Users’ Perceptions of Access to and Quality of Public Health Services in Brazil: A Cross-Sectional Study in Metropolitan Rio de Janeiro, Including Pharmaceutical Services
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Data Collection Instrument
2.3. Data Collection and Inclusion Criteria
2.4. Data Analysis
2.5. Ethical Aspects
3. Results
3.1. Population Characteristics
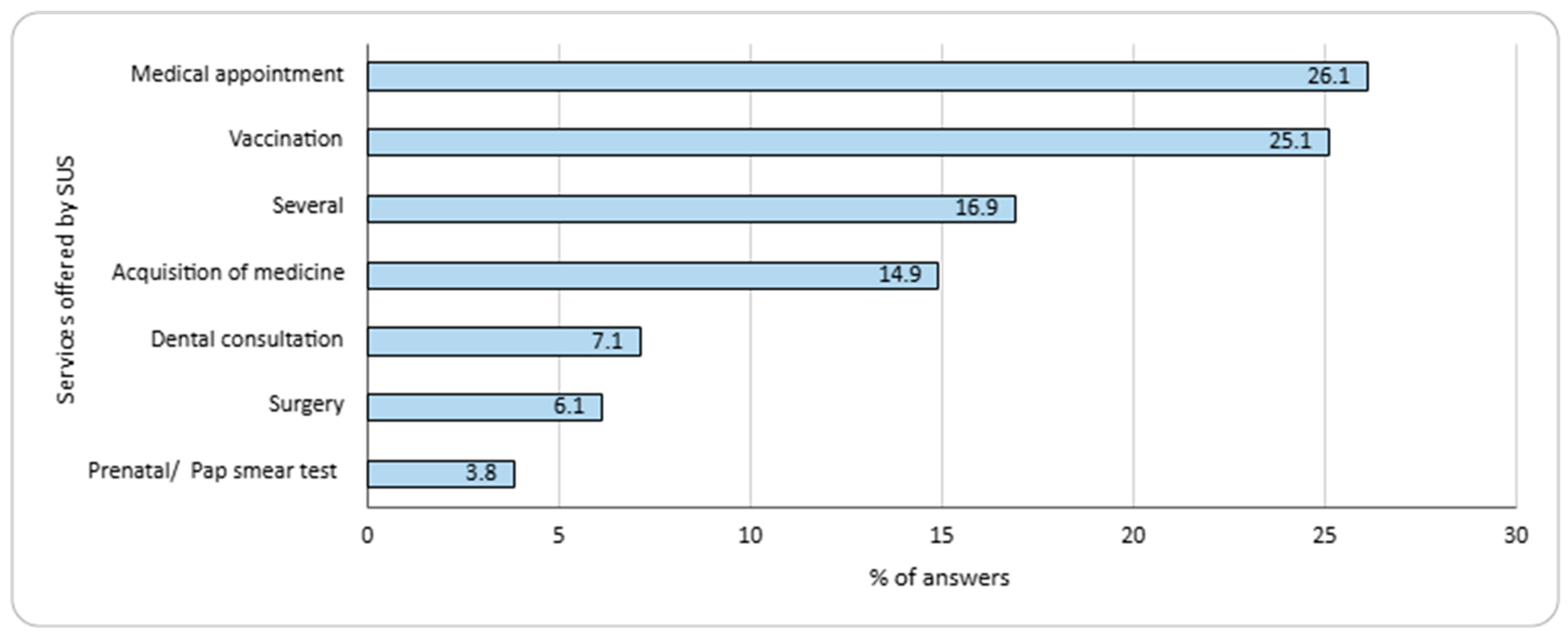
3.2. Responses from SUS Users
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brasil. Constituição da República Federativa do Brasil; Senado Federal: Brasília, Brazil, 1988.
- Brasil. Lei nº 8.080, de 19 de setembro de 1990. In Dispõe Sobre as Condições para a Promoção, Proteção e Recuperação da Saúde, a Organização e o Funcionamento dos Serviços Correspondentes e dá Outras Providências; Presidência da República: Brasília, Brazil, 1990. [Google Scholar]
- Ministério da Saúde. Carta dos Direitos dos Usuários da Saúde, 3rd ed.; Ministério da Saúde: Brasília, Brazil, 2011.
