Ecological Impacts of Structural Racism on Health Disparity Through Its Determinants and Mediating Factors: A Case Study on Low Birthweight in Three Race/Ethnicity Groups in the United States
Abstract
1. Background
2. Materials and Methods
2.1. The Literature Review
2.2. Ecological Health Disparity Analysis of County-Level Data
3. Results and Discussion
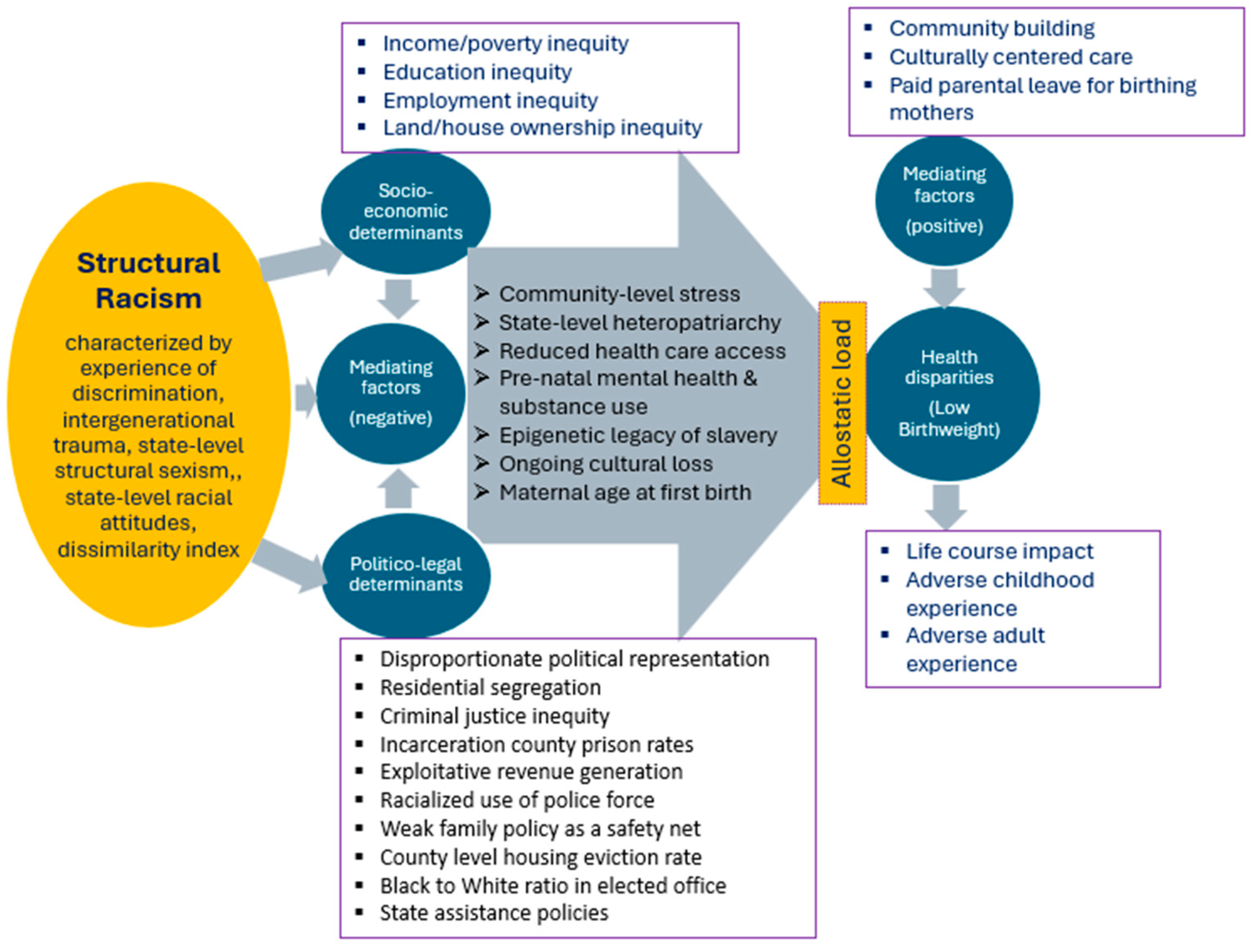
3.1. Literature Review for Contextual Background of Low Birthweight as Pathway for Structural Racism
