1. Introduction
The mental health of nursing professionals has emerged as a growing global concern, especially when considering the challenging working conditions to which these professionals are frequently exposed. In a worldwide scenario where the demand for healthcare services is constant and, at times, overwhelming, physical and emotional overload has become an intrinsic reality in these workers’ routines. Nursing practice is commonly performed under conditions that may be inadequate, with hierarchical relationships that are sometimes conflictual, factors that significantly contribute to occupational stress and, consequently, to physical and emotional exhaustion [
1,
2,
3,
4]. Specifically in Brazil, nursing professionals often operate within a public healthcare system (Sistema Único de Saúde—SUS) characterized by high patient volumes, limited resources, and intense pressure to deliver care efficiently despite systemic constraints [
5]. These particularities of the Brazilian work environment exacerbate the existing global challenges, leading to unique stressors that impact the mental well-being of nurses [
6]. The physiological response to these stressors can be effectively understood through Hans Selye’s General Adaptation Syndrome (GAS), a model positing that chronic exposure to extreme demands may lead to the exhaustion phase, thereby undermining the organism’s sustainable coping capacity [
7]. These factors, combined with excessive working hours and constant pressure, result in high rates of absenteeism and deterioration in the quality of life (QoL) of these individuals [
8,
9,
10].
Engagement with patients in critical situations, in inpatient units or emergency departments, exposes nursing professionals to a particularly intense level of physical and psychological stress. According to the Job Demands-Resources (JD-R) Model, nursing is characterized by high job demands—such as the ‘requirement for significant physical exertion,’ the need to ‘stand for long periods,’ and a ‘fast-paced work rhythm’—which, in the absence of adequate resources, can lead to exhaustion [
11]. Emergency departments, for example, are described as physically and psychologically overwhelming environments, making nursing staff more susceptible to emotional exhaustion and at risk of developing traumatic stress [
12]. This exhaustion constitutes a core component of burnout, which further encompasses depersonalization and diminished personal accomplishment [
13]. These symptoms collectively underscore the challenge of sustaining engagement and high-quality care within an environment of persistent pressure. The requirement for significant physical effort, such as standing for long periods, repetitive use of hands, and manual labor, combined with an accelerated work pace and time pressure, contributes to a high prevalence of musculoskeletal pain and other physical problems [
14,
15,
16]. Furthermore, coping with pain, suffering, and death, team anxiety, and rigid work routines add complex layers to daily stress, directly impacting the quality of life and mental well-being of these professionals [
17].
In this context, mental health and quality of life are conceptualized through the lens of the Biopsychosocial Model, which posits health and illness as outcomes of a complex interplay among biological, psychological, and social factors [
18]. This implies that nurses’ working conditions and personal experiences not only influence their psychological state but can also manifest profound biological correlates. The Quality of Life (QoL), defined as the individual’s subjective perception of their position in life, considering the cultural and value context, their goals, expectations, standards, and concerns, is a crucial element [
19]. Although measuring QoL is complex, instruments such as WHOQOL-BREF, a widely validated abbreviated version of WHOQOL-100, allow for the assessment of the impact of various conditions on an individual’s life, covering physical, psychological, social relationships, and environmental domains [
20,
21]. Recent studies, including the research that underpins this manuscript, have revealed that nursing professionals frequently exhibit levels of quality of life that indicate dissatisfaction, which is a direct reflection of the demands of their profession [
22,
23].
Dissatisfaction with the quality of life and exposure to chronic stressors contribute to the high prevalence of Minor Mental Disorders (MMD) among nursing professionals. MMDs are clinically significant conditions that manifest through alterations in mood, emotions, thinking, and behavior, frequently associated with personal distress or impaired functioning [
24,
25]. Symptoms such as forgetfulness, fatigue, depression, lack of concentration, irritability, and insomnia are common among these professionals [
26]. The nursing staff is, in fact, considered a risk group for MMD-related illness, with nursing assistants, technicians, and nurses ranking among the positions with the highest prevalence and risk of work leave due to these conditions [
27,
28,
29]. The Self-Report Questionnaire (SRQ-20), developed by the World Health Organization (WHO), is an instrument widely used in Brazil to screen for these disorders, demonstrating its relevance in the early identification of MMDs in the professional population [
30,
31].
In contrast to risk factors and minor mental disorders, resilience (R) emerges as an important protective and adaptive factor. Derived from the Latin “resilio,” resilience is defined as the capacity of an individual or group to positively construct or reconstruct themselves, even in the face of adversities and in unfavorable environments [
32,
33]. In the nursing work context, resilience is a continuous process of personal growth and development of potentialities that allow professionals to cope with the exhausting work pace, pressure, and responsibilities, minimizing stressors and promoting well-being [
34,
35,
36]. The capacity for resilience, assessed by scales such as Wagnild & Young’s, is fundamental for these professionals to maintain their mental health and quality of life in such a demanding environment [
37]. Additionally, positive psychology emphasizes resilience as a human strength that enables individuals to thrive in the face of challenges, contributing to well-being and the prevention of psychopathology [
38].
The complexity of these previously discussed interactions, encompassing the relationship between occupational stressors, quality of life, minor mental disorders, and resilience, becomes even more apparent when considering the underlying biological and psychophysiological mechanisms. Chronic occupational stress exposure can lead to dysregulation of the Hypothalamic–Pituitary–Adrenal (HPA) axis, resulting in altered cortisol levels and impacting the Autonomic Nervous System (ANS), with sympathetic nervous system predominance and a consequent reduction in heart rate variability. These biological alterations directly contribute to the symptoms of anxiety, depression, and fatigue observed in Minor Mental Disorders (MMDs). Furthermore, chronic stress can affect neurotransmitter systems (such as serotonin and dopamine) and neural plasticity in brain regions critical for emotional and cognitive regulation, including the prefrontal cortex, amygdala, and hippocampus [
39]. There is also growing evidence that prolonged stress can induce neuroinflammation and oxidative stress, processes that contribute to the pathogenesis of mental disorders and the impairment of quality of life [
40]. Resilience, in turn, is associated with more effective regulation of these biological systems, allowing for a more rapid recovery of homeostasis following stressful events and conferring protection against the deleterious effects of chronic stress.
