The Interplay Between Sleep and Safety Outcomes in the Workplace: A Scoping Review and Bibliographic Analysis of the Literature
Abstract
1. Introduction
- (a)
- How did research on sleep–safety among the working population evolve over the years up to 2023 regarding publications and citations?This question would help us to understand how research related to sleep–safety has expanded over the years, e.g., trends and working population research. It would identify and distinguish foundational work from emerging trends.
- (b)
- Which journals have garnered the most impact?Research on sleep–safety spans multiple disciplines, making it essential to identify high-impact journals as key sources of influential findings. This helps to pinpoint publications driving innovation and policy and shaping both advancements in the field.
- (c)
- What topics (keywords and themes) are associated with this research field?Research on sleep–safety among the working population spans several disciplines, including occupational health, psychology, medicine, and ergonomics. Identifying keywords and themes helps to categorise knowledge, providing a clearer picture of the scope. This would highlight how sleep–safety is conceptualised and studied across different work environments.
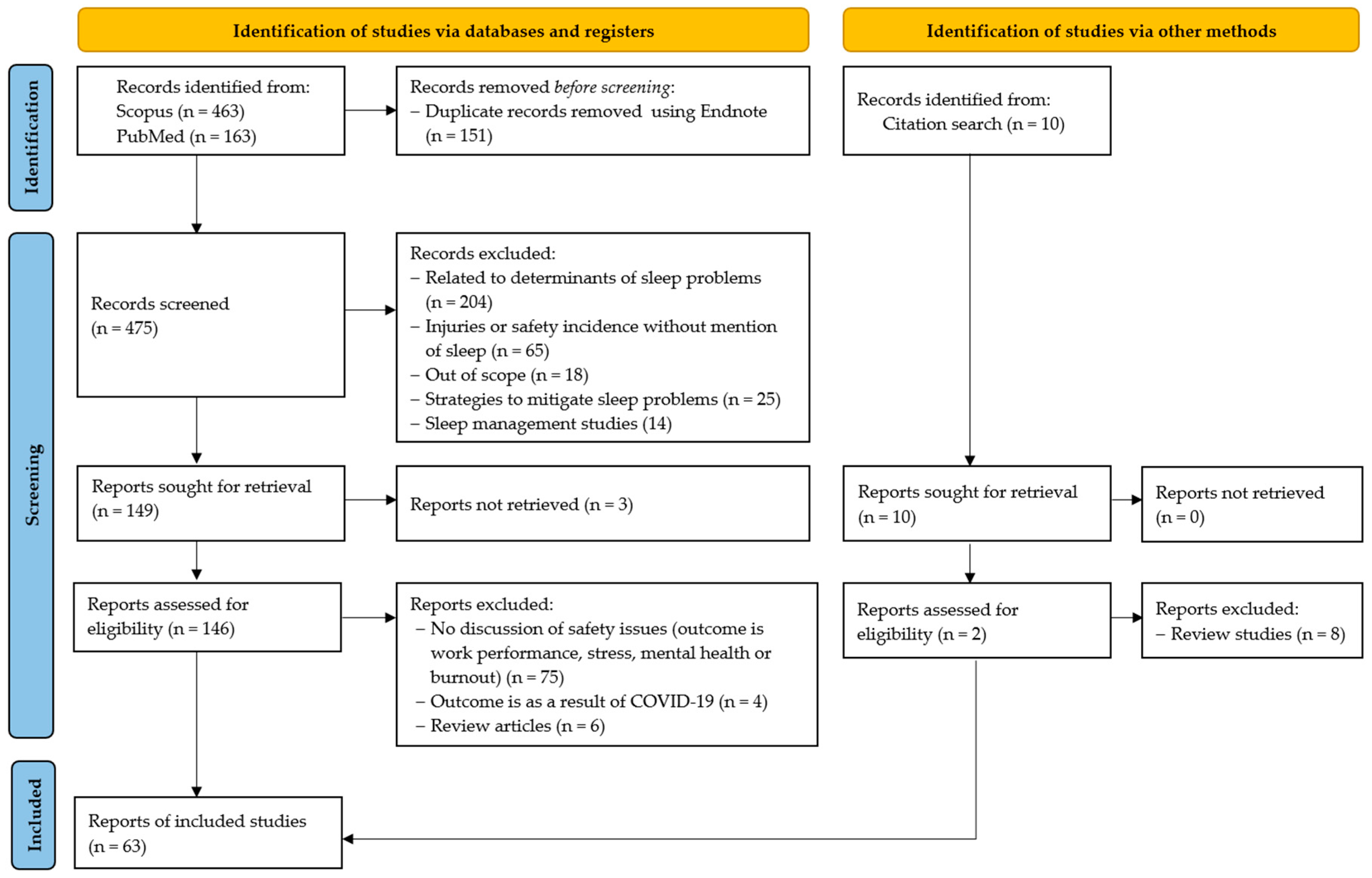
2. Materials and Methods
2.1. Unit of Analysis Employed for Bibliographic Analysis
2.1.1. Document Citation Analysis
2.1.2. Thematic Map
2.1.3. Journal Analysis Approach
2.2. Data Retrieval Process
3. Results
3.1. Sleep Assessment Tools Employed in the Studies
3.1.1. Pittsburgh Sleep Quality Index Scale (PSQI)
3.1.2. Epworth Sleepiness Scale (ESS)
3.1.3. Pittsburgh Sleep Diary
3.1.4. Sleep Hygiene Index (SHI)
| S/N | Article | Study Population | Research Method | Research Instrument for Sleep | Sleep Problem | The Outcome of Sleep Issue |
|---|---|---|---|---|---|---|
| 1 | Aderaw et al. [14] | Textile factory workers (n = 456) | Survey and interview |
|
|
|
| 2 | Alshareef [13] | Variety of occupations (n = 10,106) | Survey |
|
|
|
| 3 | Barnes and Wagner [45] | Miners (n = 14,301) | Interview |
|
| |
| 4 | Booker et al. [36] | Healthcare shift workers (n = 406) | Survey |
|
| |
| 5 | Brossoit et al. [46] | Construction workers (n = 222) | Survey |
|
|
|
| 6 | Brossoit et al. [8] | Army and Air National Guard service members (n = 704) | Survey |
|
|
|
| 7 | Buxton et al. [47] | Patient care workers (n = 1572) | Survey |
|
|
|
| 8 | Çolak and Esin [48] | Nurses (n = 83) | Survey |
|
|
|
| 9 | Daley et al. [49] | University staff (n = 20) | Experiment and survey |
|
|
|
| 10 | Das [50] | Brickfield workers, i.e., construction workers (n = 400) | Survey and interviews |
|
|
|
| 11 | Doss et al. [51] | Healthcare workers (n = 150) | Survey and interviews |
|
|
|
| 12 | Dutta [52] | Construction workers (n = 60) | Interviews and participant observations |
|
|
|
| 13 | Elfering et al. [53] | Software development and counselling (n = 40) | Experiment |
|
| |
| 14 | Fido and Ghali [54] | Blue collar workers in oil company (n = 200) | Survey |
|
|
|
| 15 | Filtness and Naweed [55] | Train drivers (n = 28) | Focus group and experiment |
|
|
|
| 16 | Fisman et al. [56] | Healthcare workers (n = 350) | Survey and interview |
|
|
|
| 17 | Fletcher and Dawson [57] | Train drivers (n = 193) | Experiment and survey |
|
|
|
| 18 | Garbarino et al. [58] | Police officers (n = 218) | Survey and interview |
|
|
|
| 19 | Gharibi et al. [23] | Oil construction company workers (n = 661) | Survey |
|
|
|
| 20 | Itani et al. [37] | Vehicle factory workers (n = 714) | Survey |
|
|
|
| 21 | Jay et al. [12] | Firefighters (n = 25) | Experiment and Survey |
|
|
|
| 22 | Kao et al. [10] | Construction services company workers (n = 3510) | Survey |
|
|
|
| 23 | Kessler et al. [59] | Not specified (n = 4991) | Survey |
|
|
|
| 24 | Kling et al. [60] | Variety of occupations (n = 69,584) | Survey |
|
| |
| 25 | Kottwitz et al. [61] | Printing company employees (n = 27) | Experiment and survey |
|
| |
| 26 | Lee et al. [62] | Variety of occupations (n = 26,468) | Survey |
|
|
|
| 27 | Léger et al. [63] | Not specified (n = 631) | Survey |
|
|
|
| 28 | Léger et al. [64] | Not specified (n = 738) | Survey |
|
|
|
| 29 | Lin et al. [65] | Firefighters (emergency medical service workers) (n = 399) | Survey |
|
|
|
| 30 | Lindholm et al. [66] | Home care personnel (n = 665) | Survey |
|
|
|
| 31 | Linton and Bryngelsson [67] | Not specified (n = 2066) | Survey |
|
|
|
| 32 | Lombardi et al. [68] | Not specified (n = 101,891) | Survey |
| ||
| 33 | Magnavita et al. [69] | Variety of occupations (n = 754) | Survey |
|
| |
