2.2. Child Intake Information
Victoria was admitted to a child mental health care centre because of behavioural difficulties. Since the age of 2, she has shown a lot of anger, especially when things go differently than she expects or wants. Every step of the daily routine (e.g., dressing, eating, etc.) is a struggle and a source of conflict. She has tantrums several times per week to several times per day, tends to express sadness as anger and stays angry for a long time. Victoria shows a lot of controlling behaviour, for example, by demanding the exact way her mother should hold her hand, the pace at which she should walk (not too slow and not too fast) and the way she should braid her hair (not too high and not too low). If such conditions are not met, she does not cooperate and, for example, will not go to school. If she thinks her mother did something wrong, she requests that she say sorry several times.
When she gets angry, she tends to hurt Alexander, Anastasia, and her mother, after which she does not seem to show any feelings of guilt. At the age of 5, she bit her mother so hard that her mother still has scars. Victoria tends to threaten when she becomes angry or when she wants something, such as to stab or cut someone while actually holding a knife. In the car, Alexander tends to hold Victoria’s hands to keep her from hitting him or the infant. Also, in contact with other children, Victoria tends to hit or bite when things do not go her way, causing her parents to avoid inviting other children into their home.
When Victoria was almost 2 years old, her mother brought her to a nanny when she had to work. She resisted this fiercely by kicking, screaming and not allowing her mother to dress her. As a toddler, she preferred certain sets of clothes, refusing to wear other clothes if the preferred clothes were washed. She could not wait a while and currently still demands an immediate response.
When Victoria suffers from stress, she shows tics (squinting her eyes and blinking one eye a lot). When she is not angry, her mood is usually neutral to positive, and in those moments, she is kind to the infant. Victoria’s hobby is dancing, which she is good at. She says she also likes to play and swing, although she finds it hard to play by herself.
During the intake, Victoria was shy around the psychologist. She made eye contact and reacted non-verbally. The infant was also present at the intake; she played and sat with the mother. During the intake, Victoria sometimes went to the mother to give her a hug.
The parents feel strongly about the parenting style they employ, and they requested a therapist who would respect the choices they make in parenting. They also did not want Victoria to receive a diagnostic classification or individual therapy. Because of this wish, a BOAM trajectory was indicated instead of regular assessment at the mental health care centre followed by treatment. The BOAM trajectory is not offered by the intake psychologist but by another therapist (DT). Meanwhile, the child psychologist who conducted the intake stayed available for anything that might be additionally required during the BOAM trajectory. The BOAM trajectory started after three weeks and consisted of an introductory session, seven sessions on a 2-weekly basis, an evaluation session, a follow-up session, and an evaluation with the intake psychologist.
2.3. BOAM Trajectory
2.3.1. Introductory Session: Meeting the BOAM Therapist (Both Parents, Week 4)
The goal of this meeting was for the parents to become acquainted with the BOAM therapist and to answer the question of whether the parents indeed wanted to start with the BOAM trajectory together with Victoria. The mother talked about the problems that she has encountered with Victoria. She said Alexander protests the unequal treatment he receives compared to his sister. She hopes to obtain tools to reduce his protest and seems to unconsciously assume that the large treatment difference cannot be reduced because it is impossible to improve Victoria’s functioning. Alexander seems to receive and take on much responsibility regarding the monitoring and supervision of his sister and co-regulating her emotions. This is not only at home but also at school where they are in the same group. The therapist argued that this seems to play a role in the fact that relatively few problems arise in school. The mother agreed with this assumption and said she was happy about that. The therapist expressed her concern about the burden Alexander is carrying and the impact it may have on him, which seems to be a new perspective for the parents. The therapist also enquired if they have worries about how the behaviour problems may develop in the future, which they said they have not thought about yet. The therapist explained that when they can find the causes for Victoria’s behaviour with the help of BOAM self-diagnostics, it might become possible to change her behaviour through parenting that is more adjusted to her specific needs. When the parents spoke about the problems, their tone and facial expressions remained flat. After the therapist raised the possibility of positively adjusting Victoria’s development, the parents seemed to be more involved and motivated for the BOAM trajectory. The parents indicated that Victoria is not keen on the sessions, and they want to stress her as little as possible. The therapist and parents agreed on the BOAM trajectory and confirmed that part of the sessions would be performed with them as parents and part of the sessions would be performed with Victoria present.
2.3.2. BOAM Session 1: Model 1 (The Whole Family, Week 6)
The parents brought the whole family to the session; they were used to doing activities with the family as a whole and did not realise that the presence of the combination of the three children would distract them from the session. When meeting the therapist, Alexander and Victoria both acted shy and polite. Alexander started playing and sometimes took care of the infant. Victoria did not seem to know what to do. She kept walking to her mother or father, did not answer any questions from the therapist, and looked at her suspiciously. The mother stated aloud that it is important for all of them to accept that Victoria is ‘ill’ and that this illness cannot be cured. She says she hopes that when this is clear, Alexander and the outside world will stop keeping her responsible for the behaviour of Victoria. The mother explained that other parents—who never found out what was wrong with their child—told her that this had made their burden heavier.
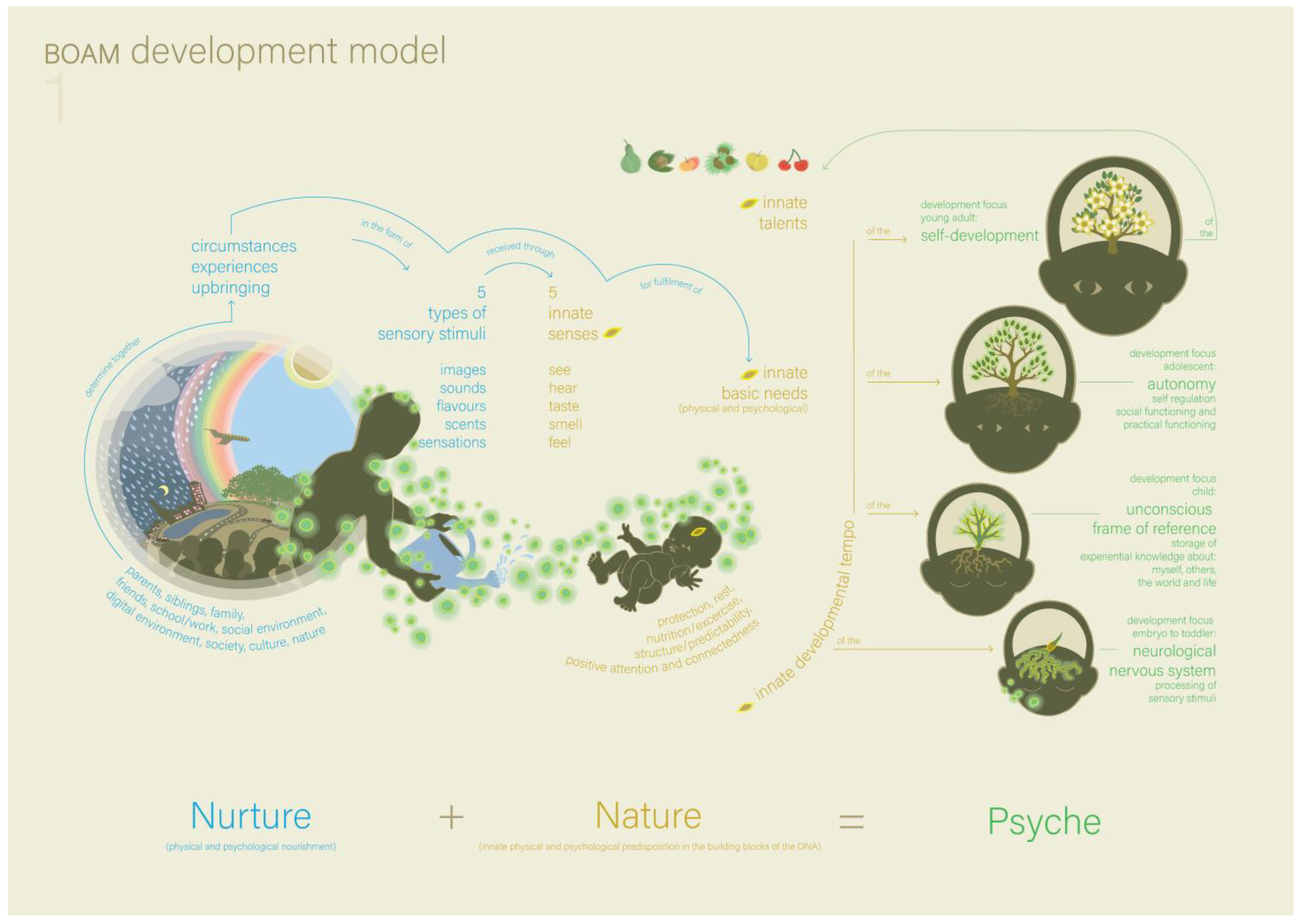
At a certain point, the father started playing with Victoria. Meanwhile, the therapist repeated to the mother that when they are able to find the causes for Victoria’s behaviour, it can become possible to change it by adjusting parenting better to her needs. The therapist gave psychoeducation based on Model 1 (the BOAM developmental model, see
Figure 1) and the explanation of Model 1 (
Box 1).
