Omotayo, A.O.; Olagunju, K.O.; Rufai, M.A.; Salman, K.K.; Omotayo, O.P.; Oyediran, B.; Adejoorin, M.V. Evaluating the Role of Households’ Food Security Status and Socioeconomic Determinants on Child Mortality in Nigeria. Child Indicators Research 2024, 17, 1687–1714. [Google Scholar] [CrossRef]
- Robinson, W.S. Ecological Correlations and the Behavior of Individuals. Am. Sociol. Rev. 1950, 15, 351–357. [Google Scholar] [CrossRef]
- King, G. A Solution to the Ecological Inference Problem: Reconstructing Individual Behavior from Aggregate Data; Princeton University Press: Princeton, NJ, USA, 1997. [Google Scholar]
- Subramanian, S.V.; O’Malley, A.J.; Kawachi, I. Health Inequalities and the Ecological Fallacy. Am. J. Public Health 2009, 99, 206–212. [Google Scholar]
- Morgenstern, H. Ecologic Studies in Epidemiology: Concepts, Principles, and Methods. Annu. Rev. Public Health 1995, 16, 61–81. [Google Scholar] [CrossRef] [PubMed]
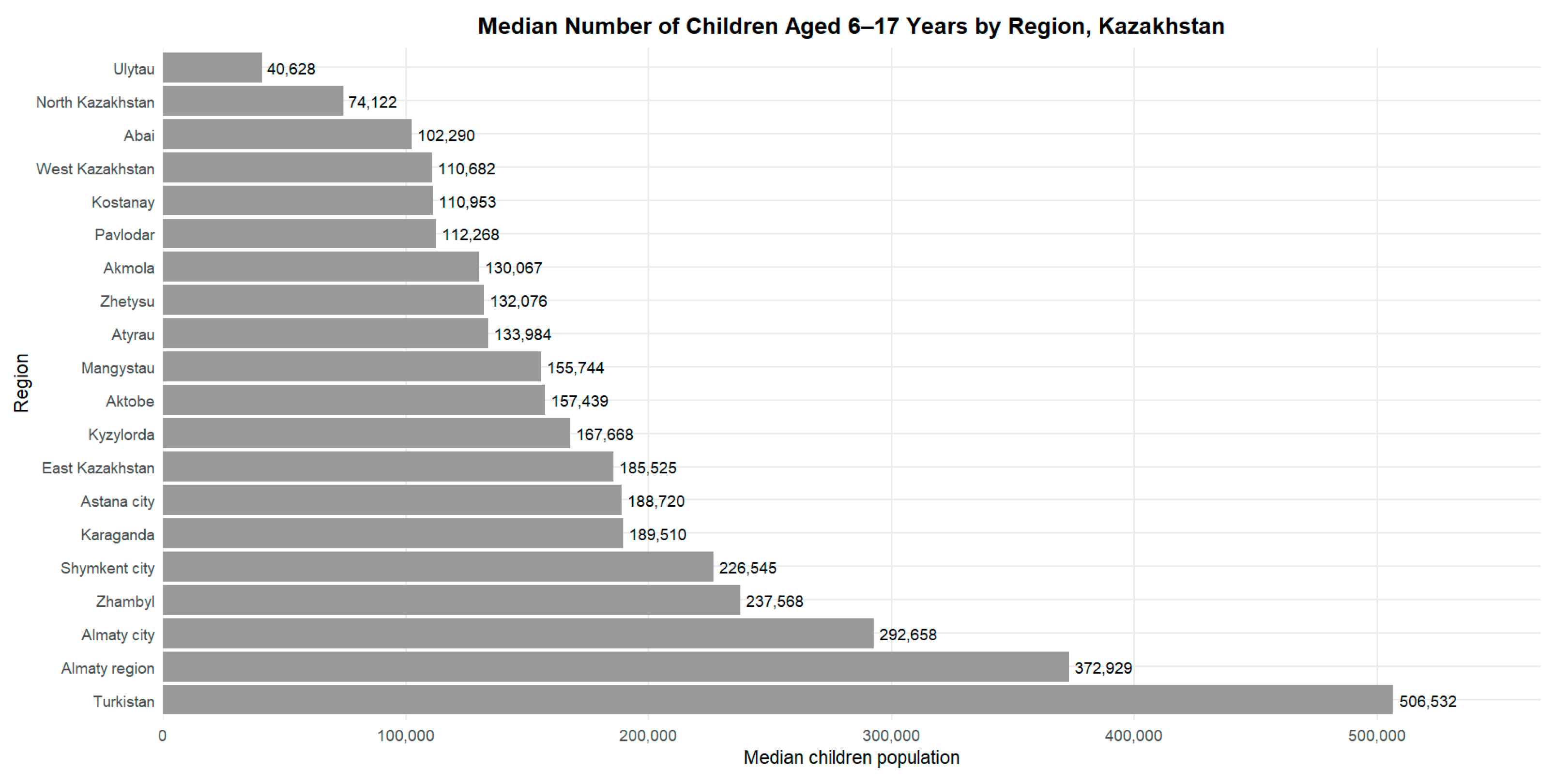
| Region | Median Number of Children, n (IQR) |
| Abai | 102,290 (101,480–102,494) |
| Akmola | 130,067 (120,304–137,949) |
| Aktobe | 157,439 (137,217–175,159) |
| Almaty city | 292,658 (253,952–331,436) |
| Almaty region | 372,929 (355,152–414,560) |
| Astana city | 188,720 (148,959–238,189) |
| Atyrau | 133,984 (117,844–144,528) |
| East Kazakhstan | 185,525 (101,805–192,794) |
| Karaganda | 189,510 (175,974–203,293) |
| Kostanay | 110,953 (105,897–114,715) |
| Kyzylorda | 167,668 (149,293–180,626) |
| Mangystau | 155,744 (129,906–175,795) |
| North Kazakhstan | 74,122 (72,622–75,171) |
| Pavlodar | 112,268 (100,942–116,206) |
| Shymkent city | 226,545 (200,275–251,596) |
| Turkistan | 506,532 (469,110–521,723) |
| Ulytau | 40,628 (39,481–41,218) |
| West Kazakhstan | 110,682 (100,198–119,580) |
| Zhambyl | 237,568 (217,602–246,293) |
| Zhetysu | 132,076 (130,965–133,353) |
| ICD-10 Code | Me (Q1–Q3) |
| XIX Injury, poisoning and certain other consequences of external causes (S00–T98) | 11.29 [5.13–17.45] |
| VI Diseases of the nervous system (G00–G99) | 4.39 [2.92–5.87] |
