Sexual and Reproductive Health Behaviors Among Young Black Women in the U.S. Before the COVID-19 Pandemic: Insights for Addressing Future Challenges in STI and Pregnancy Prevention Within Key Female Populations
Abstract
1. Introduction
1.1. Biomedical HIV Prevention Interventions
1.2. Sexual Communication Self-Efficacy
2. Materials and Methods
2.1. Data Sources
2.2. Study Population
2.3. Measures
Demographics
2.4. Variables
2.4.1. Sexual Health Behaviors and Healthcare Utilization
2.4.2. Sexual Communication Efficacy
2.4.3. Reproductive Health Behaviors and Care Utilization
2.5. Data Analysis Plan
3. Results
3.1. Socio-Demographics
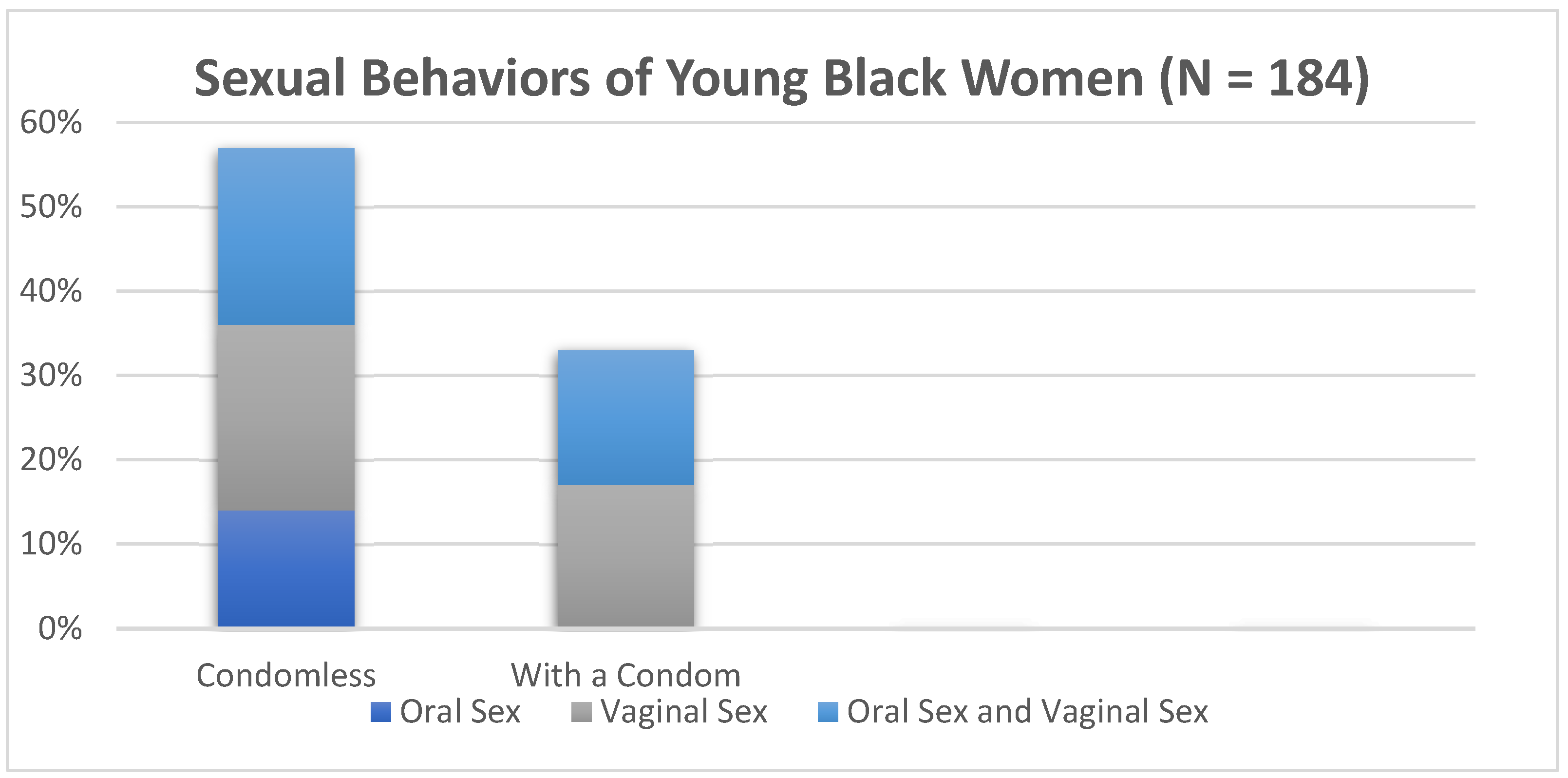
3.2. Sexual Behaviors and Healthcare Utilization
3.3. Sexual Communication Efficacy
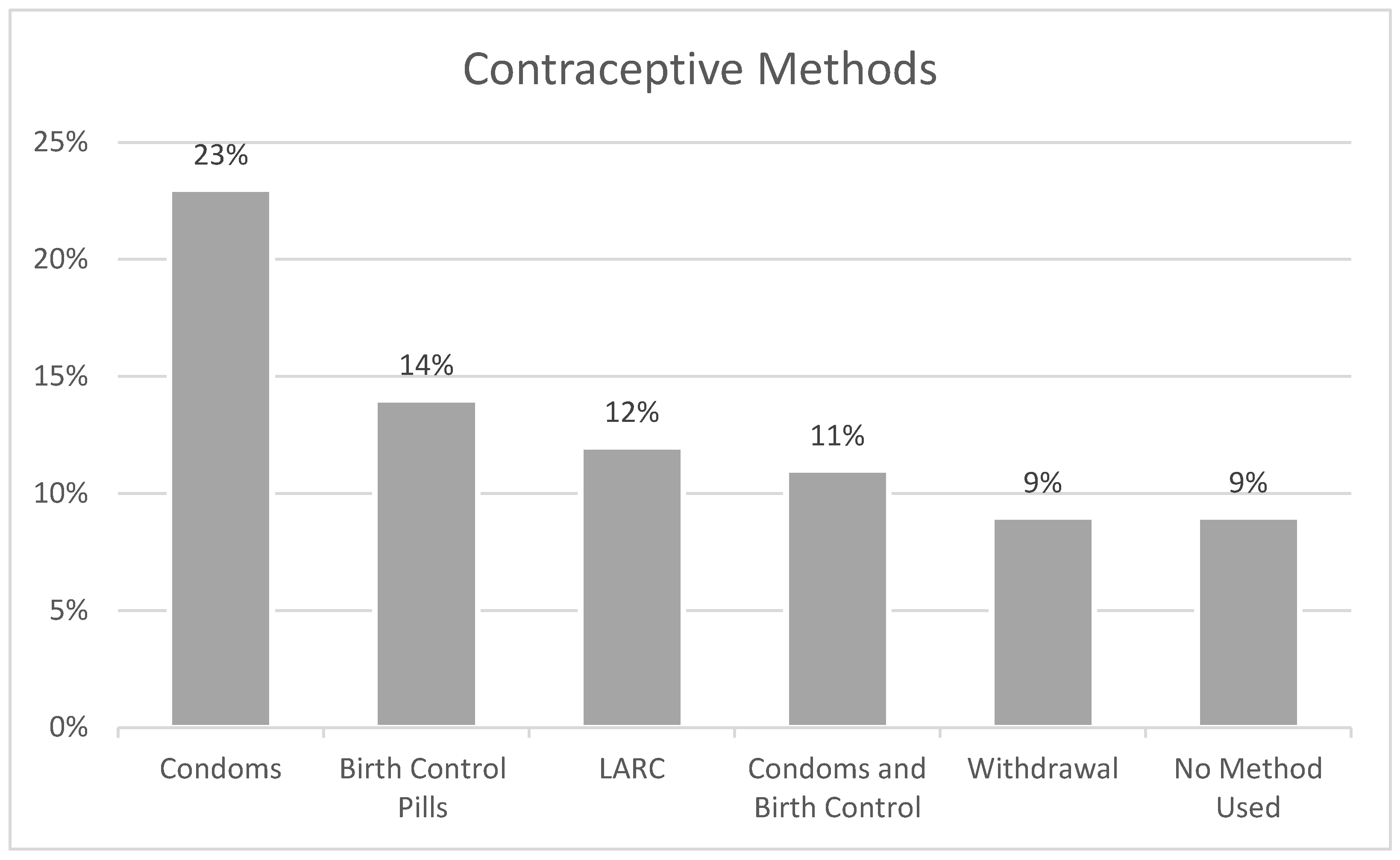
3.4. Reproductive Health Behaviors and Healthcare Utilization
4. Discussion
4.1. Sexual Health Behaviors and Sexual Healthcare Utilization
4.2. Sexual Communication Efficacy
4.3. Reproductive Health Behaviors and Healthcare Utilization
4.4. Implications for Research, Policy, and Clinical Practice and Education
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Characteristics | N | % |
