The Impact of Telepresence Robots on Family Caregivers and Residents in Long-Term Care
Abstract
1. Introduction
- What are the experiences of residents and families in using telepresence robots?
- Does the telepresence robot reduce loneliness, improve the quality of life of residents in LTC homes, and reduce the burden for family caregivers?
2. Methods
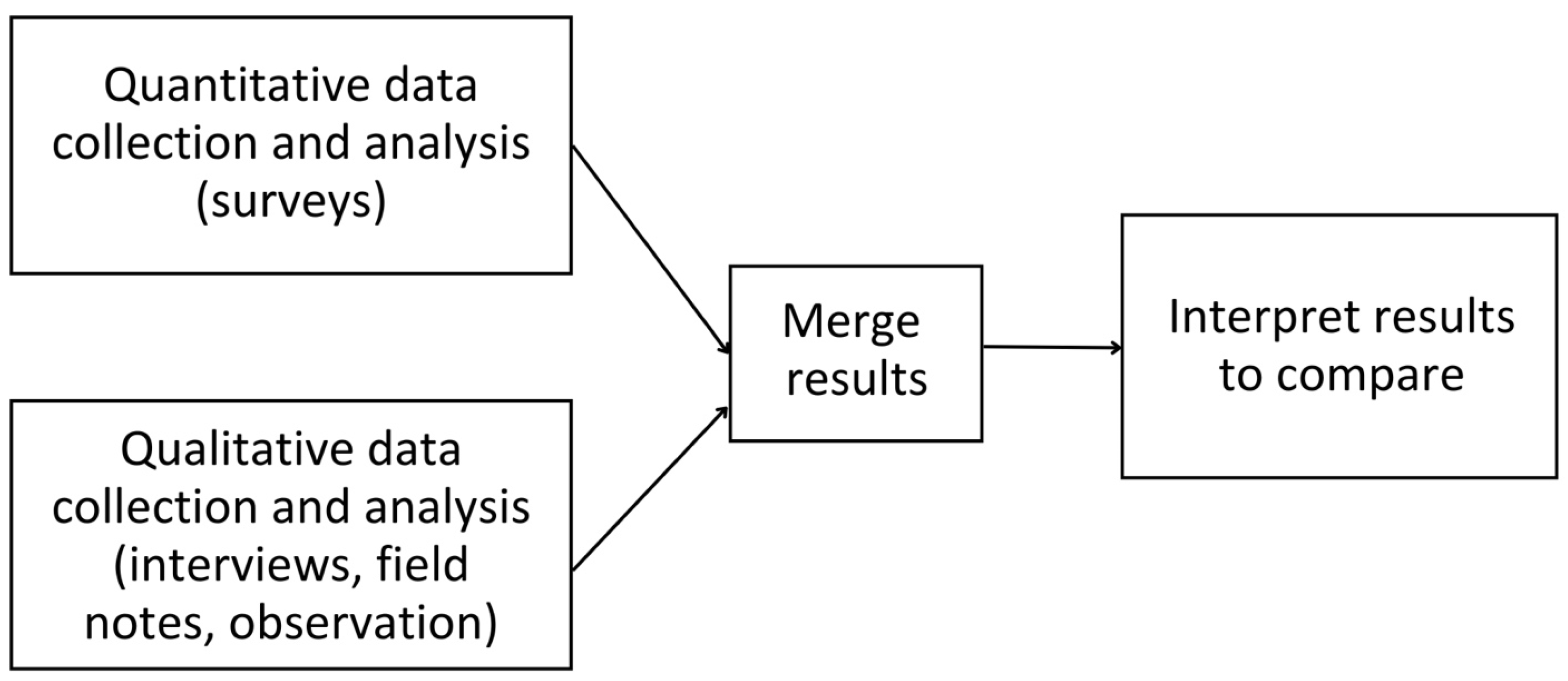
2.1. Design
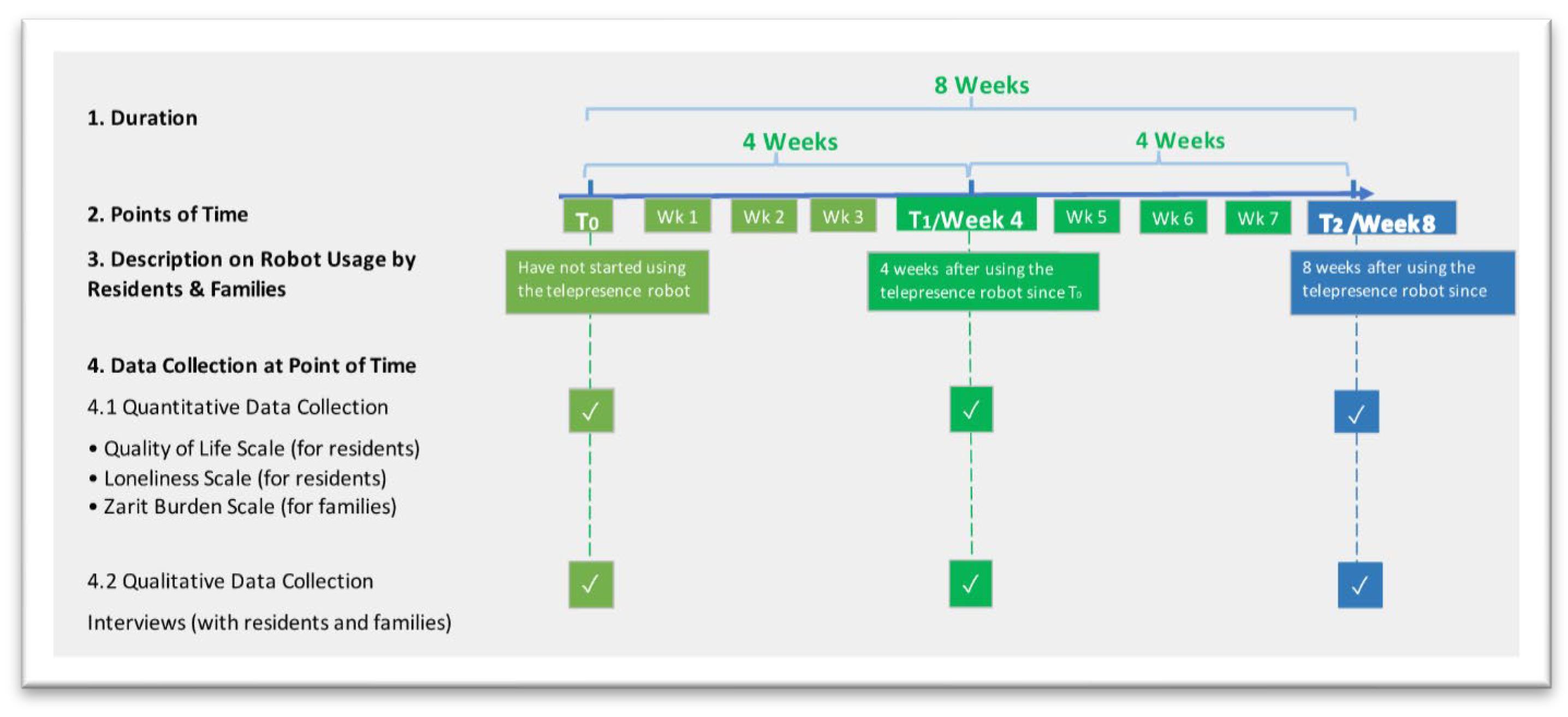
2.2. Data Collection
2.2.1. Research Instruments
2.2.2. Setting
2.2.3. Participant Recruitment and Sampling
2.2.4. Timeline
2.2.5. The Research Team
2.3. Data Analysis
2.3.1. Quantitative Data Analysis
2.3.2. Qualitative Data Analysis
2.4. Data Integration
2.5. Rigour
2.6. Ethics
3. Results
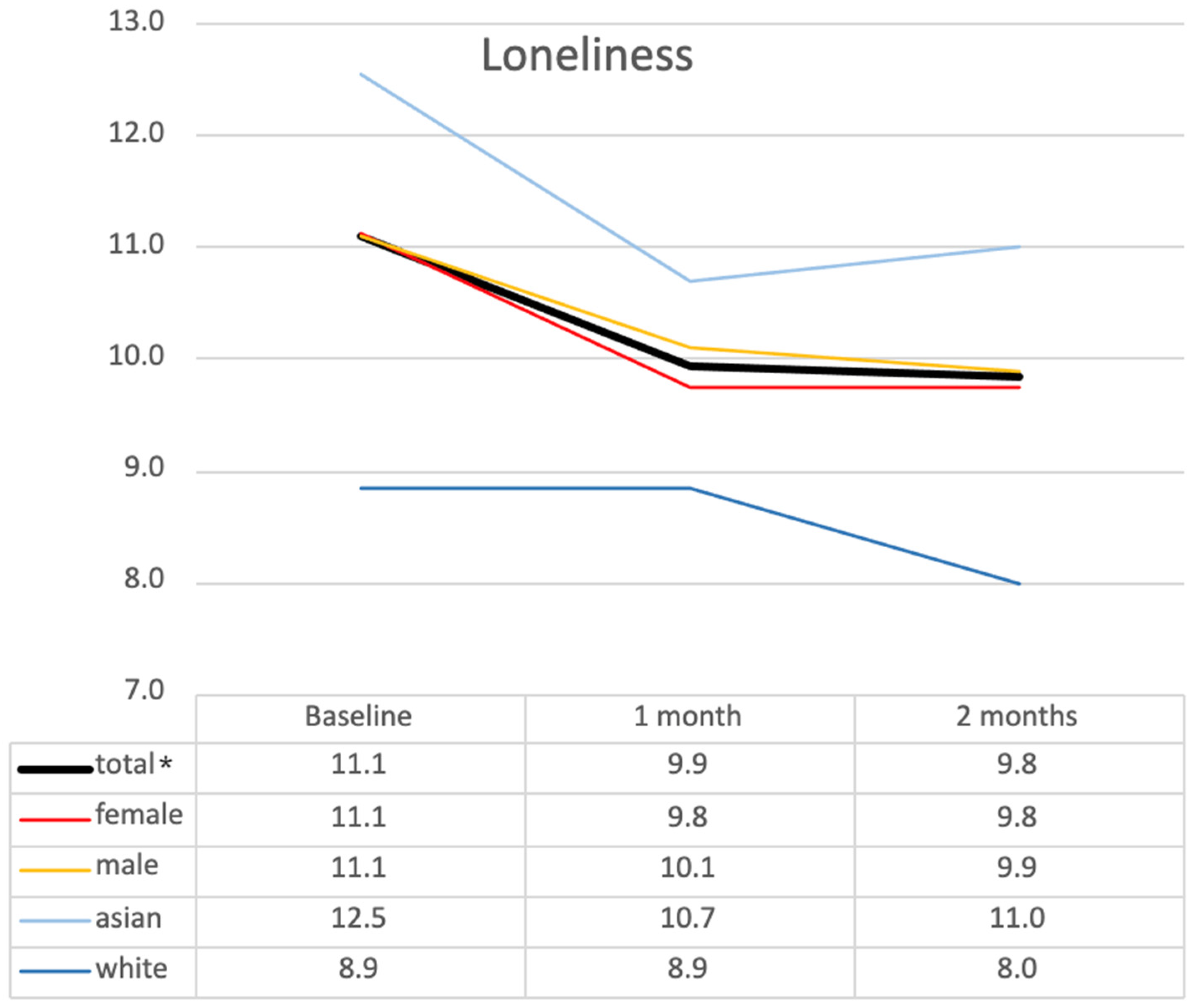
3.1. Quantitative Results
3.2. Qualitative Results
3.2.1. Impact on Residents
Promotes Connections and Nurtures Closeness
Provides Meaningful Engagement
Acknowledges Robots’ Limitations
3.2.2. Impact on Family Caregivers
Reduces Stress and Guilt
Enables Continuity in Caregiver’s Role and Complements In-Person Visits
Offers Reassurance on Residents’ Quality of Life
4. Discussion and Implications
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of variance |
| LTC | Long-term care |
| PI | Principal investigator |
| QOL-AD | Quality of Life—Alzheimer’s Disease |
References
- White, E.M.; Wetle, T.F.; Reddy, A.; Baier, R.R. Front-Line Nursing Home Staff Experiences During the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2021, 22, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Drageset, J.; Kirkevold, M.; Espehaug, B. Loneliness and Social Support among Nursing Home Residents without Cognitive Impairment: A Questionnaire Survey. Int. J. Nurs. Stud. 2011, 48, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Paque, K.; Bastiaens, H.; Van Bogaert, P.; Dilles, T. Living in a Nursing Home: A Phenomenological Study Exploring Residents’ Loneliness and Other Feelings. Scand. J. Caring Sci. 2018, 32, 1477–1484. [Google Scholar] [CrossRef] [PubMed]
- Dahlberg, L.; Andersson, L.; McKee, K.J.; Lennartsson, C. Predictors of Loneliness among Older Women and Men in Sweden: A National Longitudinal Study. Aging Ment. Health 2015, 19, 409–417. [Google Scholar] [CrossRef]