- Castro, M.C.; Massuda, A.; Almeida, G.; Menezes-Filho, N.A.; Andrade, M.V.; de Souza Noronha, K.V.M.; Rocha, R.; Macinko, J.; Hone, T.; Tasca, R.; et al. Brazil’s unified health system: The first 30 years and prospects for the future. Lancet 2019, 394, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Emenda Constitucional nº 29, de 13 de Setembro de 2000. In Constituição da República Federativa do Brasil de 1988: Altera os arts. 34, 35, 156, 160, 167 e 198 da Constituição Federal e Acrescenta Artigo ao Ato das Disposições Constitucionais Transitórias, para Assegurar os Recursos Mínimos para o Financiamento das Ações e Serviços Públicos de Saúde; Presidência da República: Brasília, Brazil, 2000. [Google Scholar]
- Brasil. Ministério da Saúde. Portaria Nº 4.279, de 30 de Dezembro de 2010. In Estabelece Diretrizes para a Organização da Rede de Atenção à Saúde no Âmbito do Sistema Único de Saúde (SUS); Diário Oficial da União: Brasília, Brazil, 2010. [Google Scholar]
- Gomes, R.M.; Barbosa, W.B.; Godman, B.; Costa, J.D.O.; Ribeiro Junior, N.G.; Simão Filho, C.; Cherchiglia, M.L.; Acurcio, F.D.A.; Guerra Junior, A.A. Effectiveness of maintenance immunosuppression therapies in a matched-pair analysis cohort of 16 years of renal transplant in the Brazilian National Health System. Int. J. Environ. Res. Public Health 2020, 17, 1974. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Ministério da Saúde. Atenção Primária e Atenção Especializada: Conheça os Níveis de Assistência do Maior Sistema Público de Saúde do Mundo. Available online: https://www.gov.br/saude/pt-br/assuntos/noticias/2022/marco/atencao-primaria-e-atencao-especializada-conheca-os-niveis-de-assistencia-do-maior-sistema-publico-de-saude-do-mundo (accessed on 15 August 2024).
- Brasil. Ministério da Saúde. Saúde da Família: Uma Estratégia para a Reorganização do Modelo Assistencial; Ministério da Saúde: Brasília, Brazil, 1997.
- Andrade, M.V.; Coelho, A.Q.; Neto, M.X.; de Carvalho, L.R.; Atun, R.; Castro, M.C. Brazil’s Family Health Strategy: Factors associated with programme uptake and coverage expansion over 15 years (1998–2012). Health Policy Plan. 2018, 33, 368–380. [Google Scholar] [CrossRef] [PubMed]
- Starfield, B.; Shi, L.; Macinko, J. Contribution of primary care to health systems and health. Milbank Q. 2005, 83, 457–502. [Google Scholar] [CrossRef]
- World Health Organization; Organization for Economic Co-operation and Development; International Bank for Reconstruction and Development. Delivering Quality Health Services: A Global Imperative for Universal Health Coverage; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Brasil. Ministério da Saúde. Portaria GM/MS nº 635, de 22 de maio de 2023. In Institui, Define e Cria Incentivo Financeiro Federal de Implantação, Custeio e Desempenho para as Modalidades de Equipes Multiprofissionais na Atenção Primária à Saúde; Diário Oficial da União: Brasília, Brazil, 2023. [Google Scholar]
- Brasil. Ministério da Saúde. Estratégia Saúde da Família. Available online: https://www.gov.br/saude/pt-br/composicao/saps/esf (accessed on 7 April 2025).
- Brasil. Ministério da Saúde. Secretaria de Ciência, Tecnologia e Insumos Estratégicos. In Componente Avaliação dos Serviços de Assistência Farmacêutica Básica: Resultados; Série PNAUM—Pesquisa Nacional sobre Acesso, Utilização e Promoção do Uso Racional de Medicamentos no Brasil; Caderno 4; Ministério da Saúde: Brasília, Brazil, 2017. [Google Scholar]
- Brasil. Ministério da Saúde. Portaria nº 2.077, de 17 de Setembro de 2012. In Institui a Pesquisa Nacional Sobre Acesso, Utilização e Promoção do Uso Racional de Medicamentos no Brasil (PNAUM); Diário Oficial da União: Brasília, Brazil, 2012. [Google Scholar]
- Brasil. Ministério da Saúde. Componente Básico da Assistência Farmacêutica (CBAF). Available online: https://www.gov.br/saude/pt-br/composicao/sectics/daf/cbaf (accessed on 7 April 2025).
