Heat Risk Perception and Vulnerability in Puerto Rico: Insights for Climate Adaptation in the Caribbean
Abstract
1. Introduction
2. Materials and Methods
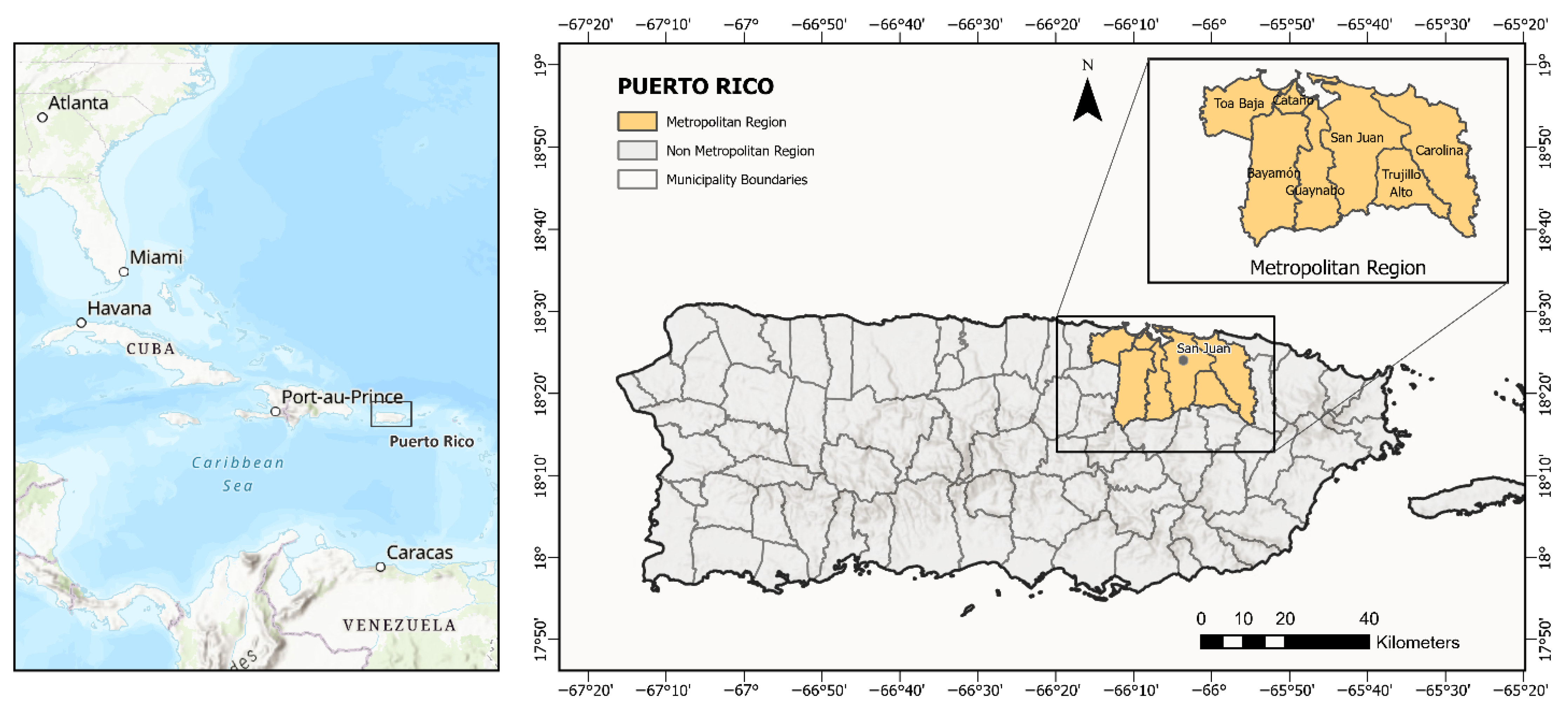
2.1. Study Area
2.2. Survey Methods
2.3. Data Analysis
3. Results
3.1. Sociodemographic Characteristics of the Participants
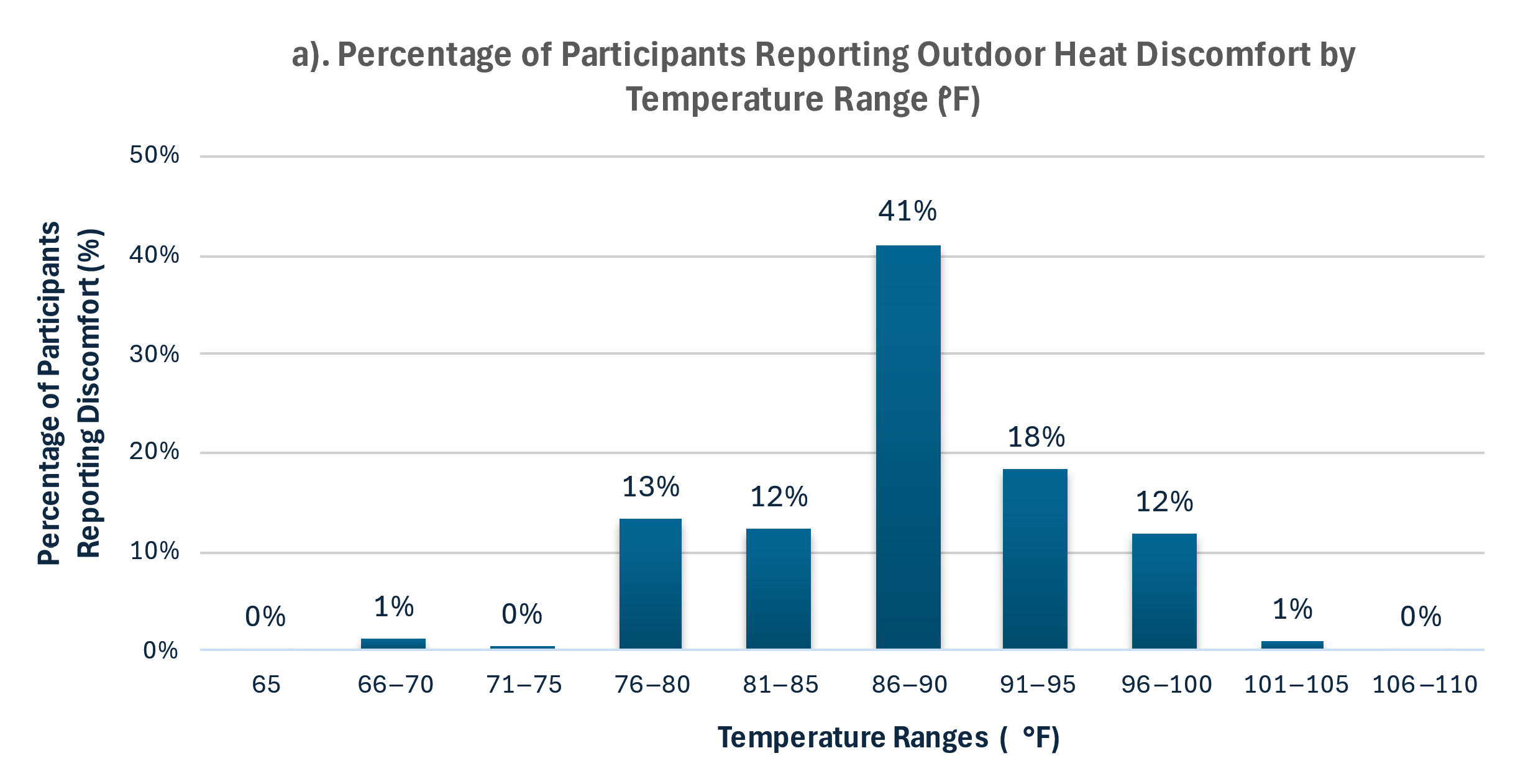
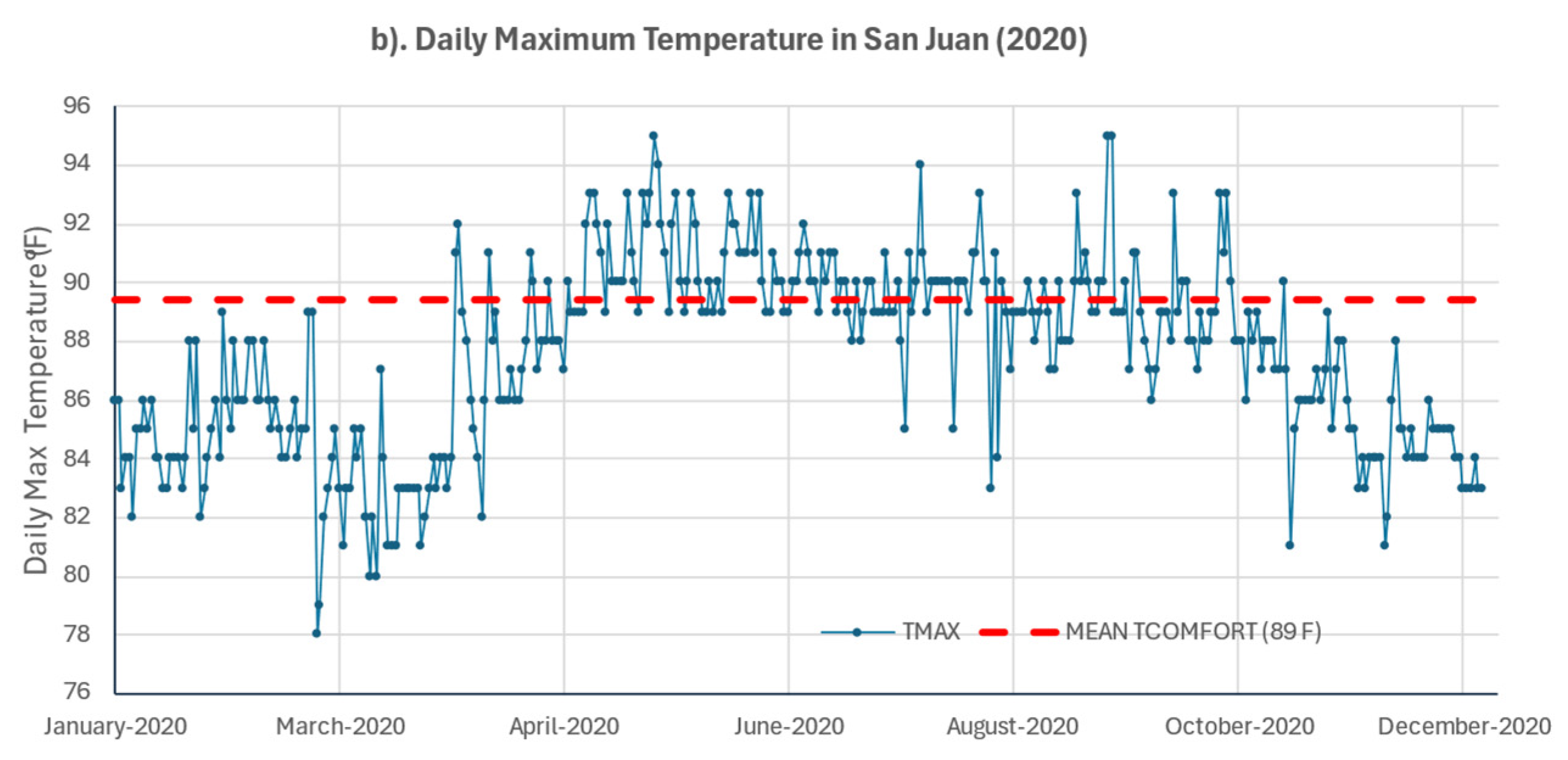
3.2. Reported Thermal Comfort Threshold
3.3. Health Risk Perception
3.4. Future Health Risk Perception
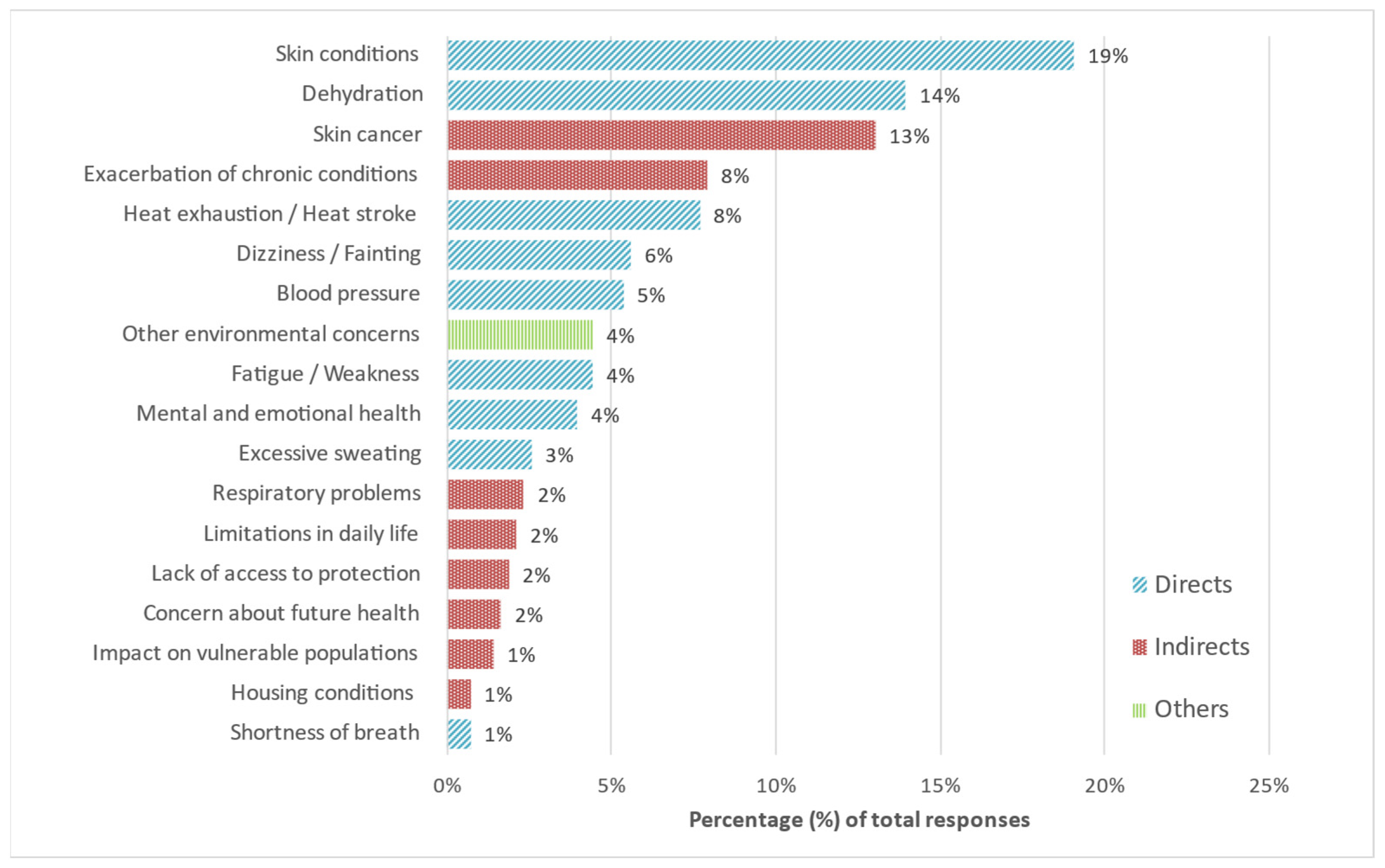
3.5. Self-Reported Concerns About High Temperatures
3.6. Perceived Heat Exposure
3.7. Heat-Related Behaviors
3.8. Predictors of Risk Perception and Heat Exposure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Domain/Variable | Description | Type | Survey Response Options | Analytical Coding |
|---|---|---|---|---|
| Sociodemographic and Socioeconomic (Social Determinants) | ||||
| Geographic region | Region in which the respondent resides, determined by the municipality of residence | Nominal | Municipality of residence (coded as 1–78) and grouped in two regions: Metropolitan (Bayamon, Carolina, Cataño, Guaynabo, San Juan, Toa Baja, and Trujillo Alto) and Non-metropolitan (confirmed by the rest of the municipalities) | (1) Metropolitan (2) Non-metropolitan |
| Age | Participant’s age in years | Categorical (ordinal) | Exact age recorded; age group selected by enumerator: (1) 21–34, (2) 35–49, (3) 50–64, or (4) 65 or more | (1) 21–34, (2) 35–49, (3) 50–64, or (4) 65 or more |
| Gender | Gender of the respondent at birth | Nominal | (1) Female, (2) Male, or (3) Other | (1) Female, (2) Male, or (3) Other |
| Employment Status | Employment Status | Nominal | (1) Employed, (2) Unemployed, (3) Retired, or (4) Unable to Work | (1) Employed, (2) Unemployed, (3) Retired, or (4) Unable to Work |
| Household Size | The total number of people currently living in the respondent′s household, including self. | Categorical (ordinal) | Any whole number | Recoded as (1) 1; (2) 2 to 3; (3) 4 or more |
| Household Income | The total annual household income (USD) from all sources, before taxes | Categorical (ordinal) | 1 = Less than $10,000 2 = $10,000–$14,999 3 = $15,000–$24,999 4 = $25,000–$34,999 5 = $35,000–$49,999 6 = $50,000–$74,999 7 = $75,000 or more | Same as collected |
| Educational Attainment | The highest level of education completed | Categorical (ordinal) | 1 = Less than high school 2 = High school diploma 3 = Bachelor’s degree 4 = Master’s degree 5 = Doctoral degree 6 = Other (open) | Recoded as (1) less than high school, (2) high school, (3) technical/vocational course or associate degree, (4) bachelor′s degree, or (5) master′s degree or doctoral degree |
| Health Insurance Coverage | Indicates whether the respondent has health insurance. | Binary (categorical) | 1 = Yes, private insurance 2 = Yes, government health plan (Plan VITAL, known as “La Reforma de Salud”) 3 = Yes, Medicare 4 = No health insurance | Recoded: 0 = No (response 4); 1 = Yes (responses 1–3) |
