Delays in the Stroke Care Pathway in a Low-Income Setting: An Audit Study from Mozambique
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
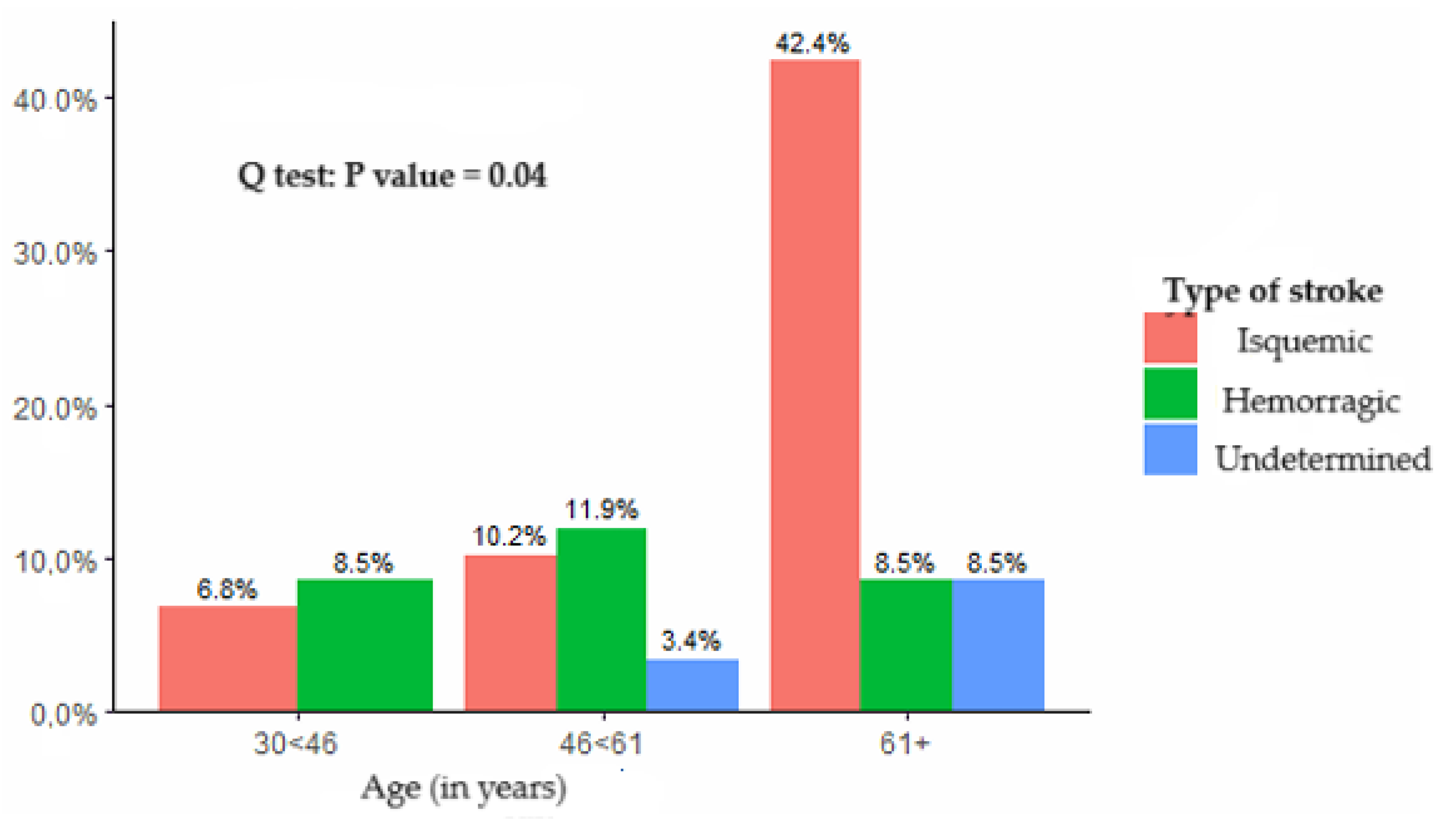
3.1. Socio-Demographic Profile
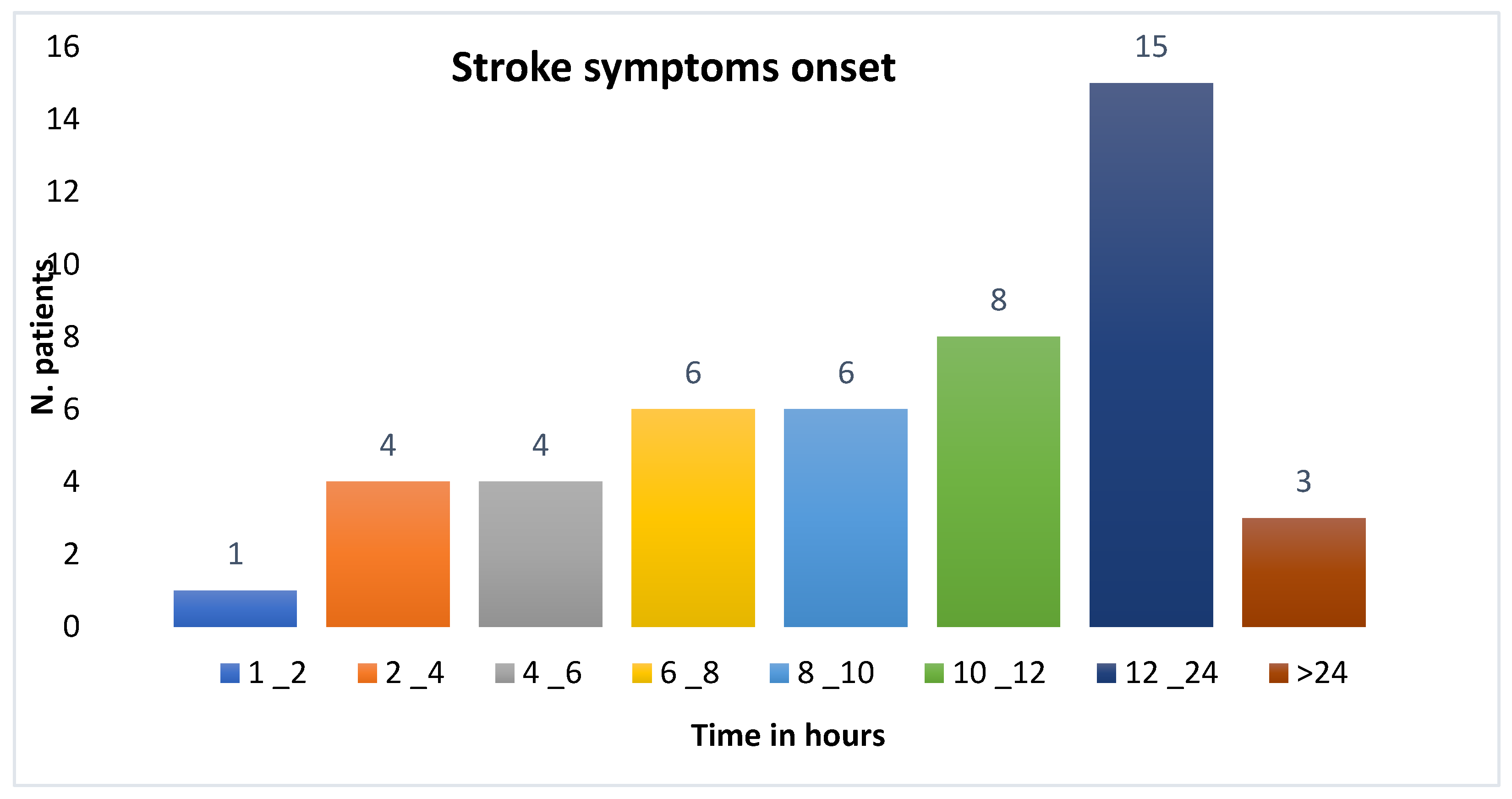
3.2. Time from Symptom Onset to Arrival at the Emergency Department