| 34 | McMahon et al. [70] | Not specified (n = 23) | Experiment and survey |
|
|
|
| 35 | Melamed and Oksenberg [39] | Variety of occupations (n = 740) | Experiment and survey |
|
|
|
| 36 | Mohd et al. [71] | Electronic company workers (n = 255) | Survey |
|
|
|
| 37 | Morassaei and Smith [72] | Variety of occupations * | Survey |
|
|
|
| 38 | Muller et al. [73] | Minerals extraction and processing production workers (n = 48) | Survey |
|
|
|
| 39 | Mulrine et al. [74] | Not specified (n = 24) | Experiment and survey |
|
|
|
| 40 | Mulugeta et al. [75] | Textile factory workers (n = 311) | Survey |
|
| |
| 41 | Mutifasari and Ramdhan [76] | Truck drivers (n = 45) | Experiment and survey |
|
|
|
| 42 | Nakata [77] | Variety of occupations (n = 1891) | Survey |
|
| |
| 43 | Nishimura et al. [78] | Nurses (n = 30) | Survey |
|
|
|
| 44 | Patterson et al. [79] | Emergency medical services (EMS) workers (n = 355) | Survey |
|
|
|
| 45 | Petitta et al. [80] | Variety of occupations (n = 1000) | Survey |
|
|
|
| 46 | Pirrallo et al. [38] | Emergency medical technicians (n = 1854) | Survey |
|
|
|
| 47 | Powell and Copping [5] | Construction workers ** (n = 100) | Experiment |
|
|
|
| 48 | Powell and Copping [81] | Construction workers (n = 105) | Experiment |
|
|
|
| 49 | Rashid et al. [82] | Medical doctors (n = 375) | Survey |
|
|
|
| 50 | Renn and Cote [83] | Not specified (n = 49) | Experiment and survey |
|
|
|
| 51 | Robbins et al. [84] | Taxi drivers (n = 27) | Survey |
|
|
|
| 52 | Rosekind et al. [85] | Not specified (n = 4188) | Survey |
|
|
|
| 53 | Sabbagh-Ehrlich et al. [86] | Truck drivers (n = 160) | Mixed methods (questionnaire and interview) |
|
|
|
| 54 | Sneddon et al. [87] | Drillers in oil and gas (n = 185) | Survey |
|
|
|
| 55 | Tait et al. [88] | Marine pilots (n = 35) | Experiment and survey |
|
|
|
| 56 | Thomas and Ferguson [89] | Flight crewmembers (n = 302 flight operations) | Survey |
|
| |
| 57 | Uehli et al. [11] | Not specified (n = 731) | Survey |
|
|
|
| 58 | Valent et al. [90] | Hospital workers (n = 200) | Survey |
|
|
|
| 59 | Vargas-Garrido et al. [91] | Not specified (n = 1993) | Survey |
|
|
|
| 60 | Verma et al. [92] | Nurses (n = 480) | Survey |
|
|
|
| 61 | Wilhelm et al. [93] | Construction workers (n = 34) | Experiment |
|
|
|
| 62 | Wilson et al. [94] | Nurses (n = 22) | Experiment and survey |
|
|
|
| 63 | Wong et al. [95] | Not specified Study 1 (n = 4238); study 2 (n = 202); study 3 (n = 71) | Survey |
|
|
3.1.5. STOP-Bang Questionnaire
3.1.6. Jenkins Sleep Problems Scale
3.1.7. Karolinska Sleep Questionnaire (KSQ)
3.1.8. Karolinska Sleepiness Scale (KSS)
3.2. Document Citation Analysis for Sleep-Safety Research
3.2.1. Most Locally Cited Documents
3.2.2. Most Globally Cited Documents
3.2.3. Geographical Distribution of Study Population
| S/N | Country | Number of Studies |
|---|---|---|
| 1 | United States of America | 15 |
| 2 | Australia | 8 |
| 3 | Canada | 6 |
| 4 | Italy | 4 |
| 5 | Japan | 3 |
| 6 | India | 3 |
| 7 | Switzerland | 3 |
| 8 | New Zealand | 3 |
| 9 | United Kingdom | 3 |
| 10 | Malaysia | 2 |
| 11 | Israel | 2 |
| 12 | Sweden | 2 |
| 13 | France | 2 |
| 14 | Ethiopia | 2 |
| 15 | Iran | 1 |
| 16 | Saudi Arabia | 1 |
| 17 | South Korea | 1 |
| 18 | Taiwan | 1 |
| 19 | Kuwait | 1 |
| 20 | Singapore | 1 |
| 21 | Indonesia | 1 |
| 22 | Turkey | 1 |
| 23 | Chile | 1 |
| 24 | Germany | 1 |
| Total | 68 |
3.3. Representative Journals
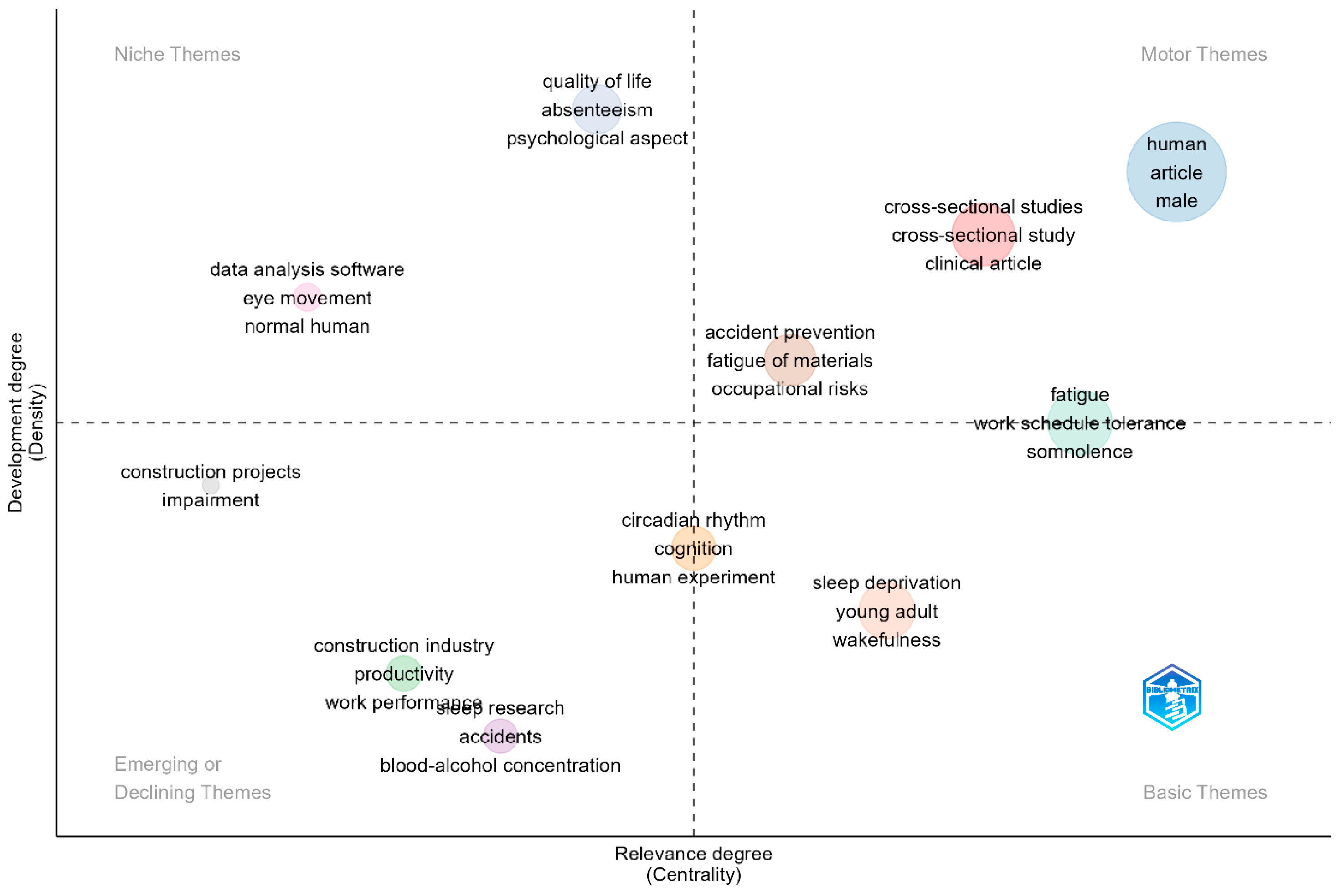
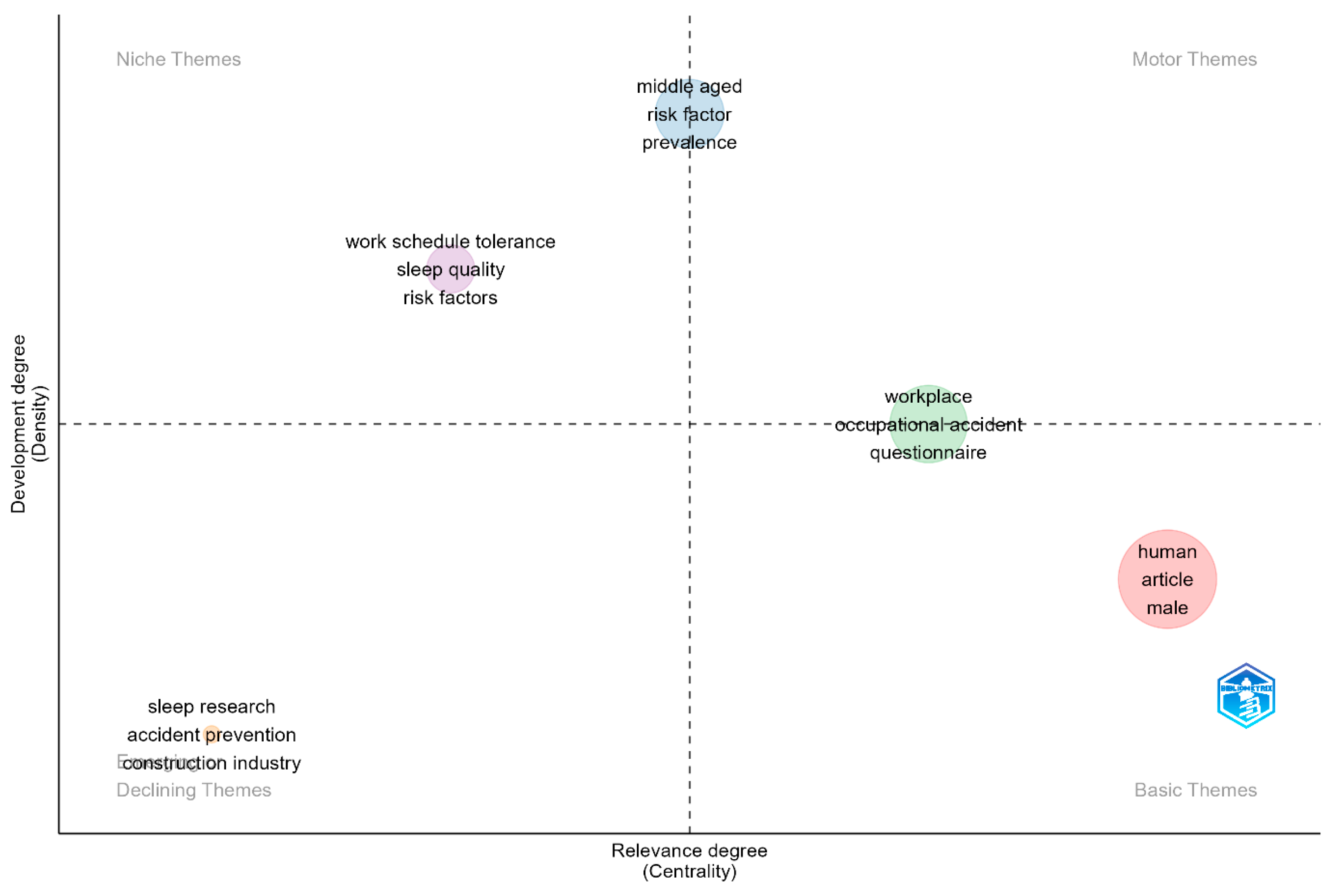
3.4. Keywords and Topic Trends Analysis
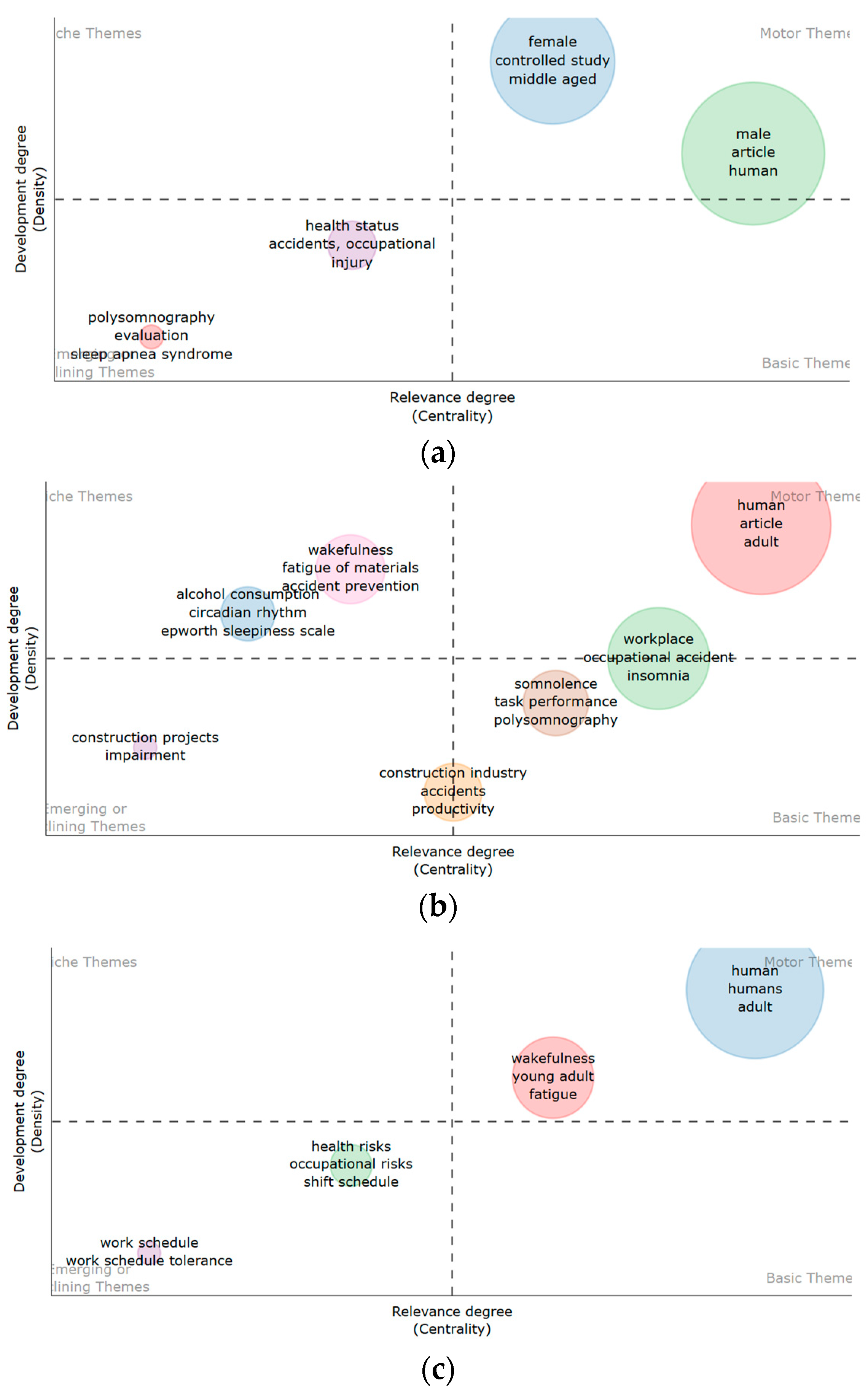
3.4.1. Thematic Analysis and Map for Sleep-Safety Research
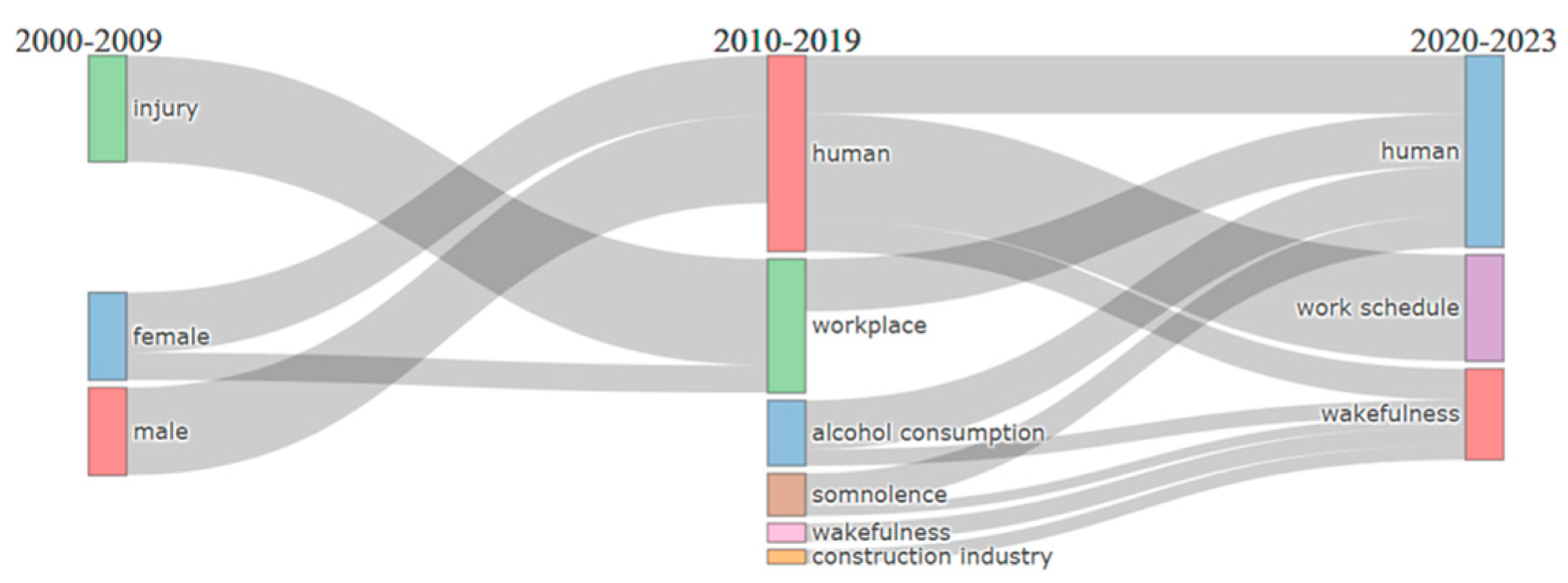
3.4.2. Thematic Evolution
4. Discussion
4.1. Areas of Sleep Incidence Research
4.1.1. Sleep Disorders
4.1.2. Cognition and Performance
4.1.3. Work Schedule
4.1.4. Impact on Quality of Life (Physical Health Impact)
4.1.5. Injury and Accident Prevention in the Construction Sector
4.1.6. Demographic and Lifestyle Factors
5. Future Directions
5.1. Sleep Questionnaires
5.2. Sleep Quality Model
5.3. Safety Management Audit
5.4. Methodological Gaps
5.5. Effect of Sleep Issue Intensity
6. Limitations
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| S/N | Sources (Journal Outlets) | Frequency | Zone | Articles per Zone |
|---|---|---|---|---|
| 1 | International Journal of Environmental Research and Public Health | 5 | 1 | 22 |
| 2 | Sleep | 5 | 1 | |
| 3 | Chronobiology International | 3 | 1 | |
| 4 | Journal of Workplace and Environmental Medicine | 3 | 1 | |
| 5 | Journal of Workplace Health Psychology | 3 | 1 | |
| 6 | Journal of Sleep Research | 3 | 1 | |