- Brasil. Ministério da Saúde. Componente Estratégico da Assistência Farmacêutica (CESAF). Available online: https://www.gov.br/saude/pt-br/composicao/sectics/daf/cesaf (accessed on 7 April 2025).
- Brasil. Ministério da Saúde. Componente Especializado da Assistência Farmacêutica (CEAF). Available online: https://www.gov.br/saude/pt-br/composicao/sectics/daf/ceaf (accessed on 7 April 2025).
- Brasil. Ministério da Saúde. Portaria nº 111, de 28 de Janeiro de 2016. In Dispõe Sobre o Programa Farmácia Popular do Brasil (PFPB); Diário Oficial da União: Brasília, Brazil, 2016. [Google Scholar]
- Barbosa, M.M.; Nascimento, R.C.; Garcia, M.; Acurcio, F.A.; Godman, B.; Guerra, A.A., Jr.; Alvares-Teodoro, J. Strategies to improve the availability of medicines in primary health care in Brazil: Findings and implications. J. Comp. Eff. Res. 2021, 10, 243–253. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. Programa Nacional de Imunizações—Vacinação. Available online: https://www.gov.br/saude/pt-br/acesso-a-informacao/acoes-e-programas/pni (accessed on 15 August 2024).
- Fernandes, C.M.; Dias, S.L.; Ferreira, M.C.; Luna, E.J.A. COVID-19 post-vaccination in healthcare workers and vaccine effectiveness. Clinics 2021, 76, 100109. [Google Scholar] [CrossRef]
- Paixao, E.S.; Wong, K.L.M.; Alves, F.J.O.; de Araújo Oliveira, V.; Cerqueira-Silva, T.; Júnior, J.B.; Machado, T.M.; Junior, E.P.P.; Boaventura, V.S.; Penna, G.O.; et al. CoronaVac vaccine is effective in preventing symptomatic and severe COVID-19 in pregnant women in Brazil: A test-negative case-control study. BMC Med. 2022, 20, 146. [Google Scholar] [CrossRef]
- Zheng, C.; Shao, W.; Chen, X.; Zhang, B.; Wang, G.; Zhang, W. Real-world effectiveness of COVID-19 vaccines: A literature review and meta-analysis. Int. J. Infect. Dis. 2021, 114, 252–260. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. Assistência Farmacêutica e Insumos Estratégicos: Sobre o DAF. Available online: https://www.gov.br/saude/pt-br/composicao/sectics/daf (accessed on 13 March 2025).
- Hasenclever, L.; Miranda, C.; Chaves, G.; Peixoto, A.L.A.; Mattos, L.V.; Viana, J.S. Controversial aspects of the concept of health needs and their impact on the accessibility of medicine and health services. Cien. Saude Colet. 2021, 26, 5401–5410. [Google Scholar] [CrossRef]
- Boing, A.; Andrade, F.; Bertoldi, A.; Peres, K.; Massuda, A.; Boing, A. Prevalências e desigualdades no acesso aos medicamentos por usuários do Sistema Único de Saúde no Brasil em 2013 e 2019. Cad. Saude Publica 2022, 28, e280316. [Google Scholar] [CrossRef]
- Conselho Federal de Farmácia. Nossos dados. Available online: https://site.cff.org.br/estatistica (accessed on 15 August 2024).