| Type of Health Insurance | Type of insurance among those with coverage | Categorical (nominal) | 1 = Yes, private insurance 2 = Yes, government health plan (Plan VITAL, known as “La Reforma de Salud”) 3 = Yes, Medicare 4 = No health insurance | Recoded: 1 = Private; 2 = Government; 3 = Medicare; response 4 (No) excluded |
| Health Status and Conditions | ||||
| Health Status | Self-rated general health status reported by the respondent | Categorical (ordinal) | 1 = Excellent 2 = Good 3 = Fair 4 = Poor 5 = Very Poor | Recoded: 1 = Excellent/Group (responses 1–2); 2 = Fair (response 3); 3 = Poor/Very Poor (responses 4–5) |
| Health Conditions (15 items) (Descriptive) | Health conditions reported by the respondent across 15 listed health conditions. | Categorical (nominal) | Yes/No | Used descriptively; conditions grouped in broader categories |
| Number of Health Conditions | The total number of conditions reported across 15 listed health conditions | Continuous (discrete) Categorical (ordinal) | Yes/No | The total count of “yes” responses. Grouped: 0 = None; 1 = 1 condition; 2 = 2–3; 3 = 4 or more |
| The Minimum Number of Health Conditions | Binary variables derived from the total number of reported health conditions, indicating whether the respondent had 1 or more, 2 or more, 3 or more, or 4 or more conditions. | Binary (categorical) | Derived from the total count of conditions (Yes responses) | Yes = 1 or No = 0 (for each threshold, 1, 2, 3, and 4) |
| Heat Risk Perception | ||||
| Perceived Health Risk | Self-reported level of concern about personal health during hot weather | Categorical (ordinal) | Likert scale from 1 to 5, where 1 = “Not concerned at all” and 5 = “Extremely concerned” | Recoded: 1 = Low (scores 1–2), 2 = Moderate (3), or 3 = High (scores 4–5) |
| Perceived Likelihood of Personal Illness | Perceived likelihood of experiencing a heat-related illness requiring medical attention within 5 years | Categorical (ordinal) | Likert scale from 1 to 5, where 1 = “Very unlikely” and 5 = “Very likely” | Recoded: 1 = Low (scores 1–2), 2 = Moderate (3), or 3 = High (scores 4–5) |
| Perceived Likelihood of Family Illness | Perceived likelihood of a family member experiencing a heat-related illness requiring medical attention within 5 years | Categorical (ordinal) | Likert scale from 1 to 5, where 1 = “Very unlikely” and 5 = “Very likely” | Recoded: 1 = Low (scores 1–2), 2 = Moderate (3), or 3 = High (scores 4–5) |
| Perceived Likelihood of Community Illness | Perceived likelihood of someone in the community experiencing a heat-related illness requiring medical attention within 5 years | Categorical (ordinal) | Likert scale from 1 to 5, where 1 = “Very unlikely” and 5 = “Very likely” | Recoded: 1 = Low (scores 1–2), 2 = Moderate (3), or 3 = High (scores 4–5) |
| Descriptive Heat Risk Perception | ||||
| Primary Reason for Heat Concern | Open-ended question where participants stated their main reason for concern during hot weather | Thematic categories (descriptive) | Open-ended response | Grouped: Direct health effects (responses indicating immediate physical symptoms or direct exposure to heat); indirect health effects (responses indicating secondary consequences or the worsening of existing conditions); other (environmental or other concerns) |