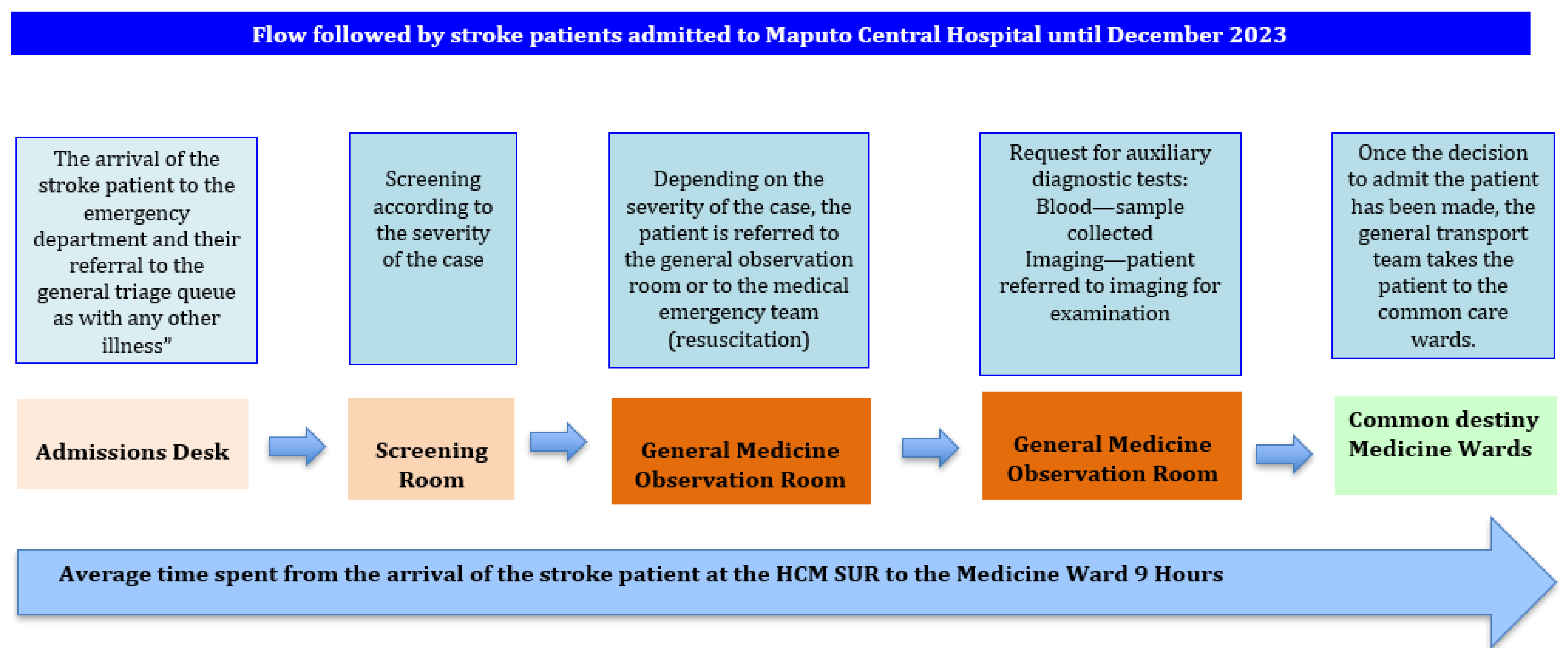
3.3. Waiting Time and Priority Assessment in the Emergency Department
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morgenstern, L.B.; Smith, W.S. Setting priorities for stroke care and research. Int. J. Stroke 2013, 8, 445–446. [Google Scholar] [CrossRef] [PubMed]
- GBD 2016 Lifetime Risk of Stroke Collaborators. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N. Engl. J. Med. 2018, 379, 2429–2437. [Google Scholar] [CrossRef]
- Saver, J.L. Time Is Brain-Quantified. 2005. Available online: http://www.americanheart.org/ (accessed on 9 July 2023).
