Systematic Intervention with Formal Caregivers to Promote Nutritional Health of Older People with Dementia: An Impact Evaluation Study
Abstract
:1. Introduction
2. Materials and Methods
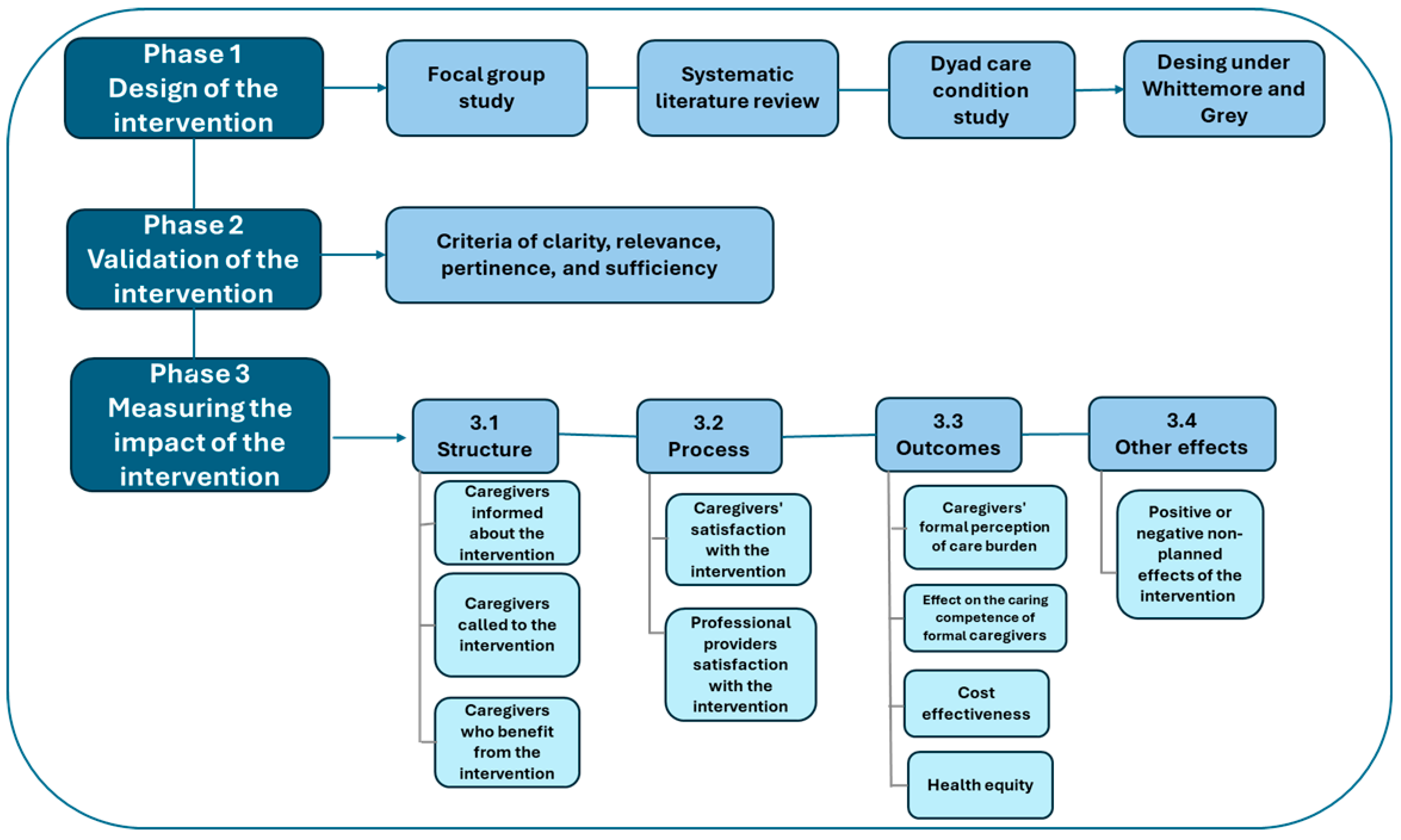
2.1. Phase 1: Intervention Design
2.2. Phase 2: Intervention Validation
2.3. Phase 3: Impact Measurement
3. Results
3.1. Intervention Design
3.2. Impact Measurement
3.3. Unexpected Effects of the Intervention
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Aging and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 2 January 2025).