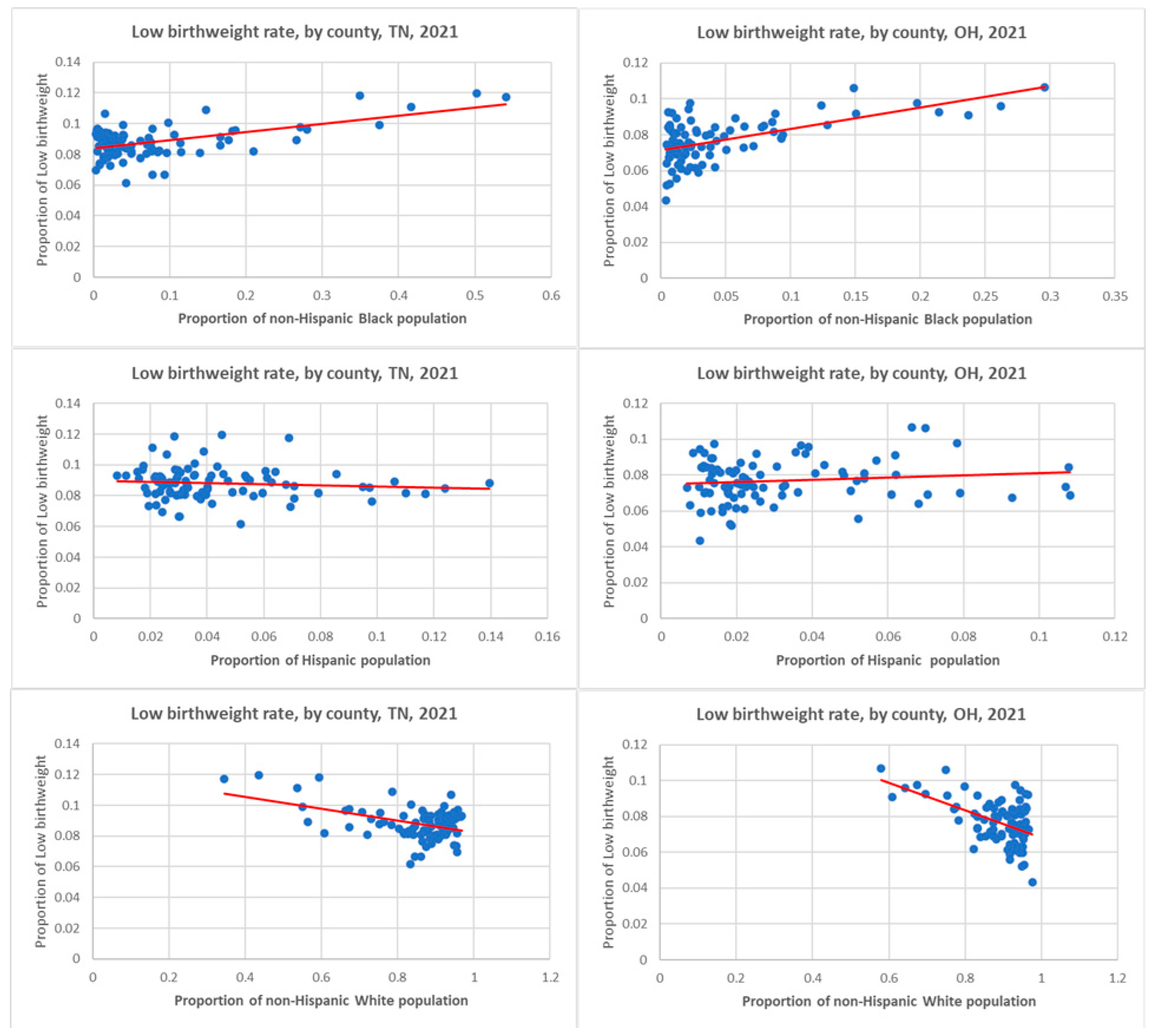
3.2. Ecological Case Study of Two US Counties
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Whitehead, M. The Concepts and Principles of Equity and Health. Int. J. Health Serv. 1992, 22, 429–445. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (US CDC). CDC Health Disparities and Inequalities Report United States; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2011. Available online: https://stacks.cdc.gov/view/cdc/5837 (accessed on 27 January 2025).