- Wennman, I.; Carlström, E.; Fridlund, B.; Wijk, H. Actions taken affecting lead time in the care pathway for low-priority patients with a suspected stroke: A critical incident study. Int. Emerg. Nurs. 2022, 60, 101105. [Google Scholar] [CrossRef] [PubMed]
- Cash, R.E.; Boggs, K.M.; Richards, C.T.; Camargo, C.A.; Zachrison, K.S. Emergency Medical Service Time Intervals for Patients with Suspected Stroke in the United States. Stroke 2022, 29, E75–E78. [Google Scholar] [CrossRef]
- Langhorne, P.; Ramachandra, S. Organised inpatient (stroke unit) care for stroke: Network meta-analysis. Cochrane Database Syst. Rev. 2020, 2020, CD000197. [Google Scholar]
- Owolabi, M.O.; Thrift, A.G.; Mahal, A.; Ishida, M.; Martins, S.; Johnson, W.D.; Pandian, J.; Abd-Allah, F.; Yaria, J.; Phan, H.T.; et al. Primary stroke prevention worldwide: Translating evidence into action. Lancet Public Health 2022, 7, e74–e85. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e110. [Google Scholar] [CrossRef]
- Al Hashmi, A.M.; Imam, Y.; Mansour, O.Y.; Shuaib, A. Accreditation of Stroke Programs at the MENA + Region; Between Aspiration and Reality. J. Stroke Cerebrovasc. Dis. 2024, 33, 107639. [Google Scholar] [CrossRef]
- Cisse, F.A.; Damien, C.; Bah, A.K.; Touré, M.L.; Barry, M.; Djibo Hamani, A.B.; Haba, M.; Soumah, F.M.; Naeije, G. Minimal setting stroke unit in a sub-Saharan African public hospital. Front. Neurol. 2019, 10, 856. [Google Scholar] [CrossRef]
- Akinyemi, R.O.; Ovbiagele, B.; Adeniji, O.A.; Sarfo, F.S.; Abd-Allah, F.; Adoukonou, T.; Ogah, O.S.; Naidoo, P.; Damasceno, A.; Walker, R.W.; et al. Stroke in Africa: Profile, progress, prospects and priorities. Nat. Rev. Neurol. 2021, 17, 634–656. [Google Scholar] [CrossRef]
- Mandizvidza, V.; London, L.; Bryer, A. Shortfall in stroke care: A study of ischaemic stroke care practices in a South African metropole. S. Afr. Med. J. 2021, 111, 215. [Google Scholar] [CrossRef] [PubMed]
- Okekunle, A.P.; Jones, S.; Adeniji, O.; Watkins, C.; Hackett, M.; Di Tanna, G.L.; Owolabi, M.; Akinyemi, R. Stroke in Africa: A systematic review and meta-analysis of the incidence and case-fatality rates. Int. J. Stroke 2023, 18, 634–644. [Google Scholar] [CrossRef]
- Arabambi, B.; Oshinaike, O.; Ogun, S.A.; Eze, C.; Bello, A.H.; Igetei, S.; Yusuf, Y.; Olanigan, R.A.; Ashiru, S.Y. Stroke units in Nigeria: A report from a Nationwide organizational cross-sectional survey. Pan Afr. Med. J. 2022, 42, 140. [Google Scholar] [CrossRef]
- Baatiema, L.; Chan, C.K.Y.; Sav, A.; Somerset, S. Interventions for acute stroke management in Africa: A systematic review of the evidence. Syst. Rev. 2017, 6, 213. [Google Scholar] [CrossRef] [PubMed]
- Baduro, Y.; Ndala, O.; Helena Buque, D.V.; Sebastião, F.; Baco, J.; Arroz, N.; Casas, C.; Lorenzo, E.; Arroz, J.A. Stroke in Maputo central hospital, Mozambique: A cross-sectional study 2014–2018. J. Neurol. Stroke 2022, 12, 50–55. [Google Scholar] [CrossRef]
- Damasceno, A.; Gomes, J.; Azevedo, A.; Carrilho, C.; Lobo, V.; Lopes, H.; Madede, T.; Pravinrai, P.; Silva-Matos, C.; Jalla, S.; et al. An epidemiological study of stroke hospitalizations in maputo, mozambique: A high burden of disease in a resource-poor country. Stroke 2010, 41, 2463–2469. [Google Scholar] [CrossRef]
- Botelho, A.; Rios, J.; Fidalgo, A.P.; Ferreira, E.; Nzwalo, H. Organizational Factors Determining Access to Reperfusion Therapies in Ischemic Stroke-Systematic Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 16357. [Google Scholar] [CrossRef] [PubMed]
- Soto-Cámara, R.; González-Santos, J.; González-Bernal, J.; Martín-Santidrian, A.; Cubo, E.; Trejo-Gabriel-Galán, J.M. Factors Associated with Shortening of Prehospital Delay among Patients with Acute Ischemic Stroke. J. Clin. Med. 2019, 8, 1712. [Google Scholar] [CrossRef]
- Martins, S.C.O.; Matuja, S.S. Acute stroke care in low and middle-income countries. Curr. Opin. Neurol. 2025, 38, 47–53. [Google Scholar]
- Kakame, K.T.; Nakibuuka, J.; Mukiza, N.; Andia-Biraro, I.; Kaddumukasa, M.; Burant, C.; Katabira, E.; Sajatovic, M. Prevalence and factors associated with pre-hospital delay among acute stroke patients at Mulago and Kiruddu national referral hospitals, Kampala: A cross-sectional study. BMC Neurol. 2023, 23, 381. [Google Scholar] [CrossRef]
- John Oluwole, O.; Kunle Salawu, F.; Ogunniyi, A. Pre-and Intra-Hospital Delays to Acute Stroke Treatment in a Tertiary Hospital in North-East Nigeria. Available online: www.spss.com (accessed on 24 February 2025).
