Low-Level PM2.5 Exposure and Mortality in the Medicare Cohort: The Role of Native American Beneficiaries
Abstract
1. Introduction
2. Materials and Methods
2.1. Medicare Data
2.2. Ambient Air Pollution Data
2.3. Covariate Data
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
3.2. Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PM2.5 | Fine particulate matter |
| HR | Hazard ratio |
| EPA | U.S. Environmental Protection Agency |
| NAAQS | National Ambient Air Quality Standard |
| CRF | Concentration response function |
| CMS | Centers for Medicare and Medicaid Services |
| MBSF | Master Beneficiary Summary File |
| ICD-10 | International Classification of Diseases Tenth Revision |
| NO2 | Nitrogen dioxide |
| O3 | Ozone |
| SEDAC | Socioeconomic Data and Applications Center |
| SVI | Social vulnerability index |
| CDC | U.S. Centers for Disease Control and Prevention |
| RUCA | Rural-Urban Commuting Area |
| SES | Socioeconomic status |
| NAN | North American Native |
| OR | Odds ratio |
| USD | US dollar |
| COPD | Chronic obstructive pulmonary disease |
| SDOH | Social determinants of health |
| IHS | Indian Health Service |
References
- Health Effects Institute. New HEI Program to Examine Potential Health Effects at Low-Levels of Air Pollution; Health Effects Institute: Boston, MA, USA, 2016; Available online: https://www.healtheffects.org/system/files/HEI-Research-on-Low-Concentrations-2016_2.pdf (accessed on 30 April 2025).
- Shi, L.; Zanobetti, A.; Kloog, I.; Coull, B.A.; Koutrakis, P.; Melly, S.J.; Schwartz, J.D. Low-Concentration PM2.5 and Mortality: Estimating Acute and Chronic Effects in a Population-Based Study. Environ. Health Perspect. 2016, 124, 46–52. [Google Scholar] [CrossRef]
- Di, Q.; Wang, Y.; Zanobetti, A.; Wang, Y.; Koutrakis, P.; Choirat, C.; Dominici, F.; Schwartz, J.D. Air Pollution and Mortality in the Medicare Population. N. Engl. J. Med. 2017, 376, 2513–2522. [Google Scholar] [CrossRef]
- Wu, X.; Braun, D.; Schwartz, J.; Kioumourtzoglou, M.A.; Dominici, F. Evaluating the impact of long-term exposure to fine particulate matter on mortality among the elderly. Sci. Adv. 2020, 6, eaba5692. [Google Scholar] [CrossRef]
- Wei, Y.; Yazdi, M.D.; Di, Q.; Requia, W.J.; Dominici, F.; Zanobetti, A.; Schwartz, J. Emulating causal dose-response relations between air pollutants and mortality in the Medicare population. Environ. Health Glob. Access Sci. Source 2021, 20, 53. [Google Scholar] [CrossRef]
- Dominici, F.; Zanobetti, A.; Schwartz, J.; Braun, D.; Sabath, B.; Wu, X. Assessing Adverse Health Effects of Long-Term Exposure to Low Levels of Ambient Air Pollution: Implementation of Causal Inference Methods. Res. Rep. 2022, 2022, 1–56. [Google Scholar]
- U.S. Environmental Protection Agency. Final Rule to Strengthen the National Air Quality Health Standard for Particulate Matter. 2024. Available online: https://www.epa.gov/system/files/documents/2024-02/pm-naaqs-overview.pdf (accessed on 30 April 2025).
- Schwartz, J.; Wei, Y.; Yitshak-Sade, M.; Di, Q.; Dominici, F.; Zanobetti, A. A national difference in differences analysis of the effect of PM2.5 on annual death rates. Environ. Res. 2021, 194, 110649. [Google Scholar] [CrossRef]
- Chen, J.; Hoek, G. Long-term exposure to PM and all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ. Int. 2020, 143, 105974. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Diseases Tenth Revision (ICD-10), 6th ed.; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Wei, Y.; Xing, X.; Shtein, A.; Castro, E.; Hultquist, C.; Yazdi, M.D.; Li, L.; Schwartz, J. Daily and Annual PM2.5, O3, and NO2 Concentrations at ZIP Codes for the Contiguous US, 2000-2016, v1.0 (Version 1.00) [Data Set]; NASA Socioeconomic Data and Applications Center (SEDAC): Palisades, NY, USA, 2022. [Google Scholar] [CrossRef]
- Di, Q.; Amini, H.; Shi, L.; Kloog, I.; Silvern, R.; Kelly, J.; Sabath, M.B.; Choirat, C.; Koutrakis, P.; Lyapustin, A.; et al. An ensemble-based model of PM2.5 concentration across the contiguous United States with high spatiotemporal resolution. Environ. Int. 2019, 130, 104909. [Google Scholar] [CrossRef] [PubMed]
- Thornton, M.M.; Shrestha, R.; Wei, Y.; Thornton, P.E.; Kao, S.C. Daymet: Daily Surface Weather Data on a 1-km Grid for North America, Version 4 R1 (Version 4.1); ORNL Distributed Active Archive Center: Oak Ridge, TN, USA, 2022. [Google Scholar] [CrossRef]
- Center for International Earth Science Information Network, (CIESIN), Columbia University. U.S. Social Vulnerability Index Grids, Revision 01 (Version 1.01) [Data Set]; NASA Socioeconomic Data and Applications Center (SEDAC): Palisades, NY, USA, 2023. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture Economic Research Service. Rural-Urban Commuting Area Codes—Documentation. 2025. Available online: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation (accessed on 30 April 2025).
