A Typology of Livable Communities and Older Adults’ Health in the U.S
Abstract
1. Introduction
1.1. Neighborhood Types and Health
1.2. Person–Environment Fit
2. Materials and Methods
2.1. Data Sources
2.2. Sample
2.3. Measures
2.3.1. Livable Community
2.3.2. Self-Rated Health
2.3.3. Covariates
2.4. Data Analysis
3. Results
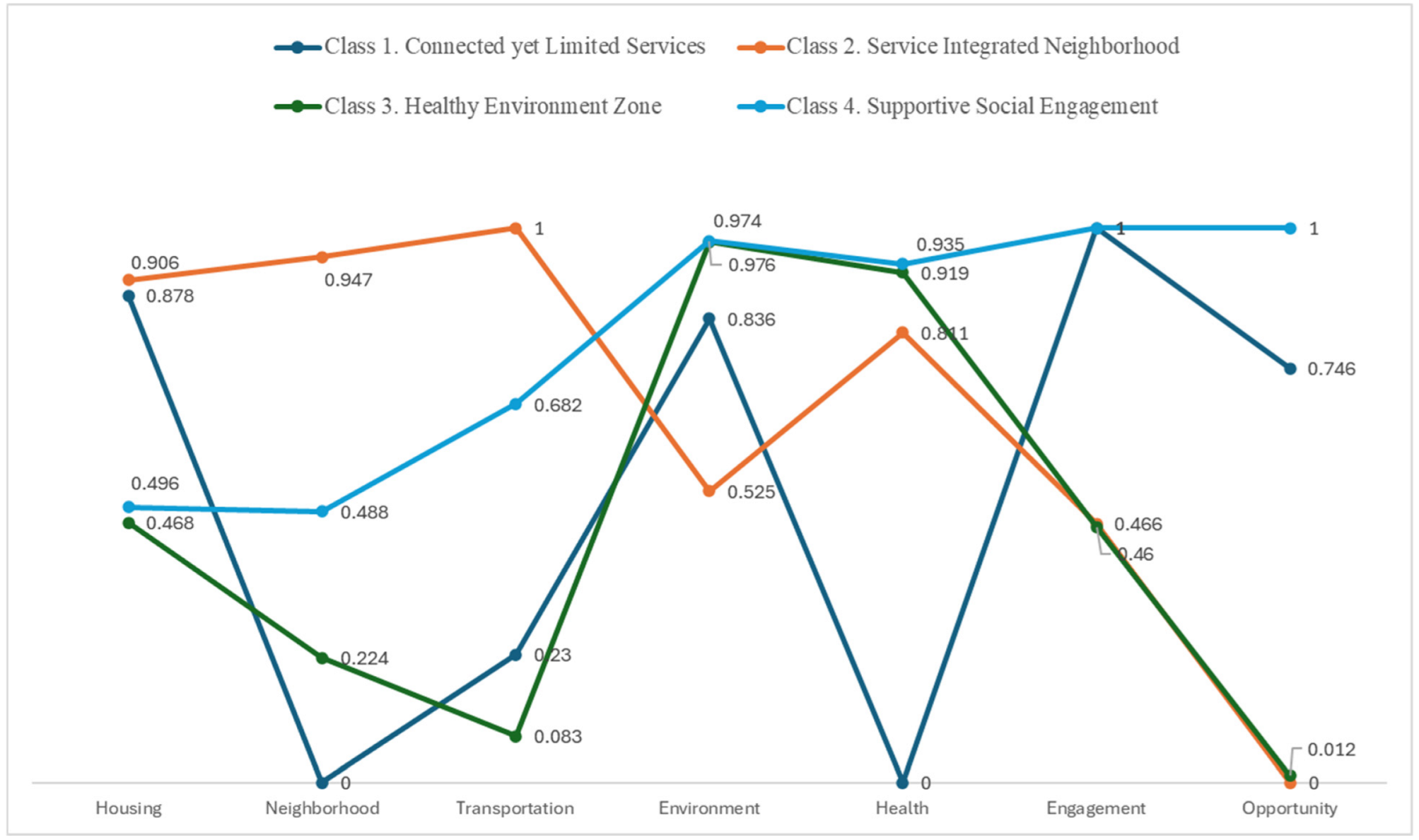
3.1. Livable Neighborhood Types
3.2. Comparison of Background Characteristics According to Livable Neighborhood Types
3.3. Livable Community Type and Health and the Role of Functional Limitations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Krout, J.A.; Wethington, E. Residential Choices and Experiences of Older Adults: Pathways to Life Quality; Springer Publishing Company: New York, NY, USA, 2003. [Google Scholar]
- Saha, S.; Pandit, D. Neighborhood Characteristics and Quality of Life (QoL) of Older Adults: A Qualitative Exploration from the Perspective of Indian Older Adults (Case Study of Kolkata, India). Ageing Int. 2024, 49, 78–111. [Google Scholar] [CrossRef]
- Sapkota, K.P.; Shrestha, A.; Ghimire, S. Neighborhood Environment and Quality of Life of Older Adults in Eastern Nepal: Findings from a Cross-Sectional Study. BMC Geriatr. 2024, 24, 679. [Google Scholar] [CrossRef] [PubMed]
- Hackman, D.A.; Robert, S.A.; Grübel, J.; Weibel, R.; Anagnostou, E.; Hölscher, C.; Schinazi, V. Neighborhood Environments Influence Emotion and Physiological Reactivity. Sci. Rep. 2019, 9, 45876. [Google Scholar] [CrossRef]
- Choi, Y.J. Understanding Aging in Place: Home and Community Features, Perceived Age-Friendliness of Community, and Intention Toward Aging in Place. Gerontologist 2022, 62, 46–55. [Google Scholar] [CrossRef]
- Kim, K.; Buckley, T.; Burnette, D.; Kim, S.; Cho, S. Measurement Indicators of Age-Friendly Communities: Findings from the AARP Age-Friendly Community Survey. Gerontologist 2022, 62, e17–e27. [Google Scholar] [CrossRef]
- Meeks, S. Age-Friendly Communities: Introduction to the Special Issue. Gerontologist 2022, 62, 1–5. [Google Scholar] [CrossRef]
- World Health Organization. The Global Network for Age-Friendly Cities and Communities: Looking Back Over the Last Decade, Looking Forward to the Next; World Health Organization: Geneva, Switzerland, 2018; Available online: https://apps.who.int/iris/bitstream/handle/10665/278979/WHO-FWC-ALC-18.4-eng.pdf?sequence=1&isAllowed=y (accessed on 11 April 2025).
- Van Hoof, J.; Marston, H.R.; Kazak, J.K.; Buffel, T. Ten Questions Concerning Age-Friendly Cities and Communities and the Built Environment. Build. Environ. 2021, 199, 107922. [Google Scholar] [CrossRef]
