Healthcare Service Utilisation Across Continuum of Care for Type 2 Diabetes Among Culturally and Linguistically Diverse Populations: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
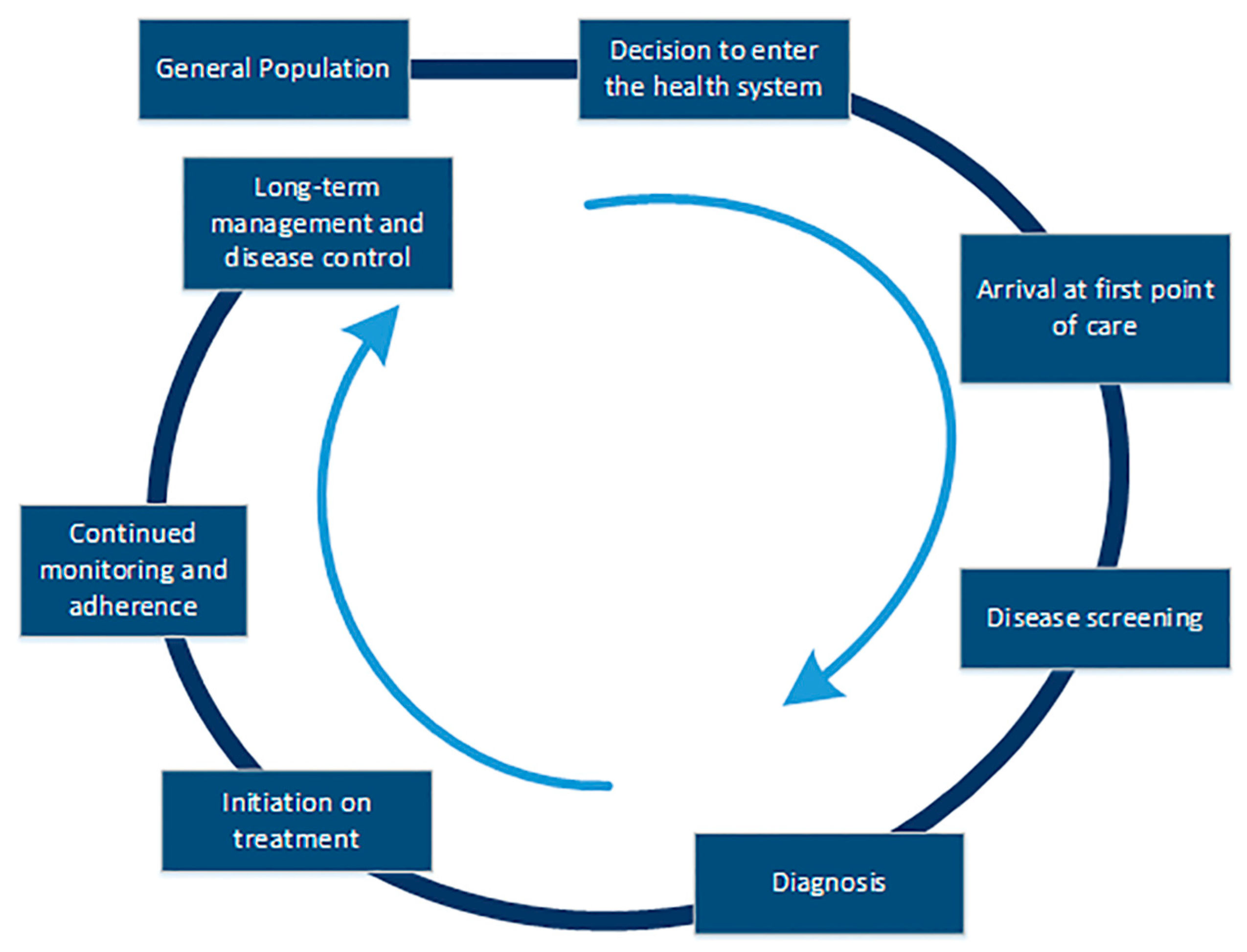
2.1. Design and Framework
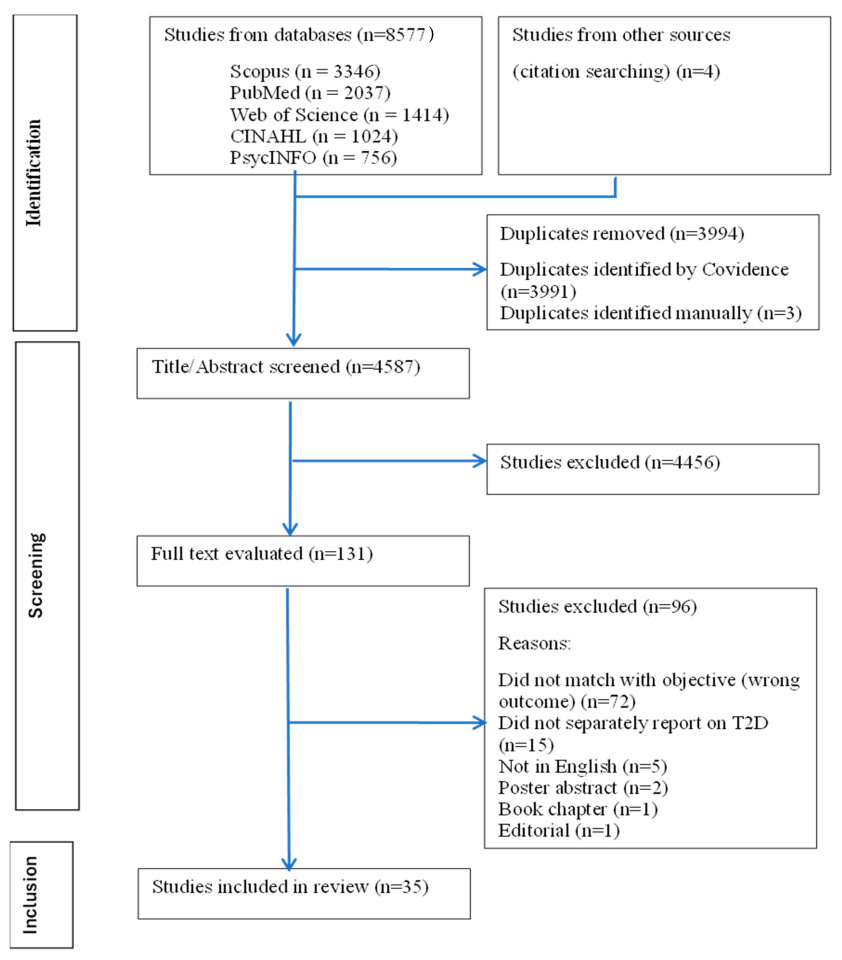
2.2. Search Strategy and Study Selection
2.3. Quality Appraisal
2.4. Data Extraction and Synthesis
3. Results
3.1. Barriers and Facilitators
3.2. Diagnosis
“Diabetes is a big stigma-related problem in our community, especially among the Black African community, because of the lack of awareness and ignorance of people. Going for treatment or diagnosis at the hospital is not always the first call for people because of the stigma. People self-diagnose, self-medicate, and some ignore it because of beliefs or other family commitment”(An African participant living with T2D in the UK [47])
3.3. Initiation of Treatment
“It’s a question of ethics, but also professionalism because if they make a mistake in the manipulation of the products, it can maybe cause a complete loss of eyesight.”(A Pakistani T2D patient living in Canada [56])
“I feel like they’re still a little bit hesitant about the western medication, which can be, you know, scary at times for them”(A Hmong American case manager providing services in the USA [48])
“A patient whose immigration case was in the process of being reviewed, and who was afraid that revealing her chronic illness by requesting government assistance to obtain supplies would jeopardise her chances of gaining US citizenship.”(A Diabetic Educator in the USA [41])
3.4. Continued Monitoring and Adherence
“The doctor doesn’t know what Karela (South Asian vegan recipe) is, you see, so he must give his advice grounded on his culture, his food-tradition, not ours”(A Pakistani T2D patient living in Norway [30])
“I don’t have money to buy the medicine, nor do I have a doctor to prescribe it. Here [referring to the free community clinic], we [referring to Hispanics] used to get medical attention, but not anymore.”(A Hispanic woman living in the USA [34])