| II Neoplasms (C00–D48) | 2.34 [1.26–3.42] |
| IX Diseases of the circulatory system (I00–I99) | 1.63 [0.87–2.4] |
| X Diseases of the respiratory system (J00–J99) | 1.53 [0.77–2.29] |
| Region | Bread (kg per Capita per Year) | Meat (kg per Capita per Year) | Fish (kg per Capita per Year) | Milk (L per Capita per Year) | Eggs (Pieces per Capita per Year) | Oils (kg per Capita per Year) | Fruits (kg per Capita per Year) | Vegetables (kg per Capita per Year) | Potatoes (kg per Capita per Year) | Sugar (kg per Capita per Year) | GRP |
| Abai | 123.2 (120.6–124.3) | 72.1 (66.3–72.6) | 12.5 (11.9–12.6) | 227.5 (216.5–244.3) | 186.6 (169.3–191.5) | 14.1 (13.3–14.3) | 53.9 (50.2–55.7) | 56.3 (54.2–57.8) | 29.6 (28.7–30.7) | 35.9 (32.3–39.9) | 2,505,040 (2,246,826–2,781,901) |
| Akmola | 135.0 (127.7–147.0) | 92.0 (74.2–93.3) | 17.3 (10.1–18.6) | 285.1 (262.5–314.0) | 248.7 (237.6–255.0) | 20.5 (19.4–22.1) | 69.7 (53.2–77.1) | 68.4 (66.1–72.2) | 51.0 (49.0–54.3) | 46.0 (41.3–50.7) | 2,108,760 (1,552,704–3,484,573) |
| Aktobe | 128.0 (120.9–128.9) | 72.6 (67.4–74.9) | 11.7 (8.8–12.0) | 226.3 (210.0–247.3) | 164.4 (160.0–172.0) | 16.5 (15.7–18.4) | 73.2 (70.3–75.7) | 65.5 (61.8–71.9) | 46.0 (42.6–49.0) | 42.8 (41.0–43.6) | 2,965,647 (2,341,889–4,187,588) |
| Almaty city | 103.8 (103.4–110.8) | 84.9 (82.1–89.0) | 14.5 (11.4–15.3) | 265.1 (261.5–290.5) | 221.2 (208.2–228.9) | 17.9 (15.8–19.3) | 90.8 (78.9–97.8) | 97.6 (95.4–99.4) | 44.7 (44.0–46.7) | 44.3 (42.3–47.1) | 13,503,381 (11,893,226–19,154,537) |
| Almaty region | 148.4 (134.5–153.0) | 87.9 (79.3–92.8) | 13.6 (12.0–14.7) | 226.0 (212.3–247.5) | 190.1 (156.0–193.1) | 14.0 (13.1–15.1) | 71.6 (68.8–74.0) | 90.6 (77.9–98.1) | 42.4 (41.7–44.1) | 45.9 (43.4–46.9) | 3,312,907 (2,472,042–4,267,665) |
| Astana city | 105.3 (102.6–106.7) | 73.3 (70.8–80.7) | 11.7 (8.0–12.4) | 264.1 (250.4–272.1) | 215.6 (186.6–228.0) | 13.1 (11.7–15.5) | 83.2 (69.3–89.9) | 76.7 (72.8–81.5) | 46.4 (45.2–46.9) | 36.0 (34.6–37.1) | 7,905,056 (5,775,621–10,672,481) |
