A Rapid Review of Ethical and Equity Dimensions in Telerehabilitation for Physiotherapy and Occupational Therapy
Abstract
1. Introduction
2. Methodology
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Screening and Data Extraction
2.4. Quality Assessment (Risk of Bias)
2.5. Data Synthesis
Analysis of Subgroups or Subsets
2.6. Changes on the Protocol
3. Results
3.1. Search Results and Characteristics of Included Studies
3.2. Study Design
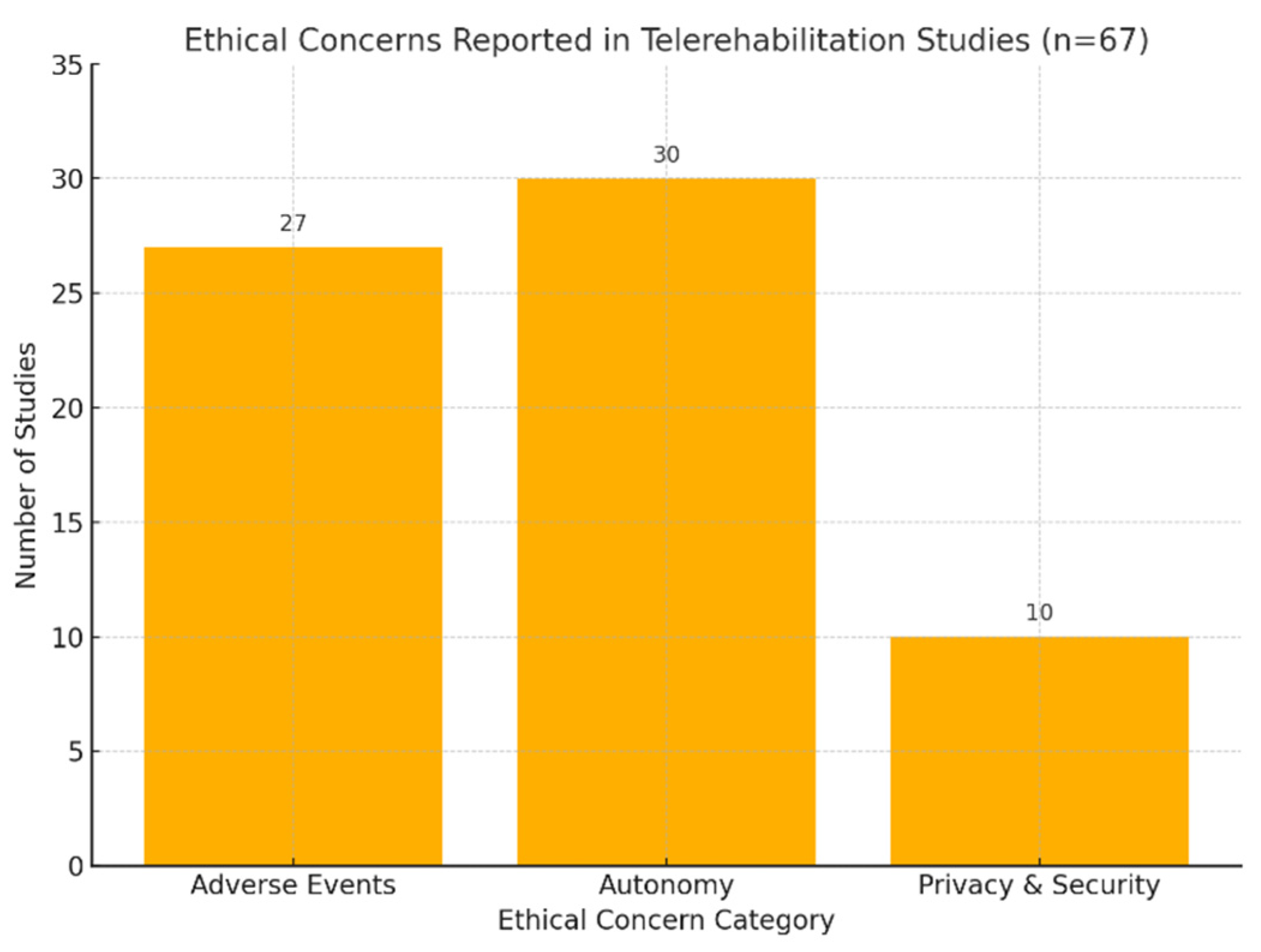
3.3. Ethics Considerations
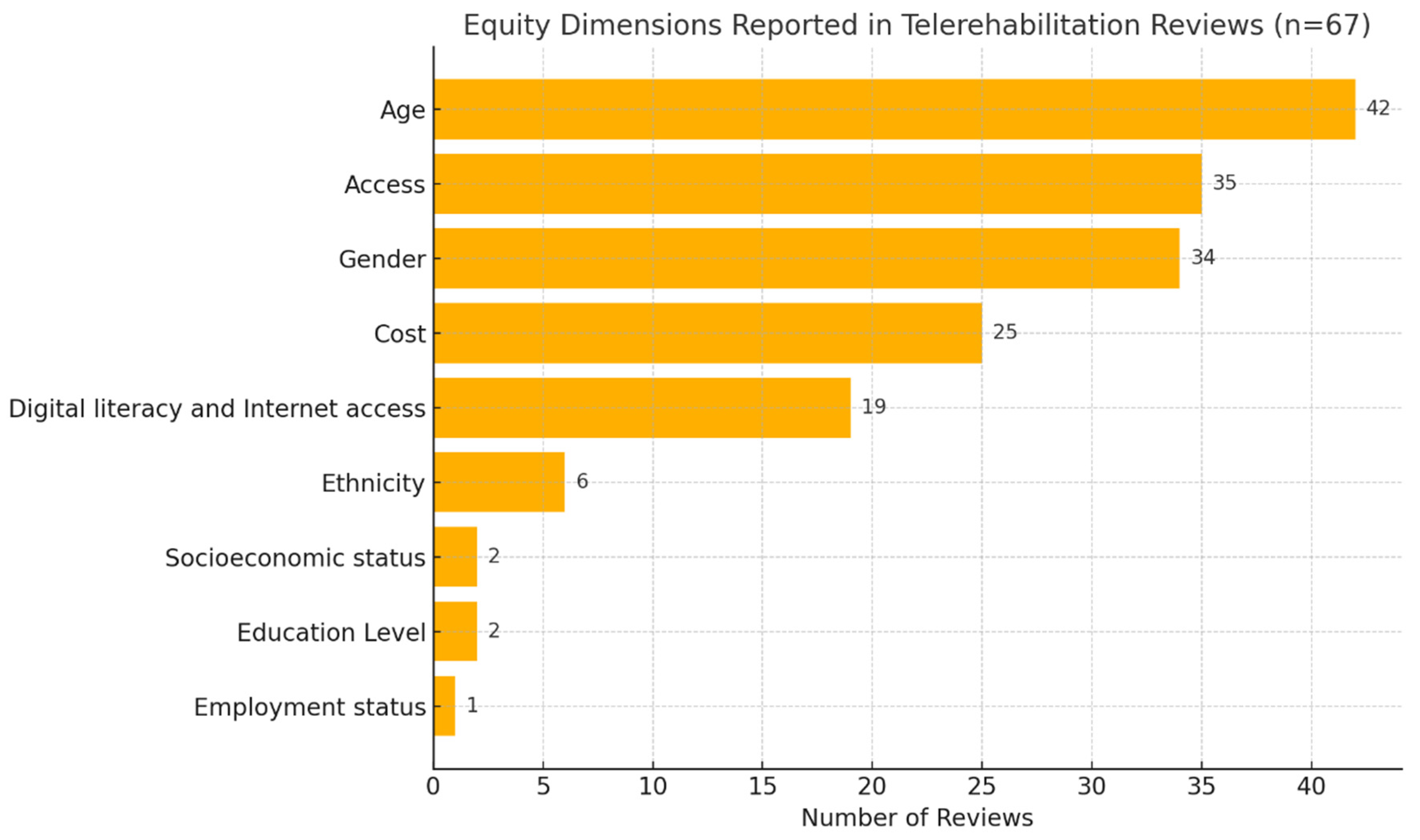
3.4. Equity Considerations
3.5. Quality Assessment (Risk of Bias)
4. Discussion
4.1. Ethics Aspects
4.2. Equity Aspects
4.3. Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Xu, J.; Willging, A.; Bramstedt, K.A. A scoping review of the ethical issues within telemedicine: Lessons from COVID-19 pandemic. J. Health Soc. Sci. Ital. J. Interdiscip. Health Soc. Dev. 2021, 6, 31–40. [Google Scholar]
- Shem, K.; Irgens, I.; Alexander, M. Chapter 2. Getting Started: Mechanisms of Telerehabilitation. In Telerehabilitation; Alexander, M., Ed.; Elsevier: Amsterdam, The Netherlands, 2022; pp. 5–20. [Google Scholar]
- Seron, P.; Oliveros, M.J.; Gutierrez-Arias, R.; Fuentes-Aspe, R.; Torres-Castro, R.C.; Merino-Osorio, C.; Nahuelhual, P.; Inostroza, J.; Jalil, Y.; Solano, R.; et al. Effectiveness of Telerehabilitation in Physical Therapy: A Rapid Overview. Phys. Ther. 2021, 101, pzab053. [Google Scholar] [CrossRef] [PubMed]
- Veras, M.; Sigouin, J.; Auger, C.; Auger, L.-P.; Ahmed, S.; Boychuck, Z.; Cavallo, S.; Lévesque, M.; Lovo, S.; Miller, W.C.; et al. A rapid review protocol of physiotherapy and occupational therapy telerehabilitation to inform ethical and equity concerns. Digit. Health 2024, 10, 20552076241260367. [Google Scholar] [CrossRef] [PubMed]
- Varkey, B. Principles of Clinical Ethics and Their Application to Practice. Med. Princ. Pract. 2021, 30, 17–28. [Google Scholar] [CrossRef]
- Baroni, M.P.; Jacob, M.F.A.; Rios, W.R.; Fandim, J.V.; Fernandes, L.G.; Chaves, P.I.; Fioratti, I.; Saragiotto, B.T. The state of the art in telerehabilitation for musculoskeletal conditions. Arch. Physiother. 2023, 13, 1. [Google Scholar] [CrossRef]
- Kairy, D.; Lehoux, P.; Vincent, C.; Visintin, M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil. Rehabil. 2009, 31, 427–447. [Google Scholar] [CrossRef]
- Nittari, G.; Khuman, R.; Baldoni, S.; Pallotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. J. E Health 2020, 26, 1427–1437. [Google Scholar] [CrossRef]
- Mahmoudi, E.; Meade, M.A. Disparities in access to health care among adults with physical disabilities: Analysis of a representative national sample for a ten-year period. Disabil. Health J. 2015, 8, 182–190. [Google Scholar] [CrossRef]
- Choukou, M.-A.; Maddahi, A.; Polyvyana, A.; Monnin, C. Digital health technology for Indigenous older adults: A scoping review. Int. J. Med. Inform. 2021, 148, 104408. [Google Scholar] [CrossRef]
- Zhang, D.; Wang, G.; Zhu, W.; Thapa, J.R.; Switzer, J.A.; Hess, D.C.; Smith, M.L.; Ritchey, M.D. Expansion Of Telestroke Services Improves Quality Of Care Provided In Super Rural Areas. Health Aff. 2018, 37, 2005–2013. [Google Scholar] [CrossRef]
