Knowledge, Attitude, and Practice Towards Antibiotic Use and Resistance Among Non-Medical University Students, Riyadh, Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Consideration
2.2. Study Design and Settings
Inclusion/Exclusion Criteria
2.3. Sample Size
2.3.1. Sample Technique
2.3.2. Data Collection Instrument
2.3.3. Quality Assurance
2.3.4. Data Presentation and Analysis
3. Results
3.1. Demographic Characteristics:
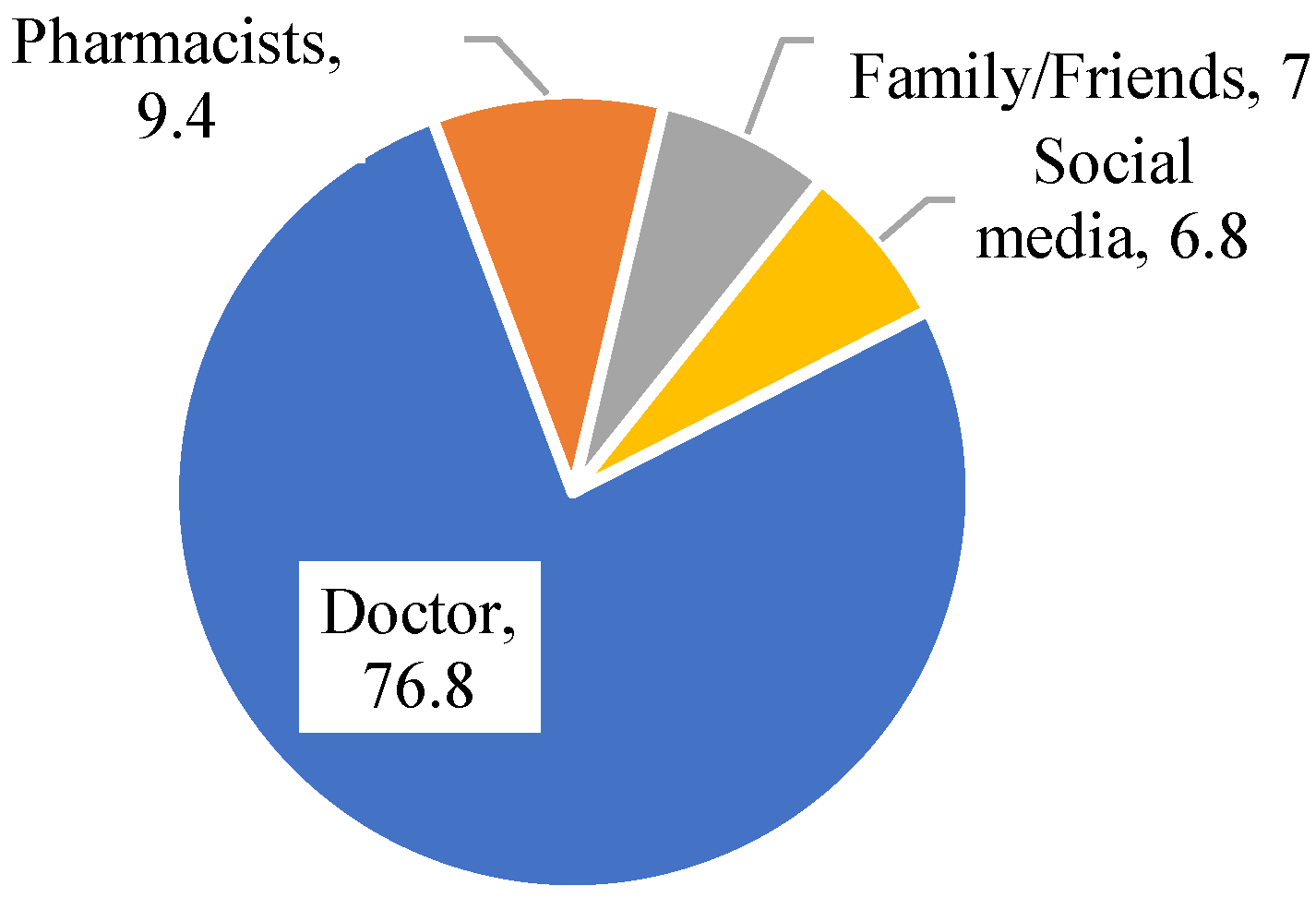
3.2. Knowledge, Attitude, and Practice of Antibiotic Resistance
4. Discussion
4.1. Strength
4.2. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al Shuhoumi, M.A.; Ghafri, S.A.; Hameed, F.J.; Hinai, A.A.; Ghafri, A.A.; Mony, S.R.; Sawafi, B.A.; Govindaraj, G.; Yaqoobi, A.A.; Alawi, B.A.J.M.R. Burden of Multidrug-Resistant Organisms in Oman: A Six-Year Study Calling for Urgent Actions. Microbiol. Res. 2025, 16, 45. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). How Antibiotic Resistance Happens. 2022. Available online: https://www.cdc.gov/antibiotic-use/media/pdfs/how_antibiotic_resistance_happens_508.pdf (accessed on 10 July 2024).