- U.S. Census Bureau. Explore Census Data. Available online: https://data.census.gov/ (accessed on 30 April 2025).
- Bowe, B.; Xie, Y.; Yan, Y.; Al-Aly, Z. Burden of Cause-Specific Mortality Associated with PM2.5 Air Pollution in the United States. JAMA Netw. Open 2019, 2, e1915834. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wu, T.; Zhou, W.; Han, L.; Neophytou, A.M. Reducing air pollution does not necessarily reduce related adults’ mortality burden: Variations in 177 countries with different economic levels. Sci. Total Environ. 2024, 933, 173037. [Google Scholar] [CrossRef]
- Bunnell, J.E.; Garcia, L.V.; Furst, J.M.; Lerch, H.; Olea, R.A.; Suitt, S.E.; Kolker, A. Navajo coal combustion and respiratory health near Shiprock, New Mexico. J. Environ. Public Health 2010, 2010, 260525. [Google Scholar] [CrossRef]
- Seltenrich, N. Healthier tribal housing: Combining the best of old and new. Environ. Health Perspect. 2012, 120, A460–A469. [Google Scholar] [CrossRef]
- Hadeed, S.J.; O’Rourke, M.K.; Canales, R.A.; Joshweseoma, L.; Sehongva, G.; Paukgana, M.; Gonzalez-Figueroa, E.; Alshammari, M.; Burgess, J.L.; Harris, R.B. Household and behavioral determinants of indoor PM2.5 in a rural solid fuel burning Native American community. Indoor Air 2021, 31, 2008–2019. [Google Scholar] [CrossRef]
- Office of Disease Prevention and Health Promotion, U.S. Department of Health and Human Services. Social Determinants of Health. Available online: https://odphp.health.gov/healthypeople/priority-areas/social-determinants-health (accessed on 30 April 2025).
- Jones, D.S. The persistence of American Indian health disparities. Am. J. Public Health 2006, 96, 2122–2134. [Google Scholar] [CrossRef] [PubMed]
- Arias, E.; Xu, J.; Curtin, S.; Bastian, B.; Tejada-Vera, B. Mortality Profile of the Non-Hispanic American Indian or Alaska Native Population, 2019. Natl. Vital Stat. Rep. 2021, 70, 1–27. [Google Scholar] [PubMed]
- Medicaid and CHIP Payment and Access Commission (MACPAC). Issue Brief: Medicaid’s Role in Health Care for American Indians and Alaska Natives; Medicaid and CHIP Payment and Access Commission: Washington, DC, USA, 2021. Available online: https://www.macpac.gov/wp-content/uploads/2021/02/Medicaids-Role-in-Health-Care-for-American-Indians-and-Alaska-Natives.pdf (accessed on 30 April 2025).
- Odani, S.; Armour, B.S.; Graffunder, C.M.; Garrett, B.E.; Agaku, I.T. Prevalence and Disparities in Tobacco Product Use Among American Indians/Alaska Natives—United States, 2010–2015. MMWR. Morb. Mortal. Wkly. Rep. 2017, 66, 1374–1378. [Google Scholar] [CrossRef] [PubMed]
- Arrazola, R.A.; Griffin, T.; Lunsford, N.B.; Kittner, D.; Bammeke, P.; Courtney-Long, E.A.; Armour, B.S. US Cigarette Smoking Disparities by Race and Ethnicity—Keep Going and Going! Prev. Chronic Dis. 2023, 20, 220375. [Google Scholar] [CrossRef]
- Azagba, S.; Shan, L.; Latham, K.; Qeadan, F. Trends in cigarette smoking among American Indians and Alaska Natives in the USA: 1992–2015. Cancer Causes Control 2020, 31, 73–82. [Google Scholar] [CrossRef]
- U.S. Environmental Protection Agency. Integrated Science Assessment (ISA) for Particulate Matter (Final Report, December 2019); EPA/600/R-19/188; U.S. Environmental Protection Agency: Washington, DC, USA, 2019.
- Boccuti, C.; Swoope, C.; Artiga, S. The Role of Medicare and the Indian Health Service for American Indians and Alaska Natives: Health, Access and Coverage; The Henry J. Kaiser Family Foundation: San Francisco, CA, USA, 2014; Available online: https://www.kff.org/medicare/report/the-role-of-medicare-and-the-indian-health-service-for-american-indians-and-alaska-natives-health-access-and-coverage/ (accessed on 6 August 2025).
- United States Government Accountability Office. Indian Health Service: Health Care Services Are Not Always Available to Native Americans; GAO-05-789; Report to the Committee on Indian Affairs; United States Government Accountability Office: Washington, DC, USA, 2005.