| Climate-Related Concerns | ||||
| Concern about Climate Change | Level of concern about climate change | Categorical (ordinal) | Likert scale from 1 to 5, where 1 = “Not concerned at all” and 5 = “Extremely concerned” | Recoded: 1 = Low (scores 1–2), 2 = Moderate (3), or 3 = High (scores 4–5) |
| Concern about Hot Temperatures | Level of concern about increasing hot temperatures | Categorical (ordinal) | Likert scale from 1 to 5, where 1 = “Not concerned at all” and 5 = “Extremely concerned” | Recoded: 1 = Low (scores 1–2), 2 = Moderate (3), or 3 = High (scores 4–5) |
| Concern about Heatwaves | Level of concern about extreme heat events or heatwaves | Categorical (ordinal) | Likert scale from 1 to 5, where 1 = “Not concerned at all” and 5 = “Extremely concerned” | Recoded: 1 = Low (scores 1–2), 2 = Moderate (3), or 3 = High (scores 4–5) |
| Perceived Heat Exposure | ||||
| Threshold Temperature for Outdoor Discomfort | Self-reported temperature (F) for outdoor heat discomfort based on combined responses from a structured and an open-ended question | Continuous (numeric) Binary (categorical) | Open numeric responses in °F or °C | Used as reported for descriptive analysis; values standardized to °F Grouped: 1 = Below 86 °F; 2 = 86 °F or higher |
| Frequency of Heat-Related Symptoms | The number of times the respondent experienced symptoms believed to be heat-related during summer, such as fainting, rapid heartbeat, hallucinations, confusion, dizziness, or muscle pain | Categorical (ordinal) | Open numeric response | Grouped: 1 = 1–2 times; 2 = 3–4 times; 3 = 5 or more |
| Experienced Heat-Related Symptoms | Binary indicator of whether the respondent experienced heat-related symptoms during the summer of 2020 | Binary (categorical) | Derived from the frequency of heat-related symptoms | 0 = No (frequency = 0); 1 = Yes (frequency ≥ 1) |
| Heat-Related Behaviors | ||||
| Frequency of Visits to a Public Space to Cool down | The frequency with which the respondent or household members visited public spaces (e.g., malls and restaurants) specifically to cool down during the summer of 2020 | Categorical (ordinal) | Five-point scale from 1 to 5, where 1 = “Never” to 5 = “Very frequently” | Recoded: 0 = Never (score 1); 1 = Low (scores 2–3), 2 = High (scores 4–5) |
| Visited a Public Space to Cool down | Binary indicator of whether respondents visited a public space to cool down | Binary (categorical) | Derived from 5-point scale responses | Recoded: 0 = No (score = 1); 1 = Yes (score ≥ 1) |
| Frequency: Slept in Uncomfortably Hot Temperatures | Frequency with which the respondent slept in uncomfortably hot temperatures during the summer of 2020 | Categorical (ordinal) | Five-point scale: 1 = Never, 2 = Rarely, 3 = Sometimes, 4 = Often, or 5 = Always | Recoded: 0 = Never (score 1); 1 = Low (scores 2–3); 2 = High (scores 4–5) |
| Slept in Uncomfortably Hot Temperatures | Binary indicator of whether respondents ever slept in uncomfortably hot temperatures | Binary (categorical) | Derived from frequency scale | Recoded: 0 = No (score 1); 1 = Yes (score ≥ 1) |