- Public Health Agency of Canada (PHAC). Key Health Inequalities in Canada: A National Portrait; Public Health Agency of Canada: Ottawa, ON, Canada, 2018; Available online: https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/science-research/key-health-inequalities-canada-national-portrait-executive-summary/key_health_inequalities_full_report-eng.pdf (accessed on 27 January 2025).
- Rasali, D.; Kao, D.; Fong, D.; Qiyam, L. Priority Health Equity Indicators for British Columbia: Preventable and Treatable Premature Mortality; BC Center for Disease Control, Provincial Health Services Authority: Vancouver, BC, Canada, 2019; Available online: http://www.bccdc.ca/health-professionals/professional-resources/health-equity-indicators (accessed on 27 January 2025).
- Rasali, D.; Li, C.; Mak, S.; Rose, C.; Janjua, N.; Patrick, D. Correlations of COVID-19 Incidence with Neighborhood Demographic Factors in BC. Ann. Epidemiol. 2021, 61, 17. [Google Scholar] [CrossRef]
- Brown, T.H.; Homan, P.A. Frontiers in Measuring Structural Rcism and its Health Effects. Health Serv. Res. 2022, 57, 443–447. [Google Scholar] [CrossRef]
- GBD US Health Disparities Collaborators. Life Expectancy by County, Race, and Ethnicity in the USA, 2000 19: A Systematic Analysis of Health Disparities. Lancet 2022, 400, 25–38. [Google Scholar] [CrossRef]
- Gee, G.C.; Ford, C.L. Structural Racism and Health Inequities: Old Issues, New Directions. Du. Bois Rev. Social. Sci. Res. Race 2011, 8, 115–132. [Google Scholar] [CrossRef]
- Krieger, N. Discrimination and Health Inequities. Int. J. Health Serv. 2014, 44, 643–710. [Google Scholar] [CrossRef]
- Bailey, Z.D.; Krieger, N.; Agénor, M.; Graves, J.; Linos, N.; Bassett, M.T. Structural Racism and Health Inequities in the USA: Evidence and Interventions. Lancet 2017, 389, 1453–1463. [Google Scholar] [CrossRef]
- Sweeting, J.A.; Akinyemi, A.A.; Holman, E.A. Parental Preconception Adversity and Offspring Health in African Americans: A Systematic Review of Intergenerational Studies. Trauma Violence Abus. 2023, 24, 1677–1692. [Google Scholar] [CrossRef]
- Williams, D.R.; Lawrence, J.A.; Davis, B.A. Racism and Health: Evidence and Needed Research. Annu. Rev. Public Health 2019, 40, 105–125. [Google Scholar] [CrossRef]
- Rasali, D.P.; Woodruff, B.M.; Alzyoud, F.A.; Kiel, D.; Schaffzin, K.T.; Osei, W.D.; Ford, C.L.; Johnson, S. Cross-Disciplinary Rapid Scoping Review of Structural Racial and Caste Discrimination Associated with Population Health Disparities in the 21st Century. Societies 2024, 14, 186. [Google Scholar] [CrossRef]
- Global Nutrition Target Collaborators. Global, Regional, and National Progress towards the 2030 Global Nutrition Targets and Forecasts to 2050: A Systematic Analysis for the Global Burden of Disease Study 2021. Lancet 2025, 404, 2543–2583. [Google Scholar] [CrossRef]
- Nguyen, T.T.; Adams, N.; Huang, D.; Glymour, M.M.; Allen, A.M.; Nguyen, Q.C. The Association Between State-Level Racial Attitudes Assessed from Twitter Data and Adverse Birth Outcomes: Observational Study. JMIR Public Health Surveill. 2020, 6, e17103. [Google Scholar] [CrossRef]
- Chegwin, V.; Teitler, J.; Muchomba, F.M.; Reichman, N.E. Racialized Police Use of Force and Birth Outcomes. Social Sci. Med. 2023, 321, 115767. [Google Scholar] [CrossRef]