- Wright, M.R.; Hammersmith, A.M.; Brown, S.L.; Lin, I.-F. The Roles of Marital Dissolution and Subsequent Repartnering on Loneliness in Later Life. J. Gerontol. Ser. B 2020, 75, 1796–1807. [Google Scholar] [CrossRef]
- de Boise, S.; Hearn, J. Are Men Getting More Emotional? Critical Sociological Perspectives on Men, Masculinities and Emotions. Sociol. Rev. 2017, 65, 779–796. [Google Scholar] [CrossRef]
- Kemperman, A.; van den Berg, P.; Weijs-Perrée, M.; Uijtdewillegen, K. Loneliness of Older Adults: Social Network and the Living Environment. Int. J. Environ. Res. Public Health 2019, 16, 406. [Google Scholar] [CrossRef]
- Mueller, A.; Beach, S.R.; Bowers, B.J.; Fields, B. Relationship between Health Care Interactions and Care Partner Burden. Fam. Syst. Health 2022, 40, 225–231. [Google Scholar] [CrossRef]
- Fowler, J.; Blundell, B.; Morrisby, C.; Hendrick, A. ‘You’ve Got No Support’: The Experiences of Older Male Caregivers When Their Partner Enters Residential Care. J. Gerontol. Soc. Work. 2022, 65, 529–544. [Google Scholar] [CrossRef]
- Crawford, K.; Digby, R.; Bloomer, M.; Tan, H.; Williams, A. Transitioning from Caregiver to Visitor in a Long-Term Care Facility: The Experience of Caregivers of People with Dementia. Aging Ment. Health 2015, 19, 739–746. [Google Scholar] [CrossRef]
- Street, D.; Burge, S.; Quadagno, J.; Barrett, A. The Salience of Social Relationships for Resident Well-Being in Assisted Living. J. Gerontol. Ser. B 2007, 62, S129–S134. [Google Scholar] [CrossRef] [PubMed]
- Double Robotics. Double 3. The Future of Work Is Hybrid. Available online: https://www.doublerobotics.com (accessed on 10 March 2025).
- Zamir, S.; Hennessy, C.H.; Taylor, A.H.; Jones, R.B. Video-Calls to Reduce Loneliness and Social Isolation within Care Environments for Older People: An Implementation Study Using Collaborative Action Research. BMC Geriatr. 2018, 18, 62. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.H.; Yee, A.; Stamatopoulos, V. Poor and Lost Connections: Essential Family Caregivers’ Experiences Using Technology with Family Living in Long-Term Care Homes during COVID-19. J. Appl. Gerontol. 2022, 41, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Hung, L.; Hu, G.; Wong, J.; Ren, H.; Ahmed, N.; Hussein, A.; Young, E.; Berndt, A.; Mann, J.; Corepal, R.; et al. Telepresence Robots in Long-Term Care Settings in British Columbia During the COVID-19 Pandemic: Analyzing the Experiences of Residents and Family Members. Gerontol. Geriatr. Med. 2023, 9, 233372142311662. [Google Scholar] [CrossRef]