- King, V.J.; Stevens, A.; Nussbaumer-Streit, B.; Kamel, C.; Garritty, C. Paper 2: Performing rapid reviews. Syst. Rev. 2022, 11, 151. [Google Scholar] [PubMed]
- Garritty, C.; Gartlehner, G.; Nussbaumer-Streit, B.; King, V.J.; Hamel, C.; Kamel, C.; Affengruber, L.; Stevens, A. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J. Clin. Epidemiol. 2021, 130, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Matchar, D.B. Chapter 1: Introduction to the Methods Guide for Medical Test Reviews. J. Gen. Intern. Med. 2012, 27, 4–10. [Google Scholar] [CrossRef]
- Veras, M.; Kairy, D.; Rogante, M.; Giacomozzi, C. Outcome Measures in Tele-Rehabilitation and Virtual Reality for Stroke Survivors: Protocol for a Scoping Review. Glob. J. Health Sci. 2015, 8, 79–82. [Google Scholar]
- Covidence Systematic Reviews Software. Veritas Health Innovations: Melbourne, Australia. Available online: www.covidence.org (accessed on 3 January 2022).
- Veras, M.; Labbé, D.R.; Furlano, J.; Zakus, D.; Rutherford, D.; Pendergast, B.; Kairy, D. A framework for equitable virtual rehabilitation in the metaverse era: Challenges and opportunities. Front. Rehabil. Sci. 2023, 4, 1241020. [Google Scholar] [CrossRef]
- O’Neill, J.; Tabish, H.; Welch, V.; Petticrew, M.; Pottie, K.; Clarke, M.; Evans, T.; Pardo Pardo, J.; Waters, E.; White, H.; et al. Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J. Clin. Epidemiol. 2014, 67, 56–64. [Google Scholar] [CrossRef]
- Mays, N.; Pope, C.; Popay, J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J. Health Serv. Res. Policy 2005, 10 (Suppl. S1), 6–20. [Google Scholar] [CrossRef]
- Chan, C.; Yamabayashi, C.; Syed, N.; Kirkham, A.; Camp, P.G. Exercise Telemonitoring and Telerehabilitation Compared with Traditional Cardiac and Pulmonary Rehabilitation: A Systematic Review and Meta-Analysis. Physiother. Can. 2016, 68, 242–251. [Google Scholar]
- Chirra, M.; Marsili, L.; Wattley, L.; Sokol, L.L.; Keeling, E.; Maule, S.; Sobrero, G.; Artusi, C.A.; Romagnolo, A.; Zibetti, M.; et al. Telemedicine in Neurological Disorders: Opportunities and Challenges. Telemed. J. E Health 2019, 25, 541–550. [Google Scholar] [CrossRef]
- Ninnis, K.; Van Den Berg, M.; Lannin, N.A.; George, S.; Laver, K. Information and communication technology use within occupational therapy home assessments: A scoping review. Br. J. Occup. Ther. 2018, 82, 141–152. [Google Scholar] [CrossRef]
- Agostini, M.; Moja, L.; Banzi, R.; Pistotti, V.; Tonin, P.; Venneri, A.; Turolla, A. Telerehabilitation and recovery of motor function: A systematic review and meta-analysis. J. Telemed. Telecare 2015, 21, 202–213. [Google Scholar] [CrossRef] [PubMed]
- Amatya, B.; Galea, M.P.; Kesselring, J.; Khan, F. Effectiveness of telerehabilitation interventions in persons with multiple sclerosis: A systematic review. Mult. Scler. Relat. Disord. 2015, 4, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Amatya, B.; Khan, F.; Galea, M. Rehabilitation for people with multiple sclerosis: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2019, 1, Cd012732. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Jin, W.; Zhang, X.-X.; Xu, W.; Liu, X.-N.; Ren, C.-C. Telerehabilitation Approaches for Stroke Patients: Systematic Review and Meta-analysis of Randomized Controlled Trials. J. Stroke Cerebrovasc. Dis. 2015, 24, 2660–2668. [Google Scholar] [CrossRef]