- Fahrenkamp-Uppenbrink, J.J.S. Countering antibiotic resistance. Science 2015, 347, 1109–1111. [Google Scholar] [CrossRef]
- The Lancet. Antimicrobial resistance: An agenda for all. Lancet 2024, 403, 2349. [Google Scholar] [CrossRef]
- Naghavi, M.; Vollset, S.E.; Ikuta, K.S.; Swetschinski, L.R.; Gray, A.P.; Wool, E.E.; Aguilar, G.R.; Mestrovic, T.; Smith, G.; Han, C. Global burden of bacterial antimicrobial resistance 1990–2021: A systematic analysis with forecasts to 2050. Lancet 2024, 404, 1199–1226. [Google Scholar] [CrossRef] [PubMed]
- Ahmadini, H. Antimicrobial resistance in Saudi Arabia: A review for immediate action and solution. Int. J. Med. Dev. Ctries. 2020, 4, 1703–1708. [Google Scholar] [CrossRef]
- Alomi, Y.A. National antimicrobial stewardship program in Saudi Arabia; initiative and the future. Open Access J. Surg. 2017, 4, 1–7. [Google Scholar] [CrossRef]
- Alzahrani, K.O.; Alshahrani, S.M.; Alajel, S.M. Evaluating the effectiveness of the Ministry of Health restriction policy on seasonal antibiotic consumption trends in Saudi Arabia, 2016–2020. Front. Pharmacol. 2023, 14, 1242087. [Google Scholar] [CrossRef]
- MOH. Kingdom Saudi Arabia National Action Plan on Combating Antimicrobial Resistance; Ministry of Health: Riyadh, Saudi Arabia, 2017. Available online: https://faolex.fao.org/docs/pdf/sau171813.pdf (accessed on 10 April 2024).
- Shibl, A.M.; Memish, Z.A.; Kambal, A.M.; Ohaly, Y.A.; Ishaq, A.; Senok, A.C.; Livermore, D.M. National surveillance of antimicrobial resistance among Gram-positive bacteria in Saudi Arabia. J. Chemother. 2014, 26, 13–18. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Moving WHO Guidance on Antibiotics into the Heart of Clinical Practice. 2024. Available online: https://www.who.int/news/item/09-12-2022-moving-who-guidance-on-antibiotics-into-the-heart-of-clinical-practice (accessed on 10 December 2023).