| Used AC | Used air conditioning at home to stay cool (predefined survey option: “Used air conditioning”) | Binary (categorical) | Selected/Not Selected | Recoded: 0 = No; 1 = Yes |
| Used Fans | Used fans at home to stay cool (predefined survey option: “Used ceiling fans or others”) | Binary (categorical) | Selected/Not Selected | Recoded: 0 = No; 1 = Yes |
| Opened Windows and Doors at Night | Opened windows and doors at night to stay cool (predefined survey option) | Binary (categorical) | Selected/Not Selected | Recoded: 0 = No; 1 = Yes |
| AC Usage (hours) | Average number of hours per day air conditioning was used during the summer of 2020 | Continuous (numeric) | Open numeric response | Grouped: 1 = < 8 h; 2 = 8–12; 3 = 13–24 h |
| Descriptive Heat-Related Behaviors | ||||
| Reduced AC Use Due to Finances | Whether financial limitations reduced AC use during the summer of 2020 | Categorical (nominal) | Yes/No | 0 = No; 1 = Yes |
| Unable to Pay Electricity Bill | Whether the household was unable to pay the electricity bill during the summer of 2020 | Categorical (nominal) | Yes/No | 0 = No; 1 = Yes |
| Alternative Energy or Generator | Whether the household has a generator or alternative energy system | Categorical (nominal) | 1 = Yes, has an electric or gas generator 2 = Yes, has an alternative energy system 3 = Does not have | Used as reported for descriptive analysis |
References
- Ebi, K.L.; Capon, A.; Berry, P.; Broderick, C.; de Dear, R.; Havenith, G.; Honda, Y.; Kovats, R.S.; Ma, W.; Malik, A.; et al. Hot weather and heat extremes: Health risks. Lancet 2021, 398, 698–708. [Google Scholar] [CrossRef]
- Haines, A.; Kovats, R.S.; Campbell-Lendrum, D.; Corvalán, C. Climate change and human health: Impacts, vulnerability and public health. Public Health 2006, 120, 585–596. [Google Scholar] [CrossRef] [PubMed]
- Hajat, S.; O’Connor, M.; Kosatsky, T. Health effects of hot weather: From awareness of risk factors to effective health protection. Lancet 2010, 375, 856–863. [Google Scholar] [CrossRef]
- Liu, T.; Xu, Y.J.; Zhang, Y.H.; Yan, Q.H.; Song, X.L.; Xie, H.Y.; Luo, Y.; Rutherford, S.; Chu, C.; Lin, H.L.; et al. Associations between risk perception, spontaneous adaptation behavior to heat waves and heatstroke in Guangdong province, China. BMC Public Health 2013, 13, 913. [Google Scholar] [CrossRef] [PubMed]
- Luber, G.; McGeehin, M. Climate Change and Extreme Heat Events. Am. J. Prev. Med. 2008, 35, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Lázaro, P.A.; Pérez-Cardona, C.M.; Rodríguez, E.; Martínez, O.; Taboas, M.; Bocanegra, A.; Méndez-Tejeda, R. Climate change, heat, and mortality in the tropical urban area of San Juan, Puerto Rico. Int. J. Biometeorol 2018, 62, 699–707. [Google Scholar] [CrossRef]
- Portier, C.; Tart, K.T.; Carter, S.; Dilworth, C.; Grambsch, A.; Gohlke, J.; Hess, J.; Howard, S.; Luber, G.; Lutz, J.; et al. A Human Health Perspective on Climate Change: A Report Outlining Research Needs on the Human Health Effects of Climate Change; Environmental Health Perspectives and National Institute of Environmental Health Sciences: Research Triangle Park, NC, USA, 2010.