The most important understanding that comes from this model is that psychological and/or behavioural problems develop if nurture is not adequately attuned to a child’s nature. This understanding changed the mother’s perspective; she realised that they, as parents, may be able to help change Victoria’s behaviour. This stresses the importance of her finding explanations for her behaviour. The therapist expressed some concern about the term ‘illness’ that the mother uses in the presence of Victoria and Alexander. They agreed that only the parents (or the parents and the infant) would come for the next appointment.
Figure 1.
The BOAM Development Model (Model 1) [
16].
Figure 1.
The BOAM Development Model (Model 1) [
16].
Box 1. Model 1: the BOAM Developmental Model (
Figure 1).
Model 1 shows the development of a human psyche that is represented as a growing tree. The tree seed represents the nature of the psyche (innate senses, basic needs, talents and pace of development), and the soil in which it lands represents the nurture of the psyche (parents, family, school, social and digital environment, society, culture). All (positive and negative) nurture consists of experiences composed of sensory stimuli entering the senses. This means that nobody perceives reality directly; instead, our neurological and psychological processes determine how we experience reality. The better nurture is aligned with nature while growing up, the more accurate the unconscious frame of reference (about the self, others, the world and life) can develop, and the better the psychological development can be. Within the tree, the root system represents the neurological nervous system, and the branch system represents the unconscious frame of reference.
2.3.3. BOAM Session 2: Model 2 and 3 (Both Parents and the Infant, Week 8)
Model 2 (the BOAM basic model, see
Figure 2, and the explanation in
Box 2) was explained to the parents. The parents understand the model immediately and also understand that Victoria’s need for order is not fulfilled, which means that she has ‘ordering problems’ that lead to a dysfunctional perception of reality. Both parents recognised the characteristics of ordering problems in their daughter; her need for structure and predictability is much stronger than Alexander’s at the same age. They recognise that Victoria finds it difficult to oversee and understand situations, which undermines her basic security. The father added that, from this perspective, it makes sense that changes always lead to anger and resistance. Model 3 (the BOAM autonomy model, not included in this article, and the explanation in
Box 3) is presented and discussed shortly. From this model, the parents understood that when Victoria’s need for ordering is not fulfilled (for example, because of sensory overload or lack of clarity), she loses her basic safety, is incapable of functional behavioural strategies and loses her self-regulation.
Box 2. Model 2: the BOAM Basic Model (
Figure 2).
Model 2 shows a tree that represents the human psyche and is based on the Pyramid of Maslow. It explains that the human psyche is constantly focused on the fulfilment of four core psychological needs (in hierarchical order: basic needs, order, autonomy, and meaning), of which the starting letters form the acronym BOAM. The basic needs of the psyche (represented by the soil the tree grows in) are protection, rest, nutrition/exercise, structure/predictability, positive attention and connectedness, all of which need to be fulfilled both physically and psychologically to be able to function well. If the basic needs are fulfilled, the next need to be fulfilled is the need for ordering. Ordering is the neuropsychological process by which the continuous flow of sensory stimuli is converted into a perception of reality. This is performed quickly and unconsciously by using the unconscious frame of reference about the self, others, the world and life, which is built up over a lifetime (depicted by the tree trunk and branches). The frame of reference contains not only core beliefs and cultural values but also foundational knowledge about practical and social structures. Because the frame of reference largely determines the perception of reality, it also determines the thoughts and feelings that are a reaction to that perception and thus cause the behaviour. This behaviour influences the new experiential knowledge that is collected, and in this way, this frame of reference is further refined. The more comprehensive the frame of reference is, the faster and better the ordering processes can take place, and new experiences can be understood. When the need for ordering is fulfilled, basic security can be experienced, and the subsequent need for autonomy (depicted by the leaves) arises. Only when the (imperceptible) ordering goes well enough (meaning the perception of reality sufficiently matches (other‘s) reality) can behavioural strategies emerge that lead to (perceptible) autonomy. The core need for autonomy is fulfilled by self-regulating behaviour, such as executive functioning and social abilities, which allow self-organisation of basic needs in practical and social circumstances. After fulfilment of the need for autonomy, the need for meaning arises, which consists of different forms of self-development (depicted by blossom) and, in the case of adults, servitude (depicted by fruits or nuts).
Box 3. Model 3: the BOAM Autonomy Model (not included in this article).
Model 3 zooms in on the middle (two) layers of the BOAM basic model and shows that behaviour strategy arises unconsciously from the perception of reality. New situations are ordered quickly, automatically and unconsciously with the help of the unconscious frame of reference about the self, others, the world and life. This frame of reference is always subjective because it arises from a person‘s unique nature and unique nurture. Therefore, the reality perception that is based on this frame of reference constitutes one‘s personal idea of cause-and-effect in the current circumstances and may be more or less coherent and adequate. A more functional reality perception leads to a more functional behaviour strategy. Depending on the functionality of the behaviour strategy, self-regulation can occur: thoughts, feelings and behaviour can be efficiently directed towards the fulfilment of the basic needs or need for Meaning. Functional behaviour consists of 12 core psychological functions including, for example, concentration, taking initiative, flexibility and bounding. These functions can be deployed both practically and socially.
Both parents had already assumed that Victoria was ‘unable’ and not ‘unwilling’, and after discussing the models, they seemed relieved that these models confirmed this assumption. The parents had translated this understanding into their parenting practices by not punishing Victoria and not becoming angry with her. The therapist complimented the parents for this, which seemed important for them. They visibly relaxed more. The mother shared more about the difficulties that arise (not being able to work when her daughter is present and her own fatigue). The father has fewer obligations when he is at home with the children and copes by playing with Victoria a lot and by taking her out for something else to eat when she does not want what has been cooked. Because the first sessions were still focused on gaining insights, new ways of dealing with Victoria’s behaviour were not discussed. The main hypothesis arising from this session is that she suffers from ‘ordering problems’ that negatively influence her self-regulation.
In the next session, Victoria would be present again. The therapist explained to the parents that she could play or draw during the sessions but not read or use digital devices so she could hear what was being discussed and may choose to react. The homework assignment was for the parents to analyse difficult situations with the help of Models 1 to 3.
2.3.4. BOAM Session 3: Models 4 and 5 (Both Parents, Victoria and the Infant, Week 10)
At the beginning of the session, Victoria was drawing. The therapist only asked some light-hearted and ‘closed’ short questions, to which she nodded yes or shook no. Victoria did talk to her parents in their own language. If the therapist showed, in a funny way, that she did not understand what was being said and told them that she was very curious about what they said, Victoria laughed and looked triumphant. The therapist reassured Victoria that she would only talk with the parents today, after which Victoria seemed to relax.