- Sierra, F. Geroscience and the challenges of aging societies. Aging Med. 2019, 2, 132. [Google Scholar] [CrossRef] [PubMed]
- Phelan, A.; Ayalon, L. The intersection of ageism and elder abuse. In Advances in Elder Abuse Research: Practice, Legislation, and Policy; Springer: Berlin, Germany, 2020; pp. 11–22. [Google Scholar] [CrossRef]
- Vaupel, J.W.; Villavicencio, F.; Bergeron-Boucher, M.P. Demographic perspectives on the rise of longevity. Proc. Natl. Acad. Sci. USA 2021, 118, e2019536118. [Google Scholar] [CrossRef] [PubMed]
- Hakim, M. Dementia: Guide to diagnosis and management. Bangladesh J. Med. 2023, 35, 138–139. [Google Scholar] [CrossRef]
- Cahill, S. WHO’s global action plan on the public health response to dementia: Some challenges and opportunities. Aging Ment. Health 2020, 24, 197–199. [Google Scholar] [CrossRef]
- Cao, X.P.; Xu, W.; Wang, Z.T.; Tan, L.; Yu, J.T. Dietary Components and Nutritional Strategies for Dementia Prevention in the Elderly. Curr. Alzheimer Res. 2023, 20, 224–243. [Google Scholar] [CrossRef]
- Wu, Y.T.; Beiser, A.S.; Breteler, M.M.; Fratiglioni, L.; Helmer, C.; Hendrie, H.C.; Honda, H.; Ikram, M.A.; Langa, K.M.; Lobo, A.; et al. The changing prevalence and incidence of dementia over time—Current evidence. Nat. Rev. Neurol. 2017, 13, 327–339. [Google Scholar] [CrossRef]
- Arifin, H.; Chen, R.; Banda, K.J.; Kustanti, C.Y.; Chang, C.Y.; Lin, H.C.; Liu, D.; Lee, T.Y.; Chou, K.R. Meta-analysis and moderator analysis of the prevalence of malnutrition and malnutrition risk among older adults with dementia. Int. J. Nurs. Stud. 2024, 150, 104648. [Google Scholar] [CrossRef]
- Murphy, J.L. Improving nutrition and hydration in older people with dementia in care homes. Nurs. Older People 2022, 34, 35–42. [Google Scholar] [CrossRef]
- Kauzor, K.; Drewel, M.; Gonzalez, H.; Rattinger, G.B.; Hammond, A.G.; Wengreen, H.; Lyketsos, C.G.; Tschanz, J.T. Malnutrition, and neuropsychiatric symptoms in dementia: The Cache County dementia progression study. Int. Psychogeriatr. 2023, 35, 653–663. [Google Scholar] [CrossRef]
- Volkert, D. Nutrition and Dementia-Dementia and Nutrition. Ther. Umschau. Rev. Ther. 2023, 80, 217–225. [Google Scholar] [CrossRef]
- Passos, L.; Tavares, J.; Batchelor, M.; Figueiredo, D. Interventions to address mealtime support needs in dementia: A scoping review. PLoS ONE 2024, 19, e0300987. [Google Scholar] [CrossRef] [PubMed]
- Labyak, C.; Sealey-Potts, C.; Wright, L.; Kriek, C.; Dilts, S. Informal caregiver and healthcare professional perspectives on dementia and nutrition. J. Hum. Nutr. Diet. 2024, 37, 1308–1319. [Google Scholar] [CrossRef]
- Sharma, S.; Halim, N.A.A.; Maniam, P. Caregiver experiences with dementia-related feeding/eating difficulties. Healthcare 2024, 12, 133. [Google Scholar] [CrossRef] [PubMed]
- Vicente de Sousa, O.; Mendes, J.; Amaral, T.F. Association between nutritional and functional status indicators with caregivers’ burden in Alzheimer’s disease. Nutr. Diet. 2022, 79, 380–389. [Google Scholar] [CrossRef]
- Gilsenan, J.; Gorman, C.; Shevlin, M. Explaining caregiver burden in a large sample of UK dementia caregivers: The role of contextual factors, behavioural problems, psychological resilience, and anticipatory grief. Aging Ment. Health 2023, 27, 1274–1281. [Google Scholar] [CrossRef]