- Al-Shibani, N.; Hamed, A.; Labban, N.; Al-Kattan, R.; Al-Otaibi, H.; Alfadda, S. Knowledge, attitude and practice of antibiotic use and misuse among adults in Riyadh, Saudi Arabia. Saudi Med. J. 2017, 38, 1038–1044. [Google Scholar] [CrossRef]
- Alnasser, A.H.A.; Al-Tawfiq, J.A.; Ahmed, H.A.A.; Alqithami, S.M.H.; Alhaddad, Z.M.A.; Rabiah, A.S.M.; Albrahim, M.A.A.; Al Kalif, M.S.H.; Barry, M.; Temsah, M.H.; et al. Public knowledge, attitude and practice towards antibiotics use and antimicrobial resistance in Saudi Arabia: A web-based cross-sectional survey. J. Public Health Res. 2021, 10, 2276. [Google Scholar] [CrossRef]
- Mostafa, A.; Abdelzaher, A.; Rashed, S.; AlKhawaga, S.I.; Afifi, S.K.; AbdelAlim, S.; Mostafa, S.A.; Zidan, T.A. Is health literacy associated with antibiotic use, knowledge and awareness of antimicrobial resistance among non-medical university students in Egypt? A cross-sectional study. BMJ Open 2021, 11, e046453. [Google Scholar] [CrossRef] [PubMed]
- McNulty, C.A.; Collin, S.M.; Cooper, E.; Lecky, D.M.; Butler, C.C.J.B.o. Public understanding and use of antibiotics in England: Findings from a household survey in 2017. BMJ Open 2019, 9, e030845. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Licata, F.; Zucco, R.; Papadopoli, R.; Pavia, M. Knowledge and practices regarding antibiotics use: Findings from a cross-sectional survey among Italian adults. Evol. Med. Public Health 2020, 2020, 129–138. [Google Scholar] [CrossRef]
- Sullman, M.J.; Lajunen, T.J.; Baddal, B.; Apostolou, M.J.A. Antibiotics knowledge, attitudes and behaviours among the population living in Cyprus. Antibiotics 2023, 12, 897. [Google Scholar] [CrossRef]
- Ajulo, S.; Awosile, B. Global antimicrobial resistance and use surveillance system (GLASS 2022): Investigating the relationship between antimicrobial resistance and antimicrobial consumption data across the participating countries. PLoS ONE 2024, 19, e0297921. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Antibiotic Resistance. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed on 10 November 2023).
- Aykaç, A.; Tuncay, B.; Şehirli, A.Ö. Assessments of Students’ Numeracy Knowledge Levels in Health Literacy and Their Knowledge, Attitude, and Behavior Regarding Antibiotic Use. Middle Black Sea J. Health Sci. 2020, 9, 572–590. [Google Scholar] [CrossRef]
- Mudenda, S.; Chisha, P.; Chabalenge, B.; Daka, V.; Mfune, R.L.; Kasanga, M.; Kampamba, M.; Skosana, P.; Nsofu, E.; Hangoma, J. Antimicrobial stewardship: Knowledge, attitudes and practices regarding antimicrobial use and resistance among non-healthcare students at the University of Zambia. JAC Antimicrob. Resist. 2023, 5, dlad116. [Google Scholar] [CrossRef]
- Ortega-Paredes, D.; Larrea-Álvarez, C.M.; Torres-Elizalde, L.; de Janon, S.; Vinueza-Burgos, C.; Hidalgo-Arellano, L.; Šefcová, M.A.; Molina-Cuasapaz, G.; Fernandez-Moreira, E.; Larrea-Álvarez, M. Antibiotic resistance awareness among undergraduate students in Quito, Ecuador. Antibiotics 2022, 11, 197. [Google Scholar] [CrossRef]
- Precha, N.; Sukmai, S.; Hengbaru, M.; Chekoh, M.; Laohaprapanon, S.; Makkaew, P.; Dom, N.C. Knowledge, attitudes, and practices regarding antibiotic use and resistance among health science and non-health science university students in Thailand. PLoS ONE 2024, 19, e0296822. [Google Scholar] [CrossRef]
- Shah, P.; Shrestha, R.; Mao, Z.; Chen, Y.; Chen, Y.; Koju, P.; Liu, X.; Li, H. Knowledge, attitude, and practice associated with antibiotic use among university students: A survey in Nepal. Int. J. Environ. Res. Public Health 2019, 16, 3996. [Google Scholar] [CrossRef]
- Suaifan, G.; Shehadeh, M.; Darwish, D.A.; Al-Ijel, H.; Yousef, A.; Darwish, R.M. A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. Afr. J. Pharm. Pharmacol. 2012, 6, 763–770. [Google Scholar] [CrossRef]