|---|---|---|
| Ever tested for HIV/AIDS | ||
| No | 70 | 33.98 |
| Yes | 136 | 66.02 |
| Last time tested for HIV/AIDS | ||
| Less than 6 Months | 76 | 57.14 |
| More than 6 months ago | 57 | 42.86 |
| Ever tested for STIs | ||
| No | 70 | 33.98 |
| Yes | 136 | 66.02 |
| Last time tested for STIs | ||
| Less than 6 months ago | 85 | 62.96 |
| More than 6 months ago | 50 | 37.04 |
| Pap (Smear) Test | ||
| No | 118 | 57.28 |
| Yes | 88 | 42.72 |
| Birth Control Prescription in the past year | ||
| No | 89 | 43.2 |
| Yes | 117 | 56.8 |
| Birth control related medical exam in the past year | ||
| No | 110 | 53.4 |
| Yes | 96 | 46.60 |
| Birth Control Counseling in the past year | ||
| No | 103 | 50 |
| Yes | 103 | 50 |
| Emergency Contraception Use in the past year | ||
| No | 176 | 85.44 |
| Yes | 30 | 14.56 |
| Pregnancy Test in the past year | ||
| No | 144 | 69.9 |
| Yes | 62 | 30.1 |
| Abortion Care in the past year | ||
| No | 198 | 96.59 |
| Yes | 7 | 3.41 |
References
- World Health Organization. Sexual and Reproductive Health and Rights. Overview. 2025. Available online: https://www.who.int/health-topics/sexual-and-reproductive-health-and-rights#tab=tab_1 (accessed on 1 April 2025).
- Centers for Disease Control and Prevention. Estimated HIV Incidence and prevalence in the United States. HIV Surveillance Report, vol. 32. 2024. Available online: https://www.cdc.gov/hiv/data-research/facts-stats/race-ethnicity.html (accessed on 2 November 2024).
- Centers for Disease Control and Prevention. National Overview of STIs in 2023. 2024. Available online: https://www.cdc.gov/sti-statistics/annual/summary.html#:~:text=Findings,1.6%20million%20cases%20of%20chlamydia. (accessed on 2 November 2024).
- United States Department of Health and Human Services. Healthy People 2030. Sexually Transmitted Infections, Overview and Objectives. Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary. 2024. Available online: https://health.gov/healthypeople/objectives-and-data/browse-objectives/sexually-transmitted-infections#:~:text=Healthy%20People%202030%20focuses%20on,higher%20risk%20of%20getting%20HIV (accessed on 1 April 2025).
- Centers for Disease Control Prevention. Ending the HIVEpidemic in the, U.S. (EHE). 2023. Available online: https://www.cdc.gov/endhiv/index.html (accessed on 2 November 2024).