“…Women did not use buses as they could not ask for directions or understand when to get off; moreover, buses were considered unsafe for women for fear of racist abuse or vulnerability to mugging”(Bangladeshi women with T2D, living in the UK [53])
“I don’t go to that doctor anymore because I heard the medication, they gave my friend stopped his kidneys working.”(A Maltese patient with T2D living in Australia [24])
“You ask questions but don’t know enough about particular habits to adequately respond to that. With Dutch people, often you know what they do and what they don’t do, but with migrants, this is more difficult”(A Dutch dietician [36])
“The first dietitian that I saw said, ‘Oh don’t take this, don’t take that’… then I was so anxious. [It] makes me not want to listen. But the second dietitian I spoke to know about our food. She had a model of fufu, so it makes me more welcome… that makes me more compliant listening to her because she knows what we eat.”(An African woman with T2D living in the UK [45])
“…because it’s really important that all my records and things are kept with the one doctor that I know”(A Tongan woman with T2D, living in Australia [51])
3.5. Long-Term Care and Management
“When it isn’t explained properly, you just do what you think is best… people need to be given advice that is closer to their own culture and language.”(A Turkish patient with T2D, living in Norway [29])
“No, the doctor (male) always rushes. I tell my daughter-in-law all my problems then she tells the nurse (female) everything openly. It’s easier to tell another woman but with the doctor it’s not possible”(A Bangladeshi woman with T2D, living in the UK [53])
“I didn’t know I needed to get my feet checked. I normally check my feet at home, the doctor doesn’t have time to teach you all the things you need to know”(A Maltese patient with T2D, living in Australia [24])
3.6. Narrative Synthesis of Quantitative Findings
4. Discussion
- Implications for Policy, Practice, and Future Research
- Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CALD | Culturally and linguistically diverse |
| CoC | Continuum of care |
| HSP | Health service provider |
| T2D | Type 2 diabetes |
References
- IDF Facts and Figures: International Diabetes Federation. 2024. Available online: https://idf.org/about-diabetes/diabetes-facts-figures/ (accessed on 10 January 2025).
- Ong, K.L.; Stafford, L.K.; McLaughlin, S.A.; Boyko, E.J.; Vollset, S.E.; Smith, A.E.; Dalton, B.E.; Duprey, J.; Cruz, J.A.; Hagins, H.; et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef]
- Mikhail, N.; Wali, S.; Brown, A.F. Ethnic disparities in diabetes. Endocrinol. Metab. Clin. 2021, 50, 475–490. [Google Scholar] [CrossRef]
- Nisar, M.; Uddin, R.; Kolbe-Alexander, T.; Khan, A. The prevalence of chronic diseases in international immigrants: A systematic review and meta-analysis. Scand. J. Public Health 2023, 51, 442–453. [Google Scholar] [CrossRef]
- Pham, T.T.L.; Berecki-Gisolf, J.; Clapperton, A.; O’Brien, K.S.; Liu, S.; Gibson, K. Definitions of culturally and linguistically diverse (CALD): A literature review of epidemiological research in Australia. Int. J. Environ. Res. Public Health 2021, 18, 737. [Google Scholar] [CrossRef] [PubMed]
- Marcus, K.; Balasubramanian, M.; Short, S.; Sohn, W. Culturally and linguistically diverse (CALD): Terminology and standards in reducing healthcare inequalities. Aust. N. Z. J. Public Health 2022, 46, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Goff, L.M. Ethnicity and type 2 diabetes in the UK. Diabet. Med. 2019, 36, 927–938. [Google Scholar] [CrossRef]
- Cheng, Y.J.; Kanaya, A.M.; Araneta, M.R.G.; Saydah, S.H.; Kahn, H.S.; Gregg, E.W.; Fujimoto, W.Y.; Imperatore, G. Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. JAMA 2019, 322, 2389–2398. [Google Scholar] [CrossRef] [PubMed]
- Statistics ABo. Characterisitcs of People with Diabetes 2023. Available online: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/diabetes/latest-release#characteristics-of-people-with-diabetes (accessed on 9 August 2025).