- Salvador, C.; Gullón, P.; Franco, M.; Vicedo-Cabrera, A.M. Heat-related first cardiovascular event incidence in the city of Madrid (Spain): Vulnerability assessment by demographic, socioeconomic, and health indicators. Environ. Res. 2023, 226, 115698. [Google Scholar] [CrossRef]
- Romanello, M.; di Napoli, C.; Green, C.; Kennard, H.; Lampard, P.; Scamman, D.; Walawender, M.; Ali, Z.; Ameli, N.; Ayeb-Karlsson, S.; et al. Countdown The 2023 report of the Lancet Countdown on health and climate change: The imperative for a health-centred response in a world facing irreversible harms. Lancet 2023, 402, 2346–2394. [Google Scholar] [CrossRef]
- WHO. 2021 WHO Health and Climate Change Global Survey Report; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Hass, A.L.; Runkle, J.D.; Sugg, M.M. The driving influences of human perception to extreme heat: A scoping review. Environ. Res. 2021, 197, 111173. [Google Scholar] [CrossRef]
- Lwasa, S.; Seto, K.C.; Bai, X.; Blanco, H.; Gurney, K.R.; Kılkış, Ş.; Lucon, O.; Murakami, J.; Pan, J.; Sharifi, A.; et al. Urban Systems and Other Settlements. In IPCC, 2022: Climate Change 2022: Mitigation of Climate Change. Contribution of Working Group III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Shukla, P.R., Skea, J., Slade, R., Al Khourdajie, A., van Diemen, R., McCollum, D., Pathak, M., Some, S., Vyas, P., Fradera, R., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2022. [Google Scholar] [CrossRef]
- Akompab, D.A.; Bi, P.; Williams, S.; Grant, J.; Walker, I.A.; Augoustinos, M. Heat waves and climate change: Applying the health belief model to identify predictors of risk perception and adaptive behaviours in Adelaide, Australia. Int. J. Environ. Res. Public Health 2013, 10, 2164–2184. [Google Scholar] [CrossRef]
- Ban, J.; Shi, W.; Cui, L.; Liu, X.; Jiang, C.; Han, L.; Wang, R.; Li, T. Health-risk perception and its mediating effect on protective behavioral adaptation to heat waves. Environ. Res. 2019, 172, 27–33. [Google Scholar] [CrossRef]
- Cutler, M.J.; Marlon, J.R.; Howe, P.D.; Leiserowitz, A. The influence of political ideology and socioeconomic vulnerability on perceived health risks of heat waves in the context of climate change. Weather. Clim. Soc. 2018, 10, 731–746. [Google Scholar] [CrossRef]
- Hass, A.L.; Ellis, K.N. Motivation for heat adaption: How perception and exposure affect individual behaviors during hot weather in Knoxville, Tennessee. Atmosphere 2019, 10, 591. [Google Scholar] [CrossRef]
- Li, H.; Guan, J.; Ye, H.; Yang, H. A survey of rural residents’ perception and response to health risks from hot weather in ethnic minority areas in southwest china. Int. J. Environ. Res. Public Health 2019, 16, 2190. [Google Scholar] [CrossRef]
- Ye, H.; Ma, J.; Wu, Y.; Zhang, Y. Perceptions of health risks from hot weather, and coping behaviors among ethnic minority groups in mountain areas of China: A case study in the tujia and Miao Autonomous Prefecture. Int. J. Environ. Res. Public Health 2018, 15, 2498. [Google Scholar] [CrossRef]
- Howe, P.D.; Marlon, J.R.; Wang, X.; Leiserowitz, A. Public perceptions of the health risks of extreme heat across US states, counties, and neighborhoods. Proc. Natl. Acad. Sci. USA 2019, 116, 6743–6748. [Google Scholar] [CrossRef] [PubMed]
- Rise, N.; Oura, C.; Drewry, J. Climate change and health in the Caribbean: A review highlighting research gaps and priorities. J. Clim. Change Health 2022, 8, 100126. [Google Scholar] [CrossRef]
- Rafael, M.-T.; Santos-Corrada, M.; Sandra, M. Perceptions of Climate Change in Puerto Rico before and after Hurricane Maria. Am. J. Clim. Change 2021, 10, 153–166. [Google Scholar] [CrossRef]
- Santos-Corrada, M.; Méndez-Tejeda, R. Public perception of climate change in a period of economic crisis in Puerto Rico. AIMS. Environ. Sci. 2017, 4, 83–93. [Google Scholar] [CrossRef]
- Estudios Tecnicos Inc. Estudio de Percepción Pública sobre el Riesgo y la Resiliencia al Cambio Climatico en Puerto Rico: Informe Final; Estudios Tecnicos Inc.: San Juan, Puerto Rico, 2018. [Google Scholar]
- Runkle, J.; Kunkel, K.E.; Stevens, L.E.; Champion, S.M.; Easterling, D.R.; Terando, A.; Sun, L.; Stewart, B.C.; Landers, G.; Rayne, S. Puerto Rico and the U.S. Virgin Islands State Climate Summary 2022; NOAA Technical Report NESDIS 150-PR; NOAA National Centers for Environmental Information: Silver Spring, MD, USA, 2022; pp. 1–5.
- Di Napoli, C.; Allen, T.; Méndez-Lázaro, P.A.; Pappenberger, F. Heat stress in the Caribbean: Climatology, drivers, and trends of human biometeorology indices. Int. J. Climatol. 2023, 43, 405–425. [Google Scholar] [CrossRef]
- Skinner, C.S.; Tiro, J.; Champion, V.L. The Health Belief Model. In Health Behavior: Theory, Research, and Practice; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: San Francisco, CA, USA, 2015; pp. 75–94. [Google Scholar]
- CEACC. Borrador Final del Plan de Mitigación, Adaptación y Resiliencia al Cambio Climático en Puerto Rico; Comité Expertos y Asesores Sobre Cambio Climático (CEACC): San Juan, PR, USA, 2024.