- Chen, Y.; Abel, K.T.; Janecek, J.T.; Zheng, K.; Cramer, S.C. Home-based technologies for stroke rehabilitation: A systematic review. Int. J. Med. Inform. 2019, 123, 11–22. [Google Scholar] [CrossRef]
- Dávila Castrodad, I.M.; Recai, T.M.; Abraham, M.M.; Etcheson, J.I.; Mohamed, N.S.; Edalatpour, A.; Delanois, R.E. Rehabilitation protocols following total knee arthroplasty: A review of study designs and outcome measures. Ann. Transl. Med. 2019, 7 (Suppl. S7), S255. [Google Scholar]
- Khan, F.; Amatya, B.; Kesselring, J.; Galea, M. Telerehabilitation for persons with multiple sclerosis. Cochrane Database Syst. Rev. 2015, 2015, CD010508. [Google Scholar]
- Laver, K.E.; Adey-Wakeling, Z.; Crotty, M.; Lannin, N.A.; George, S.; Sherrington, C. Telerehabilitation services for stroke. Cochrane Database Syst. Rev. 2020, 1, Cd010255. [Google Scholar] [CrossRef]
- Almojaibel, A.A. Delivering Pulmonary Rehabilitation for Patients with Chronic Obstructive Pulmonary Disease at Home Using Telehealth: A Review of the Literature. Saudi J. Med. Med. Sci. 2016, 4, 164–171. [Google Scholar] [CrossRef]
- Appleby, E.; Gill, S.T.; Hayes, L.K.; Walker, T.L.; Walsh, M.; Kumar, S. Effectiveness of telerehabilitation in the management of adults with stroke: A systematic review. PLoS ONE 2019, 14, e0225150. [Google Scholar] [CrossRef]
- Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A.; et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. J. Clin. Med. 2020, 9, 2567. [Google Scholar] [CrossRef]
- Blood, K. The use of Telehealth by Physical Therapis: A review of literature. Gerinotes Acad. Geriatr. Phys. Ther. 2019, 26, 22–29. [Google Scholar]
- Flodgren, G.; Rachas, A.; Farmer, A.J.; Inzitari, M.; Shepperd, S. Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015, 2015, CD002098. [Google Scholar] [PubMed]
- Jin, K.; Khonsari, S.; Gallagher, R.; Gallagher, P.; Clark, A.M.; Freedman, B.; Briffa, T.; Bauman, A.; Redfern, J.; Neubeck, L. Telehealth interventions for the secondary prevention of coronary heart disease: A systematic review and meta-analysis. Eur. J. Cardiovasc. Nurs. 2019, 18, 260–271. [Google Scholar] [CrossRef]
- Slattery, B.W.; Haugh, S.; O’Connor, L.; Francis, K.; Dwyer, C.P.; O’Higgins, S.; Egan, J.; McGuire, B.E. An Evaluation of the Effectiveness of the Modalities Used to Deliver Electronic Health Interventions for Chronic Pain: Systematic Review with Network Meta-Analysis. J. Med. Internet Res. 2019, 21, e11086. [Google Scholar] [CrossRef]
- van der Meij, E.; Anema, J.R.; Otten, R.H.; Huirne, J.A.; Schaafsma, F.G. The Effect of Perioperative E-Health Interventions on the Postoperative Course: A Systematic Review of Randomised and Non-Randomised Controlled Trials. PLoS ONE 2016, 11, e0158612. [Google Scholar] [CrossRef]
- van Egmond, M.A.; van der Schaaf, M.; Vredeveld, T.; Vollenbroek-Hutten, M.M.R.; van Berge Henegouwen, M.I.; Klinkenbijl, J.H.G.; Engelbert, R.H.H. Effectiveness of physiotherapy with telerehabilitation in surgical patients: A systematic review and meta-analysis. Physiotherapy 2018, 104, 277–298. [Google Scholar] [CrossRef]