- Oddens, B.J. Women’s satisfaction with birth control: A population survey of physical and psychological effects of oral contraceptives, intrauterine devices, condoms, natural family planning, and sterilization among 1466 women. Contraception 1999, 59, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Gilliam, M.L.; Davis, S.D.; Neustadt, A.B.; Levey, E.J. Contraceptive attitudes among inner-city African American female adolescents: Barriers to effective hormonal contraceptive use. J. Pediatr. Adolesc. Gynecol. 2009, 22, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Silverman, J.; Torres, A.; Forrest, J.D. Barriers to contraceptive services. Fam. Plan. Perspect. 1987, 19, 94–102. [Google Scholar] [CrossRef]
- Dobbs v. Jackson Women’s Health Organization, 19–1392. Available online: https://www.oyez.org/cases/2021/19-1392 (accessed on 1 April 2025).
- Kusunoki, Y.; Barber, J.S.; Ela, E.J.; Bucek, A. Black-white differences in sex and contraceptive use among young women. Demography 2016, 53, 1399–1428. [Google Scholar] [CrossRef]
- Davis, K.R.; Weller, S.C. The Effectiveness of Condoms in Reducing Heterosexual Transmission of HIV. Fam. Plan. Perspect. 1999, 31, 272–279. [Google Scholar] [CrossRef]
- Holmes, K.K.; Levine, R.; Weaver, M. Effectiveness of condoms in preventing sexually transmitted infections. Public Health Reviews. Bull. World Health Organ. 2004, 82, 454–461. [Google Scholar]
- Pinkerton, S.D.; Abramson, P.R. Effectiveness of Condoms in Preventing HIV Transmission. Soc. Sci. Med. 1997, 44, 1303–1312. [Google Scholar] [CrossRef]
- Planned Parenthood Federation of America, Inc. (n.d.). What are the Benefits of Condoms? Available online: https://www.plannedparenthood.org/learn/birth-control/condom (accessed on 3 October 2023).
- Young-Holt, B.; Turpin, J.A.; Romano, J. Multipurpose Prevention Technologies: Opportunities and Challenges to Ensure Advancement of the Most Promising MPTs. Front. Reprod. Health 2021, 3, 704841. [Google Scholar] [CrossRef]
- Hensel, D.J.; Fortenberry, J.D.; Orr, D.P. Factors associated with event level anal sex and condom use during anal sex among adolescent women. J. Adolesc. Health 2010, 46, 232–237. [Google Scholar] [CrossRef]
- Houston, A.M.; Fang, J.; Husman, C.; Peralta, L. More than just vaginal intercourse: Anal intercourse and condom use patterns in the context of “main” and “casual” sexual relationships among urban minority adolescent females. J. Pediatr. Adolesc. Gynecol. 2007, 20, 299–304. [Google Scholar] [CrossRef]
- Fonner, V.A.; Dalglish, S.L.; Kennedy, C.E.; Baggaley, R.; O’reilly, K.R.; Koechlin, F.M.; Rodolph, M.; Hodges-Mameletzis, I.; Grant, R.M. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. Aids 2016, 30, 1973–1983. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. HIV Nexus: CDC Resources for Clinicians. 2025. Available online: https://www.cdc.gov/hivnexus/hcp/prep/index.html (accessed on 2 April 2025).