Given the complexity and the scarce scientific production focused on the relationship between quality of life, minor mental disorders, and resilience, especially in nursing literature, the relevance of this theme is undeniable. Most studies focused on the mental health of nursing professionals tend to concentrate on isolated aspects of suffering or stress, without deepening the interconnection between these constructs and the role of resilience as a crucial protective factor [
41]. Existing research often examines these variables in isolation or in simple bivariate relationships (e.g., resilience and mental health, or quality of life and mental health) [
42,
43]. However, there is a significant gap in studies that integrate resilience and Quality of Life as interacting variables within a comprehensive model to predict MMD. Specifically, previous research has not adequately explored the potential indirect or mediating role of Quality of Life in the relationship between resilience and the development of MMDs. Understanding this dynamic, by integrating psychosocial perspectives and biological mechanisms, is fundamental for developing more effective and targeted interventions, both at the individual and organizational levels, aimed at promoting mental health and preventing illness.
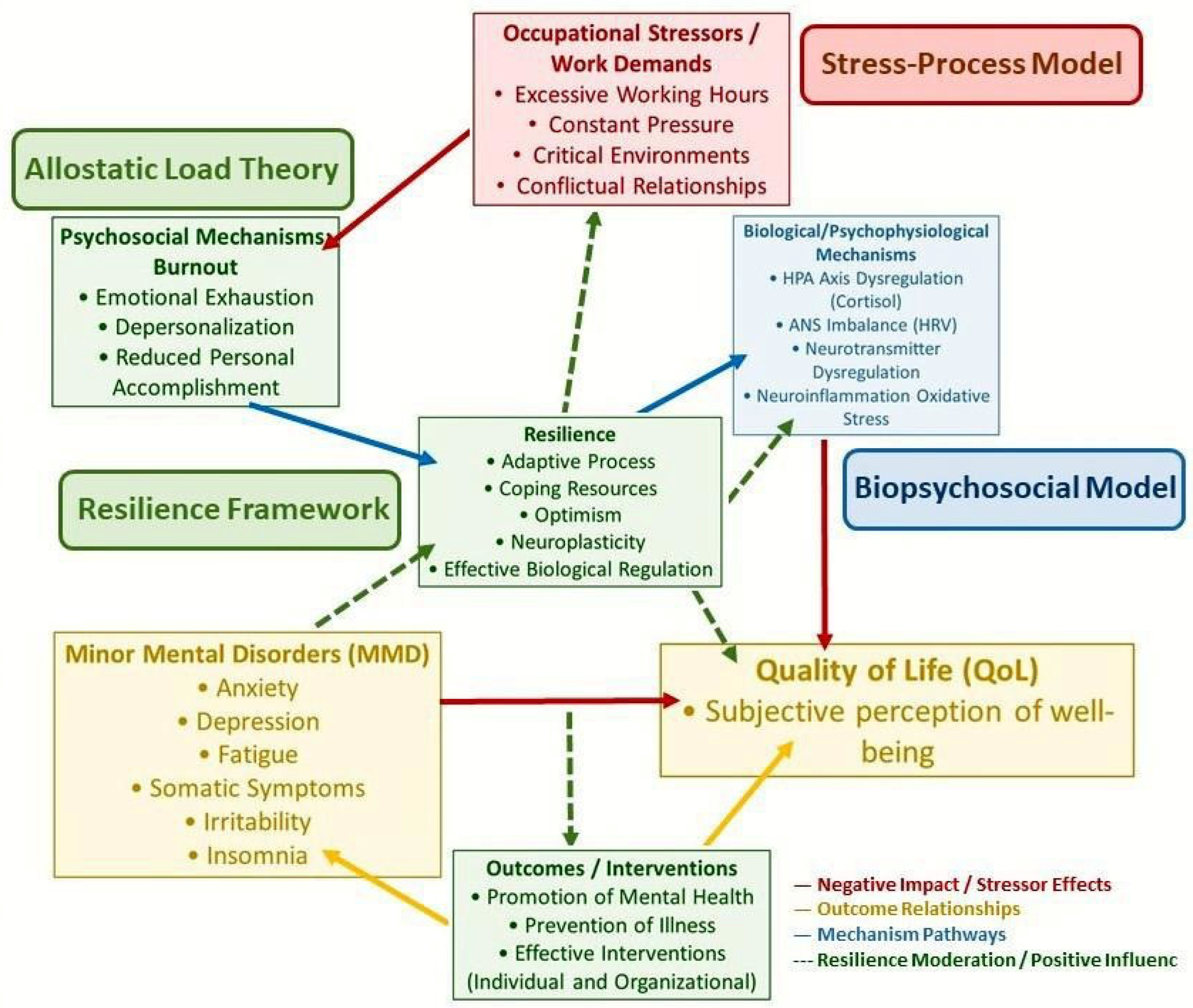
The intricate interplay among occupational stressors, psychosocial and biological mechanisms, Minor Mental Disorders (MMD), Quality of Life (QoL), and the protective role of Resilience, specifically within the context of healthcare professionals, particularly nursing, is illustrated in
Figure 1. This integrated theoretical model hypothesizes specific directional relationships: (a) occupational stressors contribute to MMD through both psychosocial and biological mechanisms; (b) higher Quality of Life directly predicts a reduction in MMD symptoms; and (c) resilience positively influences Quality of Life, thereby indirectly protecting against MMD. This conceptualization positions Quality of Life as a crucial mediator between resilience and mental health outcomes.
Based on this theoretical framework and the identified research gaps, this study proposes the following hypotheses:
H1: Higher levels of Quality of Life will be significantly associated with a lower prevalence and severity of Minor Mental Disorders among nursing professionals [
44].
H2: Resilience will be positively correlated with Quality of Life in nursing professionals [
45].
H3: Resilience will indirectly influence the prevalence and severity of Minor Mental Disorders by enhancing Quality of Life among nursing professionals (e.g., resilient individuals experience better QoL, which in turn reduces MMD symptoms) [
46].
In this scenario, the present study proposes an in-depth investigation. The main objective of this work is to investigate the prevalence of Minor Mental Disorders (MMDs) and levels of resilience among nursing professionals. It also seeks to analyze the relationship between these two constructs and identify the role of resilience as a potential protective factor, contributing to a more holistic understanding of mental health in nursing and to the development of more effective support strategies.
2. Materials and Methods
2.1. Study Design
This is a quantitative study with a descriptive, correlational, and cross-sectional design. The quantitative approach was selected to allow for objective measurement of variables and the application of robust statistical analyses, seeking to identify patterns, relationships, and the prevalence of phenomena. The descriptive character aims to characterize the sample and the attributes of the investigated variables, while the correlational aspect proposes to examine the associations between resilience, quality of life, and dimensions of mental health. The choice of a cross-sectional design implies that data were collected at a single point in time, offering a “snapshot” of the relationships between variables at the moment of collection. It is important to emphasize that, due to its cross-sectional nature, this study allows for the identification of associations but cannot establish direct causal relationships or observe changes over time. This study was conducted and reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (
Supplementary File S1).
