Reconstructing Cross-Cultural Meanings of Addiction Among Women from Three Countries
Abstract
1. Introduction
2. Study Populations
3. Materials and Methods
4. Analysis
“Stress; Capability of not coping with what’s going on around you.”
5. Results
5.1. What Causes Addiction?
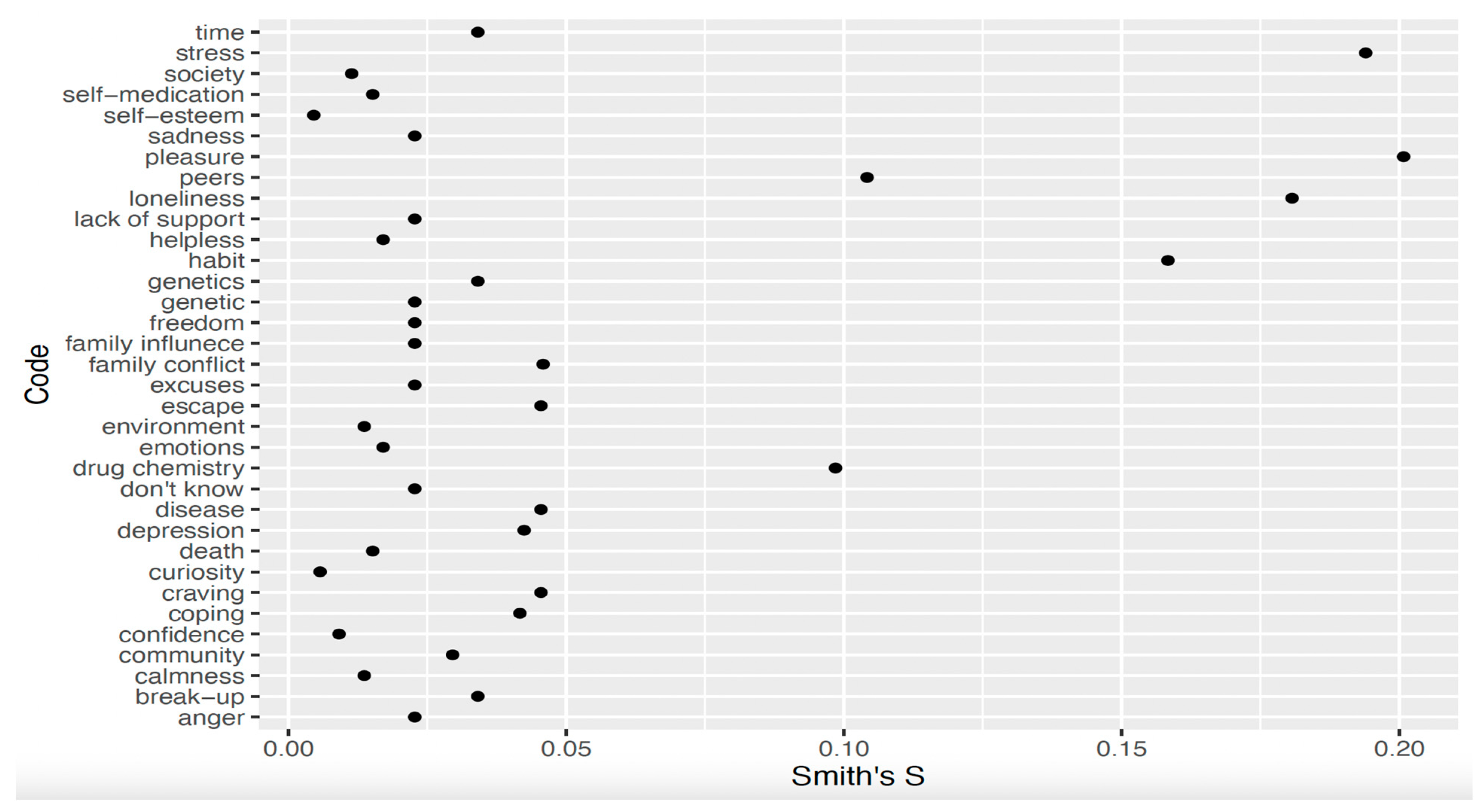
5.1.1. Delhi
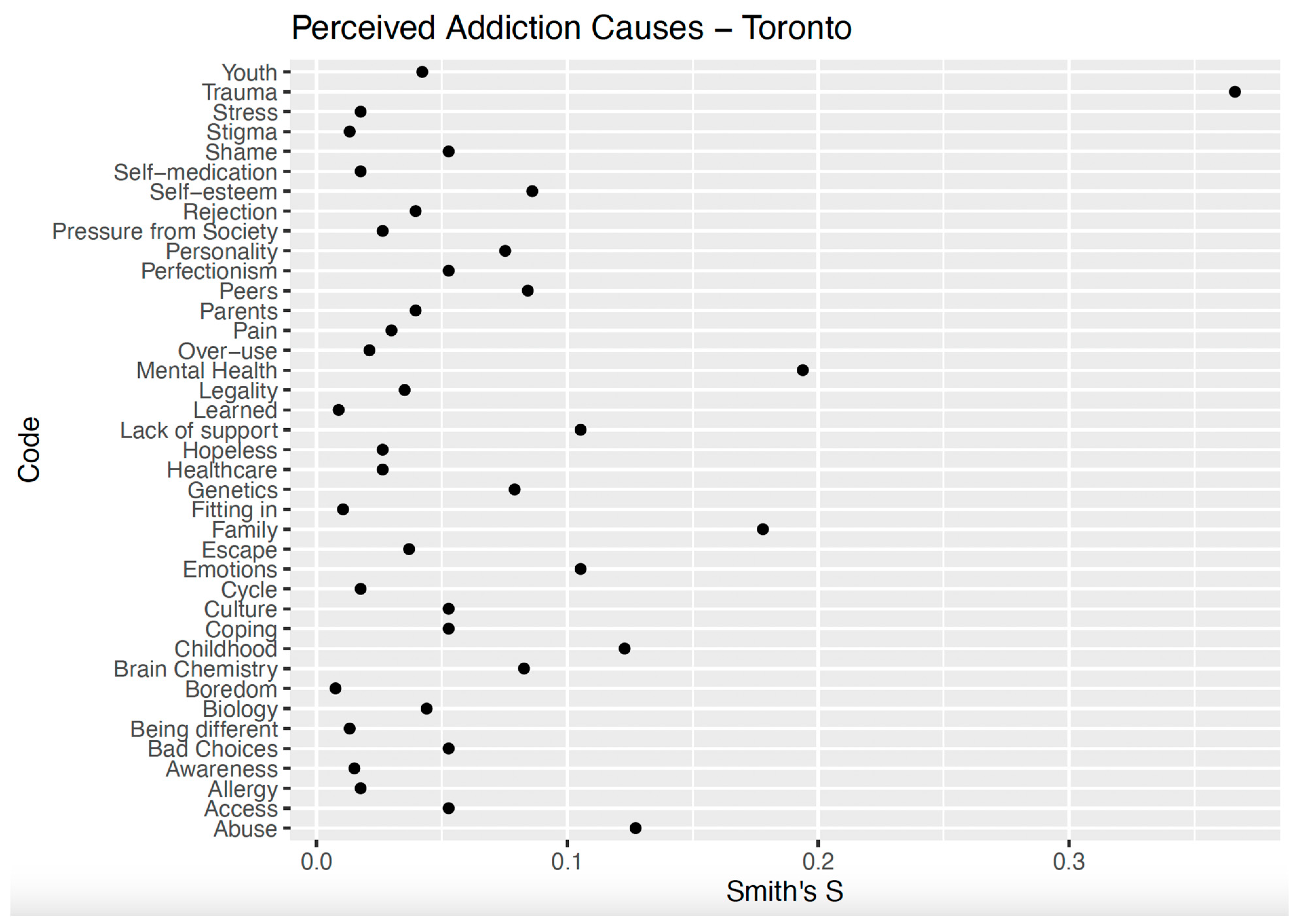
5.1.2. Toronto
“So, I think it’s just the unreal expectations that society has toward women, especially mothers, and like to be the perfect mother to look perfect to have a job, plus do all the things for your children, like extracurricular activities, to juggle that perfect life. And then, you know, when you have mental health issues like that, that are also, you know, it also, I just, I think mental health causes you to have, especially like postpartum depression or something like that.”
“Oh, that’s a real open-ended question. It could be anything from childhood trauma, abuse, mental illness. It could be physical pain from accidents. It could be homelessness or home insecurity. It could be just neglect in general. All of those. There may be even more. It could be systematic racial problems that they’ve faced or economic problems. A lot of it is all integrated. I don’t think there’s one or the—I don’t find one is without another. I think that they’re all somehow intertwined.”
“Oh, what do we think causes it? You know, I’m not really of the opinion that you have to have some sort of like, trauma, to end up a drug user. You know, I think even just something so simple as bad choices can put you in a situation where you’re doing a drug that you have to do every day, even though that’s not something that you ever thought you would end up doing, you know, what I think causes it, you know, being a kid being dumb, you know, going out, being with different people, you know, everything could put you in a situation where you’re, you know, maybe going to do drugs where you normally wouldn’t? What makes you end up a habitual drug user? I think choosing the wrong drug too many times.”