- Smit, F.; Masvawure, T.B. Barriers and facilitators to acceptability and uptake of Pre-exposure Prophylaxis (PrEP) among Black women in the United States: A systematic review. J. Racial Ethn. Health Disparities 2024, 11, 2649–2662. [Google Scholar] [CrossRef] [PubMed]
- Conley, C.; Johnson, R.; Bond, K.; Brem, S.; Salas, J.; Randolph, S. US Black cisgender women and pre-exposure prophylaxis for human immunodeficiency virus prevention: A scoping review. Women’s Health 2022, 18, 17455057221103098. [Google Scholar] [CrossRef] [PubMed]
- Baeten, J.M.; Palanee-Phillips, T.; Brown, E.R.; Schwartz, K.; Soto-Torres, L.E.; Govender, V.; Mgodi, N.M.; Kiweewa, F.M.; Nair, G.; Mhlanga, F.; et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. New Engl. J. Med. 2016, 375, 2121–2132. [Google Scholar] [CrossRef]
- World Health Organization. WHO Continues to Support Its Conditional Recommendation for the Dapivirine Vaginal Ring as an Additional Prevention Option for Women at Substantial Risk of, H.I.V. 2025. Available online: https://www.who.int/news/item/09-12-2021-who-continues-to-support-its-conditional-recommendation-for-the-dapivirine-vaginal-ring#:~:text=The%20non%2Dprofit%20International%20Partnership,and%20Drug%20Administration%20(USFDA) (accessed on 2 April 2025).
- World Health Organization. The US FDA approved cabotegravir extended-release—The first long-acting injectable option for HIV pre-exposure prophylaxis. 2025. Available online: https://www.who.int/news/item/21-12-2021-fda-approved-cabotegravir-extended-release (accessed on 3 April 2025).
- Craddock, J.; Mangum, L.C.; Aidoo-Frimpong, G.; Whitfield, D.L. The Association of HIV Pre-exposure Prophylaxis (PrEP) Interest and Sexual Risk Behaviors among Young Black Women. AIDS Patient Care and STDs 2021, 35, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Mangum, L.C.; Craddock, J.; Whitfield, D. Associations in Preventive Sexual Health Service Utilization and PrEP Interest among Young Black Women in the United States, 2018. AIDSCare 2021, 33. [Google Scholar] [CrossRef]
- Quinn-Nilas, C.; Milhausen, R.R.; Breuer, R.; Bailey, J.; Pavlou, M.; DiClemente, R.J.; Wingood, G.M. Validation of the Sexual Communication Self-Efficacy Scale. Health Educ. Behav. 2016, 43, 165–171. [Google Scholar] [CrossRef]
- Carmack, C.; Roncancio, A.M.; Gerecht, L.; Ansari, M. Perceived partner beliefs about condoms and self-efficacy communication within the context of the theory of gender and power. J. Community Psychol. 2020, 48, 1424–1437. [Google Scholar] [CrossRef]
- Crosby, R.A.; DiClemente, R.J.; Salazar, L.F.; Wingood, G.M.; McDermott-Sales, J.; Young, A.M.; Rose, E. Predictors of Consistent Condom Use Among Young African American Women. AIDS Behav. 2013, 17, 865–871. [Google Scholar] [CrossRef]
- Javier, S.J.; Abrams, J.A.; Moore, M.P.; Belgrave, F.Z. Condom Use Efficacy and Sexual Communication Skills Among African American College Women. Health Promot. Pract. 2018, 19, 287–294. [Google Scholar] [CrossRef]
- Nehl, E.J.; Elifson, K.; DePadilla, L.; Sterk, C. Sex Partner Type, Drug Use and Condom Use Self-Efficacy Among African Americans from Disadvantaged Neighborhoods: Are Associations with Consistent Condom Use Moderated by Gender? J. Sex Res. 2016, 53, 805–815. [Google Scholar] [CrossRef]
- Davis, K.C.; Hammett, J.F.; Chen, W.; Stewart, R.; Kirwan, M. A Scoping Review of Nonconsensual Condom Removal (“Stealthing”) Research. Trauma Violence Abus. 2024, 25, 215–230. [Google Scholar] [CrossRef]
- Teitelman, A.M.; Tennille, J.; Bohinski, J.M.; Jemmott, L.S.; Jemmott, J.B. Unwanted Unprotected Sex: Condom Coercion by Male Partners and Self-silencing of Condom Negotiation Among Adolescent Girls. Adv. Nurs. Sci. 2011, 34, 243–259. [Google Scholar] [CrossRef]
- Negash, S.; Roberson, P.N.E.; Seshadri, G.; Ayres, K. Relational Factors and Sexual Health for Female College Students in Exclusive Heterosexual Relationships. Sex. Cult. 2021, 25, 2111–2128. [Google Scholar] [CrossRef]
- Craddock, J.B. Sex Talks: An Examination of Young Black Women’s Sex Talks: An Examination of Young Black Women’s Social Networks, Sexual Health Communication and HIV Prevention Behaviors. Doctoral Dissertation, University of Southern California, Los Angeles, CA, USA, 2019. ProQuest Dissertations & Theses Global. [Google Scholar]
- Craddock, J.B.; Franke, N.D.; Kingori, C. Associations of Social Network- and Individual-Level Factors with HIV Testing, Condom Use, and Interest in PrEP Among Young Black Women. Arch Sex Behav. 2022, 51, 2473–2483. [Google Scholar] [CrossRef]
- United States Census Bureau (n.d.). Regions and Divisions. Available online: https://www.census.gov/history/www/programs/geography/regions_and_divisions.html#:~:text=Land%20area%2C%20population%2C%20and%20density,Texas%2C%20Northwestern%2C%20and%20California (accessed on 1 April 2025).