| 7 | Nature and Science of Sleep | 2 | 2 | 21 |
| 8 | Sleep and Vigilance | 2 | 2 | |
| 9 | Accident Analysis and Prevention | 1 | 2 | |
| 10 | Annals of Workplace Hygiene | 1 | 2 | |
| 11 | Applied Ergonomics | 1 | 2 | |
| 12 | Australian Journal of Rural Health | 1 | 2 | |
| 13 | Aviation Space and Environmental Medicine | 1 | 2 | |
| 14 | Biomedical Signal Processing and Control | 1 | 2 | |
| 15 | BMC Public Health | 1 | 2 | |
| 16 | BMJ Open | 1 | 2 | |
| 17 | Current Psychology | 1 | 2 | |
| 18 | Ergonomics | 1 | 2 | |
| 19 | Infection Control and Hospital Epidemiology | 1 | 2 | |
| 20 | Injury Prevention | 1 | 2 | |
| 21 | International Journal of Experimental Research and Review | 1 | 2 | |
| 22 | International Journal of Industrial Ergonomics | 1 | 2 | |
| 23 | International Journal of Workplace and Environmental Medicine | 1 | 2 | |
| 24 | International Journal of Workplace Medicine and Environmental Health | 1 | 2 | |
| 25 | International Journal of Psychophysiology | 1 | 2 | |
| 26 | International Nursing Review | 1 | 3 | 20 |
| 27 | Iranian Journal of Nursing and Midwifery Research | 1 | 3 | |
| 28 | Journal of Applied Psychology | 1 | 3 | |
| 29 | Journal of Construction Engineering and Management | 1 | 3 | |
| 30 | Journal of Engineering, Design and Technology | 1 | 3 | |
| 31 | Journal of Workplace Rehabilitation | 1 | 3 | |
| 32 | Journal of Tropical Medicine | 1 | 3 | |
| 33 | Malaysian Journal of Medicine and Health Sciences | 1 | 3 | |
| 34 | Medical Principles and Practice | 1 | 3 | |
| 35 | Nordic Journal of Working Life Studies | 1 | 3 | |
| 36 | Workplace and Environmental Medicine | 1 | 3 | |
| 37 | PLoS ONE | 1 | 3 | |
| 38 | Prehospital Emergency Care | 1 | 3 | |
| 39 | Safety Science | 1 | 3 | |
| 40 | Sleep and Biological Rhythms | 1 | 3 | |
| 41 | Sleep and Breathing | 1 | 3 | |
| 42 | Sleep Medicine | 1 | 3 | |
| 43 | Somnology | 1 | 3 | |
| 44 | Transportation Research Part F: Traffic Psychology and Behaviour | 1 | 3 | |
| 45 | Work and Stress | 1 | 3 |
References
- Murtin, F.; Arnaud, B.; Gallie, D.; Le Thi, C.; Parent-Thirion, A. Changes in Job Strain in the Us, Europe and Korea. Appl. Res. Qual. Life 2024, 19, 1903–1926. [Google Scholar]
- Kivimäki, M.; Nyberg, S.T.; Batty, G.D.; Fransson, E.I.; Heikkilä, K.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Casini, A. Job Strain as a Risk Factor for Coronary Heart Disease: A Collaborative Meta-Analysis of Individual Participant Data. Lancet 2012, 380, 1491–1497. [Google Scholar]
- Mensah, A. Job Stress and Mental Well-Being among Working Men and Women in Europe: The Mediating Role of Social Support. Int. J. Environ. Res. Public Health 2021, 18, 2494. [Google Scholar] [CrossRef] [PubMed]
- Fietze, I.; Rosenblum, L.; Salanitro, M.; Ibatov, A.D.; Eliseeva, M.V.; Penzel, T.; Brand, D.; Westermayer, G. The Interplay between Poor Sleep and Work-Related Health. Front. Public Health 2022, 10, 866750. [Google Scholar]
- Powell, R.I.; Copping, A.G. Measuring Fatigue-Related Impairment in the Workplace. J. Eng. Des. Technol. 2016, 14, 507–525. [Google Scholar] [CrossRef]
- Nwaogu, J.M.; Chan, A.P.C. Work-Related Stress, Psychophysiological Strain, and Recovery among on-Site Construction Personnel. Autom. Constr. 2021, 125, 103629. [Google Scholar]
- Glick, D.R.; Abariga, S.A.; Thomas, I.; Shipper, A.G.; Gunia, B.C.; Grandner, M.A.; Rosenberg, E.; Hines, S.E.; Capaldi, V.; Collen, J.; et al. Economic Impact of Insufficient and Disturbed Sleep in the Workplace. Pharmacoeconomics 2023, 41, 771–785. [Google Scholar] [PubMed]
- Brossoit, R.M.; Hammer, L.B.; Crain, T.L.; Leslie, J.J.; Bodner, T.E.; Brockwood, K.J. The Effects of a Total Worker Health Intervention on Workplace Safety: Mediating Effects of Sleep and Supervisor Support for Sleep. J. Occup. Health Psychol. 2023, 28, 263–276. [Google Scholar]
- Stemn, E.; Benyarku, C.A. Mineworkers’ Perspective of Fatigue: A Study of the Ghanaian Mining Industry. Saf. Sci. 2023, 162, 106095. [Google Scholar]
- Kao, K.Y.; Spitzmueller, C.; Cigularov, K.; Wu, H. Linking Insomnia to Workplace Injuries: A Moderated Mediation Model of Supervisor Safety Priority and Safety Behavior. J. Occup. Health Psychol. 2016, 21, 91–104. [Google Scholar] [CrossRef]
- Uehli, K.; Mehta, A.J.; Miedinger, D.; Hug, K.; Schindler, C.; Holsboer-Trachsler, E.; Leuppi, J.D.; Künzli, N. Sleep Problems and Work Injuries: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2014, 18, 61–73. [Google Scholar] [PubMed]
- Jay, S.M.; Smith, B.P.; Windler, S.; Dorrian, J.; Ferguson, S.A. Does Suspected Sleep Disordered Breathing Impact on the Sleep and Performance of Firefighting Volunteers During a Simulated Fire Ground Campaign? Int. J. Environ. Res. Public Health 2016, 13, 173. [Google Scholar] [CrossRef]