- Yen, H.-Y.; Huang, C.W.; Chiu, H.-L.; Jin, G. The Effect of Social Robots on Depression and Loneliness for Older Residents in Long-Term Care Facilities: A Meta-Analysis of Randomized Controlled Trials. J. Am. Med. Dir. Assoc. 2024, 25, 104979. [Google Scholar] [CrossRef]
- Hung, L.; Zhao, Y.; Alfares, H.; Shafiekhani, P. Ethical Considerations in the Use of Social Robots for Supporting Mental Health and Wellbeing in Older Adults in Long-Term Care. Front. Robot. AI 2025, 12. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, C.; Xiang, X.; An, R. AI Applications to Reduce Loneliness Among Older Adults: A Systematic Review of Effectiveness and Technologies. Healthcare 2025, 13, 446. [Google Scholar] [CrossRef]
- Albarqi, M.N. Exploring the Effectiveness of Technology-Assisted Interventions for Promoting Independence in Elderly Patients: A Systematic Review. Healthcare 2024, 12, 2105. [Google Scholar] [CrossRef]
- Hu, G.; Wong, J.; Ren, L.H.; Kleiss, S.; Berndt, A.; Wong, L.; Hussein, A.; Ahmed, N.; Mann, J.; Hung, L. Care Partner Experience with Telepresence Robots in Long-Term Care during COVID-19 Pandemic. Digit. Health 2025, 11, 20552076251319820. [Google Scholar] [CrossRef]
- Niemelä, M.; van Aerschot, L.; Tammela, A.; Aaltonen, I.; Lammi, H. Towards Ethical Guidelines of Using Telepresence Robots in Residential Care. Int. J. Soc. Robot. 2021, 13, 431–439. [Google Scholar] [CrossRef]
- Moyle, W.; Jones, C.; Cooke, M.; O’Dwyer, S.; Sung, B.; Drummond, S. Connecting the Person with Dementia and Family: A Feasibility Study of a Telepresence Robot. BMC Geriatr. 2014, 14, 7. [Google Scholar] [CrossRef] [PubMed]
- Teddlie, C.; Tashakkori, A. Foundations of Mixed Methods Research: Integrating Quantitative and Qualitative Approaches in the Social and Behavioral Sciences; Sage: Los Angeles, CA, USA, 2009. [Google Scholar]
- Hitchcock, J.H.; Onwuegbuzie, A.J. The Routledge Handbook for Advancing Integration in Mixed Methods Research; Routledge: London, UK, 2022; ISBN 9780429432828. [Google Scholar]