- Shamshirgaran, S.M.; Jorm, L.; Lujic, S.; Bambrick, H. Health related outcomes among people with type 2 diabetes by country of birth: Result from the 45 and Up Study. Prim. Care Diabetes 2019, 13, 71–81. [Google Scholar] [CrossRef]
- Golden, S.H.; Brown, A.; Cauley, J.A.; Chin, M.H.; Gary-Webb, T.L.; Kim, C.; Sosa, J.A.; Sumner, A.E.; Anton, B. Health disparities in endocrine disorders: Biological, clinical, and nonclinical factors—An Endocrine Society scientific statement. J. Clin. Endocrinol. Metab. 2012, 97, E1579–E1639. [Google Scholar] [CrossRef]
- Paduch, A.; Kuske, S.; Schiereck, T.; Droste, S.; Loerbroks, A.; Sørensen, M.; Maggini, M.; Icks, A. Psychosocial barriers to healthcare use among individuals with diabetes mellitus: A systematic review. Prim. Care Diabetes 2017, 11, 495–514. [Google Scholar] [CrossRef]
- Khatri, R.B.; Assefa, Y. Access to health services among culturally and linguistically diverse populations in the Australian universal health care system: Issues and challenges. BMC Public Health 2022, 22, 880. [Google Scholar] [CrossRef]
- Shahady, E. Recognizing and overcoming Barriers to effective Diabetes Care. Consultant 2009, 498, 331–339. [Google Scholar]
- Chan, K.-S.; Wan, E.Y.-F.; Chin, W.-Y.; Cheng, W.H.-G.; Ho, M.K.; Yu, E.Y.-T.; Lam, C.L.-K. Effects of continuity of care on health outcomes among patients with diabetes mellitus and/or hypertension: A systematic review. BMC Fam. Pract. 2021, 22, 145. [Google Scholar] [CrossRef]
- Gabert, R.; Ng, M.; Sogarwal, R.; Bryant, M.; Deepu, R.; McNellan, C.R.; Mehra, S.; Phillips, B.; Reitsma, M.; Thomson, B.; et al. Identifying gaps in the continuum of care for hypertension and diabetes in two Indian communities. BMC Health Serv. Res. 2017, 17, 846. [Google Scholar] [CrossRef]
- Zühlke, L.J.; Watkins, D.A.; Perkins, S.; Wyber, R.; Mwangi, J.; Markbreiter, J.; Moloi, H.S.; Engel, M.E.; Shato, T.; Hermanus, T.; et al. A Comprehensive Needs Assessment Tool for Planning Rheumatic Heart Disease Control Programs in Limited Resource Settings. Glob. Heart 2017, 12, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Wollum, A.; Gabert, R.; McNellan, C.R.; Daly, J.M.; Reddy, P.; Bhatt, P.; Bryant, M.; Colombara, D.V.; Naidoo, P.; Ngongo, B.; et al. Identifying gaps in the continuum of care for cardiovascular disease and diabetes in two communities in South Africa: Baseline findings from the HealthRise project. PLoS ONE 2018, 13, e0192603. [Google Scholar] [CrossRef] [PubMed]
- EVALUATION IFHMA. HealthRise Program 2024. Available online: https://www.healthdata.org/research-analysis/health-policy-planning/evaluations/healthrise (accessed on 16 March 2024).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Pace, R.; Pluye, P.; Bartlett, G.; Macaulay, A.C.; Salsberg, J.; Jagosh, J.; Seller, R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int. J. Nurs. Stud. 2012, 49, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Almansour, H.A.; Chaar, B.; Saini, B. Pharmacists’ perspectives about their role in care of patients with diabetes observing Ramadan. Res. Soc. Adm. Pharm. 2017, 13, 109–122. [Google Scholar] [CrossRef]
- Alzubaidi, H.; McNamara, K.; Browning, C.; Marriott, J. Barriers and enablers to healthcare access and use among Arabic-speaking and Caucasian English-speaking patients with type 2 diabetes mellitus: A qualitative comparative study. BMJ Open 2015, 5, e008687. [Google Scholar] [CrossRef]
- Barbara, S.; Krass, I. Self management of type 2 diabetes by Maltese immigrants in Australia: Can community pharmacies play a supporting role? Int. J. Pharm. Pract. 2013, 21, 305–313. [Google Scholar] [CrossRef]
- Biyikli Gültekin, E. Difficulties in health care for female Turkish immigrants with type 2 diabetes: A qualitative study in Vienna. Wien. Klin. Wochenschr. 2017, 129, 337–344. [Google Scholar] [CrossRef]