- Alshareef, S.M. Occupational Outcomes Associated with Sleep Quality and Excessive Daytime Sleepiness: Results from a National Survey. Nat. Sci. Sleep 2020, 12, 875–882. [Google Scholar]
- Aderaw, Z.; Engdaw, D.; Tadesse, T. Determinants of Occupational Injury: A Case Control Study among Textile Factory Workers in Amhara Regional State, Ethiopia. J. Trop. Med. 2011, 2011, 657275. [Google Scholar] [PubMed]
- Wong, I.S.; Quay, B.; Irvin, E.; Belzer, M.H. Describing Economic Benefits and Costs of Nonstandard Work Hours: A Scoping Review. Am. J. Ind. Med. 2022, 65, 926–939. [Google Scholar]
- Garbarino, S.; Guglielmi, O.; Sanna, A.; Mancardi, G.L.; Magnavita, N. Risk of Occupational Accidents in Workers with Obstructive Sleep Apnea: Systematic Review and Meta-Analysis. Sleep 2016, 39, 1211–1218. [Google Scholar] [CrossRef]
- Alfonsi, V.; Scarpelli, S.; Gorgoni, M.; Pazzaglia, M.; Giannini, A.M.; De Gennaro, L. Sleep-Related Problems in Night Shift Nurses: Towards an Individualized Interventional Practice. Front. Hum. Neurosci. 2021, 15, 644570. [Google Scholar]
- Sun, Q.; Ji, X.; Zhou, W.; Liu, J. Sleep Problems in Shift Nurses: A Brief Review and Recommendations at Both Individual and Institutional Levels. J. Nurs. Manag. 2019, 27, 10–18. [Google Scholar] [PubMed]
- Wagstaff, A.S.; Lie, J.A.S. Shift and Night Work and Long Working Hours—A Systematic Review of Safety Implications. Scand. J. Work Environ. Health 2011, 37, 173–185. [Google Scholar]
- Bauerle, T.J.; Sammarco, J.J.; Dugdale, Z.J.; Dawson, D. The Human Factors of Mineworker Fatigue: An Overview on Prevalence, Mitigation, and What’s Next. Am. J. Ind. Med. 2022, 65, 832–839. [Google Scholar]
- Mak, S.; Thomas, A. Steps for Conducting a Scoping Review. J. Grad. Med. Educ. 2022, 14, 565–567. [Google Scholar]
- Madsen, D.Ø.; Berg, T.; Di Nardo, M. Bibliometric Trends in Industry 5.0 Research: An Updated Overview. Appl. Syst. Innov. 2023, 6, 63. [Google Scholar] [CrossRef]
- Gharibi, V.; Mokarami, H.; Cousins, R.; Jahangiri, M.; Eskandari, D. Excessive Daytime Sleepiness and Safety Performance: Comparing Proactive and Reactive Approaches. Int. J. Occup. Environ. Med. 2020, 11, 95–107. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar]
- Aria, M.; Cuccurullo, C. Bibliometrix: An R-Tool for Comprehensive Science Mapping Analysis. J. Informetr. 2017, 11, 959–975. [Google Scholar]
- Pollock, D.; Davies, E.L.; Peters, M.D.J.; Tricco, A.C.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H.; Munn, Z. Undertaking a Scoping Review: A Practical Guide for Nursing and Midwifery Students, Clinicians, Researchers, and Academics. J Adv. Nurs. 2021, 77, 2102–2113. [Google Scholar] [PubMed]
- Page, M.J.; Shamseer, L.; Tricco, A.C. Registration of Systematic Reviews in Prospero: 30,000 Records and Counting. Syst. Rev. 2018, 7, 32. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. Prisma Extension for Scoping Reviews (Prisma-Scr): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar]
- Christensen, A.P.; Garrido, L.E.; Guerra-Peña, K.; Golino, H. Comparing Community Detection Algorithms in Psychological Data: A Monte Carlo Simulation. Behav. Res. Methods 2024, 56, 1485–1505. [Google Scholar] [CrossRef]
- Chen, X.; Lun, Y.; Yan, J.; Hao, T.; Weng, H. Discovering Thematic Change and Evolution of Utilizing Social Media for Healthcare Research. BMC Med. Inform. Decis. Mak. 2019, 19 (Suppl. S2), 50. [Google Scholar]
- Cobo, M.J.; López-Herrera, A.G.; Herrera-Viedma, E.; Herrera, F. An Approach for Detecting, Quantifying, and Visualizing the Evolution of a Research Field: A Practical Application to the Fuzzy Sets Theory Field. J. Informetr. 2011, 5, 146–166. [Google Scholar]
- Nash-Stewart, C.E.; Kruesi, L.M.; Del Mar, C.B. Does Bradford’s Law of Scattering Predict the Size of the Literature in Cochrane Reviews? J. Med. Libr. Assoc. 2012, 100, 135–138. [Google Scholar]
- Potter, J. Mapping the Literature of Occupational Therapy: An Update. J. Med. Libr. Assoc. 2010, 98, 235–242. [Google Scholar]
- Chan Albert, P.C.; Nwaogu Janet, M.; Naslund John, A. Mental Ill-Health Risk Factors in the Construction Industry: Systematic Review. J. Constr. Eng. Manag. 2020, 146, 04020004. [Google Scholar] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Booker, L.A.; Spong, J.; Hodge, B.; Deacon-Crouch, M.; Bish, M.; Mills, J.; Skinner, T.C. Differences in Shift and Work-Related Patterns between Metropolitan and Regional/Rural Healthcare Shift Workers and the Occupational Health and Safety Risks. Aust. J. Rural Health 2023, 32, 141–151. [Google Scholar]