“Well, yes, I mean, it starts as you know, like, you just don’t even think that because you grow up having it around, or people do or for me, personally, but it’s always around, and you don’t realize that you use it when you’re, you know, I’m also a smoker. So I was reading, you know, a cigarette, you can use when you’re happy when you’re sad when you’re mad like it. It’s the cure for everything.”
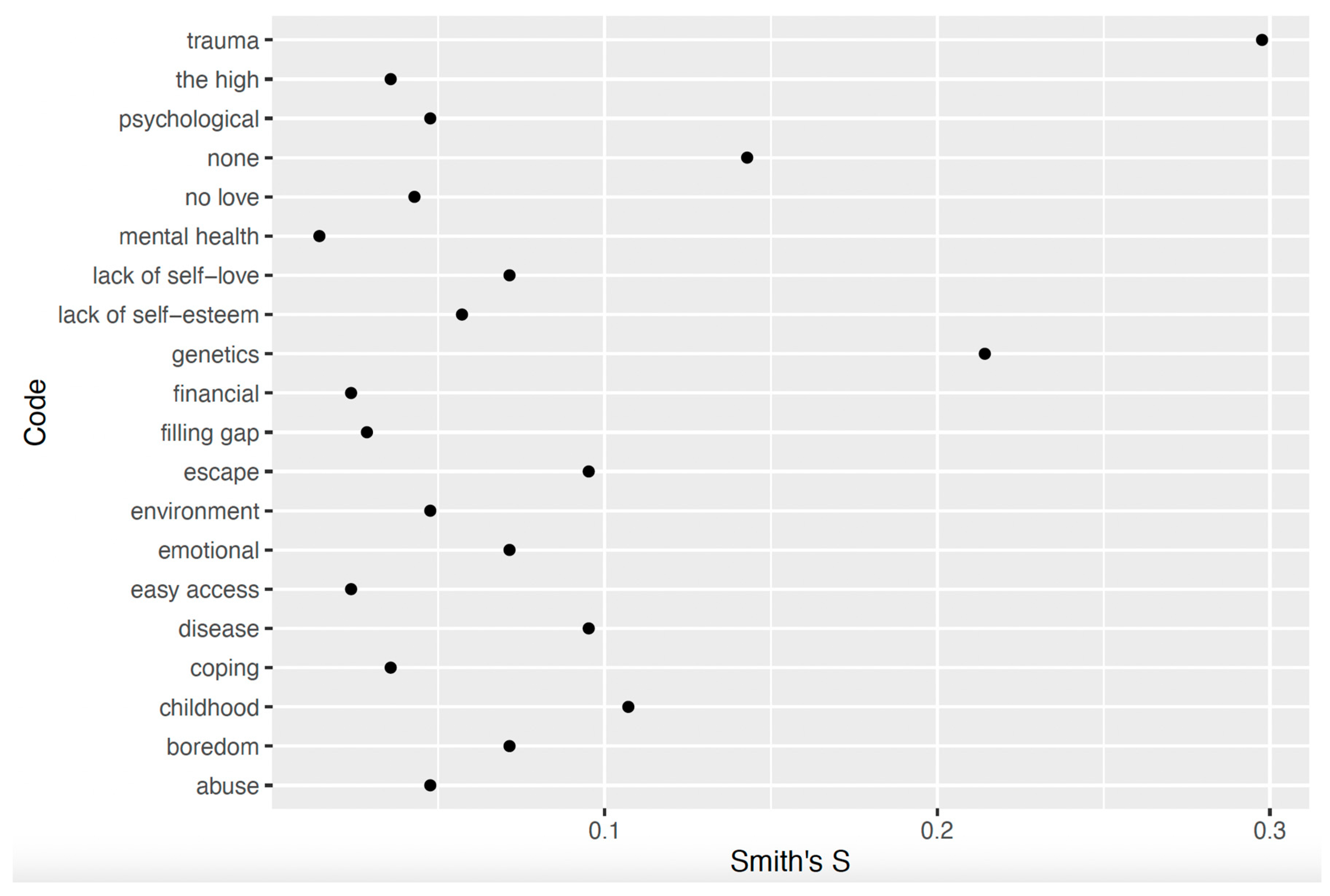
5.1.3. London
“In my opinion, trauma, behaviors copied, learned from what you witness as a child, especially around the age of seven to eight when you’re more likely to remember your life. I know for me it is the type of counseling I did and rehabilitation that I was in and what I’ve learned about myself, I was able to change some behaviors and recognize that and change those.”