- Carolan-Olah, M.; Cassar, A. The experiences of older Italian migrants with type 2 diabetes: A qualitative study. J. Transcult. Nurs. 2018, 29, 172–179. [Google Scholar] [CrossRef]
- Cha, E.; Yang, K.; Lee, J.; Min, J.; Kim, K.H.; Dunbar, S.B.; Jennings, B.M. Understanding cultural issues in the diabetes self-management behaviors of Korean immigrants. Diabetes Educ. 2012, 38, 835–844. [Google Scholar] [CrossRef]
- Choi, T.S.T.; Walker, K.Z.; Palermo, C. Diabetes management in a foreign land: A case study on Chinese Australians. Health Soc. Care Community 2018, 26, e225–e232. [Google Scholar] [CrossRef] [PubMed]
- Cokluk, B.; Tokovska, M. Self-management of type 2 diabetes among Turkish immigrants in Norway: A focus group study. J. Public Health Res. 2023, 12, 22799036231154680. [Google Scholar] [CrossRef]
- Fagerli, R.A.; Lien, M.E.; Wandel, M. Experience of dietary advice among Pakistani-born persons with type 2 diabetes in Oslo. Appetite 2005, 45, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Gele, A.A.; Torheim, L.E.; Pettersen, K.S.; Kumar, B. Beyond culture and language: Access to diabetes preventive health services among Somali women in Norway. J. Diabetes Res. 2015, 2015, 549795. [Google Scholar] [CrossRef] [PubMed]
- Heisler, M.; Spencer, M.; Forman, J.; Robinson, C.; Shultz, C.; Palmisano, G.; Graddy-Dansby, G.; Kieffer, E. Participants’ assessments of the effects of a community health worker intervention on their diabetes self-management and interactions with healthcare providers. Am. J. Prev. Med. 2009, 37, S270–S279. [Google Scholar] [CrossRef]
- Ho, E.Y.; James, J. Cultural barriers to initiating insulin therapy in Chinese people with type 2 diabetes living in Canada. Can. J. Diabetes 2006, 30, 390–396. [Google Scholar] [CrossRef]
- Hu, J.; Amirehsani, K.; Wallace, D.C.; Letvak, S. Perceptions of Barriers in Managing Diabetes: Perspectives of Hispanic Immigrant Patients and Family Members. Diabetes Educ. 2013, 39, 494–503. [Google Scholar] [CrossRef]
- Hyman, I.; Patychuk, D.; Zaidi, Q.; Kljujic, D.; Shakya, Y.; Rummens, J.; Creatore, M.; Vissandjee, B. Self-management, health service use and information seeking for diabetes care among recent immigrants in Toronto. Chronic Dis. Inj. Can. 2012, 33, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Jager, M.; den Boeft, A.; Leij-Halfwerk, S.; van der Sande, R.; van den Muijsenbergh, M. Cultural competency in dietetic diabetes care—A qualitative study of the dietician’s perspective. Health Expect. Int. J. Public Particip. Health Care Health Policy 2020, 23, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Joo, J.; Lee, H. Barriers to and facilitators of diabetes self-management with elderly Korean-American immigrants. Int. Nurs. Rev. 2016, 63, 277–284. [Google Scholar] [CrossRef]
- Kokanovic, R.; Manderson, L. Social support and self-management of type 2 diabetes among immigrant Australian women. Chronic Illn. 2006, 2, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Kollannoor-Samuel, G.; Vega-López, S.; Chhabra, J.; Segura-Pérez, S.; Damio, G.; Pérez-Escamilla, R. Food insecurity and low self-efficacy are associated with health care access barriers among Puerto-Ricans with type 2 diabetes. J. Immigr. Minor. Health 2012, 14, 552–562. [Google Scholar] [CrossRef][Green Version]
- Leung, A.Y.M.; Bo, A.; Hsiao, H.Y.; Wang, S.S.; Chi, I. Health literacy issues in the care of Chinese American immigrants with diabetes: A qualitative study. BMJ Open 2014, 4, e005294. [Google Scholar] [CrossRef]
- Lipton, R.B.; Losey, L.M.; Giachello, A.; Mendez, J.; Girotti, M.H. Attitudes and issues in treating Latino patients with type 2 diabetes: Views of healthcare providers. Diabetes Educ. 1998, 24, 67–71. [Google Scholar] [CrossRef]