- Onwuegbuzie, G.A.; Abdulai, F.; Obianozie, N. Reasons for Delay in Presentation of Acute Stroke Patients in Teritary Health Centre in Abuja. SAS J. Med. 2024, 10, 365–372. [Google Scholar]
- Mamo, B.T.; Tefera, D.B.; Altaye, M.G.; Geram, F.G.; Dano, A.M.; Bekele Sana, Y.; Bonger, Z.T. Predictors of pre-hospital delay among stroke patients in Yekatit-12 hospital Addis Ababa, Ethiopia: Unmatched case-control study. Int. J. Emerg. Med. 2025, 18, 78. [Google Scholar] [CrossRef]
- Kaddumukasa, M.; Kayima, J.; Kaddumukasa, M.N.; Ddumba, E.; Mugenyi, L.; Pundik, S.; Furlan, A.J.; Sajatovic, M.; Katabira, E. Knowledge, attitudes and perceptions of stroke: A cross-sectional survey in rural and urban Uganda. BMC Res. Notes 2015, 8, 819. [Google Scholar] [CrossRef] [PubMed]
- Jma, K. Factors influencing the longer hospital stays for acute stroke patients in a tertiary hospital in Burkina Faso. J. Rehabil. Res. Pract. 2021, 2, 21–28. [Google Scholar]
- Saini, V.; Guada, L.; Yavagal, D.R. Global Epidemiology of Stroke and Access to Acute Ischemic Stroke Interventions. Neurology 2021, 97 (Suppl. 2), S6–S16. [Google Scholar] [CrossRef]
- Yakhkind, A.; Yu, W.; Goldstein, J.N.; Mayer, S.A. Code-ICH: Time is brain. Curr. Opin. Crit. Care 2025, 31, 112–116. [Google Scholar] [CrossRef]
- Martinez, J.; Mouzinho, M.; Teles, J.; Guilherme, P.; Nogueira, J.; Félix, C.; Ferreira, F.; Marreiros, A.; Nzwalo, H. Poor intensive stroke care is associated with short-term death after spontaneous intracerebral hemorrhage. Clin. Neurol. Neurosurg. 2020, 191, 105696. [Google Scholar] [CrossRef] [PubMed]
- Zewdie, A.; Debebe, F.; Kebede, S.; Azazh, A.; Laytin, A.; Pashmforoosh, G.; Hassen, G.W. Prospective assessment of patients with stroke in Tikur Anbessa Specialised Hospital, Addis Ababa, Ethiopia. Afr. J. Emerg. Med. 2017, 8, 21. [Google Scholar] [CrossRef]
- Kankam, S.B.; Habibzadeh, A.; Amirikah, M.T.; Mensah, P.K.N.; Fordjour, C.O.; Mate-Kole, M.N.; Danso, S.E.; Jalloh, M.; Osifala, O.; Kwapong, F.L.; et al. Enhancing stroke care in Ghana: A systematic review of stroke rehabilitation services. J. Stroke Cerebrovasc. Dis. 2024, 33, 1052–3057. [Google Scholar] [CrossRef]
- Baatiema, L.; Otim, M.; Mnatzaganian, G.; Aikins, A.D.G.; Coombes, J.; Somerset, S. Towards best practice in acute stroke care in Ghana: A survey of hospital services. BMC Health Serv. Res. 2017, 17, 108. [Google Scholar] [CrossRef]
- Wiyarta, E.; Fisher, M.; Kurniawan, M.; Hidayat, R.; Geraldi, I.P.; Khan, Q.A.; Widyadharma, I.P.E.; Badshah, A.; Pandian, J.D. Global Insights on Prehospital Stroke Care: A Comprehensive Review of Challenges and Solutions in Low- and Middle-Income Countries. J. Clin. Med. 2024, 13, 4780. [Google Scholar] [CrossRef] [PubMed]
- Sarfo, F.S.; Ovbiagele, B. Quantitative and qualitative analyses of herbal medication use among Ghanaian stroke survivors. J. Neurol. Sci. 2021, 427, 117540. [Google Scholar] [CrossRef]
- Akinyemi, R.O.; Ogah, O.S.; Ogundipe, R.F.; Oyesola, O.A.; Oyadoke, A.A.; Ogunlana, M.O.; Otubogun, F.M.; Odeyinka, T.F.; Alabi, B.S.; Akinyemi, J.O.; et al. Knowledge and perception of stroke amongst hospital workers in an African community. Eur. J. Neurol. 2009, 16, 998–1003. [Google Scholar] [CrossRef] [PubMed]