- Torku, A.; Chan, A.P.C.; Yung, E.H.K. Age-Friendly Cities and Communities: A Review and Future Directions. Ageing Soc. 2021, 41, 2242–2279. [Google Scholar] [CrossRef]
- Chen, B.I.; Hsueh, M.C.; Rutherford, R.; Park, J.H.; Liao, Y. The Associations Between Neighborhood Walkability Attributes and Objectively Measured Physical Activity in Older Adults. PLoS ONE 2019, 14, e0222268. [Google Scholar] [CrossRef]
- Padeiro, M.; de Sao Jose, J.; Amado, C.; Sousa, L.; Roma Oliveira, C.; Esteves, A.; McGarrigle, J. Neighborhood Attributes and Well-Being Among Older Adults in Urban Areas: A Mixed-Methods Systematic Review. Res. Aging 2022, 44, 351–368. [Google Scholar] [CrossRef]
- Elsawahli, H.; Ahmad, F.; Ali, A.S. A Qualitative Approach to Understanding the Neighborhood Environmental Influences on Active Aging. J. Des. Built Environ. 2017, 17, 16–26. [Google Scholar] [CrossRef]
- Hawkesworth, S.; Silverwood, R.J.; Armstrong, B.; Pliakas, T.; Nanchalal, K.; Jefferis, B.J.; Lock, K. Investigating Associations Between the Built Environment and Physical Activity Among Older People in 20 UK Towns. J. Epidemiol. Community Health 2018, 72, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.; Yu, R.; Woo, J. Effects of Perceived Neighbourhood Environments on Self-Rated Health Among Community-Dwelling Older Chinese. Int. J. Environ. Res. Public Health 2017, 14, 614. [Google Scholar] [CrossRef]
- Ye, B.; Gao, J.; Fu, H. Associations Between Lifestyle, Physical and Social Environments and Frailty Among Chinese Older People: A Multilevel Analysis. BMC Geriatr. 2018, 18, 98. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Liu, Y.; Cui, C.; Xia, B. Influence of Outdoor Living Environment on Elders’ Quality of Life in Old Residential Communities. Sustainability 2019, 11, 6638. [Google Scholar] [CrossRef]
- Barnett, A.; Zhang, C.J.; Johnston, J.M.; Cerin, E. Relationships Between the Neighborhood Environment and Depression in Older Adults: A Systematic Review and Meta-Analysis. Int. Psychogeriatr. 2018, 30, 1153–1176. [Google Scholar] [CrossRef]
- Lowen, T.; Davern, M.T.; Mavoa, S.; Brasher, K. Age-Friendly Cities and Communities: Access to Services for Older People. Aust. Plan. 2015, 52, 255–265. [Google Scholar] [CrossRef]
- Au, A.M.; Chan, S.C.; Yip, H.M.; Kwok, J.Y.; Lai, K.Y.; Leung, K.M.; Lai, S.M. Age-Friendliness and Life Satisfaction of Young-Old and Old-Old in Hong Kong. Curr. Gerontol. Geriatr. Res. 2017, 2017, 1–10. [Google Scholar] [CrossRef]