“That’s a really tricky question. For me personally, I think it was hereditary. My father and my brother are both alcoholics, so I think I have the addictive gene. Personally, I didn’t believe that I could be an alcoholic because I was female, and I didn’t think that women could be alcoholics. I think it can also come down to circumstance as well in terms of overuse can just cause you to become addicted to that.”
“I think past life, like childhood or really what’s happened to you in your life. You want to forget. Do you understand? Forget things or to cope with stuff that’s going to happen.”
6. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNODC. UNODC World Drug Report 2020: Global Drug Use Rising; While COVID-19 Has Far Reaching Impact on Global Drug Markets. United Nations: Office on Drugs and Crime. 2020. Available online: https://www.unodc.org/unodc/en/press/releases/2020/June/media-advisory---global-launch-of-the-2020-world-drug-report.html (accessed on 20 March 2025).
- Brady, J.E.; Wunsch, H.; DiMaggio, C.; Lang, B.H.; Giglio, J.; Li, G. Prescription Drug Monitoring and Dispensing of Prescription Opioids. Public Health Rep. 2014, 129, 139–147. [Google Scholar] [CrossRef]
- Degenhardt, L.; Charlson, F.; Mathers, B.; Hall, W.D.; Flaxman, A.D.; Johns, N.; Vos, T. The global epidemiology and burden of opioid dependence: Results from the global burden of disease 2010 study. Addiction 2014, 109, 1320–1333. [Google Scholar] [CrossRef] [PubMed]
- Slabbert, I.; Greene, M.C.; Womersley, J.S.; Olateju, O.I.; Soboka, M.; Lemieux, A.M. Women and substance use disorders in low- and middle-income countries: A call for advancing research equity in prevention and treatment. Subst. Abus. 2020, 41, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Tuchman, E. Women and Addiction: The Importance of Gender Issues in Substance Abuse Research. J. Addict. Dis. 2010, 29, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Madhombiro, M.; Kidd, M.; Dube, B.; Dube, M.; Mutsvuke, W.; Muronzie, T.; Zhou, D.T.; Derveeuw, S.; Chibanda, D.; Chingono, A.; et al. Effectiveness of a psychological intervention delivered by general nurses for alcohol use disorders in people living with HIV in Zimbabwe: A cluster randomized controlled trial. J. Int. AIDS Soc. 2020, 23, e25641. [Google Scholar] [CrossRef]
- Mariapun, J.; Hairi, N.N.; Ng, C.-W. Socioeconomic Differences in Smoking and Cessation Across a Period of Rapid Economic Growth in an Upper-Middle-Income Country. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob. 2019, 21, 1539–1546. [Google Scholar] [CrossRef]
- Gibson, K.; Hutton, F. Women Who Inject Drugs (WWID): Stigma, Gender and Barriers to Needle Exchange Programmes (NEPs). Contemp. Drug Probl. 2021, 48, 276–296. [Google Scholar] [CrossRef]
- D’Andrade, R.G. Cultural meaning systems. In Culture Theory: Essays on Mind, Self, and Emotions; Shwede, R.A., Le Vine, R.A., Eds.; Cambridge University Press: Cambridge, UK, 1984; pp. 88–119. [Google Scholar]
- Cavalli-Sforza, L.L.; Feldman, M.W.; Chen, K.H.; Dornbusch, S.M. Theory and observation in cultural transmission. Science 1982, 218, 19–27. [Google Scholar] [CrossRef]
- Hewlett, B.S.; Cavalli-Sforza, L.L. Cultural Transmission among Aka Pygmies. Am. Anthropol. 1986, 88, 922–934. [Google Scholar] [CrossRef]
- Hewlett, B.S.; Fouts, H.N.; Boyette, A.H.; Hewlett, B.L. Social learning among Congo Basin hunter–gatherers. Philos. Trans. R. Soc. B Biol. Sci. 2011, 366, 1168–1178. [Google Scholar] [CrossRef]
- Finkler, K. Physicians At Work, Patients In Pain: Biomedical Practice and Patient Response in Mexico; Routledge: London, UK, 2019. [Google Scholar]
- Price, L. Ecuadorian illness stories: Cultural knowledge in natural discourse. In Cultural Models in Language and Thought; Cambridge University Press: Cambridge, UK, 1987; pp. 313–342. [Google Scholar] [CrossRef]