The parents told the therapist that, based on the hypothesis they formed in the last session, they tried to make situations more structured and predictable for Victoria. They saw a positive effect; Victoria seemed to listen better to her parents. The parents and therapist applied the models to a few recent situations in which difficulties occurred in order to analyse and better understand the cause of these difficulties. The new models they used were Model 4 (the BOAM Disturbance Model, see
Figure 3, and the explanation in
Box 4), and Model 5 (the BOAM Effect Model, see
Figure 4 and the explanation in
Box 5).
Figure 3.
The BOAM Disturbance Model (Model 4) [
16].
Figure 3.
The BOAM Disturbance Model (Model 4) [
16].
Box 4. The BOAM Disturbance Model (
Figure 3).
Model 4 shows the four different categories of circumstances in which nurture is not adequately attuned to a child’s nature, which disrupts basic safety and the development of a functional frame of reference. The categories are depicted as different distortions in the ground in which the tree grows, such as too much fertiliser, stones and holes in the soil. Category 1 is called overdemanding and is quite common in the 21st century. The experiences of a child are not negative per se, but (1) the experiences can be too overstimulating for the nervous system, (2) there may be too many experiences in a (too) short amount of time for the ordering processes, and/or (3) there can be too much pressure on development and performance. Category 2 is called neglect, which can be physical and/or emotional and relates to one or more basic needs. A special form of neglect occurs in the case of spoiling (material, practical, emotional or digital), with the consequence that the basic need for life experience is insufficiently fulfilled. Spoiling is often an intuitive parental response to an overdemanding child, with the intention of protecting them from too many psychological failure experiences. Category 3 is called trauma, which can be physical and/or emotional, accidental or through intentional perpetration. Trauma can have a singular or multiple-complex effect on the unconscious core beliefs and experiential knowledge in the frame of reference. Category 4 is called indirect trauma, which arises because of a secret, taboo or psychological problem in the parenting system. When dysfunctional adult behaviour is not directed at the child, no direct trauma occurs; however, indirect trauma can occur due to a lack of ‘emotional predictability’.
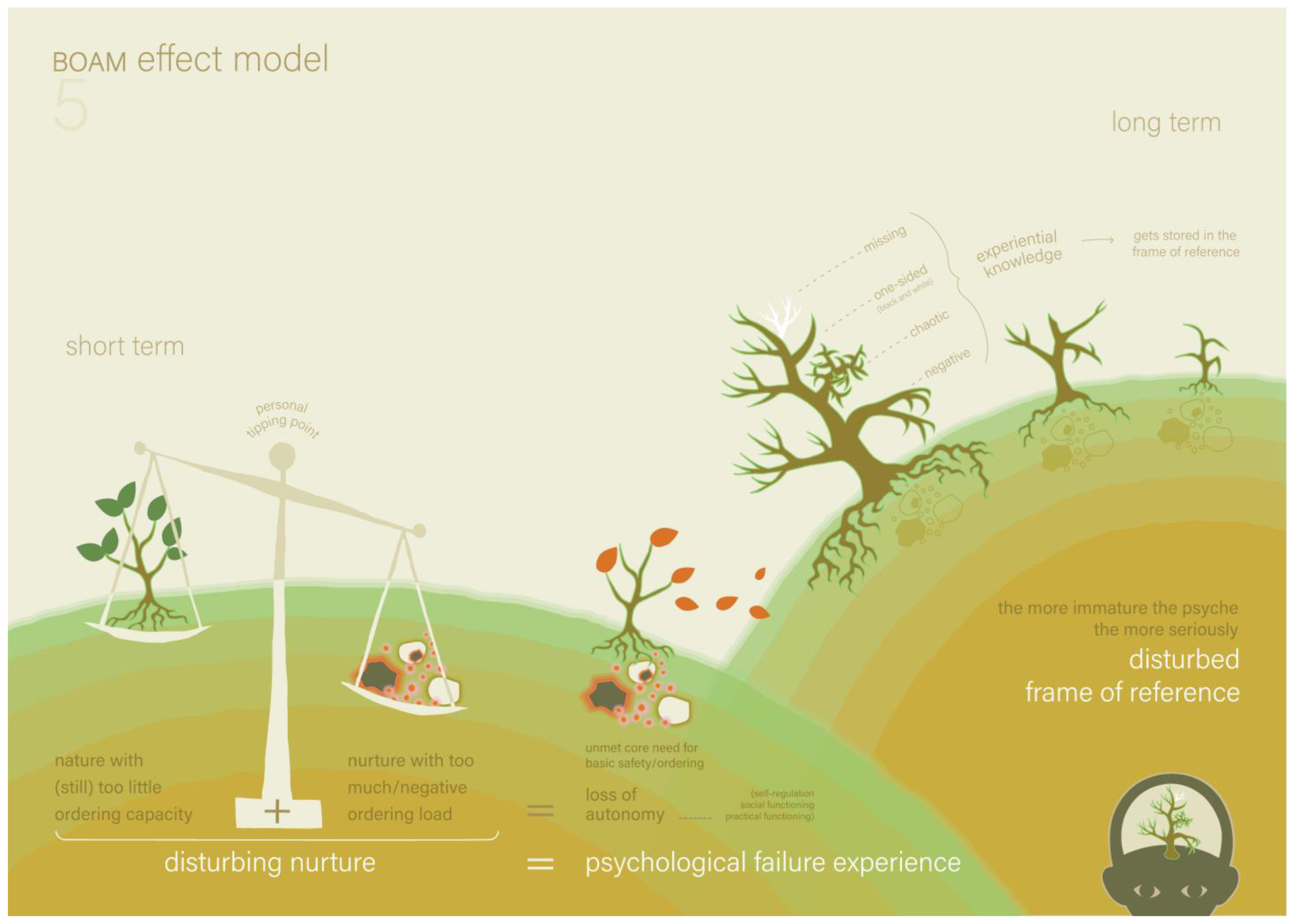
Figure 4.
The BOAM Effect Model (Model 5) [
16].
Figure 4.
The BOAM Effect Model (Model 5) [
16].
Box 5. The BOAM Effect Model (
Figure 4).
Model 5 shows the short- and long-term consequences of all four categories of disturbances. The short-term consequence is depicted as an unbalanced weighing scale and a tree that loses its leaves as a result. This means that if the ‘ordering load’ of a certain situation (nurture) is too large, too negative or both, compared to the actual state of the nervous system and frame of reference (nature), the child noticeably loses autonomy. This means the loss of self-regulation and of the 12 core psychological functions (practically or socially), and this is called a psychological failure experience. Based on the BOAM basic model, this was caused by the unnoticeable loss of the ordering and basic safety. Depending on the ordering capacity, a person has a personal ‘tipping point’ at which circumstances are too overdemanding or too negative to process. The long-term consequence of too many or too severe psychological failure experiences causes the unconscious frame of reference not to develop properly. As a result, the required experiential knowledge in the frame of reference may become missing, one-sided (black and white), chaotic or negative.