- Kaiser Family Foundation. Status of State Medicaid Expansion Decisions. Available online: https://www.kff.org/status-of-state-medicaid-expansion-decisions/ (accessed on 30 April 2025).
- Hajat, A.; MacLehose, R.F.; Rosofsky, A.; Walker, K.D.; Clougherty, J.E. Confounding by Socioeconomic Status in Epidemiological Studies of Air Pollution and Health: Challenges and Opportunities. Environ. Health Perspect. 2021, 129, 65001. [Google Scholar] [CrossRef]
- Luo, J.; Craver, A.; Jin, Z.; Zheng, L.; Kim, K.; Polonsky, T.; Olopade, C.O.; Pinto, J.M.; Ahsan, H.; Aschebrook-Kilfoy, B. Contextual Deprivation, Race and Ethnicity, and Income in Air Pollution and Cardiovascular Disease. JAMA Netw. Open 2024, 7, e2429137. [Google Scholar] [CrossRef]
- Singh, G.; Williams, S.; Lee, H.; Martin, E.; Allender, M.; Ramey, C. Trends in Physical and Mental Health, Mortality, Life Expectancy, and Social Inequalities Among American Indians and Alaska Natives, 1990–2019. Int. J. Transl. Med. Res. Public Health 2021, 5, 227–253. [Google Scholar] [CrossRef]
- Li, M.; Hilpert, M.; Goldsmith, J.; Brooks, J.L.; Shearston, J.A.; Chillrud, S.N.; Ali, T.; Umans, J.G.; Best, L.G.; Yracheta, J.; et al. Air Pollution in American Indian Versus Non-American Indian Communities, 2000–2018. Am. J. Public Health 2022, 112, 615–623. [Google Scholar] [CrossRef]
- Li, M.; Do, V.; Brooks, J.L.; Hilpert, M.; Goldsmith, J.; Chillrud, S.N.; Ali, T.; Best, L.G.; Yracheta, J.; Umans, J.G.; et al. Fine particulate matter composition in American Indian vs. Non-American Indian communities. Environ. Res. 2023, 237 Pt 2, 117091. [Google Scholar] [CrossRef]
- Nunez, Y.; Benavides, J.; Shearston, J.A.; Krieger, E.M.; Daouda, M.; Henneman, L.R.F.; McDuffie, E.E.; Goldsmith, J.; Casey, J.A.; Kioumourtzoglou, M.-A. An environmental justice analysis of air pollution emissions in the United States from 1970 to 2010. Nat. Commun. 2024, 15, 268. [Google Scholar] [CrossRef]
- Henneman, L.; Choirat, C.; Dedoussi, I.; Dominici, F.; Roberts, J.; Zigler, C. Mortality risk from United States coal electricity generation. Science 2023, 382, 941–946. [Google Scholar] [CrossRef] [PubMed]
- Henneman, L.R.F.; Rasel, M.M.; Choirat, C.; Anenberg, S.C.; Zigler, C. Inequitable Exposures to U.S. Coal Power Plant-Related PM2.5: 22 Years and Counting. Environ. Health Perspect. 2023, 131, 37005. [Google Scholar] [CrossRef] [PubMed]
- Swanson, A.; Holden, Z.A.; Graham, J.; Warren, D.A.; Noonan, C.; Landguth, E. Daily 1 km terrain resolving maps of surface fine particulate matter for the western United States 2003–2021. Sci. Data 2022, 9, 466. [Google Scholar] [CrossRef]
- U.S. Environmental Protection Agency. Air Data: Air Quality Data Collected at Outdoor Monitors Across the U.S. Available online: https://www.epa.gov/outdoor-air-quality-data (accessed on 30 April 2025).