2.2. Sample and Context
The study population consisted of nursing professionals (nursing assistants, technicians, and nurses) from Inpatient Units (IUs) and Emergency Departments (EDs) of the public healthcare network and the Base Hospital (BH) in the municipality of São José do Rio Preto, São Paulo, Brazil. The total estimated population was 444 professionals.
The final study sample consisted of 203 nursing professionals. While recognizing the rigorous requirements for a priori sample size estimation using statistical parameters (e.g., means, standard deviations, and desired effect sizes) to ensure adequate statistical power for hypothesis testing, this descriptive and correlational study adopted a comprehensive approach. The primary objective was to investigate the prevalence and relationships of mental health constructs within the entire accessible population of nursing professionals across the selected healthcare institutions. Consequently, the sample size of 203 participants was obtained through a recruitment process that aimed to include all eligible professionals who provided informed consent during the data collection period, representing approximately 45.7% of the total estimated population within these defined settings. This substantial representation from the target population allows for a detailed characterization of the phenomena under investigation and provides a robust basis for exploring correlations within this specific cohort.
The participating healthcare institutions included the Emergency Care Units (UPAs) of the municipality of São José do Rio Preto and the Base Hospital (BH) of the same city.
The UPAs: The municipal health system of São José do Rio Preto has five UPAs (UPA Jaguaré, UPA Santo Antônio, UPA Tangará/Estoril, UPA Região Norte, UPA Vila Toninho), distributed across different regions of the city (São José do Rio Preto (Municipality), 2019). This study included professionals from all five UPAs.
The Base Hospital (BH): It is one of the largest and most important hospital complexes in the State of São Paulo, being a teaching hospital affiliated with the Faculty of Medicine of São José do Rio Preto (FAMERP). The BH serves most of its patients through the Unified Health System (SUS) and serves as a medical reference center for more than two million inhabitants from 102 neighboring municipalities [
47]. It has 708 inpatient beds (including ICUs) and one of the largest emergency services in the interior of São Paulo, with approximately 12,000 monthly consultations, divided into private insurance (EC) and SUS (E-SUS) sectors. From BH, all nine inpatient units and the two emergency departments (EC and E-SUS) were included.
2.3. Data Collection
Data collection occurred between August and October 2019. The project was submitted for review by the Research Ethics Committee (REC) of the Faculty of Medicine of São José do Rio Preto (FAMERP), under Certificate of Presentation for Ethical Appraisal (CAAE) n. 89714418.0.0000.5415, and was approved on 2 July 2018, with opinion n. 2,748,173.
Data were collected after prior scheduling with the nursing managers of the participating sectors and institutions. The researchers explained the study objectives to the managers and provided the data collection instruments and the Informed Consent Forms (ICFs). The managers, in turn, passed the materials to the professionals under their management. To ensure participant anonymity, the ICFs (one version for the respondent and another for the researcher) and the completed instruments were collected in separate sealed envelopes and subsequently delivered to the researchers. Professionals on vacation and/or away from activities, as well as those who did not agree to participate, were excluded from the sample.
2.4. Instruments
Four self-administered instruments were used for data collection:
Sociodemographic and Professional Questionnaire: Developed by the researchers, this closed-question instrument collected information on sex, age, marital status, number of children, family income, professional category, work sector and institution, number of hours worked, number of employment relationships, motivation for accumulating jobs, and work shift. For nurses, it also included academic qualifications (specialization, master’s degree, doctorate). As a descriptive data collection tool, this questionnaire does not require psychometric reliability coefficients in the same manner as psychological scales. While
Figure 1 illustrates a comprehensive theoretical model including occupational stressors, this questionnaire captured specific contextual and professional characteristics (e.g., workload, number of employment relationships) that serve as relevant indicators within that broader framework, rather than directly measuring constructs like burnout.
Quality of Life Assessment Instrument (WHOQOL-BREF): Abbreviated version of WHOQOL-100, developed by The WHOQOL Group (1998) and widely validated for use in various cultures [
19,
20,
48]. It consists of 26 questions, the first two about the general quality of life and satisfaction with health, and the remaining 24 distributed across four domains: Physical, Psychological, Social Relationships, and Environment. Responses range from 1 to 5 (from “not at all satisfied” to “very satisfied”). For analysis, raw scores are transformed to a scale of from 0 to 100. Values below 70 are considered unsatisfactory, and equal to or above 70, satisfactory. Validation studies for WHOQOL-BREF have consistently reported good internal consistency, with Cronbach’s alpha values typically ranging from 0.60 to 0.90 for its domains [
20,
48]. In the current study, the composite reliability was 0.829 for the overall Quality of Life (QoL) factor, 0.561 for Physical, 0.266 for Environmental, and 0.261 for Social. The Psychological factor presented extremely low composite reliability (0.00000983) in our analysis, as detailed in the Results section.
Self-Report Questionnaire (SRQ-20): Developed by the World Health Organization (WHO) for screening minor mental disorders (MMD), this instrument consists of 20 items with dichotomous responses (yes/no) [
49,
50]. Each positive response contributes 1 point to the total score (ranging from 0 to 20). The symptoms are grouped into four categories: depressive/anxious mood, somatic symptoms, decreased vital energy, and depressive thoughts [
51,
52,
53]. The Brazilian version of the SRQ-20 has demonstrated validity and reliability in previous studies [
30,
31,
54]. A total score equal to or greater than eight points on the SRQ-20 was used as a criterion for the diagnosis of MMD, as widely adopted in the literature [
30]. Original validation studies of the SRQ-20 have reported adequate internal consistency, with Cronbach’s alpha values generally above 0.70 [
52,
53]. In this study, the composite reliability for the Decreased Vital Energy (DEV) factor was 0.842, for Depressive–Anxious Mood (HuDA) was 0.739, for Depressive Thoughts (PD) was 0.826, and for Somatic Symptoms (SS) was 0.762.