- Pearlman, J.; Robinson, D.E. State Policies, Racial Disparities, and Income Support: A Way to Address Infant Outcomes and the Persistent Black-White Gap? J. Health Politics Policy Law. 2022, 47, 225–258. [Google Scholar] [CrossRef]
- Patchen, L.; McCullers, A.; Beach, C.; Browning, M.; Porter, S.; Danielson, A.; Asegieme, E.; Richardson, S.R.; Jost, A.; Jensen, C.S.; et al. Safe Babies, Safe Moms: A Multifaceted, Trauma Informed Care Initiative. Matern. Child Health J. 2024, 28, 31–37. [Google Scholar] [CrossRef]
- Stanhope, K.K.; Kapila, P.; Umerani, A.; Hossain, A.; Salah, M.A.; Singisetti, V.; Carter, S.; Boulet, S.I. Political Representation and Perinatal Outcomes to Black, White, and Hispanic People in Georgia: A Cross-sectional Study. Ann. Epid. 2023, 87, 38–44. [Google Scholar] [CrossRef]
- Blumenshine, P.; Egerter, S.; Barclay, C.J.; Cubbin, C.; Braveman, P.A. Socioeconomic Disparities in Adverse Birth Outcomes: A Systematic Review. Am. J. Prev. Med. 2010, 39, 263–272. [Google Scholar] [CrossRef]
- Bridgeman-Bunyoli, A.M.; Cheyney, M.; Monroe, S.M.; Wiggins, N.; Vedam, S. Preterm and Low Birthweight Birth in the United States: Black Midwives Speak of Causality, Prevention, and Healing. Birth, 2022, 49, 526–539. [Google Scholar] [CrossRef]
- Davis, B.A.; Arcaya, M.C.; Williams, D.R.; Krieger, N. The impact of County-level Fees & Fines as Exploitative Revenue Generation on US Birth Outcomes 2011–2015. Health Place 2023, 80, 102990. [Google Scholar] [CrossRef]
- Mehra, R.; Boyd, L.M.; Ickovics, J.R. Racial Residential Segregation and Adverse Birth Outcomes: A Systematic Review and Meta-analysis. Soc. Sci. Med. 2017, 191, 237–250. [Google Scholar] [CrossRef]
- Chantarat, T.; Van Riper, D.C.; Hardeman, R.R. Multidimensional Structural Racism Predicts Birth Outcomes for Black and White Minnesotans. Health Serv. Res. 2022, 57, 448–457. [Google Scholar] [CrossRef]
- Chantarat, T.; Mentzer, K.M.; Van Riper, D.C.; Hardeman, R.R. Where are the Labor Markets?: Examining the Association between Structural Racism in Labor Markets and Infant Birth Weight. Health Place 2022, 74, 102742. [Google Scholar] [CrossRef]
- Wallace, M.E.; Mendola, P.; Liu, D.; Grantz, K.L. Joint Effects of Structural Racism and Income Inequality on Small-for-Gestational-Age Birth. Am. J. Public Health 2015, 105, 1681–1688. [Google Scholar] [CrossRef]
- Sonderlund, A.L.; Williams, N.L.; Charifson, M.; Ortiz, R.; Sealy-Jefferson, S.; De Leon, E.; Schoenthaler, A. Structural Racism and Health: Assessing the Mediating Role of Community Mental Distress and Health Care Access in the Association between Mass Incarceration and Adverse Birth Outcomes. SSM—Popul. Health 2023, 24, 101529. [Google Scholar] [CrossRef]
- Everett, B.G.; Limburg, A.; Homan, P.; Philbin, M.M. Structural Heteropatriarchy and Birth Outcomes in the United States. Demography 2022, 59, 89–110. [Google Scholar] [CrossRef]
- Chambers, B.D.; Erausquin, J.T.; Tanner, A.E.; Nichols, T.R.; Brown-Jeffy, S. Testing the Association Between Traditional and Novel Indicators of County-Level Structural Racism and Birth Outcomes among Black and White Women. J. Racial Ethn. Health Disparities 2018, 5, 966–977. [Google Scholar] [CrossRef]