- Jbaily, A.; Zhou, X.; Liu, J.; Lee, T.-H.; Kamareddine, L.; Verguet, S.; Dominici, F. Air pollution exposure disparities across US population and income groups. Nature 2022, 601, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Josey, K.P.; Delaney, S.W.; Wu, X.; Nethery, R.C.; DeSouza, P.; Braun, D.; Dominici, F. Air Pollution and Mortality at the Intersection of Race and Social Class. N. Engl. J. Med. 2023, 388, 1396–1404. [Google Scholar] [CrossRef]
- Loccoh, E.; Joynt Maddox, K.E.; Xu, J.; Shen, C.; Figueroa, J.F.; Kazi, D.S.; Yeh, R.W.; Wadhera, R.K. Rural-Urban Disparities In All-Cause Mortality Among Low-Income Medicare Beneficiaries, 2004–2017. Health Aff. 2021, 40, 289–296. [Google Scholar] [CrossRef]
- Danesh Yazdi, M.; Amini, H.; Wei, Y.; Castro, E.; Shi, L.; Schwartz, J.D. Long-term exposure to PM2.5 species and all-cause mortality among Medicare patients using mixtures analyses. Environ. Res. 2024, 246, 118175. [Google Scholar] [CrossRef]
- Eberly, L.A.; Shultz, K.; Merino, M.; Brueckner, M.Y.; Benally, E.; Tennison, A.; Biggs, S.; Hardie, L.; Tian, Y.; Nathan, A.S.; et al. Cardiovascular Disease Burden and Outcomes Among American Indian and Alaska Native Medicare Beneficiaries. JAMA Netw. Open 2023, 6, e2334923. [Google Scholar] [CrossRef]
- Zhao, G.; Hsia, J.; Vigo-Valentín, A.; Garvin, W.S.; Town, M. Health-Related Behavioral Risk Factors and Obesity Among American Indians and Alaska Natives of the United States: Assessing Variations by Indian Health Service Region. Prev. Chronic Dis. 2022, 19, E05. [Google Scholar] [CrossRef] [PubMed]
- Jacobs-Wingo, J.L.; Espey, D.K.; Groom, A.V.; Phillips, L.E.; Haverkamp, D.S.; Stanley, S.L. Causes and Disparities in Death Rates Among Urban American Indian and Alaska Native Populations, 1999–2009. Am. J. Public Health 2016, 106, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Melkonian, S.C.; Weir, H.K.; Jim, M.A.; Preikschat, B.; Haverkamp, D.; White, M.C. Incidence of and Trends in the Leading Cancers With Elevated Incidence Among American Indian and Alaska Native Populations, 2012–2016. Am. J. Epidemiol. 2021, 190, 528–538. [Google Scholar] [CrossRef]
- Villarroel, M.A.; Clarke, T.C.; Norris, T. Health of American Indian and Alaska Native Adults, by Urbanization Level: United States, 2014–2018. NCHS Data Brief 2020, 372, 1–8. [Google Scholar]
- Park-Lee, E.; Lipari, R.N.; Bose, J.; Hughes, A.; Greenway, K.; Glasheen, C.; Herman-Stahl, M.; Penne, M.; Pemberton, M.; Cajka, J. Substance Use and Mental Health Issues Among U.S. Born American Indians or Alaska Natives Residing on and off Tribal Lands. CBHSQ Data Review; 2018. Available online: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/DRAIANTribalAreas2018/DRAIANTribalAreas2018.pdf (accessed on 1 August 2025).
- Office of Inspector General. Data Brief: Inaccuracies in Medicare’s Race and Ethnicity Data Hinder the Ability to Assess Health Disparities; Office of Inspector General: Washington, DC, USA, 2022. [Google Scholar]