- Henderson, N.L.; Dressler, W.W. Medical Disease or Moral Defect? Stigma Attribution and Cultural Models of Addiction Causality in a University Population. Cult. Med. Psychiatry 2017, 41, 480–498. [Google Scholar] [CrossRef] [PubMed]
- Reyes-García, V.; Broesch, J.; Calvet-Mir, L.; Fuentes-Peláez, N.; McDade, T.W.; Parsa, S.; Tanner, S.; Huanca, T.; Leonard, W.R.; Martínez-Rodríguez, M.R. Cultural transmission of ethnobotanical knowledge and skills: An empirical analysis from an Amerindian society. Evol. Hum. Behav. 2009, 30, 274–285. [Google Scholar] [CrossRef]
- Teixidor-Toneu, I.; Martin, G.J.; Puri, R.K.; Ouhammou, A.; Hawkins, J.A. Treating infants with frigg: Linking disease aetiologies, medicinal plant use and care-seeking behaviour in southern Morocco. J. Ethnobiol. Ethnomedicine 2017, 13, 4. [Google Scholar] [CrossRef]
- Daniulaityte, R. Making sense of diabetes: Cultural models, gender and individual adjustment to Type 2 diabetes in a Mexican community. Soc. Sci. Med. 2004, 59, 1899–1912. [Google Scholar] [CrossRef]
- Crapanzano, K.A.; Hammarlund, R.; Ahmad, B.; Hunsinger, N.; Kullar, R. The association between perceived stigma and substance use disorder treatment outcomes: A review. Subst. Abus. Rehabil. 2018, 10, 1–12. [Google Scholar] [CrossRef]
- McLellan, A.T.; Lewis, D.C.; O’Brien, C.P.; Kleber, H.D. Drug Dependence, a Chronic Medical IllnessImplications for Treatment, Insurance, and Outcomes Evaluation. JAMA 2000, 284, 1689–1695. [Google Scholar] [CrossRef]
- Camacho-Ruiz, J.A.; Galvez-Sánchez, C.M.; Galli, F.; Limiñana Gras, R.M. Patterns and Challenges in Help-Seeking for Addiction among Men: A Systematic Review. J. Clin. Med. 2024, 13, 6086. [Google Scholar] [CrossRef]
- Tsai, A.C.; Kiang, M.V.; Barnett, M.L.; Beletsky, L.; Keyes, K.M.; McGinty, E.E.; Smith, L.R.; Strathdee, S.A.; Wakeman, S.E.; Venkataramani, A.S. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLoS Med. 2019, 16, e1002969. [Google Scholar] [CrossRef]
- Acker, C.J. How crack found a niche in the American ghetto: The historical epidemiology of drug-related harm. BioSocieties 2010, 5, 70–88. [Google Scholar] [CrossRef]
- Pescosolido, B.A.; Martin, J.K.; Long, J.S.; Medina, T.R.; Phelan, J.C.; Link, B.G. “A Disease Like Any Other”? A Decade of Change in Public Reactions to Schizophrenia, Depression, and Alcohol Dependence. Am. J. Psychiatry 2010, 167, 1321–1330. [Google Scholar] [CrossRef]
- White, W.L. Addiction recovery: Its definition and conceptual boundaries. J. Subst. Abus. Treat. 2007, 33, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Placek, C. Drug Use, Recovery, and Maternal Instinct Bias: A Biocultural and Social-Ecological Approach; Lexington Books: Lanham, MD, USA, 2024. [Google Scholar]
- Canada, H. Funding: Canadian Drugs and Substances Strategy [Transparency—Other]. Available online: https://www.canada.ca/en/health-canada/services/substance-use/canadian-drugs-substances-strategy/funding.html (accessed on 14 September 2022).
- GOV.UK. Illicit Drug Users to Face Tougher Consequences. GOV.UK. Available online: https://www.gov.uk/government/news/illicit-drug-users-to-face-tougher-consequences (accessed on 14 September 2022).
- Department of Social Justice and Empowerment. National Action Plan for Drug Demand Reduction. Available online: https://socialjustice.gov.in/schemes/42 (accessed on 4 March 2025).
- Johnson, B. From Harm to Hope: A 10-Year Drugs Plan to Cut Crime and Save Lives. GOV.UK. Available online: https://www.gov.uk/government/publications/from-harm-to-hope-a-10-year-drugs-plan-to-cut-crime-and-save-lives/from-harm-to-hope-a-10-year-drugs-plan-to-cut-crime-and-save-lives (accessed on 14 September 2022).
- Government of Canada. Canadian Drugs and Substances Strategy: Substance Use Services and Supports [Policies]. 2024. Available online: https://www.canada.ca/en/health-canada/services/substance-use/canadian-drugs-substances-strategy/substance-use-services-supports.html (accessed on 5 May 2025).