- Anagaw, T.F.; Melaku Mazengia, E.; Bogale, E.K.; Talie Fenta, E.; Eshetu, H.B.; Kebede, N.; Gelaw, S.S.; Zewdie, A.; Kassie, T.D. Health-seeking behavior among non-communicable disease patients globally, systematic review and meta-analysis. SAGE Open Med. 2023, 11, 20503121231215236. [Google Scholar] [CrossRef]
- Ahmed, A. Quality Metrics in Acute Stroke: Time to Own. Indian J. Crit. Care Med. 2023, 27, 786–787. [Google Scholar] [CrossRef]
- Bhalla, A.; Clark, L.; Fisher, R.; James, M. The new national clinical guideline for stroke: An opportunity to transform stroke care. Clin. Med. 2024, 24, 100025. [Google Scholar]
- Chapter 2 Organization of Stroke Services. 2023. Available online: www.strokeguideline.org (accessed on 23 February 2025).
- Lindsay, P.; Furie, K.L.; Davis, S.M.; Donnan, G.A.; Norrving, B. World Stroke Organization Global Stroke Services Guidelines and Action Plan. Int. J. Stroke 2014, 9, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Olaiya, M.T.; De Silva, D.A.; Norrving, B.; Bosch, J.; De Sousa, D.A.; Christensen, H.K.; Ranta, A.; Donnan, G.A.; Feigin, V.; et al. Global stroke statistics 2023: Availability of reperfusion services around the world. Int. J. Stroke 2024, 19, 253–270. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019, 50, E344–E418. [Google Scholar]
- Buque, H.; Vaz, D.; Lorenzo, E.; Tané, S.; Sidat, M.; Nzwalo, H. Severe neurocysticercosis in a quaternary hospital from Mozambique: Case series analysis. Clin. Neurol. Neurosurg. 2023, 233, 107913. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buque, H.; Smith, L.; Lopes, D.; Pizzol, D.; Lorenzo, E.; Arroz, N.; Bacallau, L.; Sidat, M.; Bauaze, E.N.; Nzwalo, H. Delays in the Stroke Care Pathway in a Low-Income Setting: An Audit Study from Mozambique. Int. J. Environ. Res. Public Health 2025, 22, 1008. https://doi.org/10.3390/ijerph22071008
Buque H, Smith L, Lopes D, Pizzol D, Lorenzo E, Arroz N, Bacallau L, Sidat M, Bauaze EN, Nzwalo H. Delays in the Stroke Care Pathway in a Low-Income Setting: An Audit Study from Mozambique. International Journal of Environmental Research and Public Health. 2025; 22(7):1008. https://doi.org/10.3390/ijerph22071008
Chicago/Turabian StyleBuque, Helena, Lee Smith, Dino Lopes, Damiano Pizzol, Elder Lorenzo, Nachan Arroz, Lazara Bacallau, Mohsin Sidat, Evangelina Namburete Bauaze, and Hipólito Nzwalo. 2025. "Delays in the Stroke Care Pathway in a Low-Income Setting: An Audit Study from Mozambique" International Journal of Environmental Research and Public Health 22, no. 7: 1008. https://doi.org/10.3390/ijerph22071008
APA StyleBuque, H., Smith, L., Lopes, D., Pizzol, D., Lorenzo, E., Arroz, N., Bacallau, L., Sidat, M., Bauaze, E. N., & Nzwalo, H. (2025). Delays in the Stroke Care Pathway in a Low-Income Setting: An Audit Study from Mozambique. International Journal of Environmental Research and Public Health, 22(7), 1008. https://doi.org/10.3390/ijerph22071008