| Atyrau | 129.5 (126.2–136.5) | 90.3 (87.2–93.6) | 19.0 (18.4–19.0) | 238.5 (192.4–242.2) | 170.8 (161.4–175.0) | 16.3 (14.6–20.8) | 64.6 (58.9–66.9) | 69.6 (66.8–78.2) | 46.4 (41.3–48.5) | 39.9 (36.2–46.4) | 8,573,038 (5,947,654–13,725,400) |
| East Kazakhstan | 138.5 (120.5–141.5) | 87.8 (86.4–90.3) | 19.2 (13.5–19.5) | 289.1 (276.1–294.9) | 217.2 (186.7–224.4) | 16.2 (15.7–21.1) | 73.2 (58.2–75.0) | 73.1 (66.8–88.9) | 49.1 (42.9–50.7) | 41.8 (41.3–43.9) | 3,753,075 (3,174,813–4,459,056) |
| Karaganda | 125.5 (111.7–133.6) | 86.5 (79.8–92.2) | 14.2 (10.0–15.8) | 275.3 (262.6–291.4) | 247.8 (220.2–270.0) | 22.4 (18.9–23.4) | 83.0 (64.7–88.3) | 80.6 (71.0–89.2) | 59.9 (50.7–60.8) | 47.2 (45.7–50.2) | 5,728,809 (4,284,363–7,278,059) |
| Kostanay | 119.3 (117.4–122.3) | 76.2 (69.2–82.2) | 17.6 (12.4–19.2) | 210.2 (201.5–219.4) | 240.9 (194.8–253.4) | 17.3 (16.7–19.7) | 64.0 (54.6–70.0) | 79.5 (78.4–83.4) | 52.1 (47.1–54.6) | 40.8 (39.2–43.0) | 2,661,973 (1,850,281–4,182,078) |
| Kyzylorda | 142.0 (133.2–151.2) | 63.8 (61.9–65.2) | 16.0 (12.7–16.0) | 189.0 (184.1–205.6) | 146.6 (122.7–153.8) | 17.9 (15.3–21.4) | 76.4 (72.1–80.1) | 84.6 (77.1–87.1) | 42.7 (42.1–43.3) | 42.5 (39.5–47.4) | 1,737,941 (1,430,980–2,417,399) |
| Mangystau | 107.0 (102.0–116.4) | 84.1 (81.7–87.1) | 9.6 (8.7–10.2) | 229.2 (203.5–239.7) | 128.5 (127.3–130.5) | 18.1 (18.1–18.2) | 85.6 (80.2–89.4) | 81.7 (74.9–83.9) | 51.2 (46.8–51.8) | 38.3 (37.2–39.8) | 3,656,196 (3,074,393–4,401,193) |
| North Kazakhstan | 119.2 (111.7–121.5) | 76.9 (69.8–80.1) | 20.2 (15.6–21.2) | 247.4 (240.1–248.3) | 238.1 (216.3–252.4) | 15.2 (14.5–18.1) | 73.8 (57.9–76.4) | 68.0 (60.6–74.7) | 48.7 (47.3–50.5) | 40.8 (37.8–42.5) | 1,477,113 (1,113,959–2,198,854) |
| Pavlodar | 128.4 (122.2–137.5) | 87.5 (81.6–90.2) | 13.9 (13.3–14.5) | 281.8 (254.3–302.1) | 187.2 (177.2–192.4) | 16.7 (16.6–17.6) | 69.5 (65.1–73.0) | 84.9 (78.0–89.7) | 53.9 (51.2–55.6) | 42.3 (36.9–45.4) | 3,074,873 (2,369,298–4,296,924) |