- Whittemore, R.; Grey, M. The systematic development of nursing interventions. J. Nurs. Scholarsh. 2002, 34, 115–120. [Google Scholar] [CrossRef]
- Tristán-López, A. Modificación al modelo de Lawshe para el dictamen cuantitativo de la validez de contenido de un instrumento objetivo. Av. Medición 2008, 6, 37–48. [Google Scholar]
- Tanahashi, T. Health service coverage and its evaluation. Bull. World Health Organ. 1978, 56, 295. [Google Scholar] [PubMed] [PubMed Central]
- Nundy, S.; Cooper, L.A.; Mate, K.S. The quintuple aim for health care improvement: A new imperative to advance health equity. JAMA 2022, 327, 521–522. [Google Scholar] [CrossRef]
- Gould, K.A. Equity: Introducing the quintuple aim. Dimens. Crit. Care Nurs. 2022, 41, 119–120. [Google Scholar] [CrossRef]
- Libera Bonilla, B.E. Impacto, impacto social y evaluación del impacto. Acimed 2007, 15. Available online: http://scielo.sld.cu/scielo.php?pid=S1024-94352007000300008&script=sci_abstract (accessed on 18 January 2025).
- Borrell, C.; Ru, M.; Pasar n, M.I.; Benach, J.; Kunst, A. La medición de las desigualdades en salud. Gac. Sanit. 2000, 14 (Suppl. S3), 20–33. [Google Scholar]
- Chaparro Díaz, L.; Sánchez Herrera, B.; González, G.M. Encuesta de caracterización del cuidado de la diada cuidador familiar-persona con enfermedad crónica. Rev. Cienc. Cuid. 2014, 11, 31–45. [Google Scholar]
- Carrillo González, G.M.; Sánchez Herrara, B.; Vargas, E. Desarrollo y pruebas psicométricas del Instrumento” cuidar”-versión corta para medir la competencia de cuidado en el hogar. Rev. Univ. Ind. Santander. Salud. 2016, 48, 222–231. [Google Scholar] [CrossRef]
- Wissema, J.G. Towards the Third-Generation University: Managing the University in Transition; Edward Elgar Publishing: Cheltenham, UK, 2009. [Google Scholar]
- Allen, A.P.; Buckley, M.M.; Cryan, J.F.; Ní Chorcoráin, A.; Dinan, T.G.; Kearney, P.M.; O’Caoimh, R.; Calnan, M.; Clarke, G.; Molloy, D.W. Informal caregiving for dementia patients: The contribution of patient characteristics and behaviours to caregiver burden. Age Ageing 2020, 49, 52–56. [Google Scholar] [CrossRef]
- Russell, J.; Fudge, N.; Greenhalgh, T. The impact of public involvement in health research: What are we measuring? Why are we measuring it? Should we stop measuring it? Res. Involv. Engagem. 2020, 6, 63. [Google Scholar] [CrossRef]
- Wójcik, D.; Szczechowiak, K.; Konopka, P.; Owczarek, M.; Kuzia, A.; Rydlewska-Liszkowska, I.; Pikala, M. Informal dementia caregivers: Current technology use and acceptance of technology in care. Int. J. Environ. Res. Public Health 2021, 18, 3167. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446, Erratum in Lancet 2023, 402, 10408. [Google Scholar] [CrossRef] [PubMed]
- D’avolio, D.; Gropper, S.S.; Appelbaum, M.; Thiengtham, S.; Holt, J.; Newman, D. The impact of a pilot telehealth coaching intervention to improve caregiver stress and well-being and to increase dietary protein intake of caregivers and their family members with dementia–Interrupted by COVID-19. Dementia 2023, 22, 1241–1258. [Google Scholar] [CrossRef]
- Kul, B.; Tülek, Z. Optimal Care in the Management of Eating Difficulties in Patients with Dementia. Geriatr. Bilim. Derg. 2024, 7, 156–166. [Google Scholar] [CrossRef]
