Trends in Malignant and Benign Brain Tumor Incidence and Mobile Phone Use in the U.S. (2000–2021): A SEER-Based Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Acquisition
2.2. Statistical Analysis
2.3. Ethical Approval
3. Results
3.1. Study Population Characteristics
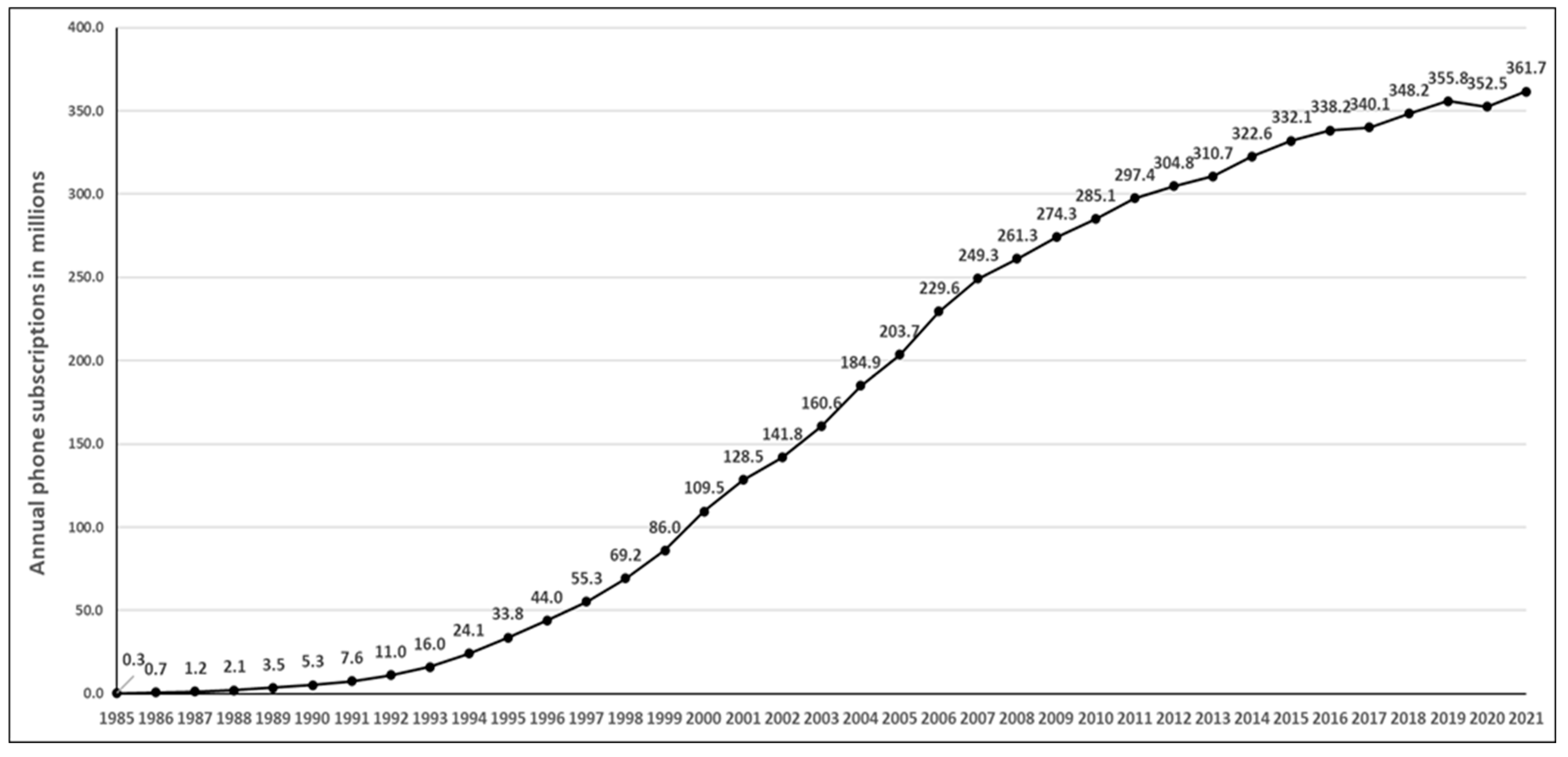
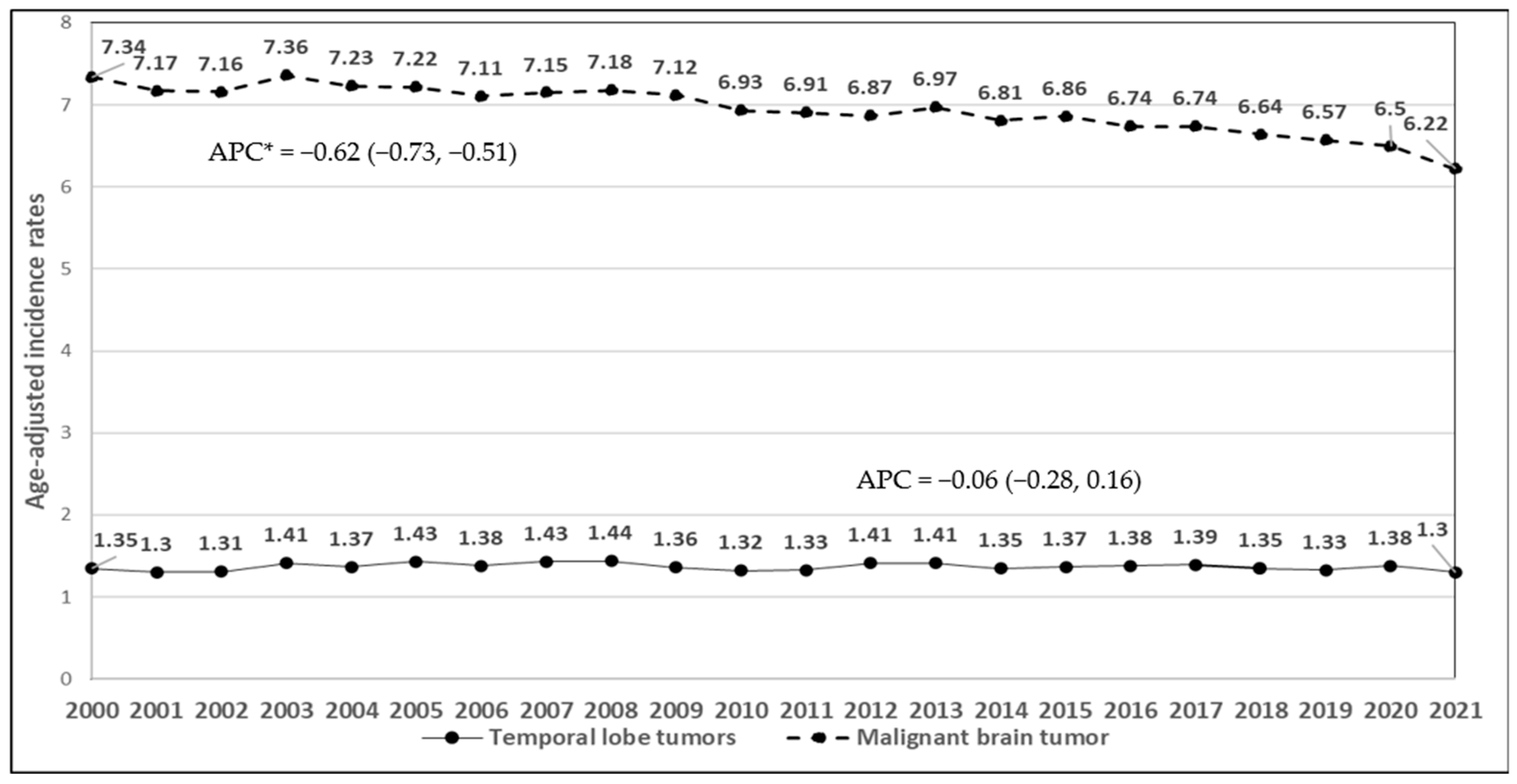
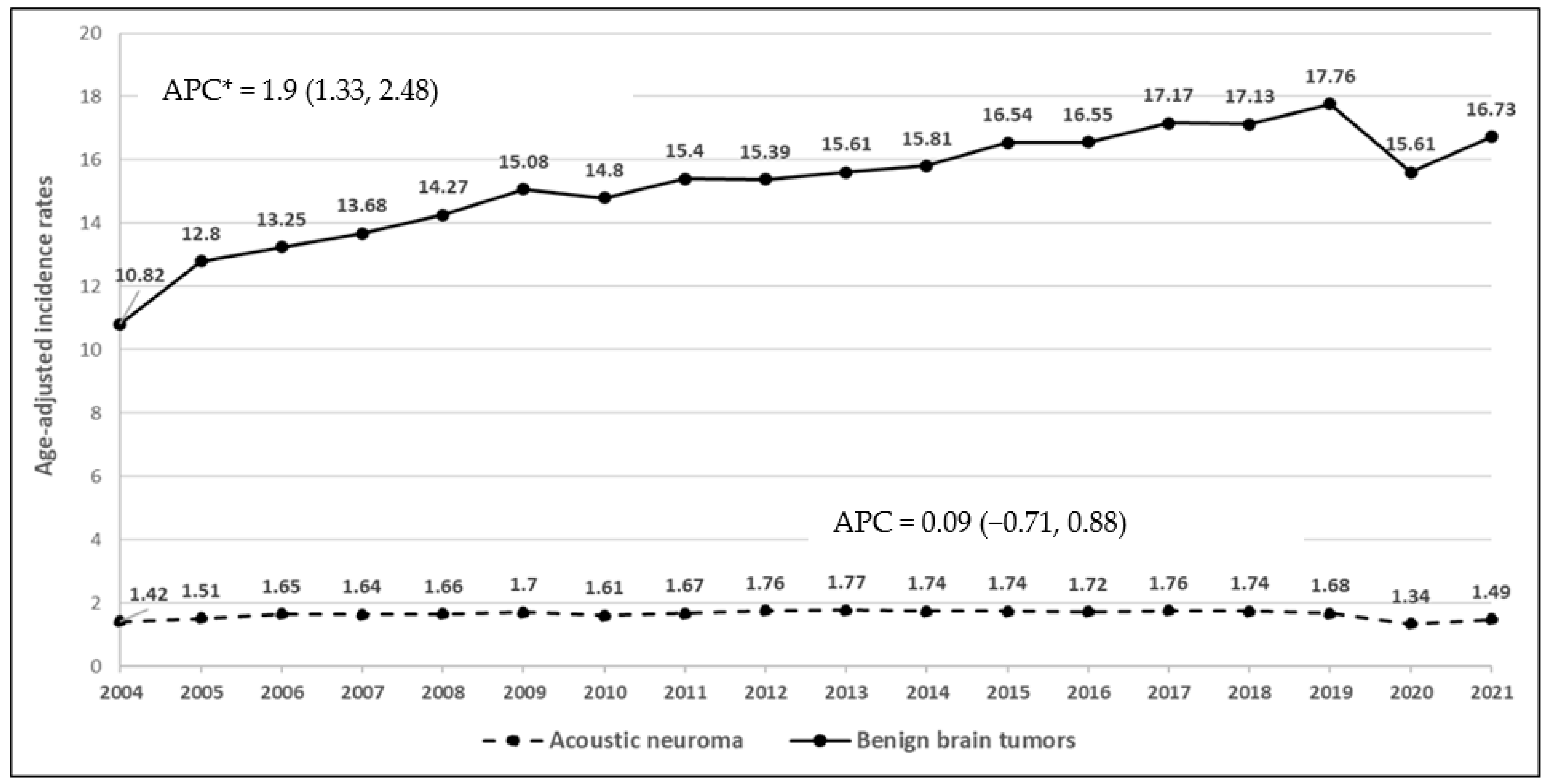
3.2. Mobile Phone Subscriptions and Time Trends of Brain Cancer Incidence Rates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SEER | Surveillance, Epidemiology, and End Results |
| IR | Incidence rate |
| APC | Annual percentage change |