- Nagle, A.; Samari, G. State-level Structural Sexism and Cesarean Sections in the United States. Soc. Sci. 2021, 289, 114406. [Google Scholar] [CrossRef] [PubMed]
- Mersky, J.P.; Jeffers, N.K.; Lee, C.P.; Shlafer, R.J.; Jackson, D.B.; Gómez, A. Linking Adverse Experiences to Pregnancy and Birth Outcomes: A Life Course Analysis of Racial and Ethnic Disparities Among Low—Income Women. J. Racial Ethn. Health Disparities 2024, 11, 1741–1753. [Google Scholar] [CrossRef]
- Christian, L.M.; Koenig, J.; Williams, D.P.; Kapuku, G.; Thayer, J.F. Impaired Vasodilation in Pregnant African Americans: Preliminary Evidence of Potential Antecedents and Consequences. Psychophysiology 2012, 58, e13699. [Google Scholar] [CrossRef]
- Karasek, D.; Raifman, S.; Dow, W.H.; Hamad, R.; Goodman, J.M. Evaluating the Effect of San Francisco’s Paid Parental Leave Ordinance on Birth Outcomes. Int. J. Environ. Res. Public Health 2022, 19, 11962. [Google Scholar] [CrossRef]
- Jasthi, D.L.; Nagle-Yang, S.; Frank, S.; Masotya, M.; Huth-Bocks, A. Associations Between Adverse Childhood Experiences and Prenatal Mental Health and Substance Use Among Urban, Low—Income Women. Community Ment. Health J. 2012, 58, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Geronimus, A.T.; Bound, J.; Hughes, L. Trend Toward Older Maternal Age Contributed to Growing Racial Inequity in Very-Low-Birthweight Infants in the US. Health Aff. 2023, 42, 674–682. [Google Scholar] [CrossRef] [PubMed]
- Harville, E.W.; Wallace, M.E.; Theall, K.P. Eviction as a Social Determinant of Pregnancy Health: County-level Eviction Rates and Adverse Birth Outcomes in the United States. Wiley-Health Soc. Care Community 2022, 30, e5579–e5587. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S.; Stellar, E. Stress and the Individual. Mechanisms Leading to Disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef]
- Guidi, J.; Lucente, M.; Sonino, N.; Fava, G.A. Allostatic Load and Its Impact on Health: A Systematic Review. Psychother. Psychosom. 2021, 90, 11–27. [Google Scholar] [CrossRef]
- Alson, J.G.; Robinson, W.R.; Pittman, L.; Doll, K.M. Incorporating Measures of Structural Racism into Population Studies of Reproductive Health in the United States: A Narrative Review. Health Equity. 2021, 5, 49–58. [Google Scholar] [CrossRef]
| Author(s) (Year of Publication) | Indicator(s) of Structural Racism as Mediating Factors of Impact on Low Birthweight | Extract from the Relevant Findings |
|---|---|---|
| Chantarat et al. (2022a) [24] |
|
|
| Chantarat et al. (2022b) [25] |
|
|
| Wallace et al. (2015) [26] |
|
|
| Sonderlund et al. (2023) [27] |
|
|
| Everett et al. (2022) [28] |
|
|
| Chambers et al. (2018) [29] |
|
|
| Mehra et al. (2017) [23] |
|
|
| Chegwin et al. (2023) [16] |
|
|
| Nagle and Samari (2019) [30] |
|
|
| Pearlman and Robinson (2022) [17] |
|
|
| Nguyen et al. (2020) [15] |
|
|
| Patchen et al. (2023) [18] |
|
|
| Mersky et al. (2023) [31] |
|
|
| Stanhope et al. (2023) [19] |
|
|
| Bridgeman-Bunyoli et al. (2022) [21] |
|
|
| Christian et al. (2021) [32] |
|
|
| Davis et al. (2023) [22] |
|
|
| Karasek et a. (2022) [33] |
|
|
| Jasthi et al. (2022) [34] |
|
|
| Geronimus et al. (2023) [35] |
|
|
| Harville et al. (2022) [36] |