One of the situations that were analysed was a dinner in which Victoria refused to eat what her mother cooked, even though it was a meal that she usually eats. After taking one bite, she said it did not taste good, became angry and refused to eat. Her father thought that she genuinely had trouble eating during those times. Because it is important that she eats enough, he takes her to the gas station, where she gets a sausage sandwich that she likes. The parents said that Victoria could be very sensitive to changes in her food: small changes in the taste, texture or colour can lead to her refusing to eat. The therapist pointed to ‘Overdemanding’ in Model 4 and said that this might be the cause of this behaviour. If a child is chronically over-stimulated neurologically, the sensations of eating can be overwhelming. The parents recognised that Victoria seemed to be overstimulated a lot and that any change in a situation, such as the eating situation, could be the last drop to make the bucket overflow. In this eating situation, overdemanding is clearly present at the bottom layer of the BOAM basic model, namely through overstimulation of the neurological system. In other situations, the parents also clearly recognised the overdemanding on the second layer of the BOAM basic model because practical changes or rapid social interactions overload her ordering processes. On the third layer of the BOAM basic model, parents recognised that her autonomy is over-demanded in certain tasks that she should be able to do given her age, such as choosing her clothes, dressing herself, or when she depends on Alexander to make contact. With model 5, they came to the conclusion that it was the imbalance in ordering load and ordering capacity that caused her frequent loss of self-regulation. The parents recognised that her ordering load was chronically quite high in the busy family, the school type without fixed structures, and the fast-paced society. They believe she experiences a combination of sensory overload and an excess of information, as well as quick changes and choices. Model 4 was then used again to assess whether other disturbances (neglect, trauma or indirect trauma) also play a role. The parents did not recognise trauma but recognised a specific form of neglect, namely spoiling, in reaction to the loss of self-regulation of Victoria. They tended to follow her in her own solutions to the problems she experienced, even if these solutions were not healthy, instructive or fair to Alexander (who did have to follow certain parenting rules). They realised that this hinders Victoria in learning to deal with situations in which she ‘does not get what she wants’, and this added dysfunctional experiential information to her frame of reference (namely that it works to have tantrums when you want something). The therapist explained that a sequence of pictograms could provide her basic need for structure and predictability and support Victoria in her ordering processes of practical and social situations.
The parents felt that ‘ordering problems’ was not a hypothesis anymore but an appropriate, explanatory diagnosis of their daughter’s behaviour problems. Also, in this session, they specified it as ‘overdemanding-related ordering problems’, which are related to several environmental factors, such as a school without fixed structures. They add spoiling as being a parenting response that worsens these problems, which arose from the powerlessness they have experienced so far, to guide her with her problems in a better way.
Victoria herself played a minor role in this session because her parents had not announced to her that she could not use a digital device during the session; they had already agreed that she could watch videos, and she had already counted on that. Given her difficulties with sudden changes, the therapist decided not to intervene but repeated her request for the next appointment. The homework assignment that was given to the parents for the next time was to make a list of (specific) family rules. The parents were now motivated to do this, while earlier, they associated rules with punishments, which they did not want to use in their parenting.
2.3.5. BOAM Session 4: Model 6 and 8 (Both Parents, Victoria and the Infant, Week 12)
This time, the mother told Victoria beforehand that she could not watch videos. Victoria’s mood seemed positive, and she was less shy than last time. The mother stated that she and her husband had a long discussion about the necessity of these rules, and for the first time, she felt that they were on the same page. She said that the number of incidents with Victoria had decreased by half since then. When the infant asked for attention, the mother asked the father to sit with her in the waiting room.
The therapist and the mother looked at the homework while Victoria played. They specifically looked at the rules regarding the meals. Even though the subject was something Victoria did not like (eating regular meals), she seemed positively interested in the structuring of the rules. Sometimes, she reacted to the rules that the mother and therapist were establishing, and her ideas were then integrated. When the mother gave examples of difficulties that occur, the therapist checked with Victoria: ‘I think that you could not understand that your mother wants you to eat vegetables because she knows that is needed to keep your body fit for dancing?’ Victoria nodded in concentration. The therapist pointed at the BOAM basic model and checked, ‘I think that it is not predictable for you how many vegetables you must eat per day for that?’ Victoria nodded. The therapist pointed to the BOAM Effect Model and checked, ‘I think that is the reason why your scales tip the wrong way and you fall out of your tree and feel panic?’ Victoria nodded again. ‘I think you would like your mother to tell you how many spoons of vegetables are exactly needed for a fit body?’ She nodded again. Together, the mother and Victoria started a list of vegetables that were not too difficult for Victoria to eat and put how many spoonfuls she should eat at dinner. The therapist suggested that they elaborate on this at home.
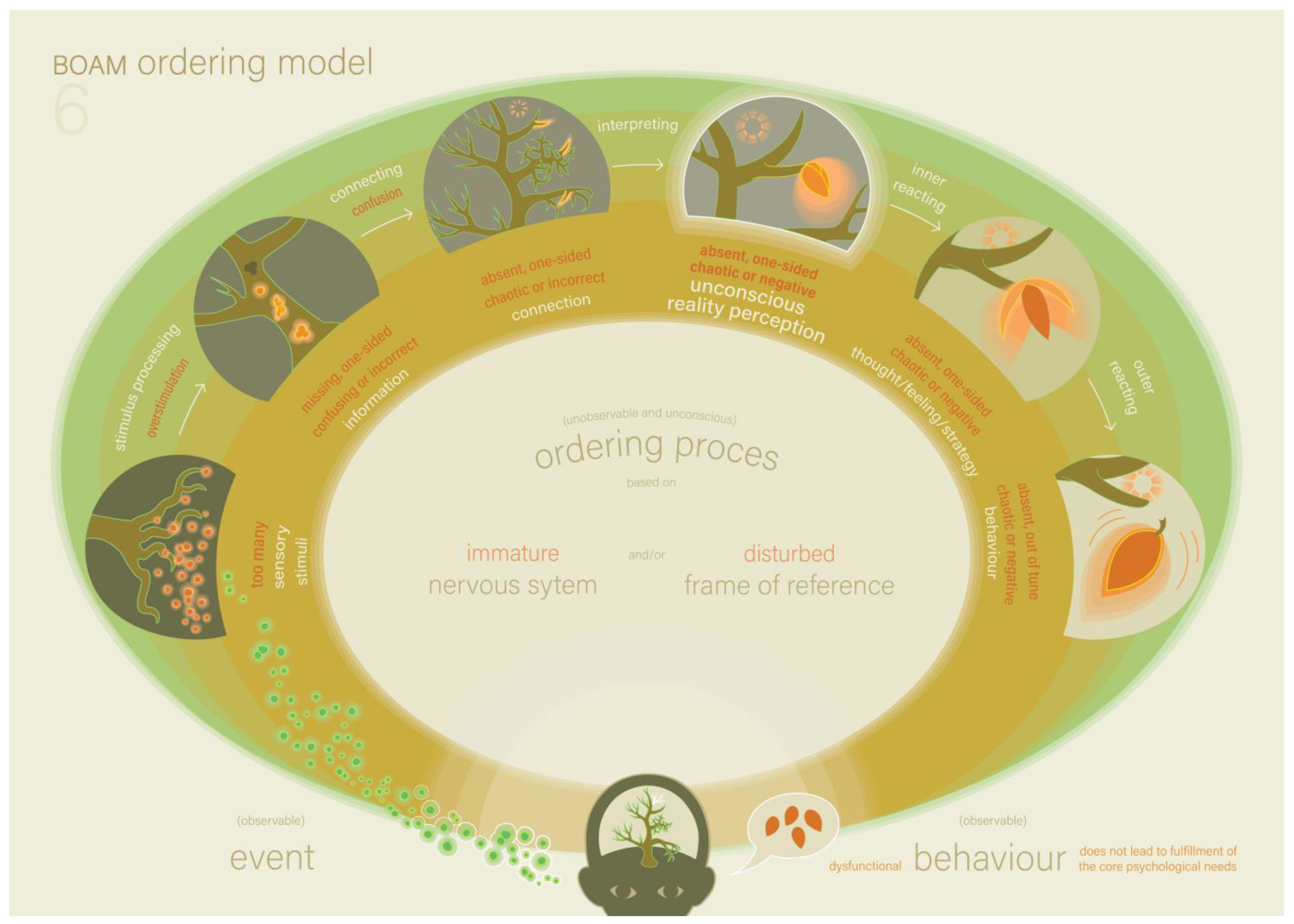
On the initiative of the therapist, the father and the infant joined again so the father could attend the explanation of the following models. The father was happy because he wanted to discuss an incident that took place last week. He and Victoria had to buy sneakers for the school sports class. Victoria preferred a different kind of shoes. However, these shoes were not suitable for sports, and the father bought the sneakers. Outside the shop, she had a tantrum. She continued to sit on the roadway of the parking lot and refused to get into the car until the father bought her the preferred shoes. The father concluded that this was not due to overstimulation because, in that case, she would have been motivated to get in the car and go home. The therapist complimented him on this good analysis and picked up Model 6, the BOAM Ordering Model (see
Figure 5 an the explanation in
Box 6).