- Lu, Y.; Serpas, L.; Genter, P.; Anderson, B.; Campa, D.; Ipp, E. Divergent perceptions of barriers to diabetic retinopathy screening among patients and care providers, Los Angeles, California, 2014–2015. Prev. Chronic Dis. 2016, 13, E140. [Google Scholar] [CrossRef]
- Lyles, E.; Burnham, G.; Fahed, Z.; Shermock, K.M.; Spiegel, P.; Doocy, S. Care-Seeking and Health Service Utilization for Hypertension and Type 2 Diabetes Among Syrian Refugee and Host Community Care-Seekers in Lebanon. J. Int. Migr. Integr. 2022, 23, 519–541. [Google Scholar] [CrossRef]
- Carolan-Olah, M.C.; Cassar, A.; Quiazon, R.; Lynch, S. Diabetes care and service access among elderly Vietnamese with type 2 diabetes. BMC Health Serv. Res. 2013, 13, 447. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.P.; Rivas, C.A.; Harding, S.; Goff, L.M. Misalignment: Understanding the challenge of engaging with self-management advice for people living with diabetes in UK Black African and Caribbean communities. Health Educ. J. 2022, 81, 679–692. [Google Scholar] [CrossRef]
- Nam, S.; Song, H.-J.; Park, S.-Y.; Song, Y. Challenges of diabetes management in immigrant Korean Americans. Diabetes Educ. 2013, 39, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Omodara, D.A.; Gibson, L.; Bowpitt, G. Exploring the impact of cultural beliefs in the self-management of type 2 diabetes among black sub-saharan africans in the uk—A qualitative study informed by the pen-3 cultural model. Ethn. Health 2022, 27, 1358–1376. [Google Scholar] [CrossRef]
- Park, L.; Vang, A.; Yang, B.; Quanbeck, A. Barriers to Type 2 Diabetes Mellitus Management for Older Hmong Patients with Minimal English Language Skills: Accounts from Caregivers, Case Managers, and Clinicians. J. Racial Ethn. Health Disparities 2023, 10, 3062–3069. [Google Scholar] [CrossRef]
- Patel, T.; Umeh, K.; Poole, H.; Vaja, I.; Ramtoola, S.; Newson, L. Health professionals interface with cultural conflict in the delivery of type 2 diabetes care. Psychol. Health 2023, 38, 230–248. [Google Scholar] [CrossRef]
- Ramal, E.; Petersen, A.B.; Ingram, K.M.; Champlin, A.M. Factors that influence diabetes self-management in Hispanics living in low socioeconomic neighborhoods in San Bernardino, California. J. Immigr. Minor. Health 2012, 14, 1090–1096. [Google Scholar] [CrossRef]
- Kokanovic, R.; Manderson, L. Exploring doctor–patient communication in immigrant Australians with type 2 diabetes: A qualitative study. J. Gen. Intern. Med. 2007, 22, 459–463. [Google Scholar] [CrossRef]
- Renfrew, M.R.; Taing, E.; Cohen, M.J.; Betancourt, J.R.; Pasinski, R.; Green, A.R. Barriers to care for Cambodian patients with diabetes: Results from a qualitative study. J. Health Care Poor Underserved 2013, 24, 633–655. [Google Scholar] [CrossRef]
- Rhodes, P.; Nocon, A.; Wright, J. Access to diabetes services: The experiences of Bangladeshi people in Bradford, UK. Ethn. Health 2003, 8, 171–188. [Google Scholar] [CrossRef]
- Rose, V.K.; Harris, M.F. Experiences of self-management support from GPs among Australian ethnically diverse diabetes patients: A qualitative study. Psychol. Health Med. 2015, 20, 114–120. [Google Scholar] [CrossRef]
- Utz, S.W.; Steeves, R.H.; Wenzel, J.; Hinton, I.; Jones, R.A.; Andrews, D.; Muphy, A.; Oliver, M.N. ‘Working Hard With It’: Self-management of Type 2 Diabetes by Rural African Americans. Fam. Community Health J. Health Promot. Maint. 2006, 29, 195–205. [Google Scholar] [CrossRef]
- van Allen, Z.; Dogba, M.J.; Brent, M.H.; Bach, C.; Grimshaw, J.M.; Ivers, N.M.; Wang, X.; McCleary, N.; Asad, S.; Chorghay, Z.; et al. Barriers to and enablers of attendance at diabetic retinopathy screening experienced by immigrants to Canada from multiple cultural and linguistic minority groups. Diabet. Med. 2021, 38, e14429. [Google Scholar] [CrossRef] [PubMed]
- Becker, G.; Arnold, R. Stigma as a social and cultural construct. In The Dilemma of Difference: A Multidisciplinary View of Stigma; Springer: Berlin/Heidelberg, Germany, 1986; pp. 39–57. [Google Scholar]