- Faraco, E.B.; Guimarães, L.; Anderson, C.; Leite, S.N. The pharmacy workforce in public primary healthcare centers: Promoting access and information on medicines. Pharm. Pract. 2020, 18, 2048. [Google Scholar] [CrossRef] [PubMed]
- Peixoto, R.T.; Campos, M.R.; Luiza, V.L.; Mendes, L.V. O farmacêutico na atenção primária à saúde no Brasil: Análise comparativa 2014–2017. Saúde Debate 2022, 46, 358–375. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. Portaria n° 154, de 24 de Janeiro de 2008. Cria os Núcleos de Apoio à Saúde da Família—NASF. Diário Oficial da União, 25 January 2008. [Google Scholar]
- Brasil. Ministério da Saúde. Equipe de Saúde da Família. Available online: https://www.gov.br/saude/pt-br/composicao/saps/esf/equipe-saude-da-familia (accessed on 27 March 2025).
- Cadastro Nacional de Estabelecimentos de Saúde (CNES); Federação Brasileira de Hospitais. Cenário dos Hospitais no Brasil 2021–2022; CNES: Brasília, Brazil, 2022.
- Brasil. Ministério da Saúde. Agência Nacional de Saúde Suplementar. Setor de Planos de Saúde Fecha 2024 com Números Recordes de Beneficiários. Available online: https://www.gov.br/ans/pt-br/assuntos/noticias/numeros-do-setor/setor-de-planos-de-saude-fecha-2024-com-numeros-recordes-de-beneficiarios (accessed on 12 March 2025).
- de Jesus, W.L.; Assis, M.M. Systematic review about the concept of access to health services: Planning contributions. Cien. Saude Colet. 2010, 15, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Ministério da Saúde. Regiões de Saúde. Available online: https://www.gov.br/saude/pt-br/composicao/saps/programa-cuida-mais-brasil/regioes-de-saude (accessed on 15 August 2024).
- Governo do Estado do Rio de Janeiro. Diagnóstico de Saúde da Região Metropolitana I; Secretaria de Saúde: Rio de Janeiro, Brazil, 2020.
- Governo do Estado do Rio de Janeiro. Diagnóstico de Saúde da Região Metropolitana II; Secretaria de Saúde: Rio de Janeiro, Brazil, 2020.
- Casa Fluminense. Mapa da Desigualdade 2020: Região Metropolitana do Rio de Janeiro. Available online: https://www.casafluminense.org.br/wp-content/uploads/2020/07/mapa-da-desigualdade-2020-final_compressed.pdf (accessed on 15 January 2025).
- Brasil. Lei nº 8.142, de 28 de Dezembro de 1990. In Dispõe Sobre a Participação da Comunidade na Gestão do Sistema Único de Saúde (SUS) e Sobre as Transferências Intergovernamentais de Recursos Financeiros na Área da Saúde e dá Outras Providências; Presidência da República: Brasília, Brazil, 1990. [Google Scholar]
- Silva, R.C.C.; de Novais, M.A.P.; Zucchi, P. Social participation in the unified health system of Brazil: An exploratory study on the adequacy of health councils to resolution 453/2012. BMC Health Serv. Res. 2021, 21, 1120. [Google Scholar] [CrossRef]
- Santos, C.L.; Santos, P.M.; Pessali, H.F.; Rover, A.J. Health councils and dissemination of SUS management instruments: An analysis of portals in Brazilian capitals. Cien. Saude Colet. 2020, 25, 4389–4399. [Google Scholar] [CrossRef]
- Koler, J.; Martinez, M.G. Participatory health councils and good governance: Healthy democracy in Brazil? Int. J. Equity Health 2015, 14, 21. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. Secretaria de Ciência, Tecnologia e Insumos Estratégicos. In Componente Populacional: Introdução, Método e Instrumentos; Série PNAUM—Pesquisa Nacional sobre Acesso, Utilização e Promoção do Uso Racional de Medicamentos no Brasil; Caderno 1; Ministério da Saúde: Brasília, Brazil, 2016. [Google Scholar]
- Brasil. Ministério da Saúde. Portaria nº 1.645, de 2 de Outubro de 2015. In Dispõe Sobre o Programa Nacional de Melhoria do Acesso e da Qualidade da Atenção Básica (PMAQ-AB); Ministério da Saúde: Brasília, Brazil, 2015. [Google Scholar]
- Protásio, A.P.L.; Gomes, L.B.; Machado Ldos, S.; Valença, A.M.G. Satisfação do usuário da atenção básica em saúde por regiões do Brasil: 1º ciclo de avaliação externa do PMAQ-AB. Cien. Saude Colet. 2017, 22, 1829–1844. [Google Scholar] [CrossRef]
- Lima, J.G.; Giovanella, L.; Fausto, M.C.R.; Bousquat, A.; da Silva, E.V. Atributos essenciais da atenção primária à saúde: Resultados nacionais do PMAQ-AB. Saude Debate 2018, 42, 52–66. [Google Scholar] [CrossRef]
- Abreu, D.M.X.; Araújo, L.H.L.; Reis, C.M.R.D.; Lima, Â.M.L.D.; Santos, A.F.D.; Jorge, A.O.; Fonseca Sobrinho, D.; Machado, A.T.G.D.M. Service users’ perception about healthcare provided by teams participating in the National Program for Primary Care Access and Quality Improvement in Brazil. Epidemiol. Serv. Saude 2018, 27, e2017111. [Google Scholar] [CrossRef]
- Instituto de Pesquisa Econômica Aplicada (IPEA). Sistema de Indicadores de Percepção Social (SIPS). Available online: https://www.ipea.gov.br/portal/images/stories/PDFs/SIPS/110207_sipssaude.pdf (accessed on 15 August 2024).