|
|
| Socio-Demographic and Health Data | US States | |
|---|---|---|
| Ohio (n = 88) | Tennessee (n = 95) | |
| State Total Population | 11,780,017 | 6,975,218 |
| % non-Hispanic Black | 12.8 | 16.6 |
| % Hispanic | 4.3 | 6.1 |
| % Asian | 2.76 | 2.0 |
| % Non-Hispanic White | 77.7 | 73.1 |
| Poor or Fair Health, % | 14.5 | 15.7 |
| Low Birthweight, % births | 8.6 | 9.1 |
| Teen Births, per 1000 live births | 20.9 | 27.2 |
| Life Expectancy, years | 76.5 | 75.3 |
| Diabetes Prevalence, % | 10.9 | 12.5 |
| Air Pollution Particulate Matter (PM2.5) | 8.9 | 7.6 |
| Severe Housing Problems, % | 13.1 | 13.4 |
| Tennessee | Ohio | |||
|---|---|---|---|---|
| R | (n) | R | (n) | |
| Non-Hispanic Black | 0.557 ** | 95 | 0.584 ** | 88 |
| Hispanic | −0.102 | 95 | 0.127 | 88 |
| Non-Hispanic White | −0.459 ** | 95 | −0.512 ** | 88 |
| High School Completion | −0.202 * | 95 | 0.116 | 88 |
| High School Graduation | −0.203 | 90 | −0.401 ** | 88 |
| School Segregation | 0.249 * | 90 | 0.485 ** | 87 |
| Income Inequality | 0.263 * | 95 | 0.594 ** | 88 |
| Median Household Income | −0.294 ** | 95 | −0.391 ** | 88 |
| Children in Poverty | 0.379 ** | 95 | 0.600 ** | 88 |
| Unemployment | 0.559 ** | 95 | 0.539 ** | 88 |
| Homeownership | −0.404 ** | 95 | −0.548 ** | 88 |
| Severe Housing Problems | 0.473 ** | 95 | 0.526 ** | 88 |
| Life Expectancy | −0.348 ** | 95 | −0.549 ** | 88 |
| Frequent Physical Distress | 0.329 ** | 95 | 0.260 * | 88 |
| Diabetes Prevalence | 0.620 ** | 95 | 0.529 ** | 88 |
| HIV Prevalence | 0.398 ** | 91 | 0.528 ** | 86 |
| Food Insecurity | 0.339 ** | 95 | 0.528 ** | 88 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rasali, D.P.; Lefler, L.L.; Ford, C.L.; Osei, W.D.; Schaffzin, K.T. Ecological Impacts of Structural Racism on Health Disparity Through Its Determinants and Mediating Factors: A Case Study on Low Birthweight in Three Race/Ethnicity Groups in the United States. Int. J. Environ. Res. Public Health 2025, 22, 715. https://doi.org/10.3390/ijerph22050715
Rasali DP, Lefler LL, Ford CL, Osei WD, Schaffzin KT. Ecological Impacts of Structural Racism on Health Disparity Through Its Determinants and Mediating Factors: A Case Study on Low Birthweight in Three Race/Ethnicity Groups in the United States. International Journal of Environmental Research and Public Health. 2025; 22(5):715. https://doi.org/10.3390/ijerph22050715
Chicago/Turabian StyleRasali, Drona P., Leanne L. Lefler, Chandra L. Ford, William D. Osei, and Katharine T. Schaffzin. 2025. "Ecological Impacts of Structural Racism on Health Disparity Through Its Determinants and Mediating Factors: A Case Study on Low Birthweight in Three Race/Ethnicity Groups in the United States" International Journal of Environmental Research and Public Health 22, no. 5: 715. https://doi.org/10.3390/ijerph22050715
APA StyleRasali, D. P., Lefler, L. L., Ford, C. L., Osei, W. D., & Schaffzin, K. T. (2025). Ecological Impacts of Structural Racism on Health Disparity Through Its Determinants and Mediating Factors: A Case Study on Low Birthweight in Three Race/Ethnicity Groups in the United States. International Journal of Environmental Research and Public Health, 22(5), 715. https://doi.org/10.3390/ijerph22050715