Wagnild & Young Resilience Scale: This scale, originally developed by Wagnild and Young (1993), assesses the individual’s ability to deal with adversities and maintain well-being [
55]. In Brazil, it was translated and adapted, with its validity and reliability confirmed in studies such as Pesce et al. (2005) and Perim et al. (2015) [
56,
57]. The original scale has 25 items with a 7-point Likert scale (1 = strongly disagree; 7 = strongly agree). Scores range from 25 to 175 points, where higher values indicate greater resilience. In the present study, based on Bayesian confirmatory factor analysis, a 14-item version with collapsed response categories was used, in order to optimize model fit and internal consistency [
58,
59,
60]. A higher score on this scale indicates a higher level of resilience. Validation studies of the Wagnild & Young Resilience Scale have consistently shown high internal consistency, with Cronbach’s alpha values often exceeding 0.90 [
55,
56]. In the current study, the composite reliability for the 14-item collapsed model was 0.860, indicating high internal consistency.
2.5. Data Analysis
Data analysis was divided into three main stages, using advanced statistical approaches to ensure the robustness and accuracy of the results. The analyses were performed using R software 4.4.0 (R Core Team, 2024), with specific packages for statistical modeling [
61]. For clarity, key statistical terms and their interpretations are provided, aiming to make the methodology accessible to a broad readership.
2.5.1. Bayesian Confirmatory Factor Analysis (BCFA)
BCFA was employed to investigate the factorial structure of the SRQ-20, Wagnild & Young Resilience Scale, and WHOQOL-BREF instruments. This approach was selected for its flexibility and robustness in handling ordinal data and moderate sample sizes, generating posterior distributions of parameters [
62,
63,
64,
65,
66,
67]. For BCFA, the Markov Chain Monte Carlo (MCMC) algorithm and the blavaan package in R software were used [
65]. The fit of Bayesian models was evaluated through the posterior predictive
p-value (ppp), Deviance Information Criterion (DIC), Watanabe-Akaike Information Criterion (WAIC), and Leave-One-Out Information Criterion (LOOIC) [
68]. Good model fit in BCFA is typically indicated by a ppp value close to 0.5, lower values for DIC, WAIC, and LOOIC (relative to alternative models), suggesting better predictive accuracy and parsimony.
For the SRQ-20, a model of four correlated factors (Depressive–Anxious Mood, Somatic Symptoms, Decreased Vital Energy, and Depressive Thoughts) was validated [
51,
52,
53].
For the Resilience Scale, models of 14 and 25 items were tested, with and without collapsed response categories. The 14-item model with collapsed categories demonstrated the best balance of fit.
For the WHOQOL-BREF, Hierarchical, Partial Bifactor, and Complete Bifactor models were evaluated. The Complete Bifactor Model proved to be the most adequate in terms of fit, although the psychological factor presented extremely low composite reliability and was not included in subsequent analyses [
69,
70,
71].
2.5.2. Estimation and Transformation of Factor Scores
After validating the factorial structures, factor scores to represent latent variables were calculated from the 2000 posterior distributions of latent variables generated by BCFA [
63,
64]. These factor scores serve as quantitative measures of the underlying psychological constructs. To mitigate the problem of factor score indeterminacy and ensure the preservation of internal correlations between factors, whitening and coloring transformations were applied [
62,
72,
73,
74,
75,
76,
77,
78,
79,
80]. These transformations standardize the scores while maintaining their relational properties, preparing them for subsequent analyses.
2.5.3. Path Analysis Modeling
Path analysis was used to examine the predictive relationships between WHOQOL-BREF domains and Resilience with dimensions of mental health. This analysis was performed using the lavaan package in R software and was based on the 2000 posterior distributions of transformed factor scores [
81]. The quality of fit of the path analysis models was evaluated through indices such as chi-square (χ
2), degrees of freedom (df),
p-value, Comparative Fit Index (CFI), Tucker–Lewis Index (TLI), and Root Mean Square Error of Approximation (RMSEA). A good model fit for path analysis is generally indicated by a non-significant chi-square
p-value (
p > 0.05), CFI and TLI values greater than 0.90 (preferably > 0.95), and RMSEA values less than 0.08 (preferably < 0.05).
3. Results
3.1. Sample Characterization
The study sample consisted of 203 nursing professionals. The response rate for this study was 45.7% of the estimated population of 444 professionals, which, while offering valuable insights, should be considered when interpreting the generalizability of findings.
Specifically, of the 203 professionals, 25 (12.3%) were nursing assistants, 99 (48.8%) were nursing technicians, and 79 (38.9%) were nurses. The sample was predominantly female (81.3%) and younger, with 58.6% under 39 years of age. Regarding marital status, 62.1% reported living with a partner, and 61.6% had one or more children. The predominant family income (66.0%) was in the range of BRL 3000 or more per month, which is consistent with middle-income brackets in the region and provides context for the economic status of the participants.
Regarding professional characteristics, 67% of participants worked between 31 and 44 h weekly, and 77% had only one employment relationship. The most prevalent work sector was emergency (71%), with 44% working in Emergency Care Units (UPAs) and 29% in hospital inpatient units. The motivation for accumulating employment relationships, for the 21% who did so, was related to financial necessity (15%) and pursuit of better remuneration (6%). Regarding academic qualifications, 21% of professionals had a specialization, and 3% had a master’s or doctoral degree.