- Jarrín, O.F.; Nyandege, A.N.; Grafova, I.B.; Dong, X.; Lin, H. Validity of Race and Ethnicity Codes in Medicare Administrative Data Compared with Gold-Standard Self-Reported Race Collected During Routine Home Health Care Visits. Med. Care 2020, 58, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare and Medicaid Services. Report to Congress: Improving Medicare Post-Acute Care Transformation (IMPACT) Act of 2014 Strategic Plan for Accessing Race and Ethnicity Data; Centers for Medicare and Medicaid Services: Washington, DC, USA, 2017. Available online: https://www.cms.gov/AboutCMS/Agency-Information/OMH/Downloads/Research-Reports-2017-Report-to-Congress-IMPACT-ACT-of-2014.pdf (accessed on 30 April 2025).
- Mork, D.; Delaney, S.; Dominici, F. Policy-induced air pollution health disparities: Statistical and data science considerations. Science 2024, 385, 391–396. [Google Scholar] [CrossRef]
| Characteristic | Decile 1, No. (%) | All Deciles, No. (%) | ||
|---|---|---|---|---|
| Cases (n = 153,781) | Controls (n = 1,537,810) | Cases (n = 2,773,647) | Controls (n = 27,736,470) | |
| Beneficiary-level covariates | ||||
| Age, mean (SD), y | 81.8 (9.3) | 74.4 (7.6) | 82.1 (9.3) | 74.9 (8.1) |
| Sex | ||||
| Male | 76,972 (50.1) | 744,196 (48.4) | 1,294,125 (46.7) | 12,577,617 (45.4) |
| Female | 76,809 (50.0) | 793,614 (51.6) | 1,479,522 (53.3) | 15,158,850 (54.7) |
| Race | ||||
| White | 141,834 (92.2) | 1,400,476 (91.1) | 2,391,249 (86.2) | 23,222,339 (83.7) |
| Black | 1589 (1.0) | 15,444 (1.0) | 240,845 (8.7) | 2,293,857 (8.3) |
| Other | 1269 (0.8) | 19,161 (1.3) | 28,146 (1.0) | 480,618 (1.7) |
| Asian | 926 (0.6) | 11,859 (0.8) | 40,284 (1.5) | 604,350 (2.2) |
| Hispanic | 2732 (1.8) | 24,296 (1.6) | 45,728 (1.7) | 515,222 (1.9) |
| Native American | 4709 (3.1) | 39,457 (2.6) | 14,217 (0.5) | 122,238 (0.4) |
| Unknown | 722 (0.5) | 27,117 (1.8) | 13,178 (0.5) | 497,846 (1.8) |
| Dual Medicaid Eligibility | 37,013 (24.1) | 165,480 (10.8) | 773,515 (27.9) | 3,669,176 (13.2) |
| Zip code-level covariates | ||||
| Urbanicity | ||||
| Metropolitan | 72,010 (46.8) | 746,108 (48.5) | 2,109,954 (76.1) | 21,704,297 (78.3) |
| Micropolitan | 36,708 (23.9) | 351,464 (22.9) | 342,613 (12.4) | 3,113,969 (11.2) |
| Small Town | 22,790 (14.8) | 216,571 (14.1) | 191,153 (6.9) | 1,704,315 (6.1) |
| Rural | 22,247 (14.5) | 223,441 (14.5) | 129,772 (4.7) | 1,212,823 (4.4) |
| Social Vulnerability Index, mean (SD) | 0.45 (0.26) | 0.43 (0.26) | 0.45 (0.27) | 0.43 (0.27) |
| Percent White | 86.4 | 86.8 | 77.7 | 77.6 |
| Percent Black | 1.7 | 1.6 | 11.5 | 11.0 |
| Percent Hispanic | 14.9 | 14.6 | 12.7 | 13.0 |
| Percent Native American | 3.8 | 3.5 | 0.8 | 0.8 |
| Median household income, USD | 50,621 | 52,003 | 52,270 | 54,840 |
| Median value owner-occupied housing, USD | 205,300 | 217,900 | 170,900 | 183,000 |
| Percent of elderly below poverty level | 8.6 | 8.3 | 9.4 | 9.0 |
| Percent w/less than HS education | 11.1 | 10.6 | 12.6 | 12.1 |
| Percent of owner-occupied housing | 70.4 | 71.2 | 66.7 | 67.2 |
| Population density, No. | 433 | 441 | 2756 | 2966 |
| Annual PM2.5, mean (SD) | 3.70 (0.74) | 3.67 (0.75) | 7.81 (1.87) | 7.81 (1.88) |
| Lag 1 1 PM2.5, mean (SD) | 3.71 (2.84) | 3.67 (2.80) | 7.64 (4.56) | 7.63 (4.58) |
| Annual NO2, mean (SD) | 11.00 (5.09) | 11.07 (5.15) | 15.63 (7.61) | 15.93 (7.72) |