- Park, S.; Lee, S. Age-Friendly Environments and Life Satisfaction Among South Korean Elders: Person–Environment Fit Perspective. Aging Ment. Health 2017, 21, 693–702. [Google Scholar] [CrossRef]
- Kim, S.; Kim, J.; Kim, K.; Buckley, T. Age-Friendly Environment and Aging in Place: Finding from Latent Profile Analysis. Int. J. Aging Hum. Dev. 2024, 98, 499–514. [Google Scholar] [CrossRef]
- Lawton, M.P.; Nahemow, L. Ecology and the Aging Process. In The Psychology of Adult Development and Aging; Eisdorfer, C., Lawton, M.P., Eds.; American Psychological Association: Washington, DC, USA, 1973; pp. 619–674. [Google Scholar] [CrossRef]
- Binette, J. Livability for All: The AARP Age-Friendly Community Surveys. Available online: https://www.aarp.org/pri/topics/livable-communities/2016-aarp-age-friendly-community-survey/ (accessed on 11 April 2025).
- Binette, J. Livability for All: The AARP 2017 Age-Friendly Community Surveys. Available online: https://www.aarp.org/pri/topics/livable-communities/aarp-2017-age-friendly-community-surveys/ (accessed on 11 April 2025).
- AARP. AARP Livability Index. Available online: https://livabilityindex.aarp.org/ (accessed on 11 April 2025).
- Kim, K.; Buckley, T.D.; Burnette, D.; Huang, J.; Kim, S. Age-Friendly Communities and Older Adults’ Health in the United States. Int. J. Environ. Res. Public Health 2022, 19, 9292. [Google Scholar] [CrossRef] [PubMed]
- Capitanio, M. The Relativity of Livability Rankings Examining the Japanese Case Against the Global Discourse. World 2018, 5, 12–18. [Google Scholar] [CrossRef]
- Mittal, S.; Chadchan, J.; Mishra, S.K. Review of Concepts, Tools and Indices for the Assessment of Urban Quality of Life. Soc. Indic. Res. 2020, 149, 187–214. [Google Scholar] [CrossRef]
- Zhang, X. Linking People’s Mobility and Place Livability: Implications for Rural Communities. Econ. Dev. Q. 2022, 36, 149–159. [Google Scholar] [CrossRef]
- Nylund-Gibson, K.; Choi, A.Y. Ten Frequently Asked Questions About Latent Class Analysis. Transl. Issues Psychol. Sci. 2018, 4, 440–461. [Google Scholar] [CrossRef]
- Nagin, D.S. Group-Based Modeling of Development; Harvard University Press: Cambridge, MA, USA, 2005. [Google Scholar]
- Asparouhov, T.; Muthén, B. Auxiliary Variables in Mixture Modeling: Using the BCH Method in Mplus to Estimate a Distal Outcome Model and an Arbitrary Second Model. Mplus Web Notes: No.21, Version 3. Available online: http://www.statmodel.com/examples/webnotes/webnote21.pdf (accessed on 11 April 2025).