- Méndez-Lázaro, P.; Martínez-Sánchez, O.; Méndez-Tejeda, R.; Rodríguez, E.; Morales, E.; Schmitt-Cortijo, N. Extreme Heat Events in San Juan Puerto Rico: Trends and Variability of Unusual Hot Weather and its Possible Effects on Ecology and Society. J. Climatol. Weather. Forecast. 2015, 3, 2. [Google Scholar] [CrossRef]
- Brick, J.M.; Waksberg, J. Avoiding sequential sampling with random digit dialing. Surv. Methodol 1991, 17, 21–41. [Google Scholar]
- Patle, S.; Ghuge, V.V. Evolution and Performance Analysis of Thermal Comfort Indices for Tropical and Subtropical Region: A Comprehensive Literature Review. Int. J. Environ. Sci. Technol. 2024, 21, 10217–10258. [Google Scholar] [CrossRef]
- Johansson, E.; Yahia, M.W.; Arroyo, I.; Bengs, C. Outdoor thermal comfort in public space in warm-humid Guayaquil, Ecuador. Int. J. Biometeorol 2018, 62, 387–399. [Google Scholar] [CrossRef] [PubMed]
- Ratwatte, P.; Wehling, H.; Kovats, S.; Landeg, O.; Weston, D. Factors associated with older adults’ perception of health risks of hot and cold weather event exposure: A scoping review. Front. Public Health 2022, 10, 939859. [Google Scholar] [CrossRef]
- Sheridan, S.C. A survey of public perception and response to heat warnings across four North American cities: An evaluation of municipal effectiveness. Int. J. Biometeorol 2007, 52, 3–15. [Google Scholar] [CrossRef]
- Dahl, K.; Spanger-Siegfried, E.; Licker, R.; Caldas, A.; Abatzoglou, J.; Mailloux, N.; Cleetus, R.; Udvardy, S. Killer Heat in the United States: Climate Choices and the Future of Dangerously Hot Days; Union of Concerned Scientists: Cambridge, MA, USA, 2019. [Google Scholar]
| Category | Persons 21 Years of Age or Older (Puerto Rico) 1 | Percentage (%) | Persons Sampled 2 |
|---|---|---|---|
| By Region | |||
| Metropolitan | 725,277 | 28.4% | 142 |
| Non-metropolitan | 1,827,386 | 71.6% | 358 |
| Total (Region) | 2,552,663 | 100% | 500 |
| By Gender and Age Group | |||
| Men 21 to 34 Years | 301,079 | 11.8% | 59 |
| Men 35 to 49 Years | 304,859 | 11.9% | 60 |
| Men 50 to 64 Years | 302,698 | 11.9% | 59 |
| Men 65 Years or More | 278,729 | 10.9% | 55 |
| Women 21 to 34 Years | 309,238 | 12.1% | 60 |
| Women 35 to 49 Years | 337,954 | 13.2% | 66 |
| Women 50 to 64 Years | 356,212 | 14.0% | 70 |
| Women 65 Years or More | 361,894 | 14.2% | 71 |
| Total (Gender and Age) | 2,552,663 | 100% | 500 |
| Variable | Category | Frequency (N) | Percentage (%) |
|---|---|---|---|
| Region | Metropolitan | 142 | 28.4% |
| Non-metropolitan | 358 | 71.6% | |
| Gender | Female | 233 | 46.6% |
| Male | 267 | 53.4% | |
| Age (Years) | 21–34 | 119 | 23.8% |
| 35–49 | 126 | 25.2% | |
| 50–64 | 129 | 25.8% | |
| 65 or More | 126 | 25.2% | |
| Education (N = 498) | Less Than High School | 52 | 10.4% |
| High School | 141 | 28.3% | |
| Assoc. Degree/Certificate | 78 | 15.7% | |
| Bachelor’s Degree | 156 | 31.3% | |
| Master’s or Doctoral Degree | 71 | 14.3% | |
| Employment Status (N = 490) | Employed | 207 | 42.2% |
| Unemployed | 103 | 21.0% | |
| Retired | 151 | 30.8% | |
| Unable to Work | 39 | 8.0% | |
| Work Environment (N = 207) | Interior | 131 | 63.3% |
| Exterior | 29 | 14.0% | |
| Interior/Exterior | 47 | 22.7% | |
| Persons per Household | 1 | 93 | 18.6% |
| 2 to 3 | 281 | 56.2% | |
| 4 or More | 126 | 25.2% | |
| Health Insurance (N = 495) | Yes | 472 | 95.4% |
| No | 23 | 4.6% | |
| Type of Health Insurance (N = 495) | Private | 226 | 45.7% |
| Public (Reforma) | 155 | 31.3% | |
| Medicare | 91 | 18.4% | |
| No Insurance | 23 | 4.6% |
| Household Size (Number of Persons) | |||||||
|---|---|---|---|---|---|---|---|
| Age Group | One (1) | Percentage (%) | Two to Three | Percentage (%) | Four or More | Percentage (%) | Total |
| 21–34 Years | 14 | 12% | 63 | 53% | 42 | 35% | 119 |
| 35–49 Years | 17 | 13% | 65 | 52% | 44 | 35% | 126 |
| 50–64 Years | 28 | 22% | 75 | 58% | 26 | 20% | 129 |
| 65+ Years | 34 | 27% | 78 | 62% | 14 | 11% | 126 |
| Total | 93 | 281 | 126 | 500 | |||
| Variable | Category | Frequency (N) | Percentage (%) |
|---|---|---|---|
| Health Status (Self-Reported) (N = 499) | Excellent/Good | 346 | 69.3% |
| Fair | 127 | 25.5% | |
| Poor/Very Poor | 26 | 5.2% | |
| Number of Health Conditions (N = 498) | None | 147 | 29.5% |
| 1 | 127 | 25.5% | |
| 2 to 3 | 133 | 26.7% | |
| 4 or More | 91 | 18.3% | |
| Type of Health Conditions (N = 498) | Cardiovascular | 199 | 40.0% |
| Metabolic | 151 | 30.3% | |
| Respiratory | 116 | 23.3% | |
| Neurological and Sleep Disorders | 188 | 37.8% | |
| Mental Health | 38 | 7.6% | |
| Other Chronic Conditions | 35 | 7.0% |
| Variable | Category | Frequency (N) | Percentage (%) |
|---|---|---|---|
| Perceived Health Risk (N = 499) | Low | 157 | 31.5% |
| Moderate | 107 | 21.4% | |
| High | 235 | 47.1% | |