- Fonseca, G.S.; Paulino, T.S.C.; Morais, I.F.; Valença, C.N.; Germano, R.M. Percepção de usuários e profissionais de saúde sobre o sistema único de saúde no município de Santa Cruz-RN. Rev. Bras. Promoc. Saude 2013, 25, 455–461. [Google Scholar] [CrossRef]
- Hamada, R.K.F.; Almeida, V.O.C.; Brasil, I.C.F.; Souza, S.G.; Luzia, R.A.B.; Campos, E.M.S.; Leite, I.C.G. Conhecendo o Sistema Único de Saúde: Um olhar da população. Rev. APS 2020, 504–515. [Google Scholar] [CrossRef]
- Szwarcwald, C.L.; Damacena, G.N.; Souza Júnior, P.R.; Almeida, W.S.; Malta, D.C. Perception of the Brazilian population on medical health care. Brazil, 2013. Cien. Saude Colet. 2016, 21, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, G.L.; Xavier, C.C.; Ribeiro, A.P.; Proietti, F.A. Users’ perception about primary care attributes in a metropolitan region of Minas Gerais. APS Rev. 2022, 4, 46–53. [Google Scholar] [CrossRef]
- Souza, J.S.; Reis, E.A.; Godman, B.; Campbell, S.M.; Meyer, J.C.; Sena, L.W.P.; Godói, I.P.D. Users’ perceptions of access to and quality of Unified Health System services in Brazil: A cross-sectional study and implications to healthcare management challenges. Int. J. Environ. Res. Public Health 2024, 21, 721. [Google Scholar] [CrossRef]
- Dornas, B.S.S.; Reis, E.A.; Campos, A.A.O.; Godói, I.P.D. Percepções sobre os serviços de saúde pública em Macaé-RJ: Um estudo transversal. Rev. Saúde Pública Paraná 2024, 7, 1–20. [Google Scholar] [CrossRef]
- Kuschnir, R.; Chorny, A.; Lira, A.M.L.; Sonoda, G.; Fonseca, T.M.P. Regionalização no estado do Rio de Janeiro: O desafio de aumentar acesso e diminuir desigualdades. In A Gestão do Sus no Âmbito Estadual: O Caso do Rio de Janeiro; Ugá, M.A.D., Martins, M., Braga Neto, F.C., Eds.; Editora Fiocruz: Rio de Janeiro, Brazil, 2010; pp. 215–240. [Google Scholar]
- Massuda, A.; Hone, T.; Leles, F.A.G.; Castro, M.C.; Atun, R. The Brazilian health system at crossroads: Progress, crisis and resilience. BMJ Glob. Health 2018, 3, e000829. [Google Scholar] [CrossRef]
- Campbell, S.M.; Roland, M.O.; Buetow, S.A. Defining quality of care. Soc. Sci. Med. 2000, 51, 1611–1625. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística (IBGE). Censo Demográfico Brasileiro de 2022. Rio de Janeiro, Brazil, 2022. Available online: https://www.ibge.gov.br/estatisticas/sociais/populacao/22827-censo-demografico-2022.html?edicao=35938&t=resultados (accessed on 15 August 2024).