| CI | Confidence interval |
| SAR | Specific absorption rate |
References
- Mead, M.N. Strong signal for cell phone effects. Environ. Health Perspect. 2008, 116, A422. [Google Scholar] [CrossRef] [PubMed]
- Bortkiewicz, A.; Gadzicka, E.; Szymczak, W. Mobile phone use and risk for intracranial tumors and salivary gland tumors—A meta-analysis. Int. J. Occup. Environ. Health 2017, 30, 27–43. [Google Scholar] [CrossRef]
- Moulder, J.E.; Foster, K.R.; Erdreich, L.S.; McNamee, J.P. Mobile phones, mobile phone base stations and cancer: A review. Int. J. Radiat. Biol. 2005, 81, 189–203. [Google Scholar] [CrossRef] [PubMed]
- Swerdlow, A.J.; Feychting, M.; Green, A.C.; Leeka Kheifets, L.K.; Savitz, D.A. Mobile phones, brain tumors, and the interphone study: Where are we now? Environ. Health Perspect. 2011, 119, 1534–1538. [Google Scholar] [CrossRef]
- Röösli, M.; Lagorio, S.; Schoemaker, M.J.; Schüz, J.; Feychting, M. Brain and Salivary Gland Tumors and Mobile Phone Use: Evaluating the Evidence from Various Epidemiological Study Designs. Annu. Rev. Public Health 2019, 40, 221–238. [Google Scholar] [CrossRef]
- National Cancer Institute. Cell Phones and Cancer Risk. 2024. Available online: https://www.cancer.gov/about-cancer/causes-prevention/risk/radiation/cell-phones-fact-sheet (accessed on 1 May 2024).