- Veras, M.; Kairy, D.; Rogante, M.; Giacomozzi, C.; Saraiva, S. Scoping review of outcome measures used in telerehabilitation and virtual reality for post-stroke rehabilitation. J. Telemed. Telecare 2016, 23, 567–587. [Google Scholar] [CrossRef]
- Hao, J.; Pu, Y.; Chen, Z.; Siu, K.C. Effects of virtual reality-based telerehabilitation for stroke patients: A systematic review and meta-analysis of randomized controlled trials. J. Stroke Cerebrovasc. Dis. 2023, 32, 106960. [Google Scholar] [CrossRef]
- Thwaites, C.; Nayyar, R.; Blennerhassett, J.; Egerton, T.; Tan, J.; Bower, K. Is telehealth an effective and feasible option for improving falls-related outcomes in community-dwelling adults with neurological conditions? A systematic review and meta-analysis. Clin. Rehabil. 2022, 37, 17–46. [Google Scholar] [CrossRef]
- Ben, B.; Latour, J.A.-O.; Tomlinson, O.A.-O. A systematic review to explore how exercise-based physiotherapy via telemedicine can promote health related benefits for people with cystic fibrosis. PLoS Digit. Health 2023, 2, e0000201. [Google Scholar] [CrossRef]
- Hao, J.; Biying, H.; Andréas, R.; He, Z. The application of virtual reality to home-based rehabilitation for children and adolescents with cerebral palsy: A systematic review and meta-analysis. Physiother. Theory Pract. 2024, 40, 1588–1608. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Yang, Y.; Wu, X.; Xiao, B.; Ma, L.; Xu, Y. The telehealth program of occupational therapy among older people: An up-to-date scoping review. Aging Clin. Exp. Res. 2023, 35, 23–40. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Parmanto, B. Reaching People with Disabilities in Underserved Areas Through Digital Interventions: Systematic Review. J. Med. Internet Res. 2019, 21, e12981. [Google Scholar] [CrossRef]
- Batsis, J.A.; DiMilia, P.R.; Seo, L.M.; Fortuna, K.L.; Kennedy, M.A.; Blunt, H.B.; Bagley, P.J.; Brooks, J.; Brooks, E.; Kim, S.Y.; et al. Effectiveness of Ambulatory Telemedicine Care in Older Adults: A Systematic Review. J. Am. Geriatr. Soc. 2019, 67, 1737–1749. [Google Scholar] [CrossRef]
- Cottrell, M.A.; Galea, O.A.; O’Leary, S.P.; Hill, A.J.; Russell, T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 625–638. [Google Scholar]
- Du, S.; Liu, W.; Cai, S.; Hu, Y.; Dong, J. The efficacy of e-health in the self-management of chronic low back pain: A meta analysis. Int. J. Nurs. Stud. 2020, 106, 103507. [Google Scholar] [CrossRef]
- Mani, S.; Sharma, S.; Omar, B.; Paungmali, A.; Joseph, L. Validity and reliability of Internet-based physiotherapy assessment for musculoskeletal disorders: A systematic review. J. Telemed. Telecare 2016, 23, 379–391. [Google Scholar] [CrossRef]
- Gilbert, A.W.; Jaggi, A.; May, C.R. What is the patient acceptability of real time 1:1 videoconferencing in an orthopaedics setting? A systematic review. Physiotherapy 2018, 104, 178–186. [Google Scholar]
- Tchero, H.; Tabue Teguo, M.; Lannuzel, A.; Rusch, E. Telerehabilitation for Stroke Survivors: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2018, 20, e10867. [Google Scholar]