| Lag 1 1 NO2, mean (SD) | 10.52 (6.36) | 10.55 (6.39) | 15.48 (10.07) | 15.71 (10.17) |
| Annual O3, mean (SD) | 41.98 (5.46) | 42.08 (5.54) | 38.75 (3.48) | 38.80 (3.59) |
| Lag 1 1 O3, mean (SD) | 41.98 (9.90) | 42.07 (9.96) | 38.85 (10.42) | 38.90 (10.48) |
| Characteristic | Decile 1, µg/m3, Mean (SD) | All Deciles, µg/m3, Mean (SD) | ||
|---|---|---|---|---|
| Cases (n = 153,781) | Controls (n = 1,537,810) | Cases (n = 2,773,647) | Controls (n = 27,736,470) | |
| All | 3.70 (0.74) | 3.67 (0.75) | 7.81 (1.87) | 7.81 (1.88) |
| Not Medicaid-eligible | 3.69 (0.74) | 3.66 (0.75) | 7.78 (1.86) | 7.78 (1.86) |
| White | 3.69 (0.74) | 3.67 (0.75) | 7.72 (1.87) | 7.71 (1.87) |
| Black | 3.77 (0.78) | 3.77 (0.80) | 8.58 (1.46) | 8.53 (1.45) |
| Hispanic | 3.54 (0.76) | 3.66 (0.76) | 8.04 (2.32) | 8.23 (2.16) |
| Native American | 3.53 (0.67) | 3.43 (0.65) | 6.31 (2.15) | 6.28 (2.18) |
| Medicaid-eligible | 3.74 (0.72) | 3.71 (0.73) | 7.91 (1.87) | 8.06 (1.95) |
| White | 3.78 (0.72) | 3.74 (0.73) | 7.73 (1.86) | 7.81 (1.93) |
| Black | 3.76 (0.83) | 3.83 (0.79) | 8.55 (1.44) | 8.59 (1.46) |
| Hispanic | 3.70 (0.74) | 3.78 (0.72) | 8.28 (2.31) | 8.43 (2.34) |
| Native American | 3.34 (0.62) | 3.27 (0.59) | 5.77 (2.37) | 5.57 (2.44) |
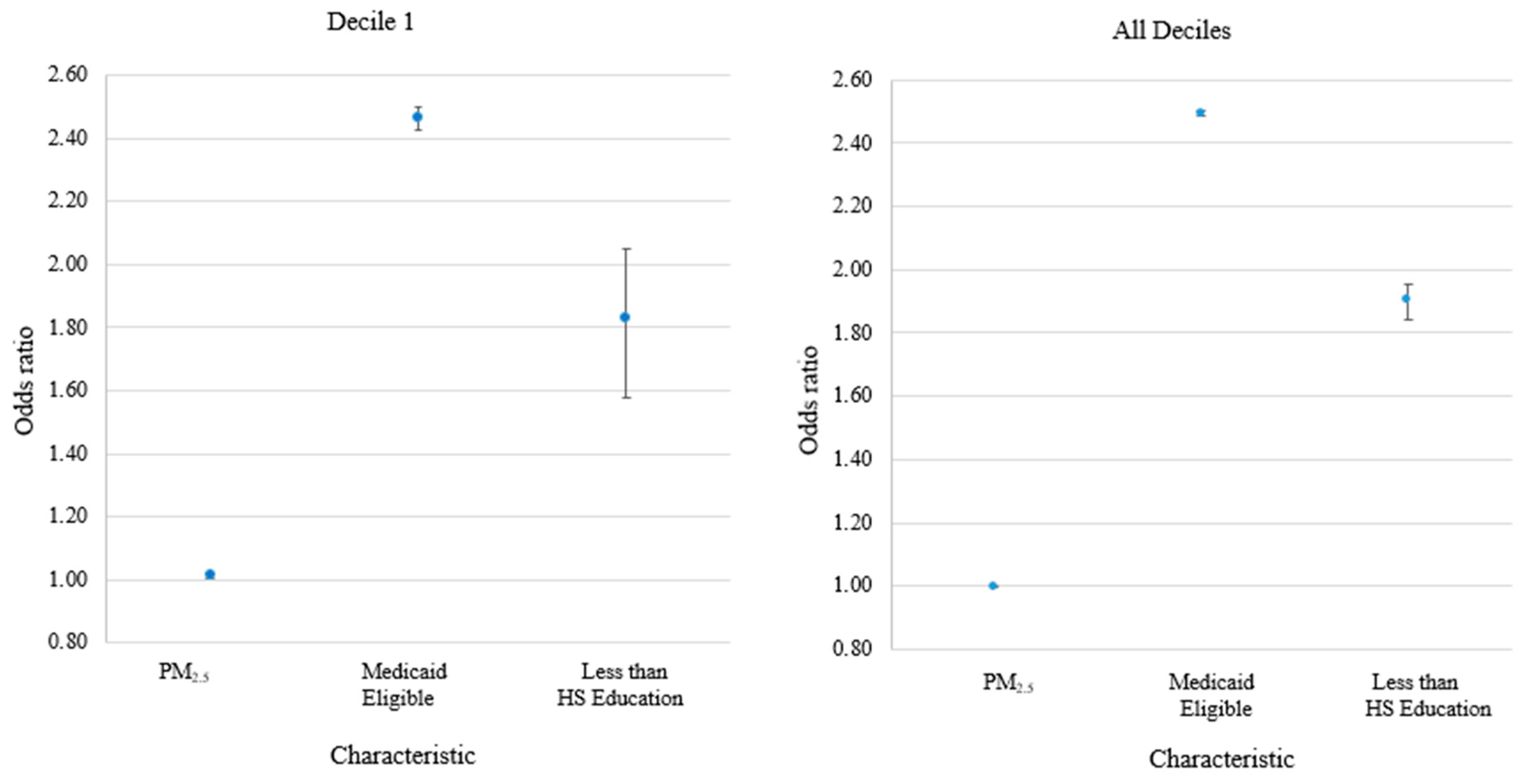
| Characteristic | Odds Ratio (95% CI) 1 | |||
|---|---|---|---|---|
| Decile 1 | All Deciles | |||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| All | 1.060 (1.052–1.067) | 1.013 (1.005–1.022) | 1.003 (1.000–1.006) | 0.998 (0.995–1.001) |
| Not Medicaid-eligible | 1.043 (1.035–1.052) | 1.012 (1.002–1.022) | 1.000 (0.996–1.003) | 0.998 (0.994–1.002) |
| White | 1.047 (1.038–1.056) | 1.009 (0.999–1.019) | 1.004 (1.001–1.008) | 0.997 (0.993–1.001) |
| Black | 1.002 (0.923–1.088) | 1.029 (0.934–1.133) | 1.012 (0.985–1.040) | 1.011 (0.978–1.044) |
| Hispanic | 0.825 (0.762–0.894) | 1.006 (0.907–1.116) | 1.114 (1.008–1.231) | 1.089 (0.937–1.267) |
| Native American | 1.239 (1.158–1.327) | 1.213 (1.112–1.324) | 1.288 (1.003–1.654) | 1.441 (1.020–2.038) |
| Medicaid-eligible | 1.066 (1.050–1.083) | 1.007 (0.988–1.026) | 0.935 (0.929–0.941) | 1.006 (0.999–1.014) |
| White | 1.064 (1.045–1.082) | 1.004 (0.984–1.025) | 0.965 (0.955–0.974) | 1.014 (1.002–1.025) |
| Black | 0.893 (0.805–0.990) | 0.893 (0.788–1.012) | 0.966 (0.928–1.004) | 0.986 (0.940–1.033) |
| Hispanic | 0.864 (0.806–0.926) | 0.978 (0.898–1.064) | 0.981 (0.936–1.029) | 1.010 (0.947–1.077) |
| Native American | 1.231 (1.150–1.318) | 1.105 (1.006–1.213) | 1.064 (0.807–1.401) | 1.110 (0.727–1.694) |
| 113 ICD-10 Cause of Death Recode | 113 ICD-10 Cause of Death Recode Description | ICD-10 Code(s) | All | Native Americans | ||
|---|---|---|---|---|---|---|
| Cases | OR 1 (95% CI) | Cases | OR 1 (95% CI) | |||
| 003 | Certain other intestinal infections | A04, A07–A09 | 631 | 1.02 (0.89–1.17) | 31 | 1.08 (0.46–2.54) |
| 010 | Septicemia | A40–A41 | 1570 | 1.10 (1.01–1.20) | 85 | 1.32 (0.79–2.22) |
| 018 | Other and unspecified infectious and parasitic diseases | A00, A05, A20–A36, A42–A44, A48–A49, A54–A79, A81–A82, A85.0–A85.1, A85.8, A86–B04, B06–B09, B25–B49, B55–B99 | 344 | 1.01 (0.85–1.20) | 14 | 5.82 (0.80–42.21) |