| Perceived Personal Likelihood of Heat-Related Illness (5 Years) (N = 479) | Low | 277 | 57.8% |
| Moderate | 84 | 17.5% | |
| High | 118 | 24.6% | |
| Perceived Family-Level Likelihood of Heat-Related Illness (5 Years) (N = 455) | Low | 266 | 58.5% |
| Moderate | 83 | 18.2% | |
| High | 106 | 23.3% | |
| Perceived Community-Level Likelihood of Heat-Related Illness (5 Years) (N = 329) | Low | 154 | 46.8% |
| Moderate | 80 | 24.3% | |
| High | 95 | 28.9% | |
| Climate-Change Concern (N = 497) | Low | 41 | 8.2% |
| Moderate | 61 | 12.3% | |
| High | 395 | 79.5% | |
| High-Temperature Concern (N = 500) | Low | 49 | 9.8% |
| Moderate | 59 | 11.8% | |
| High | 392 | 78.4% | |
| Heatwave Concern (N = 499) | Low | 56 | 11.2% |
| Moderate | 62 | 12.4% |
| Variable | Perceived Health Risk | Future Personal Risk 1 | Future Family Risk 1 | Future Community Risk 1 |
|---|---|---|---|---|
| Region | 0.047 | 0.090 | 0.184 | 0.370 |
| Age | <0.001 | 0.001 | 0.073 | 0.336 |
| Gender | <0.001 | <0.001 | 0.024 | 0.183 |
| Educational Attainment | 0.142 | 0.023 | 0.242 | 0.480 |
| Employment Status | 0.009 | 0.002 | 0.002 | 0.222 |
| Occupational Environment | 0.293 | 0.138 | 0.040 | 0.643 |
| Health Status | 0.015 | <0.001 | 0.031 | 0.132 |
| Number of Health Conditions | 0.001 | <0.001 | 0.074 | 0.039 |
| 2 or More Chronic Conditions | 0.031 | <0.001 | 0.015 | 0.007 |
| 3 or More Chronic Conditions | 0.002 | <0.001 | 0.005 | 0.029 |
| 4 or More Chronic Conditions | <0.001 | <0.001 | 0.093 | 0.313 |
| Experienced Heat-Related Symptoms | <0.001 | <0.001 | <0.001 | <0.001 |
| Experienced Heat Discomfort while Sleeping | 0.018 | 0.006 | <0.001 | <0.001 |
| Visit Public Place (to Cool Off) | 0.312 | 0.385 | 0.008 | 0.045 |
| Variable | Category | Frequency (N) | Percentage (%) |
|---|---|---|---|
| Experienced Heat-Related Symptoms (N = 500) | No | 282 | 56.4% |
| Yes | 218 | 43.6% | |
| Frequency of Symptoms (N = 218) | 1–2 times | 97 | 44.5% |
| 2–4 times | 74 | 33.9% | |
| 5 or more | 47 | 21.6% | |
| Visited Public Places to Cool Off (N = 496) | No | 275 | 55.4% |
| Yes | 221 | 44.6% | |
| Frequency of Visits (N = 221) | Low | 139 | 62.9% |
| High | 82 | 37.1% | |
| Experienced Heat Discomfort while Sleeping (N = 498) | No | 159 | 31.9% |
| Yes | 339 | 68.1% | |
| Frequency Heat Discomfort while Sleeping (N = 339) | Low | 233 | 68.7% |
| High | 106 | 31.3% | |
| Heat Mitigation Behaviors (N = 497) | AC | 319 | 64.2% |
| Fans | 418 | 84.1% | |
| Window/Door Opening | 197 | 39.6% | |
| Others | 23 | 4.6% | |
| AC Usage (Hours per Day) (N = 306) | <8 h | 59 | 19.3% |
| 8–12 h | 109 | 35.6% | |
| 13–24 h | 138 | 45.1% | |
| Uncomfortable Outdoor Temperature (N = 408) | ≤85 °F | 112 | 27.5% |
| ≥86 °F | 296 | 72.5% |
| Health Risk Perception (Category with the Highest Percentage (%)) | |||||
| Variable | High | Percentage (%) | Low | Percentage (%) | p-Value * |
| Region | Non-metropolitan | 48.7 | Metropolitan | 39.4 | 0.047 |
| Gender | Male | 55.8 | Female | 37.9 | <0.001 |
| Age (Years) | 50–64 | 63.3 | 65+ | 38.9 | <0.001 |
| Educational Level | <High School | 59.6 | Graduate Studies | 38 | 0.142 |
| Persons per Household | 4 or More | 49.6 | 1 (Living Alone) | 40.6 | 0.310 |
| Employment Status | Unable to Work | 75.0 | Retired | 35.1 | 0.009 |
| Working Environment | Exterior | 55.2 | Interior | 38.2 | 0.293 |
| Health Status | Regular | 58.7 | Excellent/Good | 35.8 | 0.015 |
| Number of Conditions | 4 or More | 65.6 | None | 35.4 | 0.001 |
| Heat-Related Symptoms | Yes | 66.8 | No | 43.3 | <0.001 |
| Uncomfortable Sleep Temp. | Yes | 50.9 | No | 39.6 | 0.018 |
| Thermal Discomfort | <86 °F | 51.8 | ≥86 °F | 27.8 | 0.856 |
| Heat-Related Symptoms (Category with the Highest Percentage (%)) | |||||
| Variable | Yes | Percentage (%) | No | Percentage (%) | p-Value * |
| Region | Non-metropolitan | 45.5 | Metropolitan | 61.3 | 0.167 |
| Gender | Male | 48.3 | Female | 61.8 | 0.023 |
| Age (Years) | 50–64 | 51.9 | 65+ | 61.1 | 0.149 |
| Educational Level | <High School | 59.6 | Graduate Studies | 66.2 | 0.034 |
| Persons per Household | 4 or More | 48.4 | 2 to 3 | 58.7 | 0.405 |
| Employment Status | Unable to Work | 69.0 | Employed | 61.4 | 0.010 |
| Working Environment | Interior/Exterior | 46.8 | Interior | 64.9 | 0.350 |
| Health Status | Regular | 67.7 | Excellent/Good | 66.5 | <0.001 |
| Number of Conditions | 4 or More | 67.0 | None | 70.1 | <0.001 |
| Uncomfortable Sleep Temp. | Yes | 48.7 | No | 67.3 | <0.001 |
| Thermal Discomfort | <86 °F | 52.7 | ≥86 °F | 53.7 | 0.249 |
| OR (Adjusted) | 95% CI | p-Value | |
|---|---|---|---|
| 1. Perceived Health Risk Associated with Heat | |||
| Region | |||
| Metropolitan | 1.00 | ||
| Non-metropolitan | 1.69 | (1.00, 2.84) | 0.047 |
| Age | |||
| 21–34 Years | 1.00 | ||