The therapist pointed at the steps of the ordering process and explained what functional and dysfunctional steps in the ordering process might look like. The first step was sensory information processing. In this step, too many stimuli may lead to overstimulation instead of accurate information. The therapist asked the family whether the family recognises this, for example, Victoria becoming overstimulated when she is at a party or at the playground. The parents confirmed this and gave an example, while Victoria listened attentively to this and seemed content. The next step in the ordering process was to make a connection between the new information and the frame of reference. If this connection is not possible because the experiential knowledge required for this is lacking in the frame of reference, this may lead to confusion. The parents recognised that this happens with Victoria if the incoming information is not specific enough or not timely enough, which happens easily in a hectic family. They reminded Victoria of a situation where they had specifically told her about a change in schedule and in which she was still confused when the situation occurred. Victoria affirmed in her own language. Lastly, the therapist explained that if a connection is made between the information and the frame of reference, this may lead to a dysfunctional reality perception if the experiential knowledge (that is unconsciously stored therein) is one-sided, chaotic or negative. The shop situation seems to be an example of problems with this last step in the ordering process. The therapist asked whether Victoria was normally allowed to choose the shoes she liked. This was indeed the case. The therapist suggested that Victoria connected the information ‘I am going to buy shoes’ to the stored information in her frame of reference: ‘when buying shoes in a shop, I can pick the shoes I like’, and thus had a perception of reality that missed the nuance that this time, she could only choose sneakers because they were meant for sports class. The parents confirmed that this indeed might have been the case. The therapist pointed out that the behaviour stemming from overstimulation, confusion or a dysfunctional reality perception is never from unwillingness but from inability.
Figure 5.
The BOAM Ordering Model (Model 6) [
16].
Figure 5.
The BOAM Ordering Model (Model 6) [
16].
Box 6. The BOAM Ordering Model (
Figure 5).
Model 6 shows the ordering process step-by-step and illustrates both functional and dysfunctional ordering at every step. Over-stimulation can occur instead of sensory information processing. This happens when the neurological nervous system becomes overstimulated due to an excess of stimuli. Confusion can occur instead of reality perception. This happens when the person cannot connect new information because the necessary experiential knowledge to do so is not available in the frame of reference. These problems in the first two steps of the ordering process are quite easy to spot because the person does not arrive at a reality perception, causing a lack of basic safety. Problems in the next steps of the ordering process are less easy to spot because the person does arrive at a reality perception, and thus has a direct experience of basic safety because the core need for ordering is fulfilled. However, if that reality perception does not sufficiently match (other’s) reality, the behaviour strategy based on it will not lead to the desired practical or social goal, and thus indirectly lead to a psychological failure experience. When someone can only link new information to ‘a frame of reference with absent, one-sided, chaotic or negative experiential knowledge and/or negative core beliefs’, this person unconsciously acquires ‘an absent, one-sided, chaotic or negative reality perception’, which will evoke corresponding thoughts and emotions, which then leads to corresponding dysfunctional behaviour.
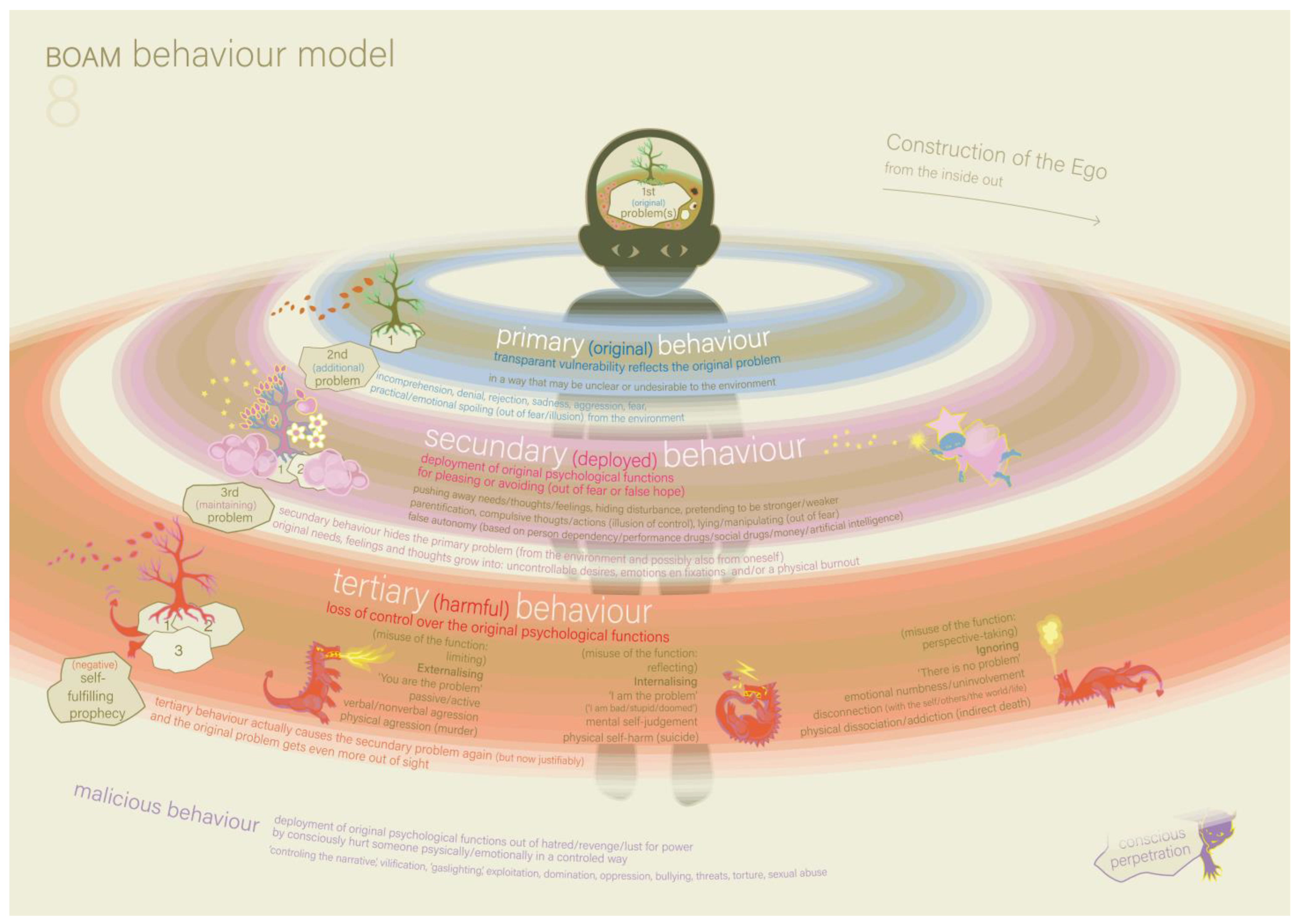
The therapist then took Model 8, the BOAM Behaviour Model, and showed it to the parents (see
Figure 6, and the explanation in
Box 7). Victoria was playing with blocks. The therapist explained that this model might be helpful in understanding the part of the shoe-buying situation in which Victoria had a tantrum in the parking lot. The therapist and the parents reconstructed and analysed this situation with the help of Model 8. The primary problem was the fact that there was an ordering problem because of Overdemanding: Victoria’s perception of reality did not match the reality (of going to the shop to buy sneakers and no other type of shoes). She first tried to convince her father that this was not what she expected to happen (primary behaviour). Her father, not realising something had gone wrong in her ordering process, reacted as if Victoria was unwilling and just whining to get her way (secondary problem). He did not respond and bought the required sneakers. While still in the shop, surrounded by other people, Victoria deployed her self-regulation out of fear of unexpected reactions from unknown people and became very quiet (secondary behaviour). This behaviour made her father think Victoria had accepted the situation. However, when they left the shop and arrived at the parking lot, Victoria’s self-regulation ‘run out’, and she fell prey to externalising (tertiary behaviour). She accused, screamed, demanded, threatened, and refused to step into the car, continuing with this until the father conceded and bought her the desired shoes as an extra pair. By applying the model to this specific incident, the parents now understand how the behaviour problems of Victoria build up in general. Doing this in the presence of the child can result in them experiencing exoneration.