| Shymkent city | 133.8 (127.6–157.1) | 54.5 (53.1–58.2) | 5.4 (4.9–8.8) | 165.7 (155.7–208.0) | 165.4 (163.2–182.0) | 13.2 (12.9–16.5) | 65.2 (60.3–66.6) | 88.6 (82.9–106.9) | 44.5 (38.7–48.1) | 33.7 (32.5–37.7) | 2,348,099 (1,712,054–3,294,392) |
| Turkistan | 172.3 (164.9–173.3) | 61.5 (58.2–62.5) | 12.4 (8.9–12.5) | 213.2 (208.6–228.9) | 166.1 (149.0–166.6) | 19.0 (17.2–21.3) | 68.2 (66.6–70.8) | 108.1 (101.7–110.0) | 44.3 (43.3–45.6) | 42.4 (41.9–43.3) | 2,200,140 (1,475,670–3,517,281) |
| Ulytau | 119.0 (113.5–120.5) | 80.8 (77.1–82.1) | 11.8 (10.8–11.9) | 254.0 (247.7–255.1) | 229.9 (215.8–237.9) | 21.8 (20.3–22.9) | 75.7 (66.6–75.9) | 70.2 (63.2–72.2) | 45.7 (42.9–47.5) | 59.0 (52.6–60.6) | 1,789,734 (1,551,534–2,099,195) |
| West Kazakhstan | 136.0 (125.4–142.1) | 79.2 (69.9–84.1) | 15.3 (13.3–18.0) | 226.5 (224.7–247.3) | 165.7 (146.6–187.5) | 19.2 (18.5–20.6) | 69.2 (57.6–73.7) | 78.0 (74.3–82.4) | 54.6 (47.8–57.3) | 38.0 (36.4–39.9) | 2,868,525 (2,337,506–4,435,131) |
| Zhambyl | 137.7 (126.6–141.6) | 74.5 (68.3–84.1) | 13.7 (12.1–14.6) | 228.0 (199.1–236.8) | 169.0 (126.0–180.6) | 17.9 (16.8–20.0) | 72.6 (58.8–76.0) | 86.2 (81.5–90.5) | 47.5 (46.2–48.1) | 44.4 (40.1–45.9) | 1,807,134 (1,350,662–2,685,460) |
| Zhetysu | 141.7 (141.3–149.6) | 93.4 (93.2–97.2) | 14.0 (13.1–14.5) | 244.1 (234.9–254.5) | 155.0 (151.2–155.2) | 13.7 (13.3–14.1) | 74.0 (70.1–75.2) | 85.5 (84.1–87.5) | 39.3 (38.9–41.5) | 48.1 (45.5–48.3) | 1,618,150 (1,376,926–1,914,049) |
| Region | Poverty Level, Median (Q1–Q3), % |
|---|---|
| Abai | 0.2 (0.1–0.6) |
| Akmola | 0.2 (0.2–0.4) |
| Aktobe | 0.1 (0.1–0.1) |
| Almaty city | 0.1 (0.1–0.2) |
| Almaty region | 0.1 (0.1–0.2) |
| Astana city | 0.1 (0.1–0.1) |
| Atyrau | NA |
| East Kazakhstan | 0.4 (0.2–0.4) |
| Karaganda | 0.2 (0.1–0.2) |
| Kostanay | 0.1 (0.1–0.2) |
| Kyzylorda | 0.1 (0.1–0.1) |
| Mangystau | 0.2 (0.1–0.4) |
| North Kazakhstan | 0.2 (0.1–0.6) |
| Pavlodar | 0.0 (0.0–0.0) |
| Shymkent city | 0.3 (0.1–0.7) |
| Turkistan | 0.2 (0.1–0.2) |
| Ulytau | 0.6 (0.5–0.6) |
| West Kazakhstan | 0.2 (0.1–0.3) |
| Zhambyl | 0.1 (0.1–0.1) |
| Zhetysu | 0.2 (0.1–0.8) |