| 35–49 Years | 1.40 | (0.73,2.70) | 0.319 |
| 50–64 Years | 3.59 | (1.66, 7.77) | 0.001 |
| 65+ Years | 1.29 | (0.50, 3.33) | 0.596 |
| Gender | |||
| Female | 1.00 | ||
| Male | 2.00 | (1.24, 3.23) | 0.005 |
| Experienced Heat-Related Symptoms | |||
| No | 1.00 | ||
| Yes | 4.94 | (2.93, 8.34) | 0.000 |
| (Number of obs. = 484; LR chi2 (30) = 126.04; prob. > chi2 = <0.001; pseudo R2 = 0.1246) | |||
| 2. Perceived Individual Risk of Heat-Related Illness (5 Years) | |||
| Age | |||
| 21–34 Years | 1.00 | ||
| 35–49 Years | 1.45 | (0.63, 3.38) | 0.385 |
| 50–64 Years | 2.78 | (1.25, 6.19) | 0.012 |
| 65+ Years | 0.959 | (0.39, 2.34) | 0.928 |
| Gender | |||
| Female | 1.00 | ||
| Male | 3.28 | (1.81, 5.93) | 0.000 |
| Experienced Heat-Related Symptoms | |||
| No | 1.00 | ||
| Yes | 2.98 | (1.66, 5.36) | 0.000 |
| (Number of obs. = 385; LR chi2 (34) = 109.39; prob. > chi2 = <0.001; pseudo R2 = 0.1433) | |||
| 3. Perceived Family Risk of Heat-Related Illness (5 Years) | |||
| Gender | |||
| Female | 1.00 | ||
| Male | 1.82 | (1.01, 3.27) | 0.045 |
| Experienced Heat-Related Symptoms | |||
| No | 1.00 | ||
| Yes | 3.43 | (1.91, 6.16) | 0.000 |
| (Number of obs. = 352; LR chi2 (34) = 77.77; prob. > chi2 = <0.001; pseudo R2 = 0.1108) | |||
| 4. Perceived Community Risk of Heat-Related Illness (5 Years) | |||
| Experienced Heat-Related Symptoms | |||
| No | 1.00 | ||
| Yes | 2.56 | (1.42, 4.62) | 0.002 |
| Slept in Heat Discomfort | |||
| No | 1.00 | ||
| Yes | 2.53 | (1.34, 4.79) | 0.004 |
| (Number of obs. = 321; LR chi2 (26) = 57.01; prob. > chi2 = 0.004; pseudo R2 = 0.0840) | |||
| Variable | Unadjusted OR | (95% CI) | p-Value | Adjusted OR * | (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Female | 1.00 | |||||
| Male | 1.51 | (1.06, 2.16) | 0.023 | 1.37 | (0.89, 2.11) | 0.150 |
| Education | ||||||
| Less Than High School | 1.00 | 1.00 | ||||
| High School | 0.53 | (0.28, 1.01) | 0.055 | 0.71 | (0.32, 1.58) | 0.396 |
| Associate Degree or Certificate | 0.68 | (0.33, 1.38) | 0.282 | 1.07 | (0.44, 2.60) | 0.878 |
| Bachelor′s Degree | 0.45 | (0.24, 0.85) | 0.014 | 0.81 | (0.34, 1.92) | 0.636 |
| Graduate Degree | 0.35 | (0.16, 0.73) | 0.005 | 0.70 | (0.27, 1.86) | 0.479 |
| Employment Status | ||||||
| Employed | 1.00 | 1.00 | ||||
| Unemployed | 1.5 | (0.93, 2.41) | 0.097 | 0.89 | (0.49, 1.63) | |
| Retired | 1.07 | (0.70, 1.65) | 0.738 | 0.87 | (0.41, 1.86) | |
| Unable to Work | 3.52 | (1.53, 8.13) | 0.003 | 1.15 | (0.41, 3.29) | 0.788 |
| Health Status | ||||||
| Excellent/Good | 1.00 | |||||
| Fair | 4.15 | (2.70, 6.42) | 0.000 | 3.07 | (1.79, 5.25) | 0.000 |
| Poor/Very Poor | 3.17 | (1.39, 7.21) | 0.006 | 2.08 | (0.73, 5.90) | 0.170 |
| Number of Chronic Conditions | ||||||
| None | 1.00 | |||||
| 1 Condition | 1.38 | (0.83, 2.28) | 0.216 | 1.30 | (0.74, 2.33) | 0.360 |
| 2–3 Conditions | 2.30 | (1.41, 3.76) | 0.001 | 1.95 | (1.07, 3.56) | 0.029 |
| 4 or More Conditions | 4.75 | (2.71, 8.35) | 0.000 | 3.09 | (1.48, 6.42) | 0.003 |
| Health Insurance Type | ||||||
| Private | 1.00 | |||||
| Public (Reforma) | 1.97 | (1.31, 2.99) | 0.001 | 1.29 | (0.76, 2.21) | 0.338 |
| Medicare | 1.06 | (0.65, 1.75) | 0.803 | |||
| Slept in Heat Discomfort | ||||||
| No | 1.00 | |||||
| Yes | 1.95 | (1.32, 2.89) | 0.001 | 2.11 | (1.31, 3.41) | 0.002 |
| Use AC | ||||||
| No | 1.00 | |||||
| Yes | 0.62 | (0.43, 0.90) | 0.012 | 0.84 | (0.51, 1.39) | 0.508 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guzman-Colon, B.; Guido, Z.; Amaya-Ardila, C.P.; Cabrera-Rivera, L.T.; Méndez-Lázaro, P.A. Heat Risk Perception and Vulnerability in Puerto Rico: Insights for Climate Adaptation in the Caribbean. Int. J. Environ. Res. Public Health 2025, 22, 1197. https://doi.org/10.3390/ijerph22081197
Guzman-Colon B, Guido Z, Amaya-Ardila CP, Cabrera-Rivera LT, Méndez-Lázaro PA. Heat Risk Perception and Vulnerability in Puerto Rico: Insights for Climate Adaptation in the Caribbean. International Journal of Environmental Research and Public Health. 2025; 22(8):1197. https://doi.org/10.3390/ijerph22081197
Chicago/Turabian StyleGuzman-Colon, Brenda, Zack Guido, Claudia P. Amaya-Ardila, Laura T. Cabrera-Rivera, and Pablo A. Méndez-Lázaro. 2025. "Heat Risk Perception and Vulnerability in Puerto Rico: Insights for Climate Adaptation in the Caribbean" International Journal of Environmental Research and Public Health 22, no. 8: 1197. https://doi.org/10.3390/ijerph22081197
APA StyleGuzman-Colon, B., Guido, Z., Amaya-Ardila, C. P., Cabrera-Rivera, L. T., & Méndez-Lázaro, P. A. (2025). Heat Risk Perception and Vulnerability in Puerto Rico: Insights for Climate Adaptation in the Caribbean. International Journal of Environmental Research and Public Health, 22(8), 1197. https://doi.org/10.3390/ijerph22081197