- Gilani, A.; Furler, J. The challenges of managing diabetes in hard-to-reach groups. Diabetes Prim. Care Aust. 2016, 1, 43–49. [Google Scholar]
- Tewari, S.; Lin, S.S. Managing diabetes in CALD communities. Endocrinol. Today 2019, 8, 28–31. [Google Scholar]
- Brundisini, F.; Vanstone, M.; Hulan, D.; DeJean, D.; Giacomini, M. Type 2 diabetes patients’ and providers’ differing perspectives on medication nonadherence: A qualitative meta-synthesis. BMC Health Serv. Res. 2015, 15, 516. [Google Scholar] [CrossRef] [PubMed]
- Wens, J.; Vermeire, E.; Van Royen, P.; Sabbe, B.; Denekens, J. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: A qualitative analysis of barriers and solutions. BMC Fam. Pract. 2005, 6, 20. [Google Scholar] [CrossRef]
- Vergani, M.; Mansouri, F.; Weng, E.; Rajkobal, P. The effectiveness of ethno-specific and mainstream health services: An evidence gap map. BMC Health Serv. Res. 2022, 22, 879. [Google Scholar] [CrossRef]
- Hoverd, E.J.; Hawker-Bond, G.; Staniszewska, S.; Dale, J. Factors influencing decisions about whether to participate in health research by people of diverse ethnic and cultural backgrounds: A realist review. BMJ Open 2022, 12, e058380. [Google Scholar] [CrossRef]
- Seixas, B.V.; Regier, D.A.; Bryan, S.; Mitton, C. Describing practices of priority setting and resource allocation in publicly funded health care systems of high-income countries. BMC Health Serv. Res. 2021, 21, 90. [Google Scholar] [CrossRef]
| Studies | Approaches | Settings | Perspectives (Patients/Caregivers or Healthcare Providers or Both) | Sample Size | Type of Participants |
|---|---|---|---|---|---|
| Almansour et al., 2017 [22] | Qualitative | Australia | Healthcare Providers | 21 | Community pharmacist |
| Alzubaidi et al., 2015 [23] | Qualitative | Australia | Patients | 60 | Arabs |
| Barbara et al., 2013 [24] | Qualitative | Australia | Patients | 24 | Maltese |
| Biyikli et al., 2017 [25] | Qualitative | Austria | Patients | 13 | Turkish |
| Carolan-Olah et al., 2018 [26] | Qualitative | Australia | Patients | 13 | Italians |
| Cha et al., 2012 [27] | Qualitative | USA | Patients | 20 | Korean Americans |
| Choi et al., 2018 [28] | Qualitative | Australia | Both | 95 (Patients) + 15 (Healthcare Providers) | Chinese patients and dieticians |
| Cokluk et al., 2023 [29] | Qualitative | Norway | Patients | 13 | Turkish |
| Fagerli et al., 2005 [30] | Qualitative | Norway | Patients | 15 | Pakistani patients |
| Gele et al., 2015 [31] | Qualitative | Norway | Patients | 30 | Somalis |
| Heisler et al., 2009 [32] | Qualitative | USA | Patients | 40 | African American and Latinos |
| Ho et al., 2006 [33] | Qualitative | Canada | Patients | 5 | Chinese |
| Hu et al., 2013 [34] | Qualitative | USA | Patients | 36 (Patients) + 37 (Caregivers) | Mexican Hispanics |
| Hyman et al., 2012 [35] | Quantitative | Canada | Patients | 130 | Asian migrants |
| Jager et al., 2020 [36] | Qualitative | The Netherlands | Healthcare Providers | 12 | Dutch, Bulgarian, and Turkish dieticians |
| Joo et al., 2016 [37] | Qualitative | USA | Patients | 23 | Korean Americans |
| Kokanovic et al., 2006 [38] | Qualitative | Australia | Patients | 16 | Greek, Indian, Chinese, and Pacific Island backgrounds |
| Kollannoor-Samuel et al., 2012 [39] | Quantitative | USA | Patients | 211 | Puerto Ricans and Latinos |
| Leung et al., 2014 [40] | Qualitative | USA | Patients | 29 | Chinese |
| Lipton et al., 1998 [41] | Qualitative | USA | Healthcare Providers | 24 | Mexican, Puerto Rican, and Hispanic healthcare professionals (GPs and nurses) |
| Lu et al., 2016 [42] | Quantitative | USA | Both | 101 (Patients) + 44 (Healthcare Providers) | Hispanic and African American, healthcare providers and staff (not specified) |