- American Chemical Society. Cellular (Cell) Phones. 2022. Available online: https://www.cancer.org/cancer/risk-prevention/radiation-exposure/cellular-phones.html (accessed on 1 April 2024).
- Morgan, L.L.; Miller, A.B.; Sasco, A.; Davis, D.L. Mobile phone radiation causes brain tumors and should be classified as a probable human carcinogen (2A) (review). Int. J. Oncol. 2015, 46, 1865–1871. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D.; Tomasi, D.; Wang, G.J.; Vaska, P.; Fowler, J.S.; Telang, F.; Alexoff, D.; Logan, J.; Wong, C. Effects of cell phone radiofrequency signal exposure on brain glucose metabolism. JAMA 2011, 305, 808–813. [Google Scholar] [CrossRef]
- Specific Absorption Rate (SAR) for Cell Phones—What It Means for You? 2019. Available online: https://www.fcc.gov/consumers/guides/specific-absorption-rate-sar-cell-phones-what-it-means-you (accessed on 15 April 2024).
- Christopher, B.; Mary Y, S.; Khandaker, M.U.; Jojo, P.J. Empirical study on specific absorption rate of head tissues due to induced heating of 4G cell phone radiation. Radiat. Phys. Chem. 2021, 178, 108910. [Google Scholar] [CrossRef]
- Davis, D.; Birnbaum, L.; Ben-Ishai, P.; Taylor, H.; Sears, M.; Butler, T.; Scarato, T. Wireless technologies, non-ionizing electromagnetic fields and children: Identifying and reducing health risks. Curr. Probl. Pediatr. Adolesc. Health Care 2023, 53, 101374. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. Non-Ionizing Radiation, Part 2: Radiofrequency Electromagnetic Fields. In International Agency for Research on Cancer Monographs on the Evaluation of Carcinogenic Risks to Humans; International Agency for Research on Cancer: Lyon, France, 2013; Available online: https://www.iarc.who.int/wp-content/uploads/2018/07/pr208_E.pdf (accessed on 28 May 2024).