| 021 | Malignant neoplasm of esophagus | C15 | 885 | 0.98 (0.88–1.09) | 13 | 1.49 (0.46–4.86) |
| 022 | Malignant neoplasm of stomach | C16 | 429 | 1.11 (0.94–1.30) | 27 | 0.74 (0.32–1.73) |
| 023 | Malignant neoplasm of colon, rectum, and anus | C18–C21 | 2722 | 0.95 (0.90–1.01) | 80 | 1.17 (0.74–1.84) |
| 024 | Malignant neoplasm of liver and intrahepatic bile ducts | C22 | 1068 | 1.04 (0.95–1.15) | 59 | 1.53 (0.81–2.87) |
| 025 | Malignant neoplasm of pancreas | C25 | 2264 | 1.05 (0.98–1.13) | 51 | 1.09 (0.62–1.92) |
| 027 | Malignant neoplasm of trachea, bronchus, and lung | C33–C34 | 7596 | 1.06 (1.02–1.10) | 152 | 1.37 (0.998–1.87) |
| 029 | Malignant neoplasm of breast | C50 | 1922 | 9.97 (0.90–1.04) | 36 | 0.81 (0.38–1.71) |
| 032 | Malignant neoplasm of ovary | C56 | 747 | 1.01 (0.90–1.14) | 18 | 1.27 (0.34–4.78) |
| 033 | Malignant neoplasm of prostate | C61 | 2269 | 0.94 (0.87–1.01) | 63 | 1.29 (0.66–2.52) |
| 034 | Malignant neoplasm of kidney and renal pelvis | C64–C65 | 775 | 0.96 (0.85–1.08) | 35 | 3.01 (1.06–8.56) |
| 035 | Malignant neoplasm of bladder | C67 | 109 | 0.94 (0.85–1.04) | 13 | 2.35 (0.55–9.98) |
| 036 | Malignant neoplasm of meninges, brain, and other parts of the central nervous system | C70–C72 | 704 | 0.93 (0.83–1.04) | 12 | 0.35 (0.02–1.15) |
| 039 | Non-Hodgkin’s lymphoma | C82–C85 | 1187 | 0.99 (0.90–1.08) | 29 | 1.17 (0.53–2.62) |
| 040 | Leukemia | C91–C95 | 1325 | 1.07 (0.98–1.17) | 20 | 0.77 (0.29–2.06) |
| 041 | Multiple myeloma and immunoproliferative neoplasms | C88, C90 | 684 | 0.97 (0.86–1.10) | 13 | 0.87 (0.19–3.88) |
| 043 | All other and unspecified malignant neoplasms | C17, C23–24, C26–C31, C37–C41, C44–C49, C51–C52, C57–C60, C62–C63, C66, C68–C69, C73–C80, C97 | 4067 | 1.02 (0.97–1.07) | 103 | 0.92 (0.61–1.39) |
| 044 | In situ neoplasms, benign neoplasms, and neoplasms of uncertain or unknown behavior | D00–D48 | 979 | 0.99 (0.89–1.09) | 22 | 0.33 (0.11–0.98) |
| 045 | Anemias | D50–D64 | 292 | 0.97 (0.80–1.18) | 17 | 1.05 (0.17–6.40) |
| 046 | Diabetes mellitus | E10–E14 | 4233 | 1.06 (1.01–1.12) | 367 | 1.53 (1.12–1.96) |
| 048 | Malnutrition | E40–E46 | 442 | 0.87 (0.74–1.03) | 20 | 0.36 (0.09–1.38) |
| 051 | Parkinson’s disease | G20–G21 | 2152 | 1.01 (0.94–1.09) | 60 | 0.95 (0.53–1.71) |
| 052 | Alzheimer’s disease | G30 | 8441 | 0.93 (0.90–0.97) | 117 | 0.86 (0.59–1.26) |
| 059 | Acute myocardial infarction | I21–I22 | 5851 | 1.10 (1.06–1.15) | 157 | 1.41 (1.02–1.95) |
| 062 | Atherosclerotic cardiovascular disease | I25.0 | 3589 | 0.86 (0.81–0.90) | 95 | 1.08 (0.72–1.61) |
| 063 | All other forms of chronic ischemic heart disease | I20, I25.1–I25.9 | 10,966 | 1.02 (0.99–1.05) | 252 | 1.12 (0.85–1.46) |
| 067 | Heart failure | I50 | 4243 | 1.10 (1.04–1.16) | 80 | 0.91 (0.57–1.48) |
| 068 | All other forms of heart disease | I26–I28, I34–I38, I42–I49, I51 | 7712 | 1.03 (0.99–1.07) | 125 | 1.12 (0.79–1.58) |
| 069 | Essential (primary) hypertension and hypertensive renal disease | I10, I12 | 1843 | 1.03 (0.95–1.11) | 51 | 1.32 (0.73–2.38) |