- Salomè, A.; Sasso D’Elia, T.; Franchini, G.; Santilli, V.; Paolucci, T. Occupational Therapy in Fatigue Management in Multiple Sclerosis: An Umbrella Review. Mult. Scler. Int. 2019, 2019, 2027947. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Tomás, M.T.; Burillo-Lafuente, M.; Vicente-Parra, A.; Sanz-Rubio, M.C.; Suarez-Serrano, C.; Marcén-Román, Y.; Franco-Sierra, M. Telerehabilitation as a Therapeutic Exercise Tool versus Face-to-Face Physiotherapy: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 4358. [Google Scholar]
- Suder, R.; DeBoth, K.K.; Carrick, A.; Davis, J.; Farrar, B. A Systematic Review of Occupational Therapy-Related Interventions for Pediatric Chronic Pain. OTJR Occup. Ther. J. Res. 2023, 43, 61–73. [Google Scholar] [CrossRef]
- Iacono, T.; Stagg, K.; Pearce, N.; Hulme Chambers, A. A scoping review of Australian allied health research in ehealth. BMC Health Serv. Res. 2016, 16, 543. [Google Scholar] [CrossRef]
- Pietrzak, E.; Cotea, C.; Pullman, S.; Nasveld, P. Self-management and rehabilitation in osteoarthritis: Is there a place for internet-based interventions? Telemed. J. E Health 2013, 19, 800–805. [Google Scholar] [CrossRef]
- Rintala, A.; Hakala, S.; Paltamaa, J.; Heinonen, A.; Karvanen, J.; Sjögren, T. Effectiveness of technology-based distance physical rehabilitation interventions on physical activity and walking in multiple sclerosis: A systematic review and meta-analysis of randomized controlled trials. Disabil. Rehabil. 2018, 40, 373–387. [Google Scholar] [CrossRef]
- Yadav, L.; Haldar, A.; Jasper, U.; Taylor, A.; Visvanathan, R.; Chehade, M.; Gill, T. Utilising Digital Health Technology to Support Patient-Healthcare Provider Communication in Fragility Fracture Recovery: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4047. [Google Scholar] [CrossRef]
- Chen, Y.-Y.; Guan, B.-S.; Li, Z.-K.; Yang, Q.-H.; Xu, T.-J.; Li, H.-B.; Wu, Q.-Y. Application of telehealth intervention in Parkinson’s disease: A systematic review and meta-analysis. J. Telemed. Telecare 2018, 26, 3–13. [Google Scholar] [CrossRef]
- Gövercin, M.; Missala, I.M.; Marschollek, M.; Steinhagen-Thiessen, E. Virtual rehabilitation and telerehabilitation for the upper limb: A geriatric review. GeroPsych J. Gerontopsychol. Geriatr. Psychiatry 2010, 23, 79–90. [Google Scholar] [CrossRef]
- Grona, S.L.; Bath, B.; Busch, A.; Rotter, T.; Trask, C.; Harrison, E. Use of videoconferencing for physical therapy in people with musculoskeletal conditions: A systematic review. J. Telemed. Telecare 2017, 24, 341–355. [Google Scholar] [CrossRef]
- Hewitt, S.; Sephton, R.; Yeowell, G. The Effectiveness of Digital Health Interventions in the Management of Musculoskeletal Conditions: Systematic Literature Review. J. Med. Internet Res. 2020, 22, e15617. [Google Scholar] [CrossRef] [PubMed]
- Pastora-Bernal, J.M.; Martín-Valero, R.; Barón-López, F.J.; Estebanez-Pérez, M.J. Evidence of Benefit of Telerehabitation After Orthopedic Surgery: A Systematic Review. J. Med. Internet Res. 2017, 19, e142. [Google Scholar] [CrossRef] [PubMed]