- Itani, O.; Kaneita, Y.; Jike, M.; Furuya, M.; Uezono, C.; Oda, F.; Agematsu, R.; Tokiya, M.; Otsuka, Y.; Ohida, T. Sleep-Related Factors Associated with Industrial Accidents among Factory Workers and Sleep Hygiene Education Intervention. Sleep Biol. Rhythm. 2018, 16, 239–251. [Google Scholar]
- Pirrallo, R.G.; Loomis, C.C.; Levine, R.; Woodson, T. The Prevalence of Sleep Problems in Emergency Medical Technicians. Sleep Breath. 2012, 16, 149–162. [Google Scholar]
- Melamed, S.; Oksenberg, A. Excessive Daytime Sleepiness and Risk of Occupational Injuries in Non-Shift Daytime Workers. Sleep 2002, 25, 315–322. [Google Scholar]
- Mulgrew, A.T.; Ryan, C.F.; Fleetham, J.A.; Cheema, R.; Fox, N.; Koehoorn, M.; FitzGerald, J.M.; Marra, C.; Ayas, N.T. The Impact of Obstructive Sleep Apnea and Daytime Sleepiness on Work Limitation. Sleep Med. 2007, 9, 42–53. [Google Scholar]
- Monk, T.H.; Reynolds, C.F., III; Kupfer, D.J.; Buysse, D.J.; Coble, P.A.; Hayes, A.J.; Machen, M.A.; Petrie, S.R.; Ritenour, A.M. The Pittsburgh Sleep Diary. J. Sleep Res. 1994, 3, 111–120. [Google Scholar] [PubMed]
- Cho, S.; Kim, G.S.; Lee, J.H. Psychometric Evaluation of the Sleep Hygiene Index: A Sample of Patients with Chronic Pain. Health Qual. Life Outcomes 2013, 11, 213. [Google Scholar] [PubMed]
- Mastin, D.F.; Siddalingaiah, H.S.; Singh, A.; Lal, V. Excessive Daytime Sleepiness, Sleep Hygiene, and Work Hours among Medical Residents in India. J. Trop. Psychol. 2012, 2, e4. [Google Scholar]
- Mastin, D.F.; Bryson, J.; Corwyn, R. Assessment of Sleep Hygiene Using the Sleep Hygiene Index. J. Behav. Med. 2006, 29, 223–227. [Google Scholar]
- Barnes, C.M.; Wagner, D.T. Changing to Daylight Saving Time Cuts into Sleep and Increases Workplace Injuries. J. Appl. Psychol. 2009, 94, 1305–1317. [Google Scholar]
- Brossoit, R.M.; Crain, T.L.; Leslie, J.J.; Hammer, L.B.; Truxillo, D.M.; Bodner, T.E. The Effects of Sleep on Workplace Cognitive Failure and Safety. J. Occup. Health Psychol. 2019, 24, 411–422. [Google Scholar]
- Buxton, O.M.; Hopcia, K.; Sembajwe, G.; Porter, J.H.; Dennerlein, J.T.; Kenwood, C.; Stoddard, A.M.; Hashimoto, D.; Sorensen, G. Relationship of Sleep Deficiency to Perceived Pain and Functional Limitations in Hospital Patient Care Workers. J. Occup. Environ. Med. 2012, 54, 851–858. [Google Scholar]
- Çolak, M.; Esin, M.N. Factors Affecting the Psychomotor Vigilance of Nurses Working Night Shift. Int. Nurs. Rev. 2023, 71, 84–93. [Google Scholar]
- Daley, M.S.; Diaz, K.; Posada-Quintero, H.F.; Kong, Y.; Chon, K.; Bolkhovsky, J.B. Archetypal Physiological Responses to Prolonged Wakefulness. Biomed. Signal Process. Control. 2022, 74, 103529. [Google Scholar]
- Das, B. Prevalence of Work-Related Occupational Injuries and Its Risk Factors among Brickfield Workers in West Bengal, India. Int. J. Ind. Ergon. 2020, 80, 103052. [Google Scholar]
- Doss, K.S.A.; Amirthalingam, B.; Kathiresan, S. Assessing the Risk of Occupational Hazard Using the Fmea Tool among Hospital Staff at Multispecialty Hospital. Int. J. Exp. Res. Rev. 2023, 35, 43–53. [Google Scholar]
- Dutta, M.J. Migration and Health in the Construction Industry: Culturally Centering Voices of Bangladeshi Workers in Singapore. Int. J. Environ. Res. Public Health 2017, 14, 132. [Google Scholar] [CrossRef]
- Elfering, A.; Gerhardt, C.; Pereira, D.; Schenker, A.; Kottwitz, M.U. The Monday Effect Revisited: A Diary and Sleep Actigraphy Study. Sleep Vigil. 2020, 4, 167–176. [Google Scholar]
- Fido, A.; Ghali, A. Detrimental Effects of Variable Work Shifts on Quality of Sleep, General Health and Work Performance. Med. Princ. Pract. 2008, 17, 453–457. [Google Scholar]
- Filtness, A.J.; Naweed, A. Causes, Consequences and Countermeasures to Driver Fatigue in the Rail Industry: The Train Driver Perspective. Appl. Ergon. 2017, 60, 12–21. [Google Scholar]
- Fisman, D.N.; Harris, A.D.; Rubin, M.; Sorock, G.S.; Mittleman, M.A. Fatigue Increases the Risk of Injury from Sharp Devices in Medical Trainees: Results from a Case-Crossover Study. Infect. Control Hosp. Epidemiol. 2007, 28, 10–17. [Google Scholar] [PubMed]
- Fletcher, A.; Dawson, D. Field-Based Validations of a Work-Related Fatigue Model Based on Hours of Work. Transp. Res. Part F Traffic Psychol. Behav. 2001, 4, 75–88. [Google Scholar]
- Garbarino, S.; Tripepi, G.; Magnavita, N. Sleep Health Promotion in the Workplace. Int. J. Environ. Res. Public Health 2020, 17, 7952. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.A.; Coulouvrat, C.; Fitzgerald, T.; Hajak, G.; Roth, T.; Shahly, V.; Shillington, A.C.; Stephenson, J.J.; Walsh, J.K. Walsh. Insomnia, Comorbidity, and Risk of Injury among Insured Americans: Results from the America Insomnia Survey. Sleep 2012, 35, 825–834. [Google Scholar] [CrossRef]