Box 7. Model 8: The BOAM Behaviour Model (
Figure 6).
The BOAM Behaviour Model shows how one’s own behaviour can cause more problems, keeping the original disturbance out of sight and unsolved. There are four forms of human behaviour: original, deployed, harmful and malicious behaviour. The latter does not occur in every human being, but the first three do. In the model, these forms of behaviour are represented by three coloured ‘behaviour circles’ that build up around the human figure, from the inside out and in response to disturbances to ‘survive’ these. The model starts with the primary problem, namely overstimulation, neglect, trauma and/or indirect trauma. Primary behaviour: a child responds to the primary disturbance by natural behaviour that transparently reflects this primary problem. The child signals to the parent that a basic need or the need for ordering is under pressure, which prevents it from experiencing basic safety. Secondary problem: the primary behaviour may be misunderstood or unwanted and causes a dysfunctional or negative reaction in the parents, such as misunderstanding, denial, rejection, fear or aggression. These reactions cause attachment ruptures (that every person suffers to some degree), resulting in a decreased trust within the child that the parents can and will fulfil the basic needs or need for ordering. Spoiling is also a problematic reaction of the parents to the expressed needs of their child. This reaction does not cause attachment ruptures but instead creates dependency and unrealistic self-confidence as the secondary problem. Secondary behaviour: the child will try to behave in a way that parents do understand, expect or desire out of fear or false hope. The child deploys (‘misuses’) self-regulation to deny the authentic needs, feelings, trauma or inability, and instead forces deployed behaviour, such as pleasing, lying, parentification, pretending, etc. Tertiary problem: The consequence of secondary behaviour is that it hides the primary problem, and, at some point, self-regulation will run out. Tertiary behaviour: During the secondary behaviour, the initial needs, thoughts and feelings were being transformed into uncontrollable desires, fixations and emotions. This causes uncontrolled behaviour, which is represented by three dragons that depict externalising behaviour, internalising behaviour and ignoring behaviour (e.g., dissociation or addiction). This behaviour logically induces negative reactions (such as misunderstanding, rejection, aggression or even more spoiling) from the environment, thus repeating the secondary problem, but this time ‘justified’ because of the extreme behaviour. This is called a self-fulfilling prophecy and leads to a vicious circle while the primary problem has gone out of sight. If mental health care is sought, it may be that the focus will be only on the tertiary (and sometimes secondary) behavioural patterns and symptoms, which will never really be resolved for the long term until the primary problem is recognised, acknowledged and addressed.
At the end of this session, the therapist introduced a topic outside the scope of the BOAM trajectory, namely the possibility of a standard diagnostic assessment at the mental health centre. The therapist told the parents that the symptoms and behaviour of some children who have overdemanding-related ordering problems could also be classified with autism spectrum disorder. The therapist explained that when children experience many ordering problems, like children with autism spectrum disorder, they may also act out and externalise or internalise their stress more often than other children. Finally, the therapist explained that a DSM-5 classification can sometimes open doors with regard to finances or special needs possibilities and can give clarity to involved professionals such as a teacher or coach, who may then be more understanding. Before the BOAM trajectory, the parents had made clear that they did not want a DSM classification for Victoria. Now, the parents said that they wanted to think about it.
In this session, the parents and therapist refined the prior diagnosis of overdemanding-related ordering problems by identifying which steps in the ordering process are often problematic for Victoria and how the ordering problems lead to secondary behaviour (trying to behave in a difficult situation by becoming quiet and withdrawing in herself), and that subsequently leads to the tertiary behaviour (shouting, threatening, hurting, etc.).
2.3.6. BOAM Session 5: Models Applied to Parents (Parents and Infant, Week 14)
The mother decided that this time, she did not want to bring Victoria to the session, so the parents and therapist could talk about the collaboration between the parents. The mother said she is frustrated with the father’s parenting. The father was somewhat shocked by the mother’s experience but listened attentively to what she shared. The therapist invited the mother to give a specific example of a situation she feels frustrated about. One example she gave was when she asked the father to take the children upstairs in the evening, which he does, but then goes to play with them instead of performing the evening routine. Then, when the mother comes upstairs, the children are hyperactive and difficult to manage.
As always, the models are on the table, and the mother takes the initiative to understand the father’s behaviour with the help of the models. She suggested that the father may also be suffering from overdemanding-related ordering problems, and the father recognised this. The therapist suggested that the father may need to hear more specific information about what to do (and not just what not to do). Together, they started a structure of the steps that he could take when bringing the children to bed, and the therapist suggested that they elaborate on this at home. The father seemed relieved that his own difficulties were becoming clearer. From this moment, he was more actively involved in the sessions and was asking more questions than before. For the mother’s self-reflection, the therapist suggested model 8. As her primary problem, she recognised that she feels overloaded by family life in combination with work and missing the support of the father in the family. Instead of addressing this problem with him, she tried not to complain and just went ahead with all the tasks (secondary behaviour). She already felt that the father’s behaviour came from inability and not unwillingness and did not know how to address this. However, she noticed that she could not keep this up forever and had already started to lose her self-regulation and act annoyed more often (tertiary behaviour).
In this session, both parents gained more self-knowledge and a better understanding of the other and expressed their confidence that they would be able to apply the models in new situations, also independently at home. The diagnosis was refined again, this time regarding the family system; the father recognised overdemanding related ordering problems also with himself, and the mother recognised signs of being overloaded. The assigned homework was to start using pictograms and a weekly planner.
2.3.7. Session with the Intake Psychologist (Parents, Week 15)
In between the BOAM sessions, the parents had a session with the psychologist, who performed the intake with them to discuss the possibility of a standard diagnostic assessment of Victoria. The mother told the psychologist that things are much better with her at home. Victoria was angry less often and behaved much better now that she experienced more structure and predictability. Alexander was no longer responsible for the regulation of his younger sister. The only situations the mother still finds difficult are with friends because these are more difficult to predict. The father also noticed improvements but still experienced difficult incidents with her and found it difficult to deal with her anger. The psychologist suggested that it may be a good idea to make a step-by-step plan for the father. She stated she would discuss this with the BOAM therapist.
The parents discussed with the psychologist that they changed their minds and wanted a standard diagnostic assessment. They believe that if a specific disorder is classified, this can give more clarity, especially to people around them. They expect that people would understand Victoria’s behaviour better and offer her more structure and predictability. The psychologist confirmed that they would perform the assessments in the alternative week from which the BOAM sessions take place.
2.3.8. BOAM Session 6: Model 10 (Parents and Victoria, Week 18)
For the first time, the mother decided to leave the infant with the babysitter. The intake psychologist announced the plan to create a step-by-step plan for the father to deal with his daughter’s anger. This was a natural occasion to introduce Model 10 (the BOAM Recovery Model), which contains the ‘recovery formula’ (for Model 10, see Potharst et al. [
17], and the explanation in
Box 8).
Box 8. Model 10: The BOAM Recovery Model (not included in this article).