- Schröder, J.; van Criekinge, T.; Embrechts, E.; Celis, X.; Van Schuppen, J.; Truijen, S.; Saeys, W. Combining the benefits of tele-rehabilitation and virtual reality-based balance training: A systematic review on feasibility and effectiveness. Disabil. Rehabil. Assist. Technol. 2019, 14, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Shukla, H.; Nair, S.R.; Thakker, D. Role of telerehabilitation in patients following total knee arthroplasty: Evidence from a systematic literature review and meta-analysis. J. Telemed. Telecare 2016, 23, 339–346. [Google Scholar] [CrossRef]
- Simek, E.M.; McPhate, L.; Haines, T.P. Adherence to and efficacy of home exercise programs to prevent falls: A systematic review and meta-analysis of the impact of exercise program characteristics. Prev. Med. 2012, 55, 262–275. [Google Scholar] [CrossRef]
- Speyer, R.; Denman, D.; Wilkes-Gillan, S.; Chen, Y.W.; Bogaardt, H.; Kim, J.H.; Heckathorn, D.E.; Cordier, R. Effects of telehealth by allied health professionals and nurses in rural and remote areas: A systematic review and meta-analysis. J. Rehabil. Med. 2018, 50, 225–235. [Google Scholar] [CrossRef]
- Srikesavan, C.; Bryer, C.; Ali, U.; Williamson, E. Web-based rehabilitation interventions for people with rheumatoid arthritis: A systematic review. J. Telemed. Telecare 2018, 25, 263–275. [Google Scholar] [CrossRef]
- Velayati, F.; Ayatollahi, H.; Hemmat, M. A Systematic Review of the Effectiveness of Telerehabilitation Interventions for Therapeutic Purposes in the Elderly. Methods Inf. Med. 2020, 59, 104–109. [Google Scholar] [CrossRef]
- Wake, E.; Atkins, H.; Willock, A.; Hawkes, A.; Dawber, J.; Weir, K.A. Telehealth in trauma: A scoping review. J. Telemed. Telecare 2020, 28, 412–422. [Google Scholar] [CrossRef]
- Wang, X.; Hunter, D.J.; Vesentini, G.; Pozzobon, D.; Ferreira, M.L. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 506. [Google Scholar] [CrossRef]
- Hung Kn, G.; Fong, K.N. Effects of telerehabilitation in occupational therapy practice: A systematic review. Hong Kong J. Occup. Ther. 2019, 32, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, A.; Nayak, P.; Deshmukh, A.; English, C.; Manikandan, N.; Solomon, M.J.; Unnikrishnan, B. Measurement, determinants, barriers, and interventions for exercise adherence: A scoping review. J. Bodyw. Mov. Ther. 2023, 33, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Giustiniani, A.; Danesin, L.; Pezzetta, R.; Masina, F.; Oliva, G.; Arcara, G.; Burgio, F.; Conte, P. Use of Telemedicine to Improve Cognitive Functions and Psychological Well-Being in Patients with Breast Cancer: A Systematic Review of the Current Literature. Cancers 2023, 15, 1353. [Google Scholar] [CrossRef] [PubMed]
- Yeroushalmi, S.; Maloni, H.; Costello, K.; Wallin, M.T. Telemedicine and multiple sclerosis: A comprehensive literature review. J. Telemed. Telecare 2019, 26, 400–413. [Google Scholar] [CrossRef]
- Davis, A.M. Osteoarthritis year 2011 in review: Rehabilitation and outcomes. Osteoarthr. Cartil. 2012, 20, 201–206. [Google Scholar] [CrossRef]
- Johansson, T.; Wild, C. Telerehabilitation in stroke care—A systematic review. J. Telemed. Telecare 2011, 17, 1–6. [Google Scholar]
- Knepley, K.D.; Mao, J.Z.; Wieczorek, P.; Okoye, F.O.; Jain, A.P.; Harel, N.Y. Impact of Telerehabilitation for Stroke-Related Deficits. Telemed. e-Health 2020, 27, 239–246. [Google Scholar] [CrossRef]