- Secretaria de Estado da Casa Civil e Desenvolvimento Econômico do Rio de Janeiro. Caderno Regional do Estado do Rio de Janeiro: Região Metropolitana Desenvolvimento Socioeconômico 2007/2014. 2017. Available online: https://www.gov.br/empresas-e-negocios/pt-br/portais-desconhecidos/observatorioapl/biblioteca-apl/publicacoes/caderno-regional-metropolitana-rj.pdf (accessed on 15 August 2024).
- IBGE—Instituto Brasileiro de Geografia e Estatística. Produto Interno Bruto dos Municípios. Available online: https://www.ibge.gov.br/estatisticas/economicas/contas-nacionais/9088-produto-interno-bruto-dos-municipios.html?t=pib-por-municipio&c=1100031 (accessed on 15 August 2024).
- Bolfarine, H.; Bussab, W.O. Elementos de Amostragem; Bucher: São Paulo, Brazil, 2005. [Google Scholar]
- Galloway, A. Non-Probability Sampling. In Encyclopedia of Social Measurement; Kempf-Leonard, K., Ed.; Elsevier: Amsterdam, The Netherlands, 2005; pp. 859–864. [Google Scholar] [CrossRef]
- World Health Organization. Medication Safety in Polypharmacy; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Brasil. Histórico de Cotação; Banco Central do Brasil: Brasília, Brazil, 2024. Available online: https://www.bcb.gov.br/estabilidadefinanceira/historicocotacoes (accessed on 15 August 2024).
- IBGE—Agência de Notícias Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde 2019: Informações sobre Domicílios, Acesso e Utilização dos Serviços de Saúde. Rio de Janeiro, 2020. Available online: https://biblioteca.ibge.gov.br/visualizacao/livros/liv101748.pdf (accessed on 27 March 2025).
- Alves, M.G.M.; Casotti, E.; Oliveira, L.G.D.; Machado, M.T.C.; Almeida, P.F.; Corvino, M.P.F.; Marin, J.; Flauzino, R.F.; Montenegro, L.A.A. Factors affecting access to the Family Health Strategy teams in Brazil. Saude Debate 2014, 38, 34–51. [Google Scholar] [CrossRef]
- IBGE—Agência de Notícias Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde 2019: Atenção Primária à Saúde e Informações Antropométricas. Rio de Janeiro, 2021. Available online: https://www.pns.icict.fiocruz.br/wp-content/uploads/2021/02/liv101758.pdf (accessed on 27 March 2025).
- Angus Reid Institute. CMA Report: Public Opinion on Healthcare in Canada. 2023. Available online: https://angusreid.org/wp-content/uploads/2023/08/2023.08.17_CMA.pdf (accessed on 15 August 2024).
- NHS—National Health Service. Understanding Public Perceptions and Attitudes to the NHS. NHS Confederation 2023. Available online: https://www.nhsconfed.org/publications/understanding-public-perceptions-and-attitudes-nhs (accessed on 15 August 2024).
- Viana, L.F.; Silva, G.H.; Godói, I.P.D. Financiamento da saúde pública no estado do Rio de Janeiro: Panorama (2015–2018), desafios e reflexões. J. Assist. Farm. Farm. 2024, 9, 35–48. [Google Scholar] [CrossRef]
- Costa, K.S.; Tavares, N.U.L.; Nascimento Júnior, J.M.d.; Mengue, S.S.; Álvares, J.; Junior, A.A.G.; de Assis Acurcio, F.; Soeiro, O.M. Pharmaceutical services in the primary health care of the Brazilian Unified Health System: Advances and challenges. Rev. Saude Publica 2017, 51, 3s. [Google Scholar] [CrossRef]
- Conselho Federal de Farmácia. XXXVII Conasems: CFF Debate Papel do Farmacêutico na Atenção Primária. 2023. Available online: https://site.cff.org.br/noticia/noticias-do-cff/21/07/2023/xxxvii-conasems-cff-debate-papel-do-farmaceutico-na-atencao-primaria (accessed on 27 March 2025).