- Ivankova, N.V.; Creswell, J.W.; Plano Clark, V.L. Foundations and Approaches to Mixed Methods Research. In First Steps in Research; Van Schaik Publishers: Pretoria, South Africa, 2016; pp. 305–336. [Google Scholar]
- Shorten, A.; Smith, J. Mixed Methods Research: Expanding the Evidence Base. Evid.-Based Nurs. 2017, 20, 74–75. [Google Scholar] [CrossRef] [PubMed]
- Creswell, J.W.; Creswell, J.D. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 5th ed.; SAGE Publications: Newbury Park, CA, USA, 2018. [Google Scholar]
- Bédard, M.; Molloy, D.W.; Squire, L.; Dubois, S.; Lever, J.A.; O’Donnell, M. The Zarit Burden Interview. Gerontologist 2001, 41, 652–657. [Google Scholar] [CrossRef] [PubMed]
- De Jong Gierveld, J.; Van Tilburg, T. The De Jong Gierveld Short Scales for Emotional and Social Loneliness: Tested on Data from 7 Countries in the UN Generations and Gender Surveys. Eur. J. Ageing 2010, 7, 121–130. [Google Scholar] [CrossRef]
- Logsdon, R.G.; Gibbons, L.E.; McCurry, S.M.; Teri, L. Assessing Quality of Life in Older Adults With Cognitive Impairment. Biopsychosoc. Sci. Med. 2002, 64, 510–519. [Google Scholar] [CrossRef]
- Olson, K. Essentials of Qualitative Interviewing; Left Coast Press: Walnut Creek, CA, USA, 2011. [Google Scholar]
- Phillippi, J.; Lauderdale, J. A Guide to Field Notes for Qualitative Research: Context and Conversation. Qual. Health Res. 2018, 28, 381–388. [Google Scholar] [CrossRef]
- Els, R.C.; Meyer, H.W. The Influence of Leaders’ Attitudes and Commitment to Quality Management of Training on Organisational Excellence: A Mixed-Methods Study. Hum. Resour. Dev. Int. 2025, 28, 79–109. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Reflecting on Reflexive Thematic Analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving Integration in Mixed Methods Designs—Principles and Practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef]
- Marvardi, M.; Mattioli, P.; Spazzafumo, L.; Mastriforti, R.; Rinaldi, P.; Polidori, M.C.; Cherubini, A.; Quartesan, R.; Bartorelli, L.; Bonaiuto, S.; et al. The Caregiver Burden Inventory in Evaluating the Burden of Caregivers of Elderly Demented Patients: Results from a Multicenter Study. Aging Clin. Exp. Res. 2005, 17, 46–53. [Google Scholar] [CrossRef] [PubMed]