3.2. Prevalence of Minor Mental Disorders (MMD)
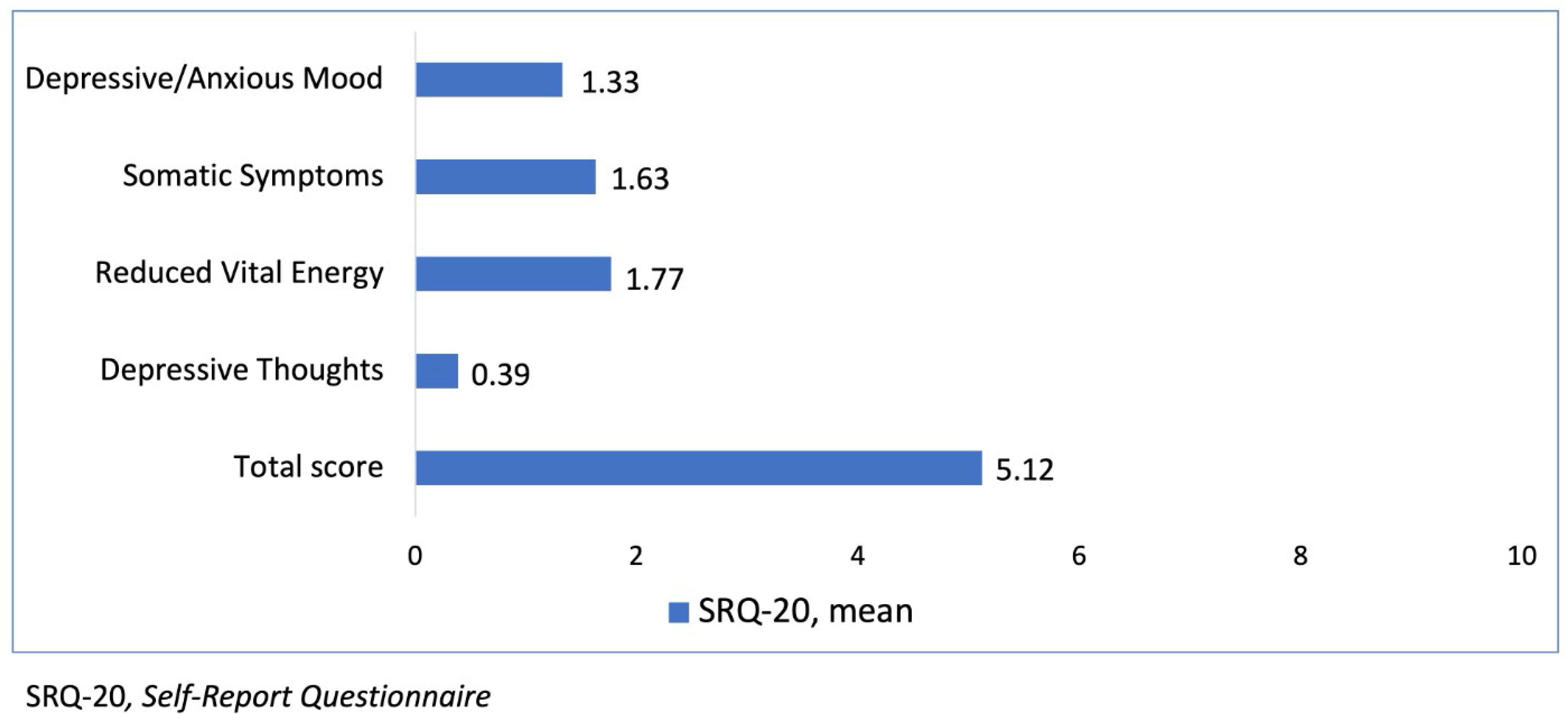
Screening for Minor Mental Disorders (MMD) was conducted using the Self-Report Questionnaire (SRQ-20). The prevalence of MMD in the studied sample was 31.0% (n = 63), defined by an SRQ-20 score equal to or greater than eight points.
The mean scores for the different domains of the SRQ-20 were 1.33 for Depressive/Anxious Mood, 1.63 for Somatic Symptoms, 1.77 for Reduced Vital Energy, 0.39 for Depressive Thoughts, and the mean total score was 5.12—
Figure 2.
Figure 2 graphically illustrates these mean scores.
3.3. Factor Analysis and Instrument Reliability
3.3.1. Self-Report Questionnaire (SRQ-20)
The factorial structure of the SRQ-20 was evaluated through Bayesian confirmatory factor analysis, adopting a model of four correlated factors: Depressive–Anxious Mood (DAM), Somatic Symptoms (SS), Decreased Vital Energy (DEV), and Depressive Thoughts (DT). The Bayesian fit indices were considered adequate: the posterior predictive p-value (ppp) was 0.344; the Deviance Information Criterion (DIC) was 3327.168; the Watanabe-Akaike Information Criterion (WAIC) was 3343.535; and the Leave-One-Out Information Criterion (LOOIC) was 3343.781.
Table 1 presents the standardized factor loadings of the items for each of the four latent factors of the SRQ-20. These loadings demonstrate how strongly each item relates to its underlying factor, providing crucial evidence for the validity of the instrument’s factorial structure. All non-zero loadings are statistically significant, indicating a robust measurement model.
The correlations between the latent factors of the SRQ-20 were high and are presented in
Table 2. This strong correlation among factors indicates that while distinct, these dimensions of minor mental disorders are highly intertwined.
The composite reliability for the Decreased Vital Energy (DEV) factor was 0.842, for Depressive–Anxious Mood (DAM) was 0.739, for Depressive Thoughts (DTs) was 0.826, and for Somatic Symptoms (SSs) was 0.762, indicating good to excellent internal consistency for all factors, thereby confirming their reliability in this sample.
3.3.2. Wagnild and Young Resilience Scale
This study tested different models for the Wagnild and Young Resilience Scale.
Table 3 compares the fit of Bayesian models for the 14- and 25-item versions, with and without collapsed response categories.
Table 4 presents the fit of these same models through the traditional confirmatory factor approach.
It was observed that categories 1, 2, 3, and 4 of the original 7-point scale had the lowest response rates and were collapsed into a single category, while categories 5, 6, and 7 became, respectively, 2, 3, and 4.
Table 5 details the percentages of original responses in each category.
As indicated by the model fit indices in
Table 3 and
Table 4, the 14-item model with collapsed categories consistently presented the best balance of fit in both Bayesian and traditional confirmatory factor analysis approaches, validating its use for this study. The standardized factor loadings for this optimal model had a mean of 0.74 (SD = 0.08) and a median of 0.77. The composite reliability for the 14-item collapsed model was 0.860, indicating high internal consistency and supporting the robustness of this version of the scale in our sample.
3.3.3. WHOQOL-BREF
The Bayesian factor analysis for WHOQOL-BREF evaluated Hierarchical, Partial Bifactor, and Complete Bifactor models.
Table 6 presents the fit indices for these models.
The Complete Bifactor Model was the most adequate in terms of DIC (10,907.31), WAIC (11,043.11), and LOOIC (11,044.76).
Table 7 details the factor loadings of this model.
The composite reliability for the Quality of Life (QoL) factor was 0.829, for the Physical factor was 0.561, for the Environmental factor was 0.266, and for the Social factor was 0.261. Critically, the Psychological factor presented extremely low composite reliability (0.00000983), indicating that the items associated with it do not significantly contribute to the measurement of the construct independently in this bifactor model. For this reason, the factor scores of the Psychological factor were not used in subsequent analyses.