| Variable | n | (%) |
|---|---|---|
| Gender | ||
| Female | 109 | 54.5% |
| Male | 87 | 43.5% |
| Other | 4 | 2.0% |
| Age Profile (years) | ||
| 18–25 | 36 | 18.0% |
| 26–45 | 72 | 36.0% |
| 46–60 | 53 | 26.5% |
| More than 60 | 39 | 19.5% |
| Skin color | ||
| White | 74 | 37.0% |
| Black | 48 | 24.0% |
| Brown | 60 | 30.0% |
| Other | 18 | 9.0% |
| Education level * | ||
| Never attended school | 1 | 0.5% |
| Incomplete elementary school | 26 | 13.0% |
| Completed elementary school | 14 | 7.0% |
| Incomplete high school | 12 | 6.0% |
| Completed high school | 65 | 32.5% |
| Incomplete college | 33 | 16.5% |
| Completed college or more | 24 | 12.0% |
| Family Income ** (Number of times the minimum wage ***) | ||
| Up to 1 | 31 | 15.5% |
| 1–2 | 34 | 17.0% |
| 2–3 | 20 | 10.0% |
| 3–5 | 25 | 12.5% |
| 5–10 | 9 | 4.5% |
| 10–20 | 3 | 1.5% |
| >20 | 0 | 0.0% |
| Use of SUS services—Yes | 172 | 86.0% |
| Has a private health plan—Yes | 58 | 29.0% |
| Access to SUS Services n (%) | ||||
|---|---|---|---|---|
| Frequency | Very Good/Good | Neither Good nor Bad | Bad/Very Bad | p-Value |
| Always | 58 (68.2%) | 15 (17.7) | 12 (14.1%) | 0.002 |
| Frequently | 19 (57.6%) | 11 (33.3%) | 3 (9.1%) | |
| Sometimes/Rarely/ Never | 23 (40.0%) | 16 (27.1%) | 20 (33.9%) | |
| TOTAL * | 100 (56.5%) | 42 (23.7%) | 35 (19.8%) | |
| Quality of SUS services n (%) | ||||
| Frequency | Very Good/Good | Neither Good nor Bad | Bad/Very Bad | p-Value |
| Always | 55 (60.4%) | 23 (25.3%) | 13 (14.3%) | |
| Frequently | 19 (55.9%) | 11 (32.3%) | 4 (11.8%) | |
| Sometimes/Rarely/ Never | 25 (41.7%) | 16 (26.7%) | 19 (31.6%) | 0.045 |
| TOTAL ** | 99 (53.5%) | 50 (27.0%) | 36 (19.5%) | |
| Access to SUS Services n (%) | ||||
|---|---|---|---|---|
| Family Income (Number of Times the Minimum Wage) | Very Good/Good | Neither Good nor Bad | Bad/Very Bad | p-Value |
| Up to 1 | 25 (83.3%) | 3 (10.0%) | 2 (6.7%) | |
| 1–2 | 19 (57.6%) | 8 (24.2%) | 6 (18.2%) | |
| 2–3 | 8 (47.1%) | 6 (35.3%) | 3 (17.6%) | |
| >3 | 11 (36.7%) | 11 (36.7%) | 8 (26.6%) | 0.024 |
| TOTAL * | 63 (57. 3%) | 28 (25.4%) | 19 (17.3%) | |
| Quality of SUS services n (%) | ||||
| Family Income (Number of Times the Minimum Wage) | Very Good/Good | Neither Good nor Bad | Bad/Very Bad | p-Value |
| Up to 1 | 23 (76.7%) | 5 (16.7%) | 2 (6.6%) | |
| 1–2 | 17 (51.5%) | 11 (33.3%) | 5 (15.2%) | |
| 2–3 | 9 (45.0%) | 7 (35.0%) | 4 (20,0%) | 0.149 |
| >3 | 13 (40.6%) | 12 (37.5%) | 7 (21.9%) | |
| TOTAL ** | 62 (53. 9%) | 35 (30.4%) | 18 (15.7%) | |
| Questions | Answers n (%) | |||||
|---|---|---|---|---|---|---|
| Very Good | Good | Nor Good or Bad | Bad | Very Bad | Total | |
| How do you consider the process for marking medical consultations with the general practitioner through the SUS? * | 14 (8.1%) | 52 (30.1%) | 40 (23.1%) | 35 (20.2%) | 32 (18.5%) | 173 (100.0%) |
| How do you consider the process for marking medical consultations with specialists through the SUS? ** | 10 (6.2%) | 44 (27.2%) | 41 (25.3%) | 26 (16.0%) | 41 (25.3%) | 162 (100.0%) |