- Schoemaker, M.J.; Swerdlow, A.J.; Ahlbom, A.; Auvinen, A.; Blaasaas, K.G.; Cardis, E.; Christensen, H.C.; Feychting, M.; Hepworth, S.J.; Johansen, C.; et al. Mobile phone use and risk of acoustic neuroma: Results of the Interphone case-control study in five North European countries. Br. J. Cancer 2005, 93, 842–848. [Google Scholar] [CrossRef]
- Hardell, L.; Carlberg, M. Mobile phones, cordless phones and the risk for brain tumours. Int. J. Oncol. 2009, 35, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Hardell, L.; Carlberg, M.; Hansson Mild, K. Pooled analysis of case-control studies on malignant brain tumours and the use of mobile and cordless phones including living and deceased subjects. Int. J. Oncol. 2011, 38, 1465–1474. [Google Scholar] [CrossRef] [PubMed]
- Cardis, E.; Armstrong, B.K.; Bowman, J.D.; Giles, G.G.; Hours, M.; Krewski, D.; McBride, M.; Parent, M.E.; Sadetzki, S.; Woodward, A.; et al. Risk of brain tumours in relation to estimated RF dose from mobile phones: Results from five Interphone countries. Occup. Environ. Med. 2011, 68, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Inskip, P.D.; Tarone, R.E.; Hatch, E.E.; Wilcosky, T.C.; Shapiro, W.R.; Selker, R.G.; Fine, H.A.; Black, P.M.; Loeffler, J.S.; Linet, M.S. Cellular-telephone use and brain tumors. N. Engl. J. Med. 2001, 344, 79–86. [Google Scholar] [CrossRef]
- Muscat, J.E.; Malkin, M.G.; Thompson, S.; Shore, R.E.; Stellman, S.D.; McRee, D.; Neugut, A.I.; Wynder, E.L. Handheld cellular telephone use and risk of brain cancer. JAMA 2000, 284, 3001–3007. [Google Scholar] [CrossRef]
- Muscat, J.E.; Malkin, M.G.; Shore, R.E.; Thompson, S.; Neugut, A.I.; Stellman, S.D.; Bruce, J. Handheld cellular telephones and risk of acoustic neuroma. Neurology 2002, 58, 1304–1306. [Google Scholar] [CrossRef]
- Coureau, G.; Bouvier, G.; Lebailly, P.; Fabbro-Peray, P.; Gruber, A.; Leffondre, K.; Guillamo, J.S.; Loiseau, H.; Mathoulin-Pélissier, S.; Salamon, R.; et al. Mobile phone use and brain tumours in the CERENAT case-control study. Occup. Environ. Med. 2014, 71, 514–522. [Google Scholar] [CrossRef]
- Feychting, M.; Schüz, J.; Toledano, M.B.; Vermeulen, R.; Auvinen, A.; Harbo Poulsen, A.; Deltour, I.; Smith, R.B.; Heller, J.; Kromhout, H.; et al. Mobile phone use and brain tumour risk—COSMOS, a prospective cohort study. Environ. Int. 2024, 185, 108552. [Google Scholar] [CrossRef]
- Frei, P.; Poulsen, A.H.; Johansen, C.; Olsen, J.H.; Steding-Jessen, M.; Schüz, J. Use of mobile phones and risk of brain tumours: Update of Danish cohort study. BMJ 2011, 343, d6387. [Google Scholar] [CrossRef]
- Schüz, J.; Pirie, K.; Reeves, G.K.; Floud, S.; Beral, V. Cellular Telephone Use and the Risk of Brain Tumors: Update of the UK Million Women Study. J. Natl. Cancer Inst. 2022, 114, 704–711. [Google Scholar] [CrossRef]
- Muscat, J.E.; Hinsvark, M.; Malkin, M. Mobile telephones and rates of brain cancer. Neuroepidemiology 2006, 27, 55–56. [Google Scholar] [CrossRef] [PubMed]
- Karipidis, K.; Elwood, M.; Benke, G.; Sanagou, M.; Tjong, L.; Croft, R.J. Mobile phone use and incidence of brain tumour histological types, grading or anatomical location: A population-based ecological study. BMJ Open 2018, 8, e024489. [Google Scholar] [CrossRef] [PubMed]
- The INTERPHONE Study Group. Brain tumour risk in relation to mobile telephone use: Results of the INTERPHONE international case-control study. Int. J. Epidemiol. 2010, 39, 675–694. [Google Scholar] [CrossRef] [PubMed]