| Lyles et al., 2022 [43] | Mixed methods | Lebanon | Both | 373 (Refugees) + 24 (Healthcare Providers) | Syrian refugees, healthcare providers (GP) |
| Carolan-Olah et al., 2013 [44] | Qualitative | Australia | Patients | 15 | Vietnamese |
| Moore et al., 2022 [45] | Qualitative | UK | Patients | 41 | African, Caribbean backgrounds |
| Nam et al., 2013 [46] | Qualitative | USA | Patients | 23 | Korean Americans |
| Omodara et al., 2022 [47] | Qualitative | UK | Patients | 36 | Sub-Saharans and Africans |
| Park et al., 2023 [48] | Qualitative | USA | Both | 13 (Caregivers) + 10 (Healthcare Providers) | Asian American, Hmong American caregivers and healthcare providers (not specified) |
| Patel et al., 2023 [49] | Qualitative | UK | Healthcare Providers | 14 | Asian healthcare providers (GPs, nurses, dieticians, podiatrists) |
| Ramal et al., 2012 [50] | Qualitative | USA | Patients | 27 | Hispanics |
| Kokanovic et al., 2007 [51] | Qualitative | Australia | Patients | 30 | Chinese, Indian, and South and Pacific Island backgrounds |
| Renfrew et al., 2013 [52] | Qualitative | USA | Both | 15 (Patients) + 30 (Healthcare Providers) | Cambodian patients and healthcare providers (GPs, nurses, dieticians) |
| Rhodes et al., 2003 [53] | Qualitative | UK | Patients | 12 | Bengalis |
| Rose et al., 2015 [54] | Qualitative | Australia | Patients | 28 | Arabs and Vietnamese |
| Utz et al., 2006 [55] | Qualitative | USA | Patients | 74 | African Americans |
| van Allen et al., 2021 [56] | Qualitative | Canada | Patients | 39 | Pakistanis, Chinese, and Africans |
| Stage of Continuum of Care | Barriers | Facilitators |
|---|---|---|
| Decision to enter the health system | No data available | No data available |
| First point of contact | No data available | No data available |
| Screening | No data available | No data available |
| Diagnosis | No data available | |
| Initiation of treatment |
| |
| Continued monitoring and adherence |
|
|
| Long-term care and management |
|
|
| Stage of Continuum of Care | Themes-Barriers | Themes-Facilitators |
|---|---|---|
| Decision to enter the health system | No data available | No data available |
| First point of contact | No data available | No data available |
| Screening | No data available | No data available |
| Diagnosis | No data available | No data available |
| Initiation of treatment | No data available | |
| Continued monitoring and adherence |
|
|
| Long-term care and management |
| No data available |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahman, M.; Khatri, R.B.; Gomersall, S.; Hossian, M.; Khan, A. Healthcare Service Utilisation Across Continuum of Care for Type 2 Diabetes Among Culturally and Linguistically Diverse Populations: A Systematic Review. Int. J. Environ. Res. Public Health 2025, 22, 1279. https://doi.org/10.3390/ijerph22081279
Rahman M, Khatri RB, Gomersall S, Hossian M, Khan A. Healthcare Service Utilisation Across Continuum of Care for Type 2 Diabetes Among Culturally and Linguistically Diverse Populations: A Systematic Review. International Journal of Environmental Research and Public Health. 2025; 22(8):1279. https://doi.org/10.3390/ijerph22081279
Chicago/Turabian StyleRahman, Mahfuzur, Resham B Khatri, Sjaan Gomersall, Mosharop Hossian, and Asaduzzaman Khan. 2025. "Healthcare Service Utilisation Across Continuum of Care for Type 2 Diabetes Among Culturally and Linguistically Diverse Populations: A Systematic Review" International Journal of Environmental Research and Public Health 22, no. 8: 1279. https://doi.org/10.3390/ijerph22081279
APA StyleRahman, M., Khatri, R. B., Gomersall, S., Hossian, M., & Khan, A. (2025). Healthcare Service Utilisation Across Continuum of Care for Type 2 Diabetes Among Culturally and Linguistically Diverse Populations: A Systematic Review. International Journal of Environmental Research and Public Health, 22(8), 1279. https://doi.org/10.3390/ijerph22081279