The BOAM Recovery Model shows the ‘recovery formula’ that transforms diagnostic insights into a concrete approach for parents in difficult moments, in which children show tertiary ‘dragon-behaviour’ (externalising, internalising or ignoring) or secondary behaviour (pleasing, avoiding, lying, etc.). With this, they can help solve their child or adolescent’s psychological problems themselves, whether or not therapy is needed for their child in addition. Before showing the three steps parents can take to de-escalate and solve the problem, it shows the attitude with which parents should approach their child. This is a ‘giving focus’ rather than falling back on their own secondary (pleasing, spoiling) or tertiary behaviour (externalising, internalising or ignoring) in response to their child’s behaviour. Step 1, Acknowledge: The parents give the child acknowledgement, not only of their feelings but particularly of the primary and secondary problems on the BOAM Behaviour Model because these were created by the environment. For example, the primary problem may be overdemanding (“I understand that this situation was unpredictable for you”) or trauma (“your father and I have had bad fights in the past, while you were present, and these moments and feelings come back to you when we don’t agree with each other”). Step 2 Release: The parents allow the child to discharge its stress and emotions in a harmless way (and do not try to have a conversation with the child meanwhile or solve the situation for as long as the child is not ready for that step yet). Step 3, Fulfil: The parents say sorry for their dysfunctional response to their child’s behaviour that caused the secondary problem (also in the case of spoiling), and this time, they try to fulfil the actual basic need or need for order that were pressured by the primary problem. In case of overdemanding, this fulfilment may involve protection from too many stimuli, changes or performance pressure and/or providing more structure and predictability. In the case of trauma, fulfilment may involve protection from new risks of traumatic experiences and providing positive attention, reassurance and a restored connectedness.
The mother recognised the steps of the recovery formula; she stated that she had already intuitively taken the steps and might use the steps even more effectively now she saw them on the model. The father stated that he does not think he will be capable of applying the model in difficult moments with tantrums. Both parents agree that preventing difficult moments rather than dealing with them should still be the priority because it proved to make a big difference for Victoria and the family, and there still seems to be room for improvement. During this session, Victoria played by herself, in contrast to the previous sessions.
The family showed the board for the pictograms, and the mother said that Victoria wanted to decide which pictograms were put on the board and which were not. It seemed that Victoria associated the pictograms more with ‘having to do what mummy wants me to’ than with supporting her ordering process. This is unfavourable but seems inevitable because not only does the family need to learn to make more use of structuring, but Victoria also needs to learn that the parents decide on the structure and set limits. The therapist’s reaction proceeds according to the recovery formula: First, she spoke loudly to give the playing Victoria acknowledgement (step 1) for the fact that her parents are becoming increasingly strict and supposed that the structure may also have actually confused her at times. Then, the therapist remained silent to give Victoria room to release her emotions (step 2), which she did by silent nodding. Then, the therapist tried to give fulfilment (step 3) to Victoria’s need for predictability when using the pictograms by explaining to the parents that before making a new structure, they should remind Victoria that the first draft of a structure will never be exactly ‘right’ and definitive, but will always have to be adjusted a few times before it ‘fits’. Victoria listened attentively, seemed to understand this and looked satisfied.
Both parents introduced the subject of the evening routine, which could take hours for Victoria and Alexander. They play a lot in between the different steps of the routine. The mother stated that she thinks that it is hard for the father to be consistent with the children. The therapist suggested removing the toys from the bathroom. The mother said that playing is important for children. The therapist agreed with this in general but gave some nuance by saying that playing is not suitable during every moment of the day, for example, when leaving the house, and that the evening routine will be done much faster without playing. The mother was still in doubt regarding this issue. The homework was to make the evening routine visible for every family member by using pictograms.
2.3.9. BOAM Session 7: Making Routines (Parents and Victoria, Week 20)
As the parents talked more freely about their parenting, the father introduced something that he experienced as difficult in the collaboration with the mother. The mother has her own habits with the children and wants to be flexible with them without considering the time that something takes. The father said that this makes it difficult for him to plan things. What also plays a role in the difficulty with planning is that the mother needs to work when she is with the children. The therapist acknowledges both parents’ situations and perspectives, and they talk about the role of structure and demands of society, school and work.
The parents also revisited the subject, stating that not only Victoria but also the father needs very clear and stepwise instructions. The parents made an evening structure for the actions that the children take in the evening routine, and as a homework assignment for the next appointment, they are asked to make a step-to-step structure for the father’s role in the evening routine with the children. Victoria did not need to come to the next session; the BOAM therapist would have an evaluation with the parents.
2.3.10. BOAM Evaluation (Parents, Week 22)
This was the last session of the BOAM trajectory, in which the therapist and parents evaluated the trajectory with the help of the BOAM models. Both parents stated that because of their understanding of Victoria’s ordering problems and her heightened need for structure and predictability, they have made their family life much more structured and predictable. Victoria seems to experience much more basic safety, and her autonomy (especially her self-regulation) has improved. Tertiary behaviour in the form of aggression and oppositional behaviour has decreased. The mother uses the BOAM recovery formula effectively, but the father said he has problems applying it. For the mother, it seems easier to recognise what went wrong in Victoria’s ordering process when Victoria gets angry, and therefore she can give her the proper acknowledgement that she needs to calm down. Because the father also experiences overdemanding-related ordering problems, it is more difficult for him to empathise with his daughter to understand her limited reality perception. This also makes it difficult for him to predict which situations will challenge her ordering processes and possibly lead to tertiary behaviour, so these moments surprise and overwhelm him. He understands that he should not relapse into his secondary behaviour (pleasing, giving in to Victoria’s demands), but he is not able to apply the recovery formula (acknowledging what Victoria experienced as unpredictable, giving space to her negative feelings, and setting a new structure). For now, the parents agreed that the mother would deal with difficult situations. The follow-up appointment with the BOAM therapist would be in four weeks. During that appointment, the parents and therapist would talk about whether more treatment is needed.
At the end of this BOAM trajectory, Victoria’s full explanatory diagnosis is that “nurture (ordering load) does not match nature (ordering capacity) well enough because of the overdemanding of her neurological system and ordering processes.” This high ordering load is related to several environmental factors: a school without fixed structures, the busy family life, and the fast-paced society she lives in. In moments that the ordering load exceeds her ordering capacity, her autonomy decreases (in particular self-regulation), which increases the number of psychological failure experiences. This is not only a short-term problem but since the frame of reference is built from experiences, it is also unfavourable in the long term because it hinders the development of a functional frame of reference. In an attempt to avoid his daughter’s failure experiences, the father tended to spoil his daughter. This deprived her of essential learning experiences and added dysfunctional experiential information to her frame of reference (namely, that it works to have tantrums when you want something). The father also recognised overdemanding-related ordering problems in himself, which made it more difficult for him to empathise with Victoria’s limited reality perception and her psychological need for structure and predictability. Victoria could hide her ordering problems to some extent with secondary behaviour but oftentimes cannot keep this up and then lapses into non-compliant and aggressive tertiary behaviour. Adding more structure and predictability to her life helps solve her primary problem by improving her ordering processes, thus increasing functional reality perceptions, basic safety and self-regulation, which automatically leads to decreasing her behavioural problems.
2.3.11. Session with the Intake Psychologist (Parents, Week 23)
The intake psychologist conducted the psychological assessment with the parents, during which they also talked about how things were going at home and whether the structures that were made were effective. The mother said that things were already going much better: Victoria was only getting angry two or three times a week instead of two or three times a day. However, Saturday mornings were still difficult because there was no school routine, and the family needed to hurry for Victoria and Alexander’s dance and sports lessons. If the father or Alexander even looked at Victoria or talked to her, she became angry. She gets especially angry if her father says something different than what her mother said or would normally say. The psychologist suggested that the parents hang a large pictogram in the room, which makes clear to all family members that, at this specific (and difficult) moment, only the mother deals with Victoria.
2.3.12. Follow-Up Session with the BOAM Therapist (Parents, Week 26)
The parents shared that they had seen a further improvement in Victoria’s behaviour in the past few weeks. Her self-regulation was still growing, and she did not usually get angry anymore (because her need for order was not fulfilled), even in situations that she experienced as difficult. Her dancing teacher also noted that Victoria was easier to teach now. The mother said that she is capable of dealing with Victoria’s ordering problems and that she has no need for further treatment. She says that the father still found it difficult to implement the new parenting routines sometimes, and the father agreed with this. He would like to have more support with this, which he would ask for at the intake psychologist.