- Health Canada. Personal Possession of Small Amounts of Certain Illegal Drugs in British Columbia [Backgrounders]. 2024. Available online: https://www.canada.ca/en/health-canada/news/2024/05/personal-possession-of-small-amounts-of-certain-illegal-drugs-in-british-columbia.html (accessed on 5 May 2025).
- Committee of Public Accounts. Reducing the Harm from Illegal Drugs—Committee of Public Accounts. 2024. Available online: https://publications.parliament.uk/pa/cm5804/cmselect/cmpubacc/72/report.html (accessed on 5 May 2025).
- Gupta, S. A Shifting Hospital and Shifting Dependencies in Jammu and Kashmir. 2021. Available online: https://somatosphere.com/2021/shifting-hospital-dependencies-jammu-kashmir.html/ (accessed on 5 May 2025).
- Colledge-Frisby, S.; Ottaviano, S.; Webb, P.; Grebely, J.; Wheeler, A.; Cunningham, E.B.; Hajarizadeh, B.; Leung, J.; Peacock, A.; Vickerman, P.; et al. Global coverage of interventions to prevent and manage drug-related harms among people who inject drugs: A systematic review. Lancet Glob. Health 2023, 11, e673–e683. [Google Scholar] [CrossRef]
- Parmar, A.; Chakraborty, R.; Balhara, Y.P.S. Current status of harm reduction in India: Are we doing enough? Indian J. Psychiatry 2024, 66, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Cormier, R.A.; Dell, C.A.; Poole, N. Women and Substance Abuse Problems. BMC Women’s Health 2004, 4, S8. [Google Scholar] [CrossRef] [PubMed]
- Placek, C.D.; Adair, L.; Baker, J.; Robson, S. The Sociocultural Ecology of Resilience in Women with Substance Use Disorders; SSM-Qualitative Health: London, UK, 2025. [Google Scholar] [CrossRef]
- Sharma, V.; Sarna, A.; Tun, W.; Saraswati, L.R.; Thior, I.; Madan, I.; Luchters, S. Women and substance use: A qualitative study on sexual and reproductive health of women who use drugs in Delhi, India. BMJ Open 2017, 7, e018530. [Google Scholar] [CrossRef]
- Singh, A.; Joshi, M.; Parmar, A. Substance Use Disorder among Women and Children in South Asia. In Current Perspectives on Substance Use Disorders in South Asia: Public Mental Health Aspects; Springer Nature: Berlin/Heidelberg, Germany, 2024. [Google Scholar]
- Medina-Perucha, L.; Scott, J.; Chapman, S.; Barnett, J.; Dack, C.; Family, H. A qualitative study on intersectional stigma and sexual health among women on opioid substitution treatment in England: Implications for research, policy and practice. Soc. Sci. Med. 2019, 222, 315–322. [Google Scholar] [CrossRef]
- Smiles, C.; McGovern, R.; Kaner, E.; Rankin, J. Drug and Alcohol Use in Pregnancy and Early Parenthood. In Perspectives on Midwifery and Parenthood; Springer: Cham, Germany, 2022; pp. 107–120. [Google Scholar] [CrossRef]
- Van Zyl, A.; Hunter, B.; Haddow, K. Still a Mam: Telling the Life Stories of Woman Who Have Experienced Child Removal. 2022. Available online: https://www.researchgate.net/publication/363337224_Still_A_Mam_Telling_the_life_stories_of_woman_who_have_experienced_child_removal?channel=doi&linkId=63187ef370cc936cd3eb7552&showFulltext=true (accessed on 5 May 2025).