- Kling, R.N.; McLeod, C.B.; Koehoorn, M. Sleep Problems and Workplace Injuries in Canada. Sleep 2010, 33, 611–618. [Google Scholar] [CrossRef]
- Kottwitz, M.U.; Gerhardt, C.; Schmied, S.; Elfering, A. Sleep, Work Stress and Headache in Printing Business: An Actigraphy Study. Sleep Vigil. 2019, 3, 9–15. [Google Scholar] [CrossRef]
- Lee, W.; Lee, J.; Kim, U.J.; Yoon, J.H.; Choi, W.J.; Ham, S.; Chung, E.K.; Kang, S.K. Working Conditions and Mental Health Status Related with Occupational Injury of Korean Outdoor Workers. J. Occup. Environ. Med. 2020, 62, e334–e339. [Google Scholar] [CrossRef]
- Léger, D.; Guilleminault, C.; Bader, G.; Lévy, E.; Paillard, M. Medical and Socio-Professional Impact of Insomnia. Sleep 2002, 25, 621–625. [Google Scholar] [CrossRef]
- Léger, D.; Massuel, M.A.; Metlaine, A. Professional Correlates of Insomnia. Sleep 2006, 29, 171–178. [Google Scholar] [PubMed]
- Lin, M.H.; Huang, Y.C.; Chen, W.K.; Wang, J.Y. Sleepiness and Injury Risk in Emergency Medical Service Workers in Taiwan. PLoS ONE 2020, 15, e0229202. [Google Scholar] [CrossRef]
- Lindholm, M.; Målqvist, I.; Alderling, M.; Hillert, L.; Lind, C.M.; Reiman, A.; Forsman, M. Sleep-Related Problems and Associations with Occupational Factors among Home Care Personnel. Nord. J. Work. Life Stud. 2022, 12, 3–25. [Google Scholar] [CrossRef]
- Linton, S.J.; Bryngelsson, I.L. Insomnia and Its Relationship to Work and Health in a Working-Age Population. J. Occup. Rehabil. 2000, 10, 169–183. [Google Scholar] [CrossRef]
- Lombardi, D.A.; Wirtz, A.; Willetts, J.L.; Folkard, S. Independent Effects of Sleep Duration and Body Mass Index on the Risk of a Work-Related Injury: Evidence from the Us National Health Interview Survey (2004–2010). Chronobiol. Int. 2012, 29, 556–564. [Google Scholar] [CrossRef]
- Magnavita, N.; Di Prinzio, R.R.; Arnesano, G.; Cerrina, A.; Gabriele, M.; Garbarino, S.; Gasbarri, M.; Iuliano, A.; Labella, M.; Matera, C.; et al. Association of Occupational Distress and Low Sleep Quality with Syncope, Presyncope, and Falls in Workers. Int. J. Environ. Res. Public Health 2021, 18, 12283. [Google Scholar] [CrossRef]
- McMahon, W.R.; Ftouni, S.; Diep, C.; Collet, J.; Lockley, S.W.; Rajaratnam, S.M.W.; Maruff, P.; Drummond, S.P.A.; Anderson, C. The Impact of the Wake Maintenance Zone on Attentional Capacity, Physiological Drowsiness, and Subjective Task Demands During Sleep Deprivation. J. Sleep Res. 2021, 30, e13312. [Google Scholar] [CrossRef]
- Mohd, S.A.H.; Mohamad, E.A.J.; Norazura, I. Sleepiness and Daily Sleep of Malaysian Shift Workers in Electronics Manufacturing Industry. Malays. J. Public Health Med. 2020, 20, 208–215. [Google Scholar]
- Morassaei, S.; Smith, P.M. Switching to Daylight Saving Time and Work Injuries in Ontario, Canada: 1993-2007. Occup. Environ. Med. 2010, 67, 878–880. [Google Scholar] [PubMed]
- Muller, R.; Carter, A.; Williamson, A. Epidemiological Diagnosis of Occupational Fatigue in a Fly-in-Fly-out Operation of the Mineral Industry. Ann. Occup. Hyg. 2008, 52, 63–72. [Google Scholar]
- Mulrine, H.M.; Signal, T.L.; Berg, M.J.V.D.; Gander, P.H. Post-Sleep Inertia Performance Benefits of Longer Naps in Simulated Nightwork and Extended Operations. Chronobiol. Int. 2012, 29, 1249–1257. [Google Scholar]
- Mulugeta, H.; Birile, A.; Ketema, H.; Tessema, M.; Thygerson, S.M. Non-Fatal Occupational Injury Prevalence and Associated Factors in an Integrated Large-Scale Textile Industry in Addis Ababa, Ethiopia. Int. J. Environ. Res. Public Health 2022, 19, 3688. [Google Scholar] [CrossRef] [PubMed]
- Mutifasari, R.S.; Ramdhan, D.H. Association between Sleep Quantity and Quality with Occupational Stress among Truck Driver. Malays. J. Med. Health Sci. 2019, 15, 153–158. [Google Scholar]
- Nakata, A. Effects of Long Work Hours and Poor Sleep Characteristics on Workplace Injury among Full-Time Male Employees of Small- and Medium-Scale Businesses. J. Sleep Res. 2011, 20, 576–584. [Google Scholar]
- Nishimura, Y.; Ikeda, H.; Matsumoto, S.; Izawa, S.; Kawakami, S.; Tamaki, M.; Masuda, S.; Kubo, T. Impaired Self-Monitoring Ability on Reaction Times of Psychomotor Vigilance Task of Nurses after a Night Shift. Chronobiol. Int. 2023, 40, 603–611. [Google Scholar] [PubMed]
- Patterson, P.D.; Buysse, D.J.; Weaver, M.D.; Callaway, C.W.; Yealy, D.M. Recovery between Work Shifts among Emergency Medical Services Clinicians. Prehosp. Emerg. Care 2015, 19, 365–375. [Google Scholar]