| 070 | Cerebrovascular diseases | I60–I69 | 8334 | 0.99 (0.96–1.03) | 207 | 0.95 (0.71–1.27) |
| 078 | Pneumonia | J12–J18 | 2711 | 1.12 (1.05–1.20) | 135 | 1.00 (0.64–1.55) |
| 084 | Emphysema | J43 | 612 | 1.01 (0.89–1.15) | 13 | 0.38 (0.09–1.72) |
| 086 | Other chronic lower respiratory disease | J44, J47 | 10,144 | 1.04 (1.00–1.07) | 180 | 1.78 (1.32–2.39) |
| 087 | Pneumoconiosis and chemical effects | J60–J66, J68 | 96 | 0.97 (0.66–1.42) | 11 | -- |
| 088 | Pneumonitis due to solids and liquids | J69 | 1236 | 0.97 (0.88–1.07) | 52 | 1.63 (0.78–3.41) |
| 089 | Other diseases of respiratory system | J00–J06, J30–J39, J67, J70–J98 | 2247 | 1.01 (0.94–1.09) | 112 | 0.84 (0.52–1.37) |
| 094 | Alcoholic liver disease | K70 | 640 | 0.99 (0.87–1.12) | 56 | 0.78 (0.38–1.62) |
| 095 | Other chronic liver disease and cirrhosis | K73–K74 | 652 | 1.05 (0.93–1.19) | 49 | 1.68 (0.82–3.46) |
| 096 | Cholelithiasis and other disorders of the gallbladder | K80–K82 | 298 | 1.00 (0.82–1.23) | 14 | 3.03 (0.33–27.90) |
| 100 | Renal failure | N17–N19 | 2366 | 1.05 (0.98–1.12) | 125 | 1.86 (1.21–2.83) |
| 110 | Symptoms, signs, and abnormal clinical and laboratory findings | R00–R99 | 1354 | 1.00 (0.91–1.11) | 41 | 0.47 (0.19–1.19) |
| 111 | All other diseases | D65–E07, E15–E34, E65–F99, G04–G12, G23–G25, G31–H93, K00–K22, K29–K31, K50–K66, K71–K72, K75–K76, K83–M99, N13.0–N13.5, N13.7–N13.9, N14, N15.0, N15.8–N15.9, N20–N23, N28–N39, N41–N64, N80–N98 | 18,946 | 1.00 (0.98–1.03) | 608 | 1.03 (0.86–1.23) |
| 114 | Motor vehicle accidents | V02–V04, V09.0, V09.2, V12–V14, V19.0–V19.2, V19.4–V19.6, V20–V79, V80.3–V80.5, V81.0–V81.1, V82.0–V82.1, V83–V86, V87.0–V87.8, V88.0–V88.8, V89.0, V89.2 | 658 | 0.91 (0.81–1.03) | 31 | 1.08 (0.45–2.61) |
| 118 | Falls | W00–W19 | 2739 | 0.97 (0.91–1.04) | 62 | 1.17 (0.67–2.06) |
| 122 | Accidental poisoning and exposure to noxious substances | X40–X49 | 224 | 0.92 (0.74–1.13) | 15 | 3.49 (0351–23.97) |
| 123 | Other and unspecified non-transport accidents | W20–W31, W35–W64, W75–W99, X10–X39, X50–X59, Y86 | 942 | 1.06 (0.95–1.18) | 47 | 1.76 (0.74–4.22) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wendt Hess, J.; Chan, W. Low-Level PM2.5 Exposure and Mortality in the Medicare Cohort: The Role of Native American Beneficiaries. Int. J. Environ. Res. Public Health 2025, 22, 1340. https://doi.org/10.3390/ijerph22091340
Wendt Hess J, Chan W. Low-Level PM2.5 Exposure and Mortality in the Medicare Cohort: The Role of Native American Beneficiaries. International Journal of Environmental Research and Public Health. 2025; 22(9):1340. https://doi.org/10.3390/ijerph22091340
Chicago/Turabian StyleWendt Hess, Judy, and Wenyaw Chan. 2025. "Low-Level PM2.5 Exposure and Mortality in the Medicare Cohort: The Role of Native American Beneficiaries" International Journal of Environmental Research and Public Health 22, no. 9: 1340. https://doi.org/10.3390/ijerph22091340
APA StyleWendt Hess, J., & Chan, W. (2025). Low-Level PM2.5 Exposure and Mortality in the Medicare Cohort: The Role of Native American Beneficiaries. International Journal of Environmental Research and Public Health, 22(9), 1340. https://doi.org/10.3390/ijerph22091340