- StataCorp. Stata Statistical Software: Release 18; StataCorp LLC.: College Station, TX, USA, 2023. [Google Scholar]
- Dyson, Y.D.; Mobley, Y.; Harris, G.; Randolph, S.D. Using the Social-Ecological Model of HIV Prevention to Explore HIV Testing Behaviors of Young Black College Women. J. Assoc. Nurses AIDS Care 2018, 29, 53–59. [Google Scholar] [CrossRef]
- Norwood, C.R.; Zhang, Y. Condom Attitudes and Use among African American College Women Students. J. Black Sex. Relatsh. 2015, 2, 83–99. [Google Scholar] [CrossRef]
- Crooks, N.; Wise, A.; Frazier, T. Addressing sexually transmitted infections in the sociocultural context of black heterosexual relationships in the United States. Soc. Sci. Med. 2020, 263, 113303. [Google Scholar] [CrossRef]
- Campbell, E.; Anderson, N. Perceptions and Knowledge of HIV/AIDS Among Black Women: An Exploratory Study. J. AIDS HIV Treat. 2025, 7, 1–12. [Google Scholar] [CrossRef]
- Eldridge, G.D.; St Lawrence, J.S.; Little, C.E.; Shelby, M.C.; Brasfield, T.L. Barriers to condom use and barrier method preferences among low-income African-American women. Women Health 1995, 23, 73–89. [Google Scholar] [CrossRef]
- McLaurin-Jones, T.; Lashley, M.-B.; Marshall, V. Minority College Women’s Views on Condom Negotiation. Int. J. Environ. Res. Public Health 2016, 13, 40. [Google Scholar] [CrossRef]
- Davis, K.C.; Stappenbeck, C.A.; Norris, J.; George, W.H.; Jacques-Tiura, A.J.; Schraufnagel, T.J.; Kajumulo, K.F. Young Men’s Condom Use Resistance Tactics: A Latent Profile Analysis. J. Sex Res. 2014, 51, 454–465. [Google Scholar] [CrossRef]
- Jenkins, C.C.; Kennedy, B.R. An Exploratory Study of Sexual Assertiveness and Characteristics of African American Women in Negotiating Condom Use at an HBCU. J. Cult. Divers. 2013, 20, 139–145. [Google Scholar]
- Crooks, N.; King, B.; Tluczek, A.; Sales, J.M. The Process of Becoming a Sexual Black Woman: A Grounded Theory Study. Perspect. Sex. Reprod. Health 2019, 51, 17–25. [Google Scholar] [CrossRef]
- Gabriel, R.C.D. “THE CALIFORNIA HEALTHY YOUTH ACT: A POLICY ANALYSIS ON CALIFORNIA’S COMPREHENSIVE SEX EDUCATION MANDATE” (2020). Electronic Theses, Projects, and Dissertations. 1119. Available online: https://scholarworks.lib.csusb.edu/etd/1119 (accessed on 7 May 2025).