- Bolck, A.; Croon, M.; Hagenaars, J. Estimating Latent Structure Models with Categorical Variables: One-Step Versus Three-Step Estimators. Polit. Anal. 2004, 12, 3–27. [Google Scholar] [CrossRef]
- Vermunt, J.K. Latent Class Modeling with Covariates: Two Improved Three-Step Approaches. Polit. Anal. 2010, 18, 450–469. [Google Scholar] [CrossRef]
- Muthén, L.; Muthén, B. Mplus (Version 8.4) [Computer Software]; Muthén & Muthén: Los Angeles, CA, USA, 2019. [Google Scholar]
- Golant, S.M. Aging in the Right Place; Health Professions Press: Baltimore, MD, USA, 2015. [Google Scholar]
- World Health Organization. Implementing Urban Health Initiative. Available online: https://www.who.int/activities/implementing-the-urban-health-initiative (accessed on 11 April 2025).
- World Health Organization. Urban Health Initiative: A Model Process for Catalyzing Change. Available online: https://www.who.int/initiatives/urban-health-initiative (accessed on 11 April 2025).
- Lehning, A.; Baik, S. Age-Friendly Communities. In Handbook on Aging and Place; Cutchin, M., Rowles, G., Eds.; Edward Elgar: Cheltenham, UK, 2024. [Google Scholar] [CrossRef]
- Buffel, T.; Doran, P.; Goff, M.; Lang, L.; Lewis, C.; Phillipson, C.; Yarker, S. COVID-19 and Inequality: Developing an Age-Friendly Strategy for Recovery in Low Income Communities. Qual. Ageing Older Adults 2020, 21, 271–279. [Google Scholar] [CrossRef]
- Parsons, P.L.; Slattum, P.W.; Bleich, M. Mainstreaming Health and Wellness: The RHWP Innovation Model to Complement Primary Care. Nurs. Forum 2019, 54, 263–269. [Google Scholar] [CrossRef]
- Zanjani, F.; Falls, K.; McQueen Gibson, E.; Patel, K.; Price, E.; Sargent, L.; Slattum, P. Richmond Health and Wellness Program: Community Advisory Council Outcomes. Innov. Aging 2018, 2, 499–500. [Google Scholar] [CrossRef]
- Clark, E.C.; Cranston, E.; Polin, T.; Ndumbe-Eyoh, S.; MacDonald, D.; Betker, C.; Dobbins, M. Structural Interventions That Affect Racial Inequities and Their Impact on Population Health Outcomes: A Systematic Review. BMC Public Health 2022, 22, 2162. [Google Scholar] [CrossRef] [PubMed]
- Black, K.; Oh, P. Assessing Age-Friendly Community Progress: What Have We Learned? Gerontologist 2022, 62, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Coyle, C.E.; Gleason, S.R.; Mutchler, J.E. Spillover Benefits and Achieving Sustainability of Age-Friendly Communities. Gerontologist 2022, 62, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Menec, V.H.; Newall, N.E.; Milgrom, R.; Camps, D. Exploring the Sustainability of Age-Friendly Initiatives in a Canadian Province. Gerontologist 2022, 62, 18–28. [Google Scholar] [CrossRef]
- Lehning, A.J.; Smith, R.J.; Kim, K. “Friendly” Initiatives: An Emerging Approach to Improve Communities for Vulnerable Populations. J. Policy Pract. 2017, 16, 46–58. [Google Scholar] [CrossRef]
| Model | AIC | BIC | Entropy | VLMR-LRT |
|---|---|---|---|---|
| 1 Class | 27,700.110 | 27,742.631 | ||
| 2 Classes | 25,606.081 | 25,697.196 | 0.857 | p < 0.001 |
| 3 Classes | 24,106.180 | 24,245.890 | 0.968 | p < 0.001 |
| 4 Classes | 23,405.456 | 23,593.761 | 0.936 | p < 0.001 |
| 5 Classes | 23,018.036 | 23,254.935 | 0.925 | p < 0.001 |
| Neighborhood Type | ||||||
|---|---|---|---|---|---|---|
| Total (n = 3211) | Connected Yet Limited Services (n = 509) | Service Integrated (n = 897) | Healthy Environment Zone (n = 762) | Supportive Social Engagement (n = 1043) | Statistic | |
| Age | x2 = 18.79 ** | |||||