2.3.13. Evaluation with the Intake Psychologist and BOAM Therapist (Parents, Week 30)
The parents were very content with their progress. They now understood the cause of Victoria’s problems well and knew how to solve them. The parents were much more on the same page than before. The mother said that she did not feel happy at all as a mother at the beginning of the trajectory, and she now feels very happy (she went from a 2 to a 9 on a scale from 1 to 10). Because the father still found it difficult to deal with Victoria’s anger, the intake psychologist suggested that parental guidance at home would be a possibility. The parents did not want that because they feared that their parenting philosophy would be questioned. They preferred to continue applying the insights and tips they gained from the BOAM trajectory and see if that was enough. The psychologist would stay in touch with them to see if an additional request for help may arise.
The psychologist and therapist had some worries about the sociocratic school and whether their educational system matches Victoria’s need for structure and predictability. They wondered whether Victoria would be able to show initiative in learning, which is a prerequisite to be offered lessons in this type of education. The parents listened to their worries and said they would speak more about this together.
2.3.14. Period of ‘Finger on the Pulse’ by the Intake Psychologist
The standard diagnostic assessment was finished, and a multidisciplinary meeting was held in which autism spectrum disorder was classified. Because the father was too busy, the psychologist shared this with the mother in week 36. The mother was happy with the diagnosis because it would help them communicate better with the outside world about Victoria’s problems and needs. The mother stated that things were still going well. She had even been able to go away for a weekend with Alexander while Victoria stayed with her father. Victoria was now capable of communicating her own needs. For example, she may ask for 10 min of screen time with a timer when she feels overstimulated. Nine out of 10 difficult situations go well. The mother stated that, for now, the father no longer had a request for more support.
In week 44, the psychologist asked the mother whether the parents were able to read the diagnostic report, whether they had any remarks, and how things were going. The mother replied that she had read the report and agreed with it, and things were still going very well. In week 53, the psychologist saw the parents for the last time. They told her that everything was still going well and that they had no request for further help.
2.4. Measures
Child psychopathology was measured using the Dutch version [
42] of the Child Behaviour Checklist (CBCL) for parents of children aged 6 to 18 years old [
43]. Both parents rated the 113 items on a 3-point Likert scale, ranging from 0 (not true) to 2 (very true or often true). Higher scores indicate higher levels of child psychopathology. Good psychometric properties have been shown for the Dutch version of the CBCL [
42]. An example of an item is ‘Gets in many fights’. The total score and two broadband syndrome scales, internalising and externalising psychopathology, were used for the current study and calculated by adding the relevant items. Scores on these scales range between 0 and 226, 0 and 64, and 0 and 70, and the cut-off point for scores in the clinical range are >49, >14 and >15, respectively. The mother completed the CBCL at waitlist assessment (week 1: right before the intake, 3 weeks before the start of the BOAM trajectory), at the pretest (week 4: right before the start of the BOAM trajectory), at post-test (week 30: at the end of the BOAM trajectory, after the evaluation with the intake psychologist and the BOAM therapist), at 3-month follow-up (week 44: 3 months after the end of the BOAM trajectory), and 5-month follow-up (week 54: 5 months after the end of the BOAM trajectory, at the moment the dossier in the mental health centre closed the dossier). The father only completed the CBCL at baseline and 5-month follow-up assessment. For the calculation of the reliable change index (RCI), a measure for clinically significant change, test–retest reliabilities and standard deviations of the mean scores of a reference group of girls from the Dutch manual were used [
42]. Test–retest reliabilities were ICC = 0.89, 0.83, and 0.87, respectively. The standard deviations were 15.4, 5.4, and 5.0, respectively. On the basis of these values, a difference greater than 11.88, 5.18, and 4.19, respectively, was interpreted as clinically significant (
p < 0.05).
Executive functioning was assessed with the parent-report version of the Dutch version [
44] of the Behaviour Rating Inventory of Executive Function (BRIEF) [
45] for children aged 5 to 18 years old. The mother rated the 75 items on a 3-point Likert scale, ranging from 1 (behaviour is never observed) to 3 (behaviour is often observed) at the pretest, post-test and 3-month follow-up. Higher scores indicate higher levels of problems in executive functioning. Psychometric properties of the Dutch version of the BRIEF were shown to be satisfactory [
44]. An example of an item is: ‘Forgets what he/she was doing’. In the current study, the total scale and the two broadband scales, metacognition and behaviour regulation, were used and were calculated by adding up the relevant items. Scores on these scales range between 72 and 216, 44 and 132, and 28 and 84, and the cut-off points for scores in the clinical range are >160, >100 and >65, respectively. For the calculation of the RCI, the test–retest reliabilities and standard deviations of a reference group of 5- to 8-year-old children from a normative study of the Dutch version of the BRIEF were used [
44]. Test–retest reliabilities were ICC = 0.86, 0.84, and 0.95, respectively. The standard deviations were 22.9, 15.6, and 9.9, respectively. On the basis of these values, a difference greater than 19.93, 14.52, and 8.12, respectively, was interpreted as clinically significant (
p < 0.05).
Parenting stress was measured with the Dutch Parenting Stress Index (PSI) short form (SF) [
46], which is based on the American Parenting Stress Index [
47]. Both parents rated 25 items on a 6-point Likert scale, ranging from 1 (totally disagree) to 6 (totally agree). Higher scores indicate higher levels of parenting stress. The Dutch PSI possesses good reliability and satisfactory validity [
46]. An example of an item is ‘Parenting this child is more difficult than I thought it would be’. Scores of the PSI-SF are calculated by adding all items, and scores range between 25 and 150. The cut-off point for very high scores is >89 for mothers and >79 for fathers. Mother completed the PSI-SF at all five measurements and father at baseline and 5-month follow-up. As the manual did not contain test–retest reliability and standard deviations of the mean scores [
46], the internal consistency and standard deviations of the mean scores of mothers and fathers of a control group of a large study that included the PSI-SF were used for the calculation of the RCI [
48]. The internal consistency of the PSI short form was Crohnbach’s
α = 0.94 for mothers and 0.95 for fathers, and the standard deviations were 19.48 and 17.74, respectively). On the basis of these values, a difference greater than 11.10 and 9.23 for the mother and father, respectively, was interpreted as clinically significant (
p < 0.05).
Partner relationship was measured by the subscale Partner relation of the Family Functioning Questionnaire (FFQ, in Dutch: Vragenlijst Gezinsfunctioneren voor Ouders) [
49]. The FFQ aims to measure different aspects of family functioning. The subscale Partner relationship consists of 5 items that are rated on a 4-point Likert scale, ranging from 1 (does not apply) to 4 (applies completely). Higher scores indicate higher levels of satisfaction with the partner and the level of appreciation and support from the partner. The mother rated the FFQ at pretest, post-test, and 3-month follow-up. An example of an item is ‘I feel supported by my partner in taking care of the children’. Scores are calculated by adding all items, and scores range between 5 and 20. The cut-off point for scores in the clinical range is >12. The psychometric properties of the FFQ are good [
49]. Because the manual of the FFQ does not report a test–retest reliability, the internal consistency was used (Crohnbach’s
α = 0.89), and the standard deviation of the mean score of the reference group of parents of 4- to 11-year-old children (2.6) [
37]. On the basis of these values, a difference greater than 2.01 was interpreted as clinically significant (
p < 0.05).
Acceptability of the BOAM trajectory was measured by a 9-item evaluation questionnaire that was completed by the mother at the post-test. The following questions were included in this questionnaire: How do you feel about the improvement that was made? How suitable was the BOAM trajectory for your request for help? To what extent would you recommend BOAM to other families? How do you feel about what you have learned as a parent? How suitable was the BOAM method for your referral? How content were you with the therapist? To what extent they could use what was learned in daily life? To what extent did your self-knowledge increase? To what extent did your confidence in the future increase?