3.4. Path Analysis Results
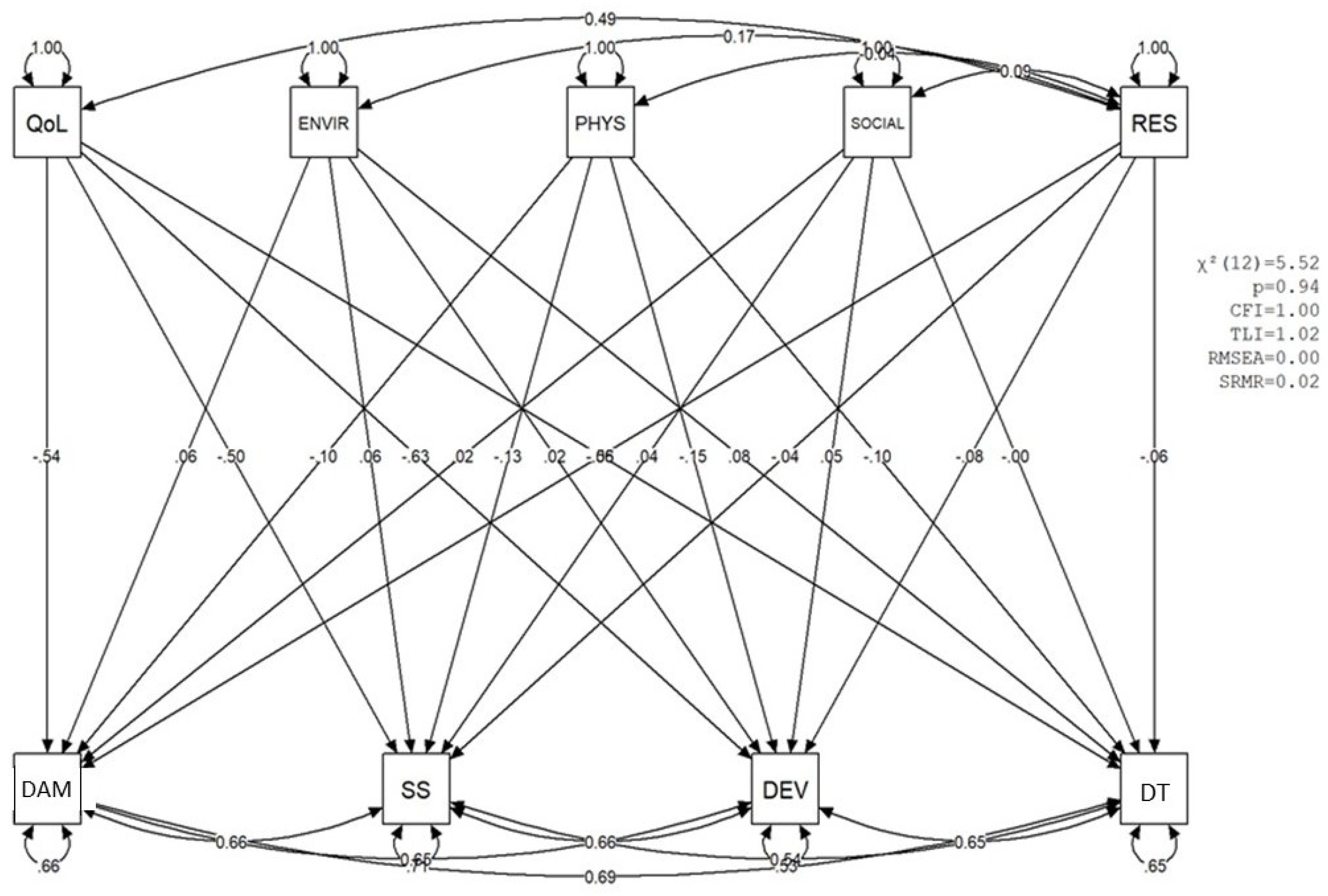
Path analysis was conducted to examine the predictive relationships between WHOQOL-BREF domains (General Quality of Life—QoL, Environmental—ENVIR, Physical—PHYS, Social—SOCIAL) and Resilience (RES) with dimensions of mental health (Decreased Vital Energy—DEV, Depressive–Anxious Mood—DAM, Depressive Thoughts—DTs, Somatic Symptoms—SSs). The analyses were based on 2000 posterior distributions of factor scores.
The fit indices of the path analysis models demonstrated excellent adequacy to the data: the mean chi-square value was 2.45 (SD = 1.36), with 12 fixed degrees of freedom and a mean p-value of 0.99 (SD = 0.03). The Comparative Fit Index (CFI) presented a mean of 1.00 (SD = 0), the Tucker–Lewis Index (TLI) a mean of 1.04 (SD = 0.01), and the Root Mean Square Error of Approximation (RMSEA) a mean of 0 (SD = 0), with a 95% confidence interval for the RMSEA reaching a maximum of 0.09.
Table 8 presents the descriptive statistics of the main results of the 2000 path analyses, including the standardized estimated values and
p-values for the relationships between variables.
The results indicated that the overall Quality of Life (QoL) factor, derived from the WHOQOL-BREF after excluding the Psychological domain due to its inadequate reliability (as detailed in
Section 3.3.3), was a robust and statistically significant predictor of all dimensions of mental health: Decreased Vital Energy (mean coef. = −0.579;
p < 0.001), Depressive–Anxious Mood (mean coef. = −0.497;
p < 0.001), Depressive Thoughts (mean coef. = −0.498;
p < 0.001), and Somatic Symptoms (mean coef. = −0.523;
p < 0.001). These strong negative relationships highlight the critical protective role of this comprehensive measure of overall QoL against mental health symptoms.
The Physical factor (PHYS) of WHOQOL-BREF also presented a significant role in predicting mental health variables, with regression coefficients ranging from −0.15 for DAM (p = 0.046) to −0.18 for SS (p = 0.024). In contrast, the Environmental (ENVIR) and Social (SOCIAL) variables of WHOQOL-BREF did not demonstrate a significant predictive role for mental health symptoms, with mean p-values above 0.3.
Resilience (RES) did not present a significant predictive role on mental health variables (high p-values, above 0.4) when the effect of quality of life was controlled. However, resilience correlated significantly with Quality of Life (QoL) (coef. = 0.515; p < 0.001). This suggests that, while resilience does not directly predict MMDs when QoL is accounted for, it maintains a strong positive association with QoL, indicating its potential indirect influence.
The mental health variables (DEV, SS, for DAM, and DT) presented relatively high explained variance (R2), with coefficients ranging from 0.586 to 0.695, indicating that between 30.5% and 41.4% of the variance in these variables was explained by the model’s predictors.
Figure 3 presents a visual example of one of the mental health prediction models in nurses, with their respective standardized estimate values.