- Blake, D.; Berry, K.; Brown, L.J. A systematic review of the impact of person-centred care interventions on the behaviour of staff working in dementia care. J. Adv. Nurs. 2020, 76, 426–444. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Kim, S.; Alessio, H. Mealtime caregiving knowledge, attitudes, and behaviors for people living with dementia: A systematic review of psychometric properties of instruments. Int. J. Nurs. Stud. 2021, 114, 103824. [Google Scholar] [CrossRef] [PubMed]
- Faraday, J.; Abley, C.; Beyer, F.; Exley, C.; Moynihan, P.; Patterson, J.M. How do we provide good mealtime care for people with dementia living in care homes? A systematic review of carer–resident interactions. Dementia 2021, 20, 3006–3031. [Google Scholar] [CrossRef] [PubMed]
- Ball, L.; Jansen, S.; Desbrow, B.; Morgan, K.; Moyle, W.; Hughes, R. Nutrition support in dementia care. Nutr. Diet. 2015, 72, 22–29. [Google Scholar] [CrossRef]
- Mueller, A.; Thao, L.; Condon, O.; Liebzeit, D.; Fields, B. A systematic review of the needs of dementia caregivers across care settings. Home Health Care Manag. Pract. 2022, 34, 133–147. [Google Scholar] [CrossRef]
|
Type of Indicators | Purpose of Measurement | Applied Formula |
|---|---|---|
| Structure | Intervention coverage | [(Formal caregivers called/Formal caregivers needing the intervention) × 100] |
| Programmed service coverage | [(# of formal caregivers registered/Formal caregivers summoned to take part in the intervention) × 100] | |
| Acceptance of the intervention | [(# of Formal caregivers who attended the intervention/# of Formal caregivers registered in the intervention) × 100] | |
| Contact coverage | [(# of Formal caregivers who completed the intervention/# of Formal caregivers registered) × 100] | |
| Process | Satisfaction of formal caregivers with the intervention | Satisfaction perception % with the intervention’s novelty, usefulness, importance, approach to the topic, and overall experience, obtained in a survey |
| Satisfaction of professional providers with the intervention | Satisfaction perception % with the intervention’s novelty, usefulness, importance, approach to the topic, and overall experience, obtained in a survey | |
| Output | Effect on the formal caregiver’s perception of care burden | Difference in the means between the level of perception of burden of care before and after the intervention |
| Coverage effectiveness | The % of formal caregivers who received help from the program: [(# of formal caregivers who improved their caring competence after the intervention/# of formal caregivers who completed the intervention) × 100] | |
| Effect on the caring competence of formal caregivers | Difference in the means between the level of caring competence of formal caregivers, globally and by components, before and after the intervention | |
| Cost–benefit of the intervention | [Cost in US$ calculated by the institution for the conventional intervention-cost in US$ of the flexible intervention] | |
| Health equity | Detail verification of the inclusion of public and private institutions, with different socioeconomic and geographical conditions |
| Intervention Section | Section Description | ||
|---|---|---|---|
| General description | Name | Nurturing Neurons—Formal Caregivers | |
| Issue to resolve | Insufficient care competence in formal caregivers of elderly people with dementia, at risk of nutritional health impairment. | ||