- Sunusi, L.S.A.; Awad, M.M.; Hassan, N.M.; Isa, C.A. Assessment of knowledge and attitude toward antibiotic use and resistance among students of International University of Africa, medical complex, Sudan. Glob. Drugs Ther. 2019, 4, 1–6. [Google Scholar] [CrossRef]
- Tiong, T.W.; Chua, S.S. Knowledge and attitude of university students on antibiotics: A cross-sectional study in Malaysia. Drug Healthc. Patient Saf. 2020, 12, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Marzan, M.; Islam, D.Z.; Lugova, H.; Krishnapillai, A.; Haque, M.; Islam, S. Knowledge, attitudes, and practices of antimicrobial uses and resistance among public university students in Bangladesh. Infect. Drug Resist. 2021, 14, 519–533. [Google Scholar] [CrossRef]
- Shahpawee, N.S.; Chaw, L.L.; Muharram, S.H.; Goh, H.P.; Hussain, Z.; Ming, L.C.J.A. University students’ antibiotic use and knowledge of antimicrobial resistance: What are the common myths? Antibiotics 2020, 9, 349. [Google Scholar] [CrossRef]
- Sharma, G.; Paudel, S.; Chalise, A.; Sapkota, B.; Marasine, N.R. Knowledge, Attitude, and Practice on Antibiotic Use and Resistance Among Undergraduates, Pokhara Metropolitan, Nepal. BioMed Res. Int. 2025, 2025, 9928264. [Google Scholar] [CrossRef]
- Prigitano, A.; Romanò, L.; Auxilia, F.; Castaldi, S.; Tortorano, A.M. Antibiotic resistance: Italian awareness survey 2016. J. Infect. Public Health 2018, 11, 30–34. [Google Scholar] [CrossRef]
- General Authority for Statistics. Population Estimates by Gender and Region. 2019. Available online: https://database.stats.gov.sa/home/indicator/410 (accessed on 10 July 2024).
- Raosoft, Inc. Raosoft Sample Size Calculator; Raosoft, Inc.: Seattle, WA, USA, 2004. [Google Scholar]
- Huang, Y.; Gu, J.; Zhang, M.; Ren, Z.; Yang, W.; Chen, Y.; Fu, Y.; Chen, X.; Cals, J.W.; Zhang, F. Knowledge, attitude and practice of antibiotics: A questionnaire study among 2500 Chinese students. BMC Med. Educ. 2013, 13, 163. [Google Scholar] [CrossRef]
- Jairoun, A.; Hassan, N.; Ali, A.; Jairoun, O.; Shahwan, M. Knowledge, attitude and practice of antibiotic use among university students: A cross sectional study in UAE. BMC Public Health 2019, 19, 1–8. [Google Scholar] [CrossRef]
- Lajunen, T.J.; Sullman, M.J.; Baddal, B.; Tekeş, B.; Apostolou, M.J.A. Antibiotics knowledge, attitudes and behaviours among the population living in Greece and Turkey. Antibiotics 2023, 12, 1279. [Google Scholar] [CrossRef]
- Horvat, O.; Tomas, A.; Paut Kusturica, M.; Bukumiric, D.; Blagojevic, B.; Kovacevic, Z. Serbian students’ knowledge, attitudes and behaviour towards antibiotic use: Is there room for improvement? Int. J. Public Health 2020, 65, 1257–1267. [Google Scholar] [CrossRef]
- WHO. Antibiotic Resistance: Multi-Country Public Awareness Survey; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Abolfotouh, M.A.; Al-Assiri, M.H.; Al-Omani, M.; Al Johar, A.; Al Hakbani, A.; Alaskar, A.S. Public awareness of blood donation in Central Saudi Arabia. Int. J. Gen. Med. 2014, 7, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Pogurschi, E.N.; Petcu, C.D.; Mizeranschi, A.E.; Zugravu, C.A.; Cirnatu, D.; Pet, I.; Ghimpețeanu, O.-M. Knowledge, attitudes and practices regarding antibiotic use and antibiotic resistance: A latent class analysis of a Romanian population. Int. J. Environ. Res. Public Health 2022, 19, 7263. [Google Scholar] [CrossRef] [PubMed]
- MOH. Ministry of Health Warns Against Selling Antibiotics Without Prescription; Ministry of Health: Riyadh, Saudi Arabia, 2018. Available online: https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/news2018-04-17-004.aspx (accessed on 10 May 2024).