- Petitta, L.; Probst, T.M.; Ghezzi, V.; Barbaranelli, C. The Impact of Emotional Contagion on Workplace Safety: Investigating the Roles of Sleep, Health, and Production Pressure. Curr. Psychol. 2023, 42, 2362–2376. [Google Scholar]
- Powell, R.; Copping, A. Sleep Deprivation and Its Consequences in Construction Workers. J. Constr. Eng. Manag. 2010, 136, 1086–1092. [Google Scholar]
- Rashid, A.A.; Devaraj, N.K.; Mohd Yusof, H.; Mustapha, F.; Wong, S.V.; Ismail, A.F.; Ismail, K.I.; Qureshi, A.M.; Nordin, R.B. Prevalence and Predictors of Road Crash Involvement among Medical Doctors in Malaysia: A Cross-Sectional Study Protocol. BMJ Open 2020, 10, e037653. [Google Scholar] [PubMed]
- Renn, R.P.; Cote, K.A. Performance Monitoring Following Total Sleep Deprivation: Effects of Task Type and Error Rate. Int. J. Psychophysiol. 2013, 88, 64–73. [Google Scholar] [PubMed]
- Robbins, R.; Trinh-Shevrin, C.; Chong, S.K.; Chanko, N.; Diaby, F.; Quan, S.F.; Kwon, S.C. Examining Demographic, Work, and Sleep Characteristics among Older South Asian American Yellow Taxi Drivers in New York City: A Brief Report. Sleep Med. 2022, 96, 128–131. [Google Scholar]
- Rosekind, M.R.; Gregory, K.B.; Mallis, M.M.; Brandt, S.L.; Seal, B.; Lerner, D. The Cost of Poor Sleep: Workplace Productivity Loss and Associated Costs. J. Occup. Environ. Med. 2010, 52, 91–98. [Google Scholar]
- Sabbagh-Ehrlich, S.; Friedman, L.; Richter, E.D. Working Conditions and Fatigue in Professional Truck Drivers at Israeli Ports. Inj. Prev. 2005, 11, 110–114. [Google Scholar]
- Sneddon, A.; Mearns, K.; Flin, R. Stress, Fatigue, Situation Awareness and Safety in Offshore Drilling Crews. Saf. Sci. 2013, 56, 80–88. [Google Scholar]
- Tait, J.L.; Chambers, T.P.; Tait, R.S.; Main, L.C. Impact of Shift Work on Sleep and Fatigue in Maritime Pilots. Ergonomics 2021, 64, 856–868. [Google Scholar]
- Thomas, M.J.W.; Ferguson, S.A. Prior Sleep, Prior Wake, and Crew Performance During Normal Flight Operations. Aviat. Space Environ. Med. 2010, 81, 665–670. [Google Scholar]
- Valent, F.; Mariuz, M.; Liva, G.; Bellomo, F.; De Corti, D.; Degan, S.; Ferrazzano, A.; Brusaferro, S. A Case-Crossover Study of Sleep, Fatigue, and Other Transient Exposures at Workplace and the Risk of Non-Fatal Occupational Injuries among the Employees of an Italian Academic Hospital. Int. J. Occup. Med. Environ. Health 2016, 29, 1001–1009. [Google Scholar]
- Vargas-Garrido, H.; Moyano-Díaz, E.; Andrades, K. Sleep Problems Are Related to Commuting Accidents Rather Than to Workplace Accidents. BMC Public Health 2021, 21, 652. [Google Scholar]
- Verma, A.; Kishore, J.; Gusain, S. A Comparative Study of Shift Work Effects and Injuries among Nurses Working in Rotating Night and Day Shifts in a Tertiary Care Hospital of North India. Iran. J. Nurs. Midwifery Res. 2018, 23, 51–56. [Google Scholar] [PubMed]
- Wilhelm, B.J.; Heine, C.; Widmann, A.; Durst, W.; Lüdtke, H.; Otto, G. How Sleepy Are Construction Workers During Extended Shifts? An Objective Investigation of Spontaneous Pupillary Oscillations in Tunnel Workmen. Somnologie 2010, 14, 200–206. [Google Scholar]
- Wilson, M.; Permito, R.; English, A.; Albritton, S.; Coogle, C.; Van Dongen, H.P.A. Performance and Sleepiness in Nurses Working 12-H Day Shifts or Night Shifts in a Community Hospital. Accid. Anal. Prev. 2019, 126, 43–46. [Google Scholar] [PubMed]
- Wong, J.H.K.; Turner, N.; Kelloway, E.K.; Wadsworth, E.J. Tired, Strained, and Hurt: The Indirect Effect of Negative Affect on the Relationship between Poor Quality Sleep and Work Injuries. Work Stress 2021, 35, 153–170. [Google Scholar]
- Chung, F.; Yegneswaran, B.; Liao, P.; Chung, S.A.; Vairavanathan, S.; Islam, S.; Khajehdehi, A.; Shapiro, C.M. Stop Questionnaire: A Tool to Screen Patients for Obstructive Sleep Apnea. Anesthesiology 2008, 108, 812–821. [Google Scholar]
- Nagappa, M.; Liao, P.; Wong, J.; Auckley, D.; Ramachandran, S.K.; Memtsoudis, S.; Mokhlesi, B.; Chung, F. Validation of the Stop-Bang Questionnaire as a Screening Tool for Obstructive Sleep Apnea among Different Populations: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0143697. [Google Scholar]
- Chung, F.; Abdullah, H.R.; Liao, P. Stop-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Chest 2016, 149, 631–638. [Google Scholar]
- Jenkins, C.D.; Stanton, B.-A.; Niemcryk, S.J.; Rose, R.M. Rose. A Scale for the Estimation of Sleep Problems in Clinical Research. J. Clin. Epidemiol. 1988, 41, 313–321. [Google Scholar]
- Gluschkoff, K.; Elovainio, M.; Kinnunen, U.; Mullola, S.; Hintsanen, M.; Keltikangas-Järvinen, L.; Hintsa, T. Work Stress, Poor Recovery and Burnout in Teachers. Occup. Med. 2016, 66, 564–570. [Google Scholar]