| Addressed recipients | This intervention targets formal caregivers addressing the nutritional needs of institutionalized individuals aged 60+ with severe neurocognitive disorders that impact daily activities. | ||
| Modifiable aspects through the intervention | The modifiable aspects are those related to the improvement in the formal caregivers’ care competence related to nutrition and feeding of the cognitively impaired elderly in their care. These include each of the domains that make up the competence: the level of knowledge; the recognition of the unique conditions as a caregiver; how to make the therapeutic instructions on nutrition and feeding of the elderly operational; the identification and management of the welfare conditions available to support feeding and nutrition; the ability to anticipate and minimize risks associated with feeding and nutrition; and the identification and consolidation of a support network to care for aspects related to feeding and nutrition. | ||
| Appropriate conditions | The conditions for the development of the intervention include generating an environment of trust, presenting the content of the educational material and explaining it before using it, conducting feedback and re-teaching processes with the participants, and explicitly thanking them in each session for their attention and dedicated time. | ||
| Necessary resources | Professional staff with experience in the work of nutritional care of the elderly with cognitive impairment and their formal caregivers. Materials for education, ability reinforcement, and field exercises in various presentation modalities. Connectivity and availability of materials to achieve access through a mobile phone. | ||
| Intervention development | Processes for its development | The intervention uses tele-support. It includes six sessions in a total of fourteen hours, as follows: two hours for each of the six dimensions addressed (one hour of training and one hour of independent work), plus two hours for the induction and evaluation. The frequency of meetings is biweekly. | |
| Expected results | Proximal | Level of perception of satisfaction of the formal caregiver. Level of knowledge, uniqueness, instrumentation, provision of well-being conditions, anticipation, and ability to recognize and generate a support network to address feeding and nutrition. | |
| Primary | Level of caring competence of the formal caregiver to address feeding and nutrition. | ||
| Secondary | Feeding practices and levels of nutrition. | ||
| Distal | The design of a menu that considers different textures and ensures an adequate nutritional balance. Guidelines that serve as a basis for a public policy about the care of people with cognitive impairment and support for their formal caregivers. | ||
| Contents of the intervention | Phase 1: “Who we are” | Session 1 | Introduction to the intervention. Presentation of the participants to learn about their expectations and for them to propose joint goals for nutritional care for the older adults in their care. Presentation of the generalities of the intervention. Addresses the topics of uniqueness and provision of well-being conditions. |
| Session 2 | Reinforcement of the topics of uniqueness and provision of well-being conditions through individual and group independent work exercises. | ||