- van der Lee, J.; Bakker, T.J.E.M.; Duivenvoorden, H.J.; Dröes, R.-M. Do Determinants of Burden and Emotional Distress in Dementia Caregivers Change over Time? Aging Ment. Health 2017, 21, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Rinaldi, P.; Spazzafumo, L.; Mastriforti, R.; Mattioli, P.; Marvardi, M.; Polidori, M.C.; Cherubini, A.; Abate, G.; Bartorelli, L.; Bonaiuto, S.; et al. Predictors of High Level of Burden and Distress in Caregivers of Demented Patients: Results of an Italian Multicenter Study. Int. J. Geriatr. Psychiatry 2005, 20, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Vespa, A.; Spatuzzi, R.; Fabbietti, P.; Di Rosa, M.; Bonfigli, A.R.; Corsonello, A.; Gattafoni, P.; Giulietti, M.V. Association between Sense of Loneliness and Quality of Life in Older Adults with Multimorbidity. Int. J. Environ. Res. Public Health 2023, 20, 2615. [Google Scholar] [CrossRef]
- Budak, K.B.; Atefi, G.; Hoel, V.; Laporte Uribe, F.; Meiland, F.; Teupen, S.; Felding, S.A.; Roes, M. Can Technology Impact Loneliness in Dementia? A Scoping Review on the Role of Assistive Technologies in Delivering Psychosocial Interventions in Long-Term Care. Disabil. Rehabil. Assist. Technol. 2023, 18, 1107–1119. [Google Scholar] [CrossRef]
- Robinson, H.; MacDonald, B.; Kerse, N.; Broadbent, E. The Psychosocial Effects of a Companion Robot: A Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2013, 14, 661–667. [Google Scholar] [CrossRef]
- Moyle, W.; Arnautovska, U.; Ownsworth, T.; Jones, C. Potential of Telepresence Robots to Enhance Social Connectedness in Older Adults with Dementia: An Integrative Review of Feasibility. Int. Psychogeriatr. 2017, 29, 1951–1964. [Google Scholar] [CrossRef]
- Beridze, G.; Ayala, A.; Ribeiro, O.; Fernández-Mayoralas, G.; Rodríguez-Blázquez, C.; Rodríguez-Rodríguez, V.; Rojo-Pérez, F.; Forjaz, M.J.; Calderón-Larrañaga, A. Are Loneliness and Social Isolation Associated with Quality of Life in Older Adults? Insights from Northern and Southern Europe. Int. J. Environ. Res. Public Health 2020, 17, 8637. [Google Scholar] [CrossRef]