- Murney, M.A.; Sapag, J.C.; Bobbili, S.J.; Khenti, A. Stigma and discrimination related to mental health and substance use issues in primary health care in Toronto, Canada: A qualitative study. Int. J. Qual. Stud. Health Well-Being 2020, 15, 1744926. [Google Scholar] [CrossRef]
- Avasthi, A.; Ghosh, A. Drug misuse in India: Where do we stand & where to go from here? Indian J. Med. Res. 2019, 149, 689–692. [Google Scholar] [CrossRef]
- Pierce, M.; van Amsterdam, J.; Kalkman, G.A.; Schellekens, A.; van den Brink, W. Is Europe facing an opioid crisis like the United States? An analysis of opioid use and related adverse effects in 19 European countries between 2010 and 2018. Eur. Psychiatry 2021, 64, e47. [Google Scholar] [CrossRef]
- Placek, C.; Budzielek, E.; White, L.; Williams, D. Anthropology in Evaluation: Free-listing to Generate Cultural Models. Am. J. Eval. 2023, 45, 133–145. [Google Scholar] [CrossRef]
- Quinlan, M. Considerations for Collecting Freelists in the Field: Examples from Ethobotany. Field Methods 2005, 17, 219–234. [Google Scholar] [CrossRef]
- Weller, S.C.; Romney, A.K. Systematic Data Collection; SAGE Publications: Thousand Oaks, CA, USA, 1988. [Google Scholar]
- Purzycki, B.G.; Pisor, A.C.; Apicella, C.; Atkinson, Q.; Cohen, E.; Henrich, J.; McElreath, R.; McNamara, R.A.; Norenzayan, A.; Willard, A.K.; et al. The cognitive and cultural foundations of moral behavior. Evol. Hum. Behav. 2018, 39, 490–501. [Google Scholar] [CrossRef]
- Gallegos, M.I.; Zaring-Hinkle, B.; Wang, N.; Bray, J.H. Detachment, peer pressure, and age of first substance use as gateways to later substance use. Drug Alcohol Depend. 2021, 218, 108352. [Google Scholar] [CrossRef] [PubMed]
- Devi, S.; Singh, S. Risk Factors for Drug Addiction: A Review. Indian J. Health Well-Being 2023, 14, 383–397. [Google Scholar]
- Jadidi, N.; Nakhaee, N. Etiology of Drug Abuse: A Narrative Analysis. J. Addict. 2014, 2014, 352835. [Google Scholar] [CrossRef]
- Konkolÿ Thege, B.; Colman, I.; el-Guebaly, N.; Hodgins, D.C.; Patten, S.B.; Schopflocher, D.; Wolfe, J.; Wild, T.C. Social judgments of behavioral versus substance-related addictions: A population-based study. Addict. Behav. 2015, 42, 24–31. [Google Scholar] [CrossRef]
- Lang, B.; Rosenberg, H. Nonprofessionals’ perceptions of the causes of behavioral and substance addictions. J. Addict. Dis. 2019, 37, 102–108. [Google Scholar] [CrossRef]
- Tompkins, C.N.E.; Neale, J. Delivering trauma-informed treatment in a women-only residential rehabilitation service: Qualitative study. Drugs Educ. Prev. Policy 2018, 25, 47–55. [Google Scholar] [CrossRef]
- Dobischok, S.; Archambault, L.; Goyer, M.-È. Trauma Informed Care (TIC) Interventions for Populations Experiencing Addiction and/or Homelessness: A Scoping Review of Outcomes. J. Drug Issues 2024, 00220426241263264. [Google Scholar] [CrossRef]
- Jagannarayan, N.; Hegde, I. Causes of addiction among youngsters in—A study with special reference to Mumbai City. Int. J. Indian Psychol. 2020, 8, 1545–1558. [Google Scholar]
- Lytle, A.; Apriceno, M.; Kowal, M. How intergroup contact and demographic factors influence attitudes toward and perceptions of addiction. Addict. Res. Theory 2020, 28, 425–432. [Google Scholar] [CrossRef]
- Henderson, N.L.; Dressler, W.W. Cultural Models of Substance Use Risk and Attributed Stigma: A Comparison of Young Adults in Brazil and the United States. Cross-Cult. Res. 2020, 54, 209–237. [Google Scholar] [CrossRef]
- Razaghi, E.; Farhoudian, A.; Pilevari, A.; Noroozi, A.; Hooshyari, Z.; Radfar, R.; Malekinejad, M. Identification of the socio-cultural barriers of drug addiction treatment in Iran. Heliyon 2023, 9, e15566. [Google Scholar] [CrossRef] [PubMed]
- Simpson, N. Ghar ki tension: Domesticity and distress in India’s aspiring middle class. 2023. Available online: https://rai.onlinelibrary.wiley.com/doi/10.1111/1467-9655.13956 (accessed on 5 May 2025).