- Jackson, A.V.; Karasek, D.; Dehlendorf, C.; Foster, D.G. Racial and ethnic differences in women’s preferences for features of contraceptive methods. Contraception 2016, 93, 406–411. [Google Scholar] [CrossRef]
- Khan, A.; Culbreath, K.; Goldstein, Z.; Greene, D.N. Access barriers in testing for sexually transmitted infections across gender and sexual identities. Clin. Lab. Med. 2024, 44, 647–663. [Google Scholar] [CrossRef]
- Treder, K.; White, K.O.; Woodhams, E.; Pancholi, R.; Yinusa-Nyahkoon, L. Racism and the reproductive health experiences of US-born Black women. Obstet. Gynecol. 2022, 139, 407–416. [Google Scholar] [CrossRef]
- US Preventive Services Task Force. Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2018, 320, 674–686. [Google Scholar] [CrossRef]
| Characteristics | ||
|---|---|---|
| M (SD) | ||
| Age | 21.14 (1.74) | |
| N | % | |
| Education Level | ||
| High School Graduate | 28 | 13.40 |
| Some College | 92 | 44.02 |
| Associate’s Degree | 7 | 3.35 |
| Bachelor’s Degree | 73 | 34.93 |
| Professional Degree | 9 | 4.31 |
| Current Health Insurance | ||
| No | 5 | 2.48 |
| Yes | 197 | 97.52 |
| Relationship Status | ||
| Single | 90 | 42.86 |
| Dating | 20 | 9.52 |
| Committed Relationship | 53 | 25.24 |
| Casual Sex Partner | 9 | 4.29 |
| Last Sexual Encounter | ||
| Within the last week | 60 | 32.43 |
| 1–4 weeks ago | 39 | 21.08 |
| 1–3 months ago | 44 | 23.78 |
| 3–6 months ago | 17 | 9.19 |
| 6–12 months ago | 13 | 7.03 |
| 1 year or longer | 12 | 6.49 |
| Last Sexual Encounter Partner Type | ||
| Life Partner, Husband, Wife, Spouse | 11 | 5.98 |
| Girlfriend or Boyfriend | 82 | 44.57 |
| Hookup or Casual Sex Partner | 53 | 28.8 |
| Friends with Benefit | 38 | 20.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mangum, L.C.; Craddock, J. Sexual and Reproductive Health Behaviors Among Young Black Women in the U.S. Before the COVID-19 Pandemic: Insights for Addressing Future Challenges in STI and Pregnancy Prevention Within Key Female Populations. Int. J. Environ. Res. Public Health 2025, 22, 793. https://doi.org/10.3390/ijerph22050793
Mangum LC, Craddock J. Sexual and Reproductive Health Behaviors Among Young Black Women in the U.S. Before the COVID-19 Pandemic: Insights for Addressing Future Challenges in STI and Pregnancy Prevention Within Key Female Populations. International Journal of Environmental Research and Public Health. 2025; 22(5):793. https://doi.org/10.3390/ijerph22050793
Chicago/Turabian StyleMangum, Laurenia C., and Jaih Craddock. 2025. "Sexual and Reproductive Health Behaviors Among Young Black Women in the U.S. Before the COVID-19 Pandemic: Insights for Addressing Future Challenges in STI and Pregnancy Prevention Within Key Female Populations" International Journal of Environmental Research and Public Health 22, no. 5: 793. https://doi.org/10.3390/ijerph22050793
APA StyleMangum, L. C., & Craddock, J. (2025). Sexual and Reproductive Health Behaviors Among Young Black Women in the U.S. Before the COVID-19 Pandemic: Insights for Addressing Future Challenges in STI and Pregnancy Prevention Within Key Female Populations. International Journal of Environmental Research and Public Health, 22(5), 793. https://doi.org/10.3390/ijerph22050793