- Boehlen, F.H.; Maatouk, I.; Friederich, H.-C.; Schoettker, B.; Brenner, H.; Wild, B. Loneliness as a Gender-Specific Predictor of Physical and Mental Health-Related Quality of Life in Older Adults. Qual. Life Res. 2022, 31, 2023–2033. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- O’cathain, A.; Murphy, E.; Nicholl, J. The Quality of Mixed Methods Studies in Health Services Research. J. Health Serv. Res. Policy 2008, 13, 92–98. [Google Scholar] [CrossRef]



| Pseudonym of LTC Site | Types of Rooms Available | Staff–Resident Ratio | Funding |
|---|---|---|---|
| Jasmine Residence | Individual and Shared Rooms | Day: 1 staff member to 6 residents | Publicly funded |
| Evening: 1 staff member to 20 residents | |||
| Rose Residence | Individual and Shared Rooms | Day: 1 staff member to 6 residents | Publicly funded |
| Evening: 1 staff member to 8 residents | |||
| Night: 1 staff member to 25 residents | |||
| Zinnia Residence | Individual Room | Day: 3 nurses and 4 care aides (7 staff members in total to 19 residents) | Publicly funded |
| Evening: 3 nurses and 3 care aides (6 staff members in total to 19 residents) | |||
| Night: 2 nurses and 2 care aides (4 staff members to 19 residents) | |||
| Tulip Residence | Individual Room | Day: 1 nurse and 2 to 3 care aides for 16 to 17 residents | Non-profit |
| Evening: 1 nurse and 2 to 3 care aides for 16 to 17 residents | |||
| Night: 1 staff member (nurse or care aid) per care neighbourhood (16–27 residents) | |||
| Sunflower Residence | Individual Room | LTC: 1 resident care partner for 5–6 residents | Privately funded, for-profit |
| Quotes | Codes | Themes |
|---|---|---|
| The robot helps with relieving the pressure of driving and commuting. I have two young kids, and it’s hard having the time to drive to him [the resident] with two hours of travelling back and forth. It had been a hard time making time for myself and my kids… and it’s hard to see my dad. The robot visits help save us time for commuting. |
| Reduces Stress and Guilt |
| She [My granddaughter] will ask me where I feel pain. I feel happy to talk to her through the robot. |
| Provides Meaningful Engagement |
| Residents | Families | ||
|---|---|---|---|
| Gender | |||
| Male | 10 (55.6%) | Male | 3 (17.6%) |
| Female | 8 (44.4%) | Female | 14 (82.3%) |
| Age group | |||
| 61–70 years | 1 (5.6%) | 21–40 years | 2 (11.8%) |
| 71–80 years | 5 (27.8%) | 31–50 years | 4 (23.5%) |
| 81- years | 12 (66.7%) | 51–60 years | 4 (23.5%) |