- The INTERPHONE Study Group. Acoustic neuroma risk in relation to mobile telephone use: Results of the INTERPHONE international case-control study. Cancer Epidemiol. 2011, 35, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Inskip, P.D.; Hoover, R.N.; Devesa, S.S. Brain cancer incidence trends in relation to cellular telephone use in the United States. Neuro-Oncol. 2010, 12, 1147–1151. [Google Scholar] [CrossRef]
- Choi, K.H.; Ha, J.; Bae, S.; Lee, A.K.; Choi, H.D.; Ahn, Y.H.; Ha, M.; Joo, H.; Kwon, H.J.; Jung, K.W. Mobile Phone Use and Time Trend of Brain Cancer Incidence Rate in Korea. Bioelectromagnetics 2021, 42, 629–648. [Google Scholar] [CrossRef]
- Lönn, S.; Ahlbom, A.; Hall, P.; Feychting, M. Long-term mobile phone use and brain tumor risk. Am. J. Epidemiol. 2005, 161, 526–535. [Google Scholar] [CrossRef]
- Deltour, I.; Poulsen, A.H.; Johansen, C.; Feychting, M.; Johannesen, T.B.; Auvinen, A.; Schüz, J. Time trends in mobile phone use and glioma incidence among males in the Nordic Countries, 1979–2016. Environ. Int. 2022, 168, 107487. [Google Scholar] [CrossRef]
- Elwood, J.M.; Win, S.S.; Aye, P.S.; Sanagou, M. Trends in brain cancers (glioma) in New Zealand from 1995 to 2020, with reference to mobile phone use. Cancer Epidemiol. 2022, 80, 102234. [Google Scholar] [CrossRef]
- Kshettry, V.R.; Hsieh, J.K.; Ostrom, Q.T.; Kruchko, C.; Barnholtz-Sloan, J.S. Incidence of vestibular schwannomas in the United States. J. Neuro-Oncol. 2015, 124, 223–228. [Google Scholar] [CrossRef]
- National Cancer Institute. About Surveillance, Epidemiology, and End Results Program (SEER). 2023. Available online: https://seer.cancer.gov/ (accessed on 22 April 2024).
- National Cancer Institute. About the SEER Registries. 2023. Available online: https://seer.cancer.gov/registries/ (accessed on 19 April 2024).
- Site Recode ICD-O-3/WHO 2008 Edition. Available online: https://seer.cancer.gov/siterecode/icdo3_dwhoheme/index.html (accessed on 10 April 2024).
- World Bank Group. The US Bureau of Economic Analysis of US Cellular Phone Subscription Using Open World Bank Data. Available online: https://data.worldbank.org/indicator/IT.CEL.SETS.P2?locations=US (accessed on 28 April 2024).
- National Cancer Institute. Surveillance Research Program, National Cancer Institute SEER*Stat Software, version 8.4.3; National Cancer Institute: Bethesda, MD, USA, 2024. Available online: https://seer.cancer.gov/seerstat (accessed on 1 May 2024).
- Richter, A.; Adkins, V.; Selkie, E. Youth Perspectives on the Recommended Age of Mobile Phone Adoption: Survey Study. JMIR Pediatr. Parent. 2022, 5, e40704. [Google Scholar] [CrossRef] [PubMed]
- Fraser, D.K. Latency period of radiation-induced cancer. CMAJ 2011, 183, 2017. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence—SEER Research Limited-Field Data, 22 Registries, Nov 2023 Sub (2000–2021)—Linked To County Attributes—Time Dependent (1990–2022) Income/Rurality, 1969–2022 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Released April 2024, Based on the November 2023 Submission. 2022. Available online: https://seer.cancer.gov/data-software/documentation/seerstat/nov2022/ (accessed on 18 April 2024).
- U.S. Population. Available online: https://www.census.gov/popclock/ (accessed on 1 May 2024).