| Phase 2: “How we care” | Session 3 | Addresses the topics of knowledge and instrumentation. | |
| Session 4 | Reinforcement of the topics of knowledge and instrumentation through individual and group independent work exercises. | ||
| Phase 3: “Who we count on” | Session 5 | Addresses the topics of anticipation and support network. | |
| Session 6 | Reinforcement of the topics of anticipation and support network through individual and group independent work exercises. Final evaluation of the intervention, checking whether it met the established expectations and goals. | ||
| Type of Indicator | Name | Results | |
|---|---|---|---|
| Structure | Intervention coverage | 100% | |
| Programmed service coverage | 86.5% | ||
| Acceptability of the intervention | 86.8% | ||
| Contact coverage | 70.7% | ||
| Process | Satisfaction with the intervention | Formal caregivers | 94.9% |
| Professional providers | 92.5% | ||
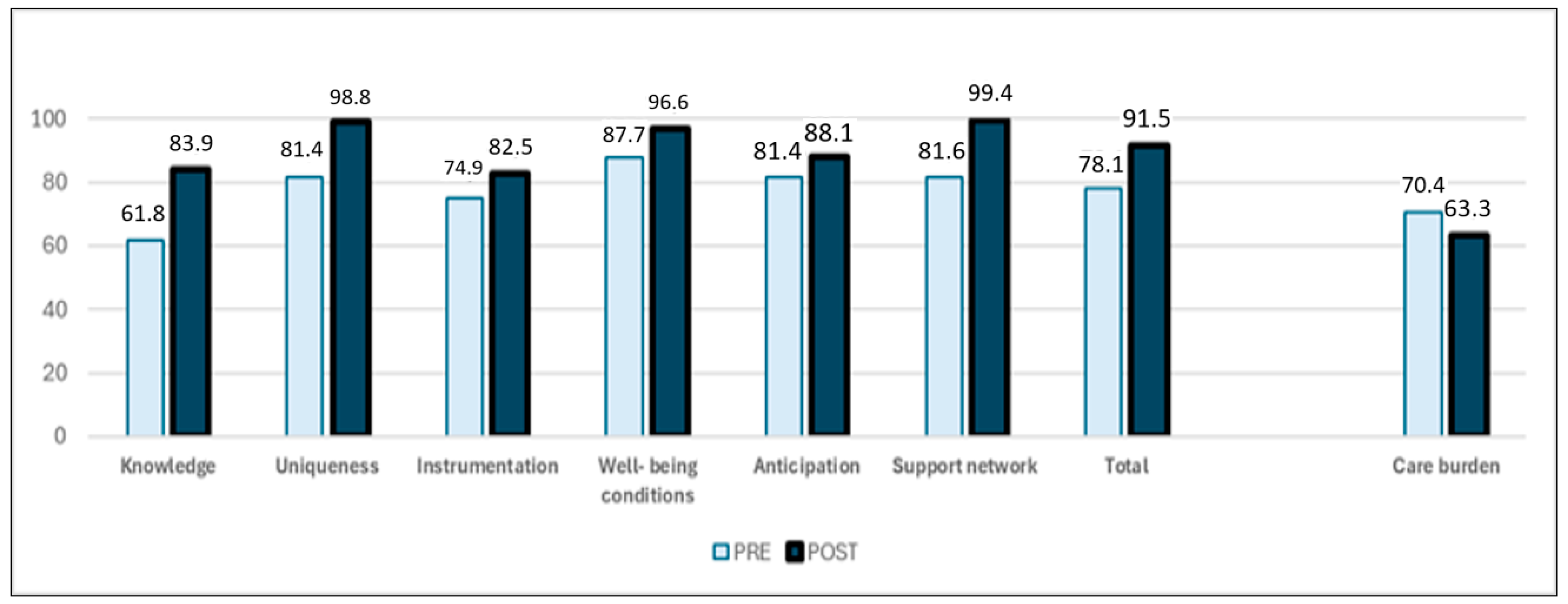
| Output | Effect on the formal caregiver’s perception of care burden | Burden of care perception diminished in 7.1% (p < 0.001) | |
| Coverage effectiveness | 100% | ||
| Effect on the care competence of formal caregivers | Global care competence—13.4% changing from the medium to high level (p < 0.001) | ||
| Cost–benefit of the intervention | Prior achievement of the purpose: Cost of the conventional modality: USD 36,099.91 Cost of the tele-support modality: USD 15,354.18 Savings: USD 20,276.90 (−56.2%) | ||
| Health equity | Participant institutions included different geographical areas, were both public and private, and had different socioeconomic levels | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarmiento-González, P.; Moreno-Fergusson, M.E.; Rojas-Rivera, A.; Cuadros-Mojica, J.A.; Ramírez-Pulido, B.; Sánchez-Herrera, B. Systematic Intervention with Formal Caregivers to Promote Nutritional Health of Older People with Dementia: An Impact Evaluation Study. Int. J. Environ. Res. Public Health 2025, 22, 849. https://doi.org/10.3390/ijerph22060849
Sarmiento-González P, Moreno-Fergusson ME, Rojas-Rivera A, Cuadros-Mojica JA, Ramírez-Pulido B, Sánchez-Herrera B. Systematic Intervention with Formal Caregivers to Promote Nutritional Health of Older People with Dementia: An Impact Evaluation Study. International Journal of Environmental Research and Public Health. 2025; 22(6):849. https://doi.org/10.3390/ijerph22060849
Chicago/Turabian StyleSarmiento-González, Paola, María Elisa Moreno-Fergusson, Alejandra Rojas-Rivera, Juan Alcides Cuadros-Mojica, Bibiana Ramírez-Pulido, and Beatriz Sánchez-Herrera. 2025. "Systematic Intervention with Formal Caregivers to Promote Nutritional Health of Older People with Dementia: An Impact Evaluation Study" International Journal of Environmental Research and Public Health 22, no. 6: 849. https://doi.org/10.3390/ijerph22060849
APA StyleSarmiento-González, P., Moreno-Fergusson, M. E., Rojas-Rivera, A., Cuadros-Mojica, J. A., Ramírez-Pulido, B., & Sánchez-Herrera, B. (2025). Systematic Intervention with Formal Caregivers to Promote Nutritional Health of Older People with Dementia: An Impact Evaluation Study. International Journal of Environmental Research and Public Health, 22(6), 849. https://doi.org/10.3390/ijerph22060849