- Ahmed, S.K.; Hussein, S.; Qurbani, K.; Ibrahim, R.H.; Fareeq, A.; Mahmood, K.A.; Mohamed, M.G. Antimicrobial resistance: Impacts, challenges, and future prospects. J. Med. Surg. Public Health 2024, 2, 100081. [Google Scholar] [CrossRef]
- Mohsen, S.; Dickinson, J.A.; Somayaji, R. Update on the adverse effects of antimicrobial therapies in community practice. Can. Fam. Physician 2020, 66, 651–659. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). 2019 Antibiotic Resistance Threats Report. 2024. Available online: https://www.cdc.gov/antimicrobial-resistance/data-research/threats/index.html (accessed on 10 July 2024).
- Alkhuraisi, L.S.; Mirghani, H.; Al Qahtani, M.M.; Alrezqi, W.A.; Alfaifi, I.A.; Jathmi, A.S.; Jathmi, A.S.; Aianazi, N.S.; Al Qahtani, M.M., Sr.; AlAnazi, N.S. Knowledge, Attitude, and Practice of Antibiotic Resistance Among General Population in Saudi Arabia: A Cross-Sectional Study. Cureus 2023, 15, 51053. [Google Scholar] [CrossRef]
- Alshehri, A.A.; Khawagi, W.Y. Knowledge, Awareness, and Perceptions Towards Antibiotic Use, Resistance, and Antimicrobial Stewardship Among Final-Year Medical and Pharmacy Students in Saudi Arabia. Antibiotics 2025, 14, 116. [Google Scholar] [CrossRef]
- Bdair, I.A.; Bdair, O.A.; Maribbay, G.M.; Elzehiri, D.; Hassan, E.S.; Tolentino, A.D.; Emara, M.M.; Ali, E.K.; Abdelmeged, R.M.; Fadul, M.O. Public awareness towards antibiotics use, misuse and resistance in Saudi community: A cross-sectional population survey. J. Appl. Pharm. Sci. 2024, 14, 217–226. [Google Scholar] [CrossRef]
- Nukaly, H.Y.; Aljuhani, R.A.; Alhartani, M.M.; Alhindi, Y.Z.; Asif, U.; Alshanberi, A.M.; Alsanosi, S.M. Knowledge of antibiotic use and resistance among medical students in Saudi Arabia. Adv. Med. Educ. 2024, 15, 501–512. [Google Scholar] [CrossRef]
- Zaidi, S.F.; Alotaibi, R.; Nagro, A.; Alsalmi, M.; Almansouri, H.; Khan, M.A.; Khan, A.; Memon, I. Knowledge and attitude towards antibiotic usage: A questionnaire-based survey among pre-professional students at King Saud bin Abdulaziz University for health sciences on Jeddah Campus, Saudi Arabia. Pharmacy 2020, 8, 5. [Google Scholar] [CrossRef]
- Anderson, A. Online health information and public knowledge, attitudes, and behaviours regarding antibiotics in the UK: Multiple regression analysis of Wellcome Monitor and Eurobarometer Data. PLoS ONE 2018, 13, e0204878. [Google Scholar] [CrossRef] [PubMed]
- Licata, F.; Angelillo, S.; Oliverio, A.; Bianco, A. The internet: Friend or foe of antibiotic resistance? Results of a cross-sectional study among Italian university students. Antibiotics 2021, 10, 1091. [Google Scholar] [CrossRef] [PubMed]
| Variable | Categories | No. | % |
|---|---|---|---|
| Age groups (years) | 17–18 | 140 | 20.8 |
| 19–20 | 247 | 36.8 | |
| 21–22 | 202 | 30.1 | |
| 23–24 | 83 | 12.4 | |
| Gender | Male | 269 | 40.0 |