- Weaver, L.J.; Karasz, A. “Tension” and distress in South Asia: A systematic literature review. SSM Ment. Health 2022, 2, 100092. [Google Scholar] [CrossRef]
- Lachaud, J.; Mejia-Lancheros, C.; Wang, R.; Wiens, K.; Nisenbaum, R.; Stergiopoulos, V.; Hwang, S.W.; O’Campo, P. Mental and substance use disorders and food insecurity among homeless adults participating in the At Home/Chez Soi study. PLoS ONE 2020, 15, e0232001. [Google Scholar] [CrossRef]
- Rollins, C.; Glass, N.E.; Perrin, N.A.; Billhardt, K.A.; Clough, A.; Barnes, J.; Hanson, G.C.; Bloom, T.L. Housing instability is as strong a predictor of poor health outcomes as level of danger in an abusive relationship: Findings from the SHARE Study. J. Interpers. Violence 2012, 27, 623–643. [Google Scholar] [CrossRef]
- Levin, Y.; Lev Bar-Or, R.; Forer, R.; Vaserman, M.; Kor, A.; Lev-Ran, S. The association between type of trauma, level of exposure and addiction. Addict. Behav. 2021, 118, 106889. [Google Scholar] [CrossRef]
- Cavanaugh, C.E.; Petras, H.; Martins, S.S. Gender-specific profiles of adverse childhood experiences, past year mental and substance use disorders, and their associations among a national sample of adults in the United States. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1257–1266. [Google Scholar] [CrossRef]
- Petruccelli, K.; Davis, J.; Berman, T. Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abus. Negl. 2019, 97, 104127. [Google Scholar] [CrossRef]
- Dube, S.R.; Felitti, V.J.; Dong, M.; Chapman, D.P.; Giles, W.H.; Anda, R.F. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics 2003, 111, 564–572. [Google Scholar] [CrossRef]
- Hser, Y.-I. Predicting Long-Term Stable Recovery from Heroin Addiction: Findings from a 33-Year Follow-Up Study. J. Addict. Dis. 2007, 26, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Pabayo, R.; Alcantara, C.; Kawachi, I.; Wood, E.; Kerr, T. The role of depression and social support in non-fatal drug overdose among a cohort of injection drug users in a Canadian setting. Drug Alcohol Depend. 2013, 132, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.; Jason, L. Sex Differences in Social Support and Self-Efficacy Within a Recovery Community. Am. J. Community Psychol. 2006, 36, 259–274. [Google Scholar] [CrossRef] [PubMed]
- Tonsing, K.N.; Tonsing, J.C.; Orbuch, T. Domestic Violence, Social Support, Coping and Depressive Symptomatology among South Asian Women in Hong Kong. J. Loss Trauma 2021, 26, 134–152. [Google Scholar] [CrossRef]
- Biswal, B.; Zhou, B.; Wen, K.; Gupta, D.; Bhatia, U.; Nadkarni, A. Explanatory models of illicit drug use in adolescents: A qualitative study from India. PLoS Glob. Public Health 2024, 4, e0003647. [Google Scholar] [CrossRef]
- Ghosh, A.; George, B.B.; Vij, J.; Pillai, R.R.; Soundappan, K.; Sharma, M.; Basu, D. Understanding Alcohol and Illicit Drug Use in Young College Students: A Qualitative Work from India Based on Social Norms Theory. Indian J. Psychol. Med. 2024, 02537176241283381. [Google Scholar] [CrossRef]
- Groshkova, T.; Best, D.; White, W. The Assessment of Recovery Capital: Properties and psychometrics of a measure of addiction recovery strengths. Drug Alcohol Rev. 2013, 32, 187–194. [Google Scholar] [CrossRef]
- Placek, C.; Wies, J. Cultural Competence for Drug Addiction and Recovery: Considerations for Research and Evaluation. Soc. Theory Health 2024, 18, 358–394. [Google Scholar]
- De Kock, C. Cultural competence and derivatives in substance use treatment for migrants and ethnic minorities: What’s the problem represented to be? Soc. Theory Health 2020, 18, 358–394. [Google Scholar] [CrossRef]
- Kleinman, A.; Benson, P. Anthropology in the Clinic: The Problem of Cultural Competency and How to Fix It. PLoS Med. 2006, 3, e294. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Placek, C.D.; Adair, L.; Jain, I.; Gupta, S.; Phadke, V.; Singh, M. Reconstructing Cross-Cultural Meanings of Addiction Among Women from Three Countries. Int. J. Environ. Res. Public Health 2025, 22, 1064. https://doi.org/10.3390/ijerph22071064
Placek CD, Adair L, Jain I, Gupta S, Phadke V, Singh M. Reconstructing Cross-Cultural Meanings of Addiction Among Women from Three Countries. International Journal of Environmental Research and Public Health. 2025; 22(7):1064. https://doi.org/10.3390/ijerph22071064
Chicago/Turabian StylePlacek, Caitlyn D., Lora Adair, Ishita Jain, Sugandh Gupta, Vandana Phadke, and Maninder Singh. 2025. "Reconstructing Cross-Cultural Meanings of Addiction Among Women from Three Countries" International Journal of Environmental Research and Public Health 22, no. 7: 1064. https://doi.org/10.3390/ijerph22071064
APA StylePlacek, C. D., Adair, L., Jain, I., Gupta, S., Phadke, V., & Singh, M. (2025). Reconstructing Cross-Cultural Meanings of Addiction Among Women from Three Countries. International Journal of Environmental Research and Public Health, 22(7), 1064. https://doi.org/10.3390/ijerph22071064