- Guay, C.; Auger, C.; Demers, L.; Mortenson, W.B.; Miller, W.C.; Gélinas-Bronsard, D.; Ahmed, S. Components and Outcomes of Internet-Based Interventions for Caregivers of Older Adults: Systematic Review. J. Med. Internet Res. 2017, 19, e313. [Google Scholar] [CrossRef]
- Hayes, K.; Dos Santos, V.; Costigan, M.; Morante, D. Profile of occupational therapy services in non-urban settings: A global scoping review. Aust. Occup. Ther. J. 2023, 70, 119–141. [Google Scholar]
- Sarfo, F.S.; Ulasavets, U.; Opare-Sem, O.K.; Ovbiagele, B. Tele-Rehabilitation after Stroke: An Updated Systematic Review of the Literature. J. Stroke Cerebrovasc. Dis. 2018, 27, 2306–2318. [Google Scholar]
- Kebapci, A.; Ozkaynak, M.; Lareau, S.C. Effects of eHealth-Based Interventions on Adherence to Components of Cardiac Rehabilitation: A Systematic Review. J. Cardiovasc. Nurs. 2020, 35, 74–85. [Google Scholar] [PubMed]
- Tricco, A.C.; Antony, J.; Zarin, W.; Strifler, L.; Ghassemi, M.; Ivory, J.; Perrier, L.; Hutton, B.; Moher, D.; Straus, S.E. A scoping review of rapid review methods. BMC Med. 2015, 13, 224. [Google Scholar] [CrossRef]
- Pang, D.; Sun, A.; Wang, F.; Lu, J.; Guo, Y.; Ding, W. The efficacy and safety of telerehabilitation for patients following total knee arthroplasty: A overviews of systematic reviews. Biomed. Eng. Online 2023, 22, 97. [Google Scholar] [CrossRef]
- Greaney, A.M.; Flaherty, S. Self-care as care left undone? The ethics of the self-care agenda in contemporary healthcare policy. Nurs. Philos. 2020, 21, e12291. [Google Scholar] [CrossRef]
- Guy, M.; Blary, A.; Ladner, J.; Gilliaux, M. Ethical Issues Linked to the Development of Telerehabilitation: A Qualitative Study. Int. J. Telerehabil 2021, 13, e6367. [Google Scholar] [CrossRef]
- ÖZden, F.; Lembarkİ, Y. The Ethical Necessities and Principles in Telerehabilitation. Sağlık Hizmetleri Ve Eğitimi Derg. 2020, 3, 35–37. [Google Scholar] [CrossRef]
- Lee, A.C.; Deutsch, J.E.; Holdsworth, L.; Kaplan, S.L.; Kosakowski, H.; Latz, R.; McNeary, L.L.; O’Neil, J.; Ronzio, O.; Sanders, K.; et al. Telerehabilitation in Physical Therapist Practice: A Clinical Practice Guideline from the American Physical Therapy Association. Phys. Ther. 2024, 104, pzae045. [Google Scholar] [CrossRef]
- Rochette, A.; Korner-Bitensky, N.; Bishop, D.; Teasell, R.; White, C.L.; Bravo, G.; Côté, R.; Green, T.; Lebrun, L.H.; Lanthier, S.; et al. The YOU CALL-WE CALL randomized clinical trial: Impact of a multimodal support intervention after a mild stroke. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 674–679. [Google Scholar] [CrossRef]
- Ouédraogo, F.; Auger, L.P.; Moreau, E.; Côté, O.; Guerrera, R.; Rochette, A.; Kairy, D. Acceptability of Telerehabilitation: Experiences and Perceptions by Individuals with Stroke and Caregivers in an Early Supported Discharge Program. Healthcare 2024, 12, 365. [Google Scholar] [CrossRef]
- Embree, J.A.; Huber, J.-M.; Kapp, V.A.; Wilson, J.F. Utilizing Telerehabilitation to Deliver Vocational Rehabilitation Services Remotely as an Alternative to Traditional Counseling. J. Appl. Rehabil. Couns. 2018, 49, 40–47. [Google Scholar] [CrossRef]