| 65–74, % | 57.52 | 57.37 | 59.75 | 58.92 | 54.65 | |
| 75–84, % | 27.75 | 29.86 | 28.21 | 26.77 | 27.04 | |
| 85 and older, % | 14.73 | 12.77 | 12.04 | 14.30 | 18.31 | |
| Sex (Female), % | 59.02 | 62.67 | 59.98 | 56.30 | 58.39 | x2 = 5.65 |
| Race/ethnicity | x2 = 216.32 *** | |||||
| White, non-Hispanic, % | 80.69 | 87.65 | 74.83 | 78.37 | 91.78 | |
| Black, non-Hispanic, % | 6.48 | 9.36 | 8.55 | 7.35 | 3.27 | |
| Hispanic, % | 7.63 | 0.60 | 15.24 | 12.52 | 1.78 | |
| Other race, non-Hispanic, % | 2.15 | 2.39 | 1.39 | 1.77 | 3.17 | |
| Education (college), % | 47.24 | 37.03 | 45.21 | 47.38 | 56.78 | x2 = 58.81 *** |
| Income, M | 4.41 | 3.97 | 4.23 | 4.43 | 4.77 | F = 21.77 *** |
| Employment (yes), % | 16.66 | 15.35 | 15.18 | 17.65 | 18.56 | x2 = 5.06 |
| Own home (yes), % | 82.75 | 88.17 | 77.79 | 86.45 | 82.55 | x2 = 33.42 *** |
| Living with spouse/partner, % | 49.08 | 47.91 | 49.55 | 49.80 | 50.78 | x2 = 1.13 |
| Five years in community (yes), % | 93.09 | 93.91 | 93.98 | 90.55 | 93.77 | x2 = 10.01 * |
| Social interaction, M | 5.06 | 5.10 | 5.05 | 5.04 | 5.08 | F = 0.39 |
| Physical limitation (yes), % | 28.99 | 35.50 | 29.12 | 29.55 | 26.63 | x2 = 12.94 ** |
| Caregiver (yes) | 15.01 | 15.38 | 15.46 | 16.13 | 14.19 | x2 = 1.38 |
| Estimate | S.E. | |
|---|---|---|
| Age 85 and older (ref) | ||
| 65–74 | −0.19 *** | 0.05 |
| 75–84 | −0.22 *** | 0.06 |
| Sex (Female) | 0.04 | 0.04 |
| Race/ethnicity | ||
| White (ref) | - | |
| Black | −0.22 ** | 0.07 |
| Hispanic | −0.15 * | 0.07 |
| Other race | −0.14 | 0.13 |
| Education (college) | 0.14 *** | 0.04 |
| Income | 0.07 *** | 0.01 |
| Employment (yes) | 0.20 *** | 0.05 |
| Own home (yes) | 0.12 * | 0.05 |
| Living with spouse/partner | −0.12 ** | 0.04 |
| Five years in community (yes) | −0.09 | 0.07 |
| Social interaction | 0.06 *** | 0.01 |
| Physical limitation (yes) | −0.95 *** | 0.04 |
| Caregiver (yes) | 0.02 | 0.05 |
| Neighborhood type | ||
| Connected yet limited services | −0.21 *** | 0.06 |
| Service integrated | −0.16 *** | 0.05 |
| Healthy environment zone | −0.05 | 0.05 |
| Supportive social engagement (ref) | - | - |
| No Functional Limitations (n = 2232) | Functional Limitations (n = 931) | |||
|---|---|---|---|---|
| Estimate | S.E. | Estimate | S.E. | |
| Connected yet limited services | −0.13 | 0.07 | −0.36 ** | 0.10 |
| Service integrated | −0.10 | 0.05 | −0.33 *** | 0.09 |
| Healthy environment zone | −0.01 | 0.05 | −0.09 | 0.10 |
| Supportive social engagement (ref) | - | - | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.; Burnette, D.; Baik, S.; Kim, S. A Typology of Livable Communities and Older Adults’ Health in the U.S. Int. J. Environ. Res. Public Health 2025, 22, 676. https://doi.org/10.3390/ijerph22050676
Kim K, Burnette D, Baik S, Kim S. A Typology of Livable Communities and Older Adults’ Health in the U.S. International Journal of Environmental Research and Public Health. 2025; 22(5):676. https://doi.org/10.3390/ijerph22050676
Chicago/Turabian StyleKim, Kyeongmo, Denise Burnette, Sol Baik, and Seon Kim. 2025. "A Typology of Livable Communities and Older Adults’ Health in the U.S" International Journal of Environmental Research and Public Health 22, no. 5: 676. https://doi.org/10.3390/ijerph22050676
APA StyleKim, K., Burnette, D., Baik, S., & Kim, S. (2025). A Typology of Livable Communities and Older Adults’ Health in the U.S. International Journal of Environmental Research and Public Health, 22(5), 676. https://doi.org/10.3390/ijerph22050676