| Predictor | β Estimate | 95% CI | p-Value |
| Bread & cereal products | −0.017 | −0.035 to +0.009 | 0.062 |
| Meat and meat products | −0.024 | −0.061 to +0.013 | 0.204 |
| Fish and seafood | −0.022 | −0.119 to +0.075 | 0.637 |
| Milk and dairy products | −0.001 | −0.014 to +0.011 | 0.891 |
| Eggs | +0.002 | −0.009 to +0.013 | 0.758 |
| Oils and fats | −0.108 | −0.226 to +0.010 | 0.072 |
| Fruits | −0.021 | −0.052 to +0.010 | 0.195 |
| Vegetables | +0.000 | −0.027 to +0.028 | 0.993 |
| Potato | +0.018 | −0.040 to +0.075 | 0.537 |
| Sugar and confectionery | +0.031 | −0.035 to +0.098 | 0.335 |
| Poverty | +0.631 | −0.576 to +1.838 | 0.305 |
| Year | +0.094 | −0.045 to +0.232 | 0.180 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Yelzhanova, Z.; Nurlan, J.; Kamalieva, M.; Zhubanysheva, K.; Tursun, A. Nutrition and Social Disadvantage as Risk Factors for Mortality Among School-Age Children: Regional Differences in Kazakhstan. Int. J. Environ. Res. Public Health 2026, 23, 39. https://doi.org/10.3390/ijerph23010039
Yelzhanova Z, Nurlan J, Kamalieva M, Zhubanysheva K, Tursun A. Nutrition and Social Disadvantage as Risk Factors for Mortality Among School-Age Children: Regional Differences in Kazakhstan. International Journal of Environmental Research and Public Health. 2026; 23(1):39. https://doi.org/10.3390/ijerph23010039
Chicago/Turabian StyleYelzhanova, Zulfiya, Jainakbayev Nurlan, Madina Kamalieva, Karlygash Zhubanysheva, and Anna Tursun. 2026. "Nutrition and Social Disadvantage as Risk Factors for Mortality Among School-Age Children: Regional Differences in Kazakhstan" International Journal of Environmental Research and Public Health 23, no. 1: 39. https://doi.org/10.3390/ijerph23010039
APA StyleYelzhanova, Z., Nurlan, J., Kamalieva, M., Zhubanysheva, K., & Tursun, A. (2026). Nutrition and Social Disadvantage as Risk Factors for Mortality Among School-Age Children: Regional Differences in Kazakhstan. International Journal of Environmental Research and Public Health, 23(1), 39. https://doi.org/10.3390/ijerph23010039