- Nicolas, B.; Leblong, E.; Fraudet, B.; Gallien, P.; Piette, P. Telerehabilitation solutions in patient pathways: An overview of systematic reviews. Digit. Health 2024, 10, 20552076241294110. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.; Amit, S.; Kafy, A.A. Gender disparity in telehealth usage in Bangladesh during COVID-19. SSM Ment. Health 2022, 2, 100054. [Google Scholar] [CrossRef] [PubMed]
- Ott, J.; Champagne, S.N.; Bachani, A.M.; Morgan, R. Scoping ‘sex’ and ‘gender’ in rehabilitation: (Mis)representations and effects. Int. J. Equity Health 2022, 21, 179. [Google Scholar] [CrossRef] [PubMed]
- Veras, M.; Stewart, J.; Deonandan, R.; Tatmatsu-Rocha, J.C.; Higgins, J.; Poissant, L.; Kairy, D. Cost-Analysis of a Home-Based Virtual Reality Rehabilitation to improve Upper Limb Function in Stroke Survivors. Glob. J. Health Sci. Can. Cener Sci. Educ. 2020, 12, 1–98. [Google Scholar]
- Duruflé, A.; Le Meur, C.; Piette, P.; Fraudet, B.; Leblong, E.; Gallien, P. Cost effectiveness of a telerehabilitation intervention vs. home based care for adults with severe neurologic disability: A randomized clinical trial. Digit. Health 2023, 9, 20552076231191001. [Google Scholar] [CrossRef]
- Sanders, C.K.; Scanlon, E. The Digital Divide Is a Human Rights Issue: Advancing Social Inclusion Through Social Work Advocacy. J. Hum. Rights Soc. Work. 2021, 6, 130–143. [Google Scholar] [CrossRef]
- Saeed, S.A.; Masters, R.M. Disparities in Health Care and the Digital Divide. Curr. Psychiatry Rep. 2021, 23, 61. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veras, M.; Sigouin, J.; Auger, L.-P.; Auger, C.; Ahmed, S.; Boychuck, Z.; Cavallo, S.; Lévesque, M.; Lovo, S.; Miller, W.C.; et al. A Rapid Review of Ethical and Equity Dimensions in Telerehabilitation for Physiotherapy and Occupational Therapy. Int. J. Environ. Res. Public Health 2025, 22, 1091. https://doi.org/10.3390/ijerph22071091
Veras M, Sigouin J, Auger L-P, Auger C, Ahmed S, Boychuck Z, Cavallo S, Lévesque M, Lovo S, Miller WC, et al. A Rapid Review of Ethical and Equity Dimensions in Telerehabilitation for Physiotherapy and Occupational Therapy. International Journal of Environmental Research and Public Health. 2025; 22(7):1091. https://doi.org/10.3390/ijerph22071091
Chicago/Turabian StyleVeras, Mirella, Jennifer Sigouin, Louis-Pierre Auger, Claudine Auger, Sara Ahmed, Zachary Boychuck, Sabrina Cavallo, Martine Lévesque, Stacey Lovo, William C. Miller, and et al. 2025. "A Rapid Review of Ethical and Equity Dimensions in Telerehabilitation for Physiotherapy and Occupational Therapy" International Journal of Environmental Research and Public Health 22, no. 7: 1091. https://doi.org/10.3390/ijerph22071091
APA StyleVeras, M., Sigouin, J., Auger, L.-P., Auger, C., Ahmed, S., Boychuck, Z., Cavallo, S., Lévesque, M., Lovo, S., Miller, W. C., Nelson, M., Norouzi-Gheidari, N., O’Neil, J., Perreault, K., Urbanowski, R., Sheehy, L., Singh, H., Vincent, C., Wang, R. H., ... Kairy, D. (2025). A Rapid Review of Ethical and Equity Dimensions in Telerehabilitation for Physiotherapy and Occupational Therapy. International Journal of Environmental Research and Public Health, 22(7), 1091. https://doi.org/10.3390/ijerph22071091