| How do you consider the medical care offered by the SUS? *** | 33 (18.4%) | 79 (44.1%) | 45 (25.1%) | 9 (5.0%) | 13 (7.4%) | 179 (100.0%) |
| Questions | Answers n (%) | |||||
|---|---|---|---|---|---|---|
| Always | Often | Sometimes | Rarely | Never | Total | |
| In the last three months, how often did you get the medicines you were looking for in public pharmacies? * | 42 (48.3%) | 17 (19.5%) | 20 (23.0%) | 4 (4.6%) | 4 (4.6%) | 87 (100.0%) |
| When collecting medicines from the SUS pharmacy, do the employees who deliver them provide instructions on how to use them? ** | 35 (38.9%) | 17 (18.9%) | 11 (12.2%) | 8 (8.9%) | 19 (21.1%) | 90 (100.0%) |
| Do you receive information on how to store medicines at home? *** | 18 (20.7%) | 7 (8.1%) | 15 (17.2%) | 4 (4.6%) | 43 (49.4%) | 87 (100.0%) |
| Have you already met the pharmaceutical professional at the basic health unit you frequent? **** | 14 (17.9%) | 18 (23.1%) | 5 (6.4%) | 8 (10.3%) | 33 (42.3%) | 78 (100.0%) |
| Is the pharmacist or other employees available to answer questions about the medicines? ***** | 39 (48.2%) | 15 (18.5%) | 15 (18.5%) | 2 (2.5%) | 10 (12.3%) | 81 (100.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raimundo, M.C.; Reis, E.A.; Ferraz, I.F.L.; Borges de Almeida, C.P.; Godman, B.; Campbell, S.M.; Meyer, J.C.; Godói, I.P.D. Users’ Perceptions of Access to and Quality of Public Health Services in Brazil: A Cross-Sectional Study in Metropolitan Rio de Janeiro, Including Pharmaceutical Services. Int. J. Environ. Res. Public Health 2025, 22, 967. https://doi.org/10.3390/ijerph22060967
Raimundo MC, Reis EA, Ferraz IFL, Borges de Almeida CP, Godman B, Campbell SM, Meyer JC, Godói IPD. Users’ Perceptions of Access to and Quality of Public Health Services in Brazil: A Cross-Sectional Study in Metropolitan Rio de Janeiro, Including Pharmaceutical Services. International Journal of Environmental Research and Public Health. 2025; 22(6):967. https://doi.org/10.3390/ijerph22060967
Chicago/Turabian StyleRaimundo, Mariana Crespo, Edna Afonso Reis, Igor Fradique Leandro Ferraz, Carlos Podalirio Borges de Almeida, Brian Godman, Stephen M. Campbell, Johanna C. Meyer, and Isabella Piassi Dias Godói. 2025. "Users’ Perceptions of Access to and Quality of Public Health Services in Brazil: A Cross-Sectional Study in Metropolitan Rio de Janeiro, Including Pharmaceutical Services" International Journal of Environmental Research and Public Health 22, no. 6: 967. https://doi.org/10.3390/ijerph22060967
APA StyleRaimundo, M. C., Reis, E. A., Ferraz, I. F. L., Borges de Almeida, C. P., Godman, B., Campbell, S. M., Meyer, J. C., & Godói, I. P. D. (2025). Users’ Perceptions of Access to and Quality of Public Health Services in Brazil: A Cross-Sectional Study in Metropolitan Rio de Janeiro, Including Pharmaceutical Services. International Journal of Environmental Research and Public Health, 22(6), 967. https://doi.org/10.3390/ijerph22060967