3.5. Quality of Life and Minor Mental Disorders by Sociodemographic and Professional Data
This section presents a comparative analysis of Quality of Life (WHOQOL-Bref domains) and Minor Mental Disorders (SRQ-20) across various sociodemographic and professional characteristics of the sample. Statistically significant findings (
p < 0.05) are highlighted within the tables for clarity. Detailed sociodemographic and professional characteristics of the participants are presented in
Table 9 and
Table 10.
4. Discussion
The mental health of nursing professionals is a critical global concern, and our study underscores the significant challenges faced by this essential workforce. This investigation aimed to delineate the prevalence of Minor Mental Disorders (MMDs) and resilience levels among nursing professionals, further exploring their intricate relationships with quality of life (QoL). Our findings highlight that a substantial proportion of nursing professionals experience MMDs, affirming the urgent need for targeted interventions. Crucially, we observed a strong relationship where a higher quality of life is strongly associated with fewer mental health symptoms, while resilience appears to bolster mental well-being indirectly through its positive influence on quality of life. These insights offer concrete directions for promoting the psychological well-being of nurses in demanding healthcare settings globally, emphasizing key protective factors and identifying areas for strategic support.
The prevalence of MMD in our sample, at 31.0%, is a compelling finding that aligns with a broad body of international literature identifying nursing as a risk group for mental health challenges [
27,
28,
29]. For instance, studies from diverse Asian cohorts have consistently reported MMD prevalence rates ranging from 20% to over 40% among nurses, often exacerbated by factors such as demanding shift work, long working hours, and high patient loads [
82]. Similarly, recent European studies underscore elevated rates of burnout, anxiety, and depression in nursing populations, particularly within high-pressure and under-resourced environments like emergency departments and intensive care units [
83]. This percentage reflects the impact of demands inherent to the profession, such as excessive working hours, constant pressure, and exposure to critical situations, which characterize a challenging and stressful work environment [
2,
84]. The SRQ-20 domains with the highest mean scores were “Reduction of Vital Energy” and “Somatic Symptoms,” indicating significant physical and emotional exhaustion, aligned with the conceptualization of burnout as a phenomenon of exhaustion [
13]. Occupational stress can lead to anxiety, depression, distress, poor performance, and hostility, outcomes that manifest in the observed MMDs.
A particularly robust and clinically relevant findings from our analysis is the consistent negative association observed between the overall General Quality of Life (QoL) (excluding the psychological domain due to its psychometric limitations, as discussed in
Section 3.3.3) and all dimensions of MMD (Decreased Vital Energy, Depressive–Anxious Mood, Depressive Thoughts, and Somatic Symptoms), as presented in
Table 8. This strong correlation indicates that a higher perceived quality of life is strongly associated with a lower presence and severity of MMD symptoms. It is crucial to emphasize that, given the cross-sectional design of this study, we cannot establish direct causal relationships; rather, these findings highlight a significant and consistent interplay where greater QoL co-occurs with better mental health outcomes. The observed relationships suggest that QoL acts as a critical factor in the overall mental well-being equation for nursing professionals, serving not merely as an indicator of well-being but as a potentially crucial protective element associated with the manifestation of mental health challenges. This emphasizes the importance of enhancing QoL as a strategic target for interventions. This result reinforces the tenets of the Biopsychosocial Model, which posits that an individual’s subjective perception of their life (QoL) interacts dynamically with psychological and social factors to profoundly influence mental health [
18].
The role of resilience, while complex, emerged as a fundamental, albeit indirect, factor. While our initial hypothesis anticipated a direct predictive role of resilience on MMDs, particularly when controlling for QoL, the results did not support this direct link. Instead, we observed a highly significant and positive correlation between resilience and Quality of Life (QoL), as shown in
Table 8. This intriguing pattern suggests that resilience may function as an indirect moderator or precursor to QoL, whereby QoL then exerts a more direct and robust influence on the reduction of MMDs. This finding resonates with emerging research from diverse international contexts; for instance, studies from European nurses indicate that, while resilience may not always directly mitigate distress, it consistently enhances coping efficacy and well-being, pathways that frequently lead to improved QoL [
83]. Similarly, research among healthcare workers in Southeast Asia points to resilience as a crucial resource for maintaining a positive outlook and adaptive functioning, particularly by fostering a sense of control and self-efficacy that underpins better quality of life perceptions even amid high occupational stress [
85,
86]. In essence, individuals demonstrating greater resilience tend to report a higher perception of their quality of life, and this elevated QoL, in turn, appears to mediate the impact of resilience on mitigating MMD symptoms. This interpretation aligns well with the Transactional Model of Stress and Coping, where resilience, understood as a dynamic process that mobilizes adaptive coping strategies, contributes to a more constructive assessment of stressors. Consequently, this fosters better QoL, thereby minimizing the deleterious effects of stress on mental health [
87]. Therefore, resilience is not merely the capacity to endure but to “positively rebuild,” manifested in the ability to maintain a satisfactory QoL even when confronted with adverse environments [
32].
The analysis of the physical factor of WHOQOL-BREF as a significant correlate of MMDs suggests the inherent physical demands of nursing work, such as prolonged standing and significant physical exertion, are indeed linked to psychological well-being [
15,
88]. This finding underscores the necessity of integrated approaches that consider both the mental and physical dimensions of occupational health. Conversely, the Environmental and Social domains of WHOQOL-BREF did not demonstrate a significant association with mental health symptoms in our analysis (
Table 8). While this non-significance could partly be attributed to the low composite reliability observed for these domains in our factor analysis of WHOQOL-BREF, suggesting a measurement artifact that likely obscured their true predictive or correlational role (as elaborated in
Section 4.1, Limitations), it also prompts a broader consideration. In highly demanding and high-stress professional environments like nursing, the immediate and direct impacts of physical strain and psychological burden on mental health might be more pronounced and perceivable than the effects of perceived environmental comfort or social relationships. This is not to diminish the importance of supportive social and environmental factors, which are crucial for overall well-being and long-term sustainability. Instead, it suggests that in a context of acute and pervasive occupational stressors, their influence on MMDs might be more subtle or indirect, perhaps mediated through other constructs not fully captured by our current model (e.g., job satisfaction, organizational support culture, or individual coping styles related to social engagement). Future research employing qualitative methods or more granular, context-specific measures of these domains could provide deeper insights into their true influence, moving beyond purely psychometric considerations and exploring their nuanced roles in different work environments.