| 61–70 years | 5 (29.4%) | ||
| 71–80 years | 2 (11.8%) | ||
| Ethnicity | |||
| White | 7 (38.9%) | White | 7 (41.2%) |
| Asian | 11 (61.1%) | Asian | 10 (58.8%) |
| Relationships | |||
| Daughter | 11 (64.7%) | ||
| Son | 3 (17.6%) | ||
| Spouse | 1 (5.9%) | ||
| Granddaughter | 1 (5.9%) | ||
| Friend | 1 (5.9%) | ||
| Total | 18 | Total | 17 |
| Time Points | Mean ± SD | ANOVA F(df), p-Value | Post Hoc Comparison (p-Value) | |
|---|---|---|---|---|
| Caregiver Burden | T0 | 21.5 ± 11.09 | F(2) = 7.464, p = 0.008 ** | T0 vs. T1 (p = 0.011) * |
| T1 | 16.5 ± 7.92 | T0 vs. T2 (p = 0.043) * | ||
| T2 | 15.8 ± 7.68 | T1 vs. T2 (p = 1.000) | ||
| Quality of Life | T0 | 29.9 ± 6.93 | F(2) = 4.024, p = 0.027 * | T0 vs. T1 (p = 0.109) |
| T1 | 31.6 ± 6.55 | T0 vs. T2 (p = 0.124) | ||
| T2 | 32.2 ± 7.62 | T1 vs. T2 (p = 1.000) | ||
| Loneliness | T0 | 11.1 ± 3.43 | F(2) = 4.084, p = 0.026 * | T0 vs. T1 (p = 0.120) |
| T1 | 9.9 ± 2.99 | T0 vs. T2 (p = 0.085) | ||
| T2 | 9.8 ± 2.73 | T1 vs. T2 (p = 1.000) |
| Impact on Residents | Impact on Family Caregivers |
|---|---|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, L.; Wong, J.O.Y.; Ren, H.; Zhao, Y.; Fu, J.J.; Mann, J.; Li, L. The Impact of Telepresence Robots on Family Caregivers and Residents in Long-Term Care. Int. J. Environ. Res. Public Health 2025, 22, 713. https://doi.org/10.3390/ijerph22050713
Hung L, Wong JOY, Ren H, Zhao Y, Fu JJ, Mann J, Li L. The Impact of Telepresence Robots on Family Caregivers and Residents in Long-Term Care. International Journal of Environmental Research and Public Health. 2025; 22(5):713. https://doi.org/10.3390/ijerph22050713
Chicago/Turabian StyleHung, Lillian, Joey Oi Yee Wong, Haopu (Lily) Ren, Yong Zhao, Jason Jincheng Fu, Jim Mann, and Lun Li. 2025. "The Impact of Telepresence Robots on Family Caregivers and Residents in Long-Term Care" International Journal of Environmental Research and Public Health 22, no. 5: 713. https://doi.org/10.3390/ijerph22050713
APA StyleHung, L., Wong, J. O. Y., Ren, H., Zhao, Y., Fu, J. J., Mann, J., & Li, L. (2025). The Impact of Telepresence Robots on Family Caregivers and Residents in Long-Term Care. International Journal of Environmental Research and Public Health, 22(5), 713. https://doi.org/10.3390/ijerph22050713