| Female | 403 | 60.0 | |
| Nationality | Saudi | 635 | 94.5 |
| Non-Saudi | 37 | 5.5 | |
| University | IMSU | 363 | 54.0 |
| KSU | 181 | 26.9 | |
| PNAU | 84 | 12.5 | |
| PSU | 11 | 1.6 | |
| AFU | 21 | 3.1 | |
| AYU | 12 | 1.8 | |
| Field of study | Business | 229 | 34.1 |
| Literary | 206 | 30.7 | |
| Engineering | 93 | 13.8 | |
| Computer science | 81 | 12.1 | |
| Sciences | 63 | 9.4 | |
| Marital status | Married | 27 | 4.0 |
| Non-married | 645 | 96.0 |
| Total Knowledge | No. | % |
|---|---|---|
| Insufficient knowledge | 275 | 40.9 |
| Sufficient knowledge | 397 | 59.1 |
| Negative attitude | 269 | 40.0 |
| Positive attitude | 403 | 60.0 |
| Inappropriate practice | 265 | 39.4 |
| Appropriate practice | 407 | 60.6 |
| Variable | Categories | Sufficient Knowledge | Sufficient Attitude | Sufficient Practices | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | p Value | No. | % | p Value | No. | % | p Value | ||
| Age | 17–18 years | 88 | 62.9 | 0.109 | 92 | 65.7 | 0.003 | 94 | 67.1 | 0.005 |
| 19–20 years | 148 | 59.9 | 147 | 59.5 | 146 | 59.1 | ||||
| 21–22 years | 122 | 60.4 | 129 | 63.9 | 130 | 64.4 | ||||
| 23–24 years | 39 | 47.0 | 35 | 42.2 | 37 | 44.6 | ||||
| Gender | Male | 153 | 56.9 | 0.343 | 144 | 53.5 | 0.005 | 152 | 56.5 | 0.079 |
| Female | 244 | 60.5 | 259 | 64.3 | 255 | 63.3 | ||||
| Nationality | Saudi | 372 | 58.6 | 0.280 | 380 | 59.8 | 0.780 | 384 | 60.5 | 0.838 |
| Non-Saudi | 25 | 67.6 | 23 | 62.2 | 23 | 62.2 | ||||
| University | IMSU | 200 | 55.1 | 0.300 | 205 | 56.5 | 0.220 | 209 | 57.6 | 0.150 |
| KSU | 118 | 65.2 | 120 | 66.3 | 121 | 66.9 | ||||
| PNAU | 50 | 59.5 | 54 | 64.3 | 51 | 60.7 | ||||
| PSU | 7 | 63.6 | 5 | 45.5 | 4 | 36.4 | ||||
| AFU | 14 | 66.7 | 13 | 61.9 | 15 | 71.4 | ||||
| AYU | 8 | 66.7 | 6 | 50.0 | 7 | 58.3 | ||||
| Field of study | Business | 136 | 59.4 | 0.003 | 151 | 65.9 | 0.004 | 147 | 64.2 | <0.001 |
| Literary | 101 | 49.0 | 106 | 51.5 | 99 | 48.1 | ||||
| Engineering | 65 | 69.9 | 66 | 71.0 | 71 | 76.3 | ||||
| Computer sc | 52 | 64.2 | 45 | 55.6 | 50 | 61.7 | ||||
| Sciences | 43 | 68.3 | 35 | 55.6 | 40 | 63.5 | ||||
| Variable | Categories | Knowledge | Attitude | Practices | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% C. I | p-Value | OR | 95% C. I | p-Value | OR | 95% C. I | p-Value | ||
| Age | 17–18 years | R | - | - | R | - | - | R | - | - |
| 19–20 years | 0.992 | 0.633–1.554 | 0.971 | 0.792 | 0.501–1.251 | 0.317 | 0.740 | 0.466–1.175 | 0.201 | |
| 21–22 years | 0.962 | 0.588–1.573 | 0.877 | 0.855 | 0.517– 1.414 | 0.543 | 0.819 | 0.493–1.361 | 0.441 | |
| 23–24 years | 0.590 | 0.331–1.054 | 0.075 | 0.410 | 0.227–0.741 | 0.003 | .416 | 0.229–0.755 | 0.004 | |
| Gender | Male | R | - | - | R | - | - | R | - | - |
| Female | 1.281 | 0.909–1.806 | 0.157 | 1.658 | 1.170–2.350 | 0.004 | 1.520 | 1.070–2.160 | 0.019 | |