Our examination of sociodemographic and professional characteristics further revealed specific vulnerabilities within the nursing cohort, as detailed in
Table 9 and
Table 10. Notably, younger professionals (up to 39 years) and females exhibited a higher prevalence of MMDs and a lower perception of QoL. These data are consistent with existing literature suggesting increased susceptibility of these demographic groups to particular types of occupational stress, often compounded by the complex interplay of professional and personal responsibilities [
26]. It is important to acknowledge that females comprised the overwhelming majority (81.3%) of our sample, which necessitates careful consideration when extrapolating these observed gender differences, as they may reflect the sample composition rather than intrinsic gender vulnerability alone.
To fully comprehend the observed interactions, it is crucial to consider the underlying biological and psychophysiological mechanisms. Chronic occupational stress can lead to dysregulation of the Hypothalamic–Pituitary–Adrenal (HPA) axis and the Autonomic Nervous System (ANS), manifesting in alterations in cortisol levels, reduced heart rate variability, and dysfunctions in neurotransmitter systems [
39]. These neuroendocrine and neural alterations directly contribute to the symptoms of anxiety, depression, and fatigue that comprise MMDs. Conversely, resilience is associated with more effective regulation of these biological systems, facilitating faster recovery of homeostasis following stressful events and conferring protection against the deleterious effects of chronic stress [
40]. This biological modulation by resilience is a fundamental aspect that underpins the protective role, albeit indirect, observed in our study. Our findings, suggesting the mediation of QoL, resonate with the need for integrated research that considers the various intrapsychic, interpersonal, familial, occupational, and social components, thereby supporting a holistic perspective on mental health.
4.1. Limitations
Despite the important contributions, this study has several limitations that should be considered in the interpretation of its results. First, the cross-sectional design inherently precludes the establishment of causal relationships between variables. Longitudinal studies are essential to explore the directionality of observed associations and the dynamic interplay of QoL, MMDs, and resilience over time.
Second, the use of self-report instruments (WHOQOL-BREF, SRQ-20, and Wagnild & Young Resilience Scale) may be subject to biases, such as social desirability bias, where participants may tend to provide socially acceptable responses.
Third, the low composite reliability of the Psychological, Environmental, and Social factors of WHOQOL-BREF in the complete bifactor model (with values of 0.00000983, 0.266, and 0.261, respectively) represents an important limitation. While the overall model fit was good, the inadequate measurement quality of these specific domains might have obscured their true predictive or correlational roles with mental health. The extremely low reliability of the Psychological factor, in particular, prevented its inclusion as an independent dimension in the path analysis, thus limiting specific conclusions about its unique contribution.
Finally, although we have discussed the underlying biological and psychophysiological mechanisms, the study did not include direct measurement of biomarkers (e.g., cortisol levels, heart rate variability). The inclusion of such measures could further strengthen the understanding of the complex interactions between psychosocial factors and the mental health of nursing professionals, providing a more solid empirical basis for discussions on the Biopsychosocial Model. Future research incorporating such direct biological measures would enhance the understanding of the complex interactions within the Biopsychosocial Model.
4.2. Implications
The results of this study have significant implications for clinical practice, occupational health management, and future research in the area of mental health of nursing professionals.
4.2.1. Implications for Practice and Occupational Health Management
Need for Comprehensive Interventions: The high prevalence of MMDs reinforces the urgency of mental health promotion programs and specific illness prevention for nursing professionals. These programs should go beyond simply detecting symptoms to address the roots of occupational stress.
Focus on Quality of Life: Given the strong prediction of the overall QoL construct (as operationalized in this study) on MMDs, healthcare organizations should prioritize strategies that improve the quality of life of their professionals. This may include optimizing workloads, promoting a healthier and more collaborative work environment, offering adequate breaks, fostering work–life balance, and ensuring recognition and support.
Resilience Programs: Although resilience did not directly predict MMDs in our model, its strong correlation with QoL suggests that developing resilience may be an effective indirect pathway to mitigate mental distress. Training programs in coping skills, emotional regulation, mindfulness, and promotion of social support networks can strengthen resilience and, consequently, improve QoL.
Targeted Interventions: The greater vulnerability of younger professionals and females points to the need to develop interventions adapted to these demographics, considering their particularities and the specific challenges they face in the work environment and in their personal lives.
Attention to Physical Aspects of Work: The physical domain of QoL being a predictor of MMDs underlines that working conditions that lead to physical wear should be reviewed. Ergonomic measures, more flexible work schedules, and the encouragement of physical health (e.g., physical activity, nutrition) can have a positive cascade impact on mental health.
4.2.2. Implications for Future Research
Longitudinal and Mediation Studies: Future research should employ longitudinal designs to establish causal relationships and investigate the mediating nature of QoL in the relationship between resilience and MMDs. More complex models can elucidate the dynamic interactions between these variables over time.
Biological and Psychophysiological Mechanisms: Integrating the assessment of stress biomarkers (e.g., salivary cortisol, HRV) in future research can deepen the understanding of the underlying mechanisms that connect occupational stress, resilience, QoL, and MMDs, providing solid empirical evidence for the complex network of interactions.
Development and Validation of Instruments: The low reliability of some domains of WHOQOL-BREF in our study points to the need to explore the adequacy of QoL assessment instruments and other constructs in specific populations of healthcare professionals, or to develop and validate new tools that better capture the nuance of these factors. Future research should particularly focus on validating and refining measures for the psychological, environmental, and social dimensions of quality of life within nursing contexts to ensure accurate and comprehensive assessment.
Resilience and Engagement: Investigate how resilience not only mitigates suffering but also promotes engagement and professional fulfillment, connecting with the dimension of low personal accomplishment in burnout.
Environmental and Social Factors in the Workplace: Despite the low reliability in the instrument, it is crucial to continue investigating the influence of social support in the work environment, organizational culture, and occupational health policies on the mental health of nurses, using methodologies that capture these complexities more effectively, especially considering the nuanced interplay suggested by our current findings.
Focus on Quality of Life: Given the strong negative association/relationship of the overall QoL construct with MMDs, healthcare organizations should prioritize strategies that improve the quality of life of their professionals. This may include optimizing workloads, promoting a healthier and more collaborative work environment, offering adequate breaks, fostering work–life balance, and ensuring recognition and support.
Attention to Physical Aspects of Work: The physical domain of QoL being associated with MMDs underlines that working conditions that lead to physical wear should be reviewed. Ergonomic measures, more flexible work schedules, and the encouragement of physical health (e.g., physical activity, nutrition) can have a positive cascade impact on mental health.