- Lin, D.D.; Lin, J.L.; Deng, X.Y.; Li, W.; Li, D.D.; Yin, B.; Lin, J.; Zhang, N.; Sheng, H.S. Trends in intracranial meningioma incidence in the United States, 2004–2015. Cancer Med. 2019, 8, 6458–6467. [Google Scholar] [CrossRef]
- Huang, R.Y.; Bi, W.L.; Griffith, B.; Kaufmann, T.J.; la Fougère, C.; Schmidt, N.O.; Tonn, J.C.; Vogelbaum, M.A.; Wen, P.Y.; Aldape, K.; et al. Imaging and diagnostic advances for intracranial meningiomas. Neuro-Oncol. 2019, 21 (Suppl. 1), i44–i61. [Google Scholar] [CrossRef]
- Smith-Bindman, R.; Kwan, M.L.; Marlow, E.C.; Theis, M.K.; Bolch, W.; Cheng, S.Y.; Bowles, E.J.A.; Duncan, J.R.; Greenlee, R.T.; Kushi, L.H.; et al. Trends in Use of Medical Imaging in US Health Care Systems and in Ontario, Canada, 2000–2016. JAMA 2019, 322, 843–856. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Wang, P.; Lan, J.; Hu, M.; Zheng, J.; Li, Y.; Hou, C.; Zhou, D. Wireless phone use and adult meningioma risk: A systematic review and Meta-analysis. Br. J. Neurosurg. 2021, 35, 444–450. [Google Scholar] [CrossRef]
- Uddin, M.; Dhanta, R.; Pitti, T.; Barsasella, D.; Scholl, J.; Jian, W.-S.; Li, Y.-C.; Hsu, M.-H.; Syed-Abdul, S. Incidence and Mortality of Malignant Brain Tumors after 20 Years of Mobile Use. Cancers 2023, 15, 3492. [Google Scholar] [CrossRef]
- Karipidis, K.; Baaken, D.; Loney, T.; Blettner, M.; Brzozek, C.; Elwood, M.; Narh, C.; Orsini, N.; Röösli, M.; Paulo, M.S.; et al. The effect of exposure to radiofrequency fields on cancer risk in the general and working population: A systematic review of human observational studies—Part I: Most researched outcomes. Environ. Int. 2024, 191, 108983. [Google Scholar] [CrossRef]
- Aydin, D.; Feychting, M.; Schüz, J.; Tynes, T.; Andersen, T.V.; Schmidt, L.S.; Poulsen, A.H.; Johansen, C.; Prochazka, M.; Lannering, B.; et al. Mobile phone use and brain tumors in children and adolescents: A multicenter case-control study. J. Natl. Cancer Inst. 2011, 103, 1264–1276. [Google Scholar] [CrossRef]
- Schönborn, F.; Burkhardt, M.; Kuster, N. Differences in energy absorption between heads of adults and children in the near field of sources. Health Phys. 1998, 74, 160–168. [Google Scholar] [CrossRef]
- Lee, A.K.; Hong, S.E.; Kwon, J.H.; Choi, H.D.; Cardis, E. Mobile phone types and SAR characteristics of the human brain. Phys. Med. Biol. 2017, 62, 2741–2761. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.K.; Hong, S.E.; Kwon, J.H.; Choi, H.D. SAR Comparison of SAM Phantom and Anatomical Head Models for a Typical Bar-Type Phone Model. IEEE Trans. Electromagn. Compat. 2015, 57, 1281–1284. [Google Scholar] [CrossRef]
- Wake, K.; Arima, T.; Watanabe, S.; Taki, M. SAR distributions in a child head phantom in the vicinity of recent mobile phones. In Proceedings of the 2011 XXXth URSI General Assembly and Scientific Symposium, Istanbul, Turkey, 13–20 August 2011; pp. 1–4. [Google Scholar] [CrossRef]
- Li, N.; Mo, Y.; Huang, C.; Han, K.; He, M.; Wang, X.; Wen, J.; Yang, S.; Wu, H.; Dong, F.; et al. A Clinical Semantic and Radiomics Nomogram for Predicting Brain Invasion in WHO Grade II Meningioma Based on Tumor and Tumor-to-Brain Interface Features. Front. Oncol. 2021, 11, 752158. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, L.; Muscat, J.E. Trends in Malignant and Benign Brain Tumor Incidence and Mobile Phone Use in the U.S. (2000–2021): A SEER-Based Study. Int. J. Environ. Res. Public Health 2025, 22, 933. https://doi.org/10.3390/ijerph22060933
Zhang L, Muscat JE. Trends in Malignant and Benign Brain Tumor Incidence and Mobile Phone Use in the U.S. (2000–2021): A SEER-Based Study. International Journal of Environmental Research and Public Health. 2025; 22(6):933. https://doi.org/10.3390/ijerph22060933
Chicago/Turabian StyleZhang, Li, and Joshua E. Muscat. 2025. "Trends in Malignant and Benign Brain Tumor Incidence and Mobile Phone Use in the U.S. (2000–2021): A SEER-Based Study" International Journal of Environmental Research and Public Health 22, no. 6: 933. https://doi.org/10.3390/ijerph22060933
APA StyleZhang, L., & Muscat, J. E. (2025). Trends in Malignant and Benign Brain Tumor Incidence and Mobile Phone Use in the U.S. (2000–2021): A SEER-Based Study. International Journal of Environmental Research and Public Health, 22(6), 933. https://doi.org/10.3390/ijerph22060933