| Nationality | Saudi | 0.772 | 0.346–1.725 | 0.528 | 0.651 | 0.291–1.456 | 0.296 | 0.975 | 0.437–2.172 | 0.950 |
| Non-Saudi | R | - | - | R | - | - | R | - | - | |
| University | IMSU | 0.957 | 0.258–3.549 | 0.947 | 1.839 | 0.508–6.662 | 0.354 | 1.550 | 0.422–5.700 | 0.509 |
| KSU | 1.132 | 0.304–4.209 | 0.853 | 2.722 | 0.751–9.872 | 0.128 | 1.741 | 0.473–6.407 | 0.404 | |
| PNAU | 0.770 | 0.197–3.020 | 0.708 | 1.751 | 0.457–6.704 | 0.413 | 0.993 | 0.255–3.870 | 0.992 | |
| PSU | 0.953 | 0.159–5.711 | 0.958 | .801 | 0.140–4.595 | 0.803 | 0.337 | 0.056–2.032 | 0.235 | |
| AFU | 0.845 | 0.180–3.962 | 0.831 | 1.462 | 0.324–6.596 | 0.621 | 1.588 | 0.334–7.553 | 0.561 | |
| AYU | R | - | - | R | - | - | R | - | - | |
| Field of study | Business | 0.749 | .393–1.428 | 0.380 | 1.988 | 1.053–3.753 | 0.034 | 1.124 | 0.591–2.134 | 0.722 |
| Literary | 0.478 | 0.252–0.908 | 0.024 | 0.996 | .533–1.862 | 0.990 | 0.543 | 0.287–1.025 | 0.059 | |
| Engineering | 1.166 | 0.574–2.369 | 0.672 | 2.265 | 1.127–4.552 | 0.022 | 2.243 | 1.082–4.651 | 0.030 | |
| Computer sc | 0.886 | 0.435–1.804 | 0.738 | 1.158 | 0.582–2.304 | 0.677 | 1.053 | 0.521–2.126 | 0.886 | |
| Sciences | R | - | - | R | - | - | R | - | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bawazir, A.; Bohairi, A.; Badughaysh, O.; Alhussain, A.; Abuobaid, M.; Abuobaid, M.; Al Jabber, A.; Mardini, Y.; Alothman, A.; Alsomih, F.; et al. Knowledge, Attitude, and Practice Towards Antibiotic Use and Resistance Among Non-Medical University Students, Riyadh, Saudi Arabia. Int. J. Environ. Res. Public Health 2025, 22, 868. https://doi.org/10.3390/ijerph22060868
Bawazir A, Bohairi A, Badughaysh O, Alhussain A, Abuobaid M, Abuobaid M, Al Jabber A, Mardini Y, Alothman A, Alsomih F, et al. Knowledge, Attitude, and Practice Towards Antibiotic Use and Resistance Among Non-Medical University Students, Riyadh, Saudi Arabia. International Journal of Environmental Research and Public Health. 2025; 22(6):868. https://doi.org/10.3390/ijerph22060868
Chicago/Turabian StyleBawazir, Amen, Abdullah Bohairi, Omar Badughaysh, Abdulmohsen Alhussain, Mohannad Abuobaid, Majd Abuobaid, Azzam Al Jabber, Yaman Mardini, Abdulaziz Alothman, Faris Alsomih, and et al. 2025. "Knowledge, Attitude, and Practice Towards Antibiotic Use and Resistance Among Non-Medical University Students, Riyadh, Saudi Arabia" International Journal of Environmental Research and Public Health 22, no. 6: 868. https://doi.org/10.3390/ijerph22060868
APA StyleBawazir, A., Bohairi, A., Badughaysh, O., Alhussain, A., Abuobaid, M., Abuobaid, M., Al Jabber, A., Mardini, Y., Alothman, A., Alsomih, F., AlMuzaini, A., & BaHamdan, M. (2025). Knowledge, Attitude, and Practice Towards Antibiotic Use and Resistance Among Non-Medical University Students, Riyadh, Saudi Arabia. International Journal of Environmental Research and Public Health, 22(6), 868. https://doi.org/10.3390/ijerph22060868