- Juhola, J.; Arokoski, J.P.A.; Ervasti, J.; Kivimäki, M.; Vahtera, J.; Myllyntausta, S.; Saltychev, M. Internal Consistency and Factor Structure of Jenkins Sleep Scale: Cross-Sectional Cohort Study among 80 000 Adults. BMJ Open 2021, 11, e043276. [Google Scholar] [PubMed]
- Monterrosa-Castro, Á.; Portela-Buelvas, K.; Salguedo-Madrid, M.; Mo-Carrascal, J.; Duran-Méndez Leidy, C. Instruments to Study Sleep Disorders in Climacteric Women. Sleep Sci. 2016, 9, 169–178. [Google Scholar] [PubMed]
- Nordin, M.; Åkerstedt, T.; Nordin, S. Psychometric Evaluation and Normative Data for the Karolinska Sleep Questionnaire. Sleep Biol. Rhythm. 2013, 11, 216–226. [Google Scholar]
- Laverde-López, M.C.; Escobar-Córdoba, F.; Eslava-Schmalbach, J. Validation of the Colombian Version of the Karolinska Sleepiness Scale. Sleep Sci 2022, 15, 97–104. [Google Scholar]
- Shahid, A.; Wilkinson, K.; Marcu, S.; Shapiro, C.M. Shapiro. Karolinska Sleepiness Scale (Kss). In Stop, That and One Hundred Other Sleep Scales; Shahid, A., Wilkinson, K., Marcu, S., Shapiro, C.M., Eds.; Springer: New York, NY, USA, 2012; pp. 209–210. [Google Scholar]
- Montez, J.K. Us State Polarization, Policymaking Power, and Population Health. Milbank Q 2020, 98, 1033–1052. [Google Scholar] [PubMed]
- Wong, I.S.; Popkin, S.; Folkard, S. Working Time Society Consensus Statements: A Multi-Level Approach to Managing Occupational Sleep-Related Fatigue. Ind. Health 2019, 57, 228–244. [Google Scholar]
- Zhang, J.; Yu, Q.; Zheng, F.; Long, C.; Lu, Z.; Duan, Z. Comparing Keywords Plus of Wos and Author Keywords: A Case Study of Patient Adherence Research. J. Assoc. Inf. Sci. Technol. 2016, 67, 967–972. [Google Scholar]
- Kim, T.K.; Lee, H.C.; Lee, S.G.; Han, K.T.; Park, E.C. The Combined Effect of Sleep Duration and Quality on Mental Health among Republic of Korea Armed Forces. Mil. Med. 2016, 181, e1581–e1589. [Google Scholar]
- Lian, Y.; Xiao, J.; Liu, Y.; Ning, L.; Guan, S.; Ge, H.; Li, F.; Liu, J. Associations between Insomnia, Sleep Duration and Poor Work Ability. J. Psychosom. Res. 2015, 78, 45–51. [Google Scholar]
- Omachi, T.A.; Claman, D.M.; Blanc, P.D.; Eisner, M.D. Obstructive Sleep Apnea: A Risk Factor for Work Disability. Sleep 2009, 32, 791–798. [Google Scholar]
- Rae, A.J.; Provan, D.J.; Weber, D.E.; Dekker, S.W. Safety Clutter: The Accumulation and Persistence of ‘Safety’work That Does Not Contribute to Operational Safety. Policy Pract. Health Saf. 2018, 16, 194–211. [Google Scholar] [CrossRef]
- DeVon, H.A.; Block, M.E.; Moyle-Wright, P.; Ernst, D.M.; Hayden, S.J.; Lazzara, D.J.; Savoy, S.M.; Kostas-Polston, E. A Psychometric Toolbox for Testing Validity and Reliability. J. Nurs. Scholarsh. 2007, 39, 155–164. [Google Scholar] [CrossRef]
- Appleton, S.; Theorell-Haglöw, J. Why Harmonizing Cohorts in Sleep Is a Good Idea and the Labor of Doing So? Sleep 2024, 47, zsae129. [Google Scholar] [CrossRef]
- Aledavood, T.; Torous, J.; Triana Hoyos, A.M.; Naslund, J.A.; Onnela, J.-P.; Keshavan, M. Smartphone-Based Tracking of Sleep in Depression, Anxiety, and Psychotic Disorders. Curr. Psychiatry Rep. 2019, 21, 49. [Google Scholar] [CrossRef] [PubMed]
- Roos, L.G.; Slavich, G.M. Wearable Technologies for Health Research: Opportunities, Limitations, and Practical and Conceptual Considerations. Brain Behav Immun 2023, 113, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Vijayan, V.; Connolly, J.P.; Condell, J.; McKelvey, N.; Gardiner, P. Review of Wearable Devices and Data Collection Considerations for Connected Health. Sensors 2021, 21, 5589. [Google Scholar] [CrossRef]
- Jahrami, H.; Trabelsi, K.; Vitiello, M.V.; BaHammam, A.S. The Tale of Orthosomnia: I Am So Good at Sleeping That I Can Do It with My Eyes Closed and My Fitness Tracker on Me. Nat Sci Sleep 2023, 15, 13–15. [Google Scholar] [CrossRef]
- Vital-Lopez, F.G.; Balkin, T.J.; Reifman, J. Models for Predicting Sleep Latency and Sleep Duration. Sleep 2020, 44, zsaa263. [Google Scholar] [CrossRef]
- Kim, J.; Park, M. A Study on Ml-Based Sleep Score Model Using Lifelog Data. Appl. Sci. 2023, 13, 1043. [Google Scholar] [CrossRef]
- Størkersen, K.; Thorvaldsen, T.; Kongsvik, T.; Dekker, S. How Deregulation Can Become Overregulation: An Empirical Study into the Growth of Internal Bureaucracy When Governments Take a Step Back. Saf. Sci. 2020, 128, 104772. [Google Scholar] [CrossRef]
- Bieder, C.; Bourrier, M. Trapping Safety into Rules: How Desirable or Avoidable is Proceduralization? 1st ed.; CRC Press: Milton, ON, Canada, 2013. [Google Scholar]
- Takano, Y.; Ibata, R.; Nakano, N.; Sakano, Y. Association between insomnia severity and presenteeism among Japanese daytime workers. J. Sleep Res. 2023, 32, e13711. [Google Scholar] [PubMed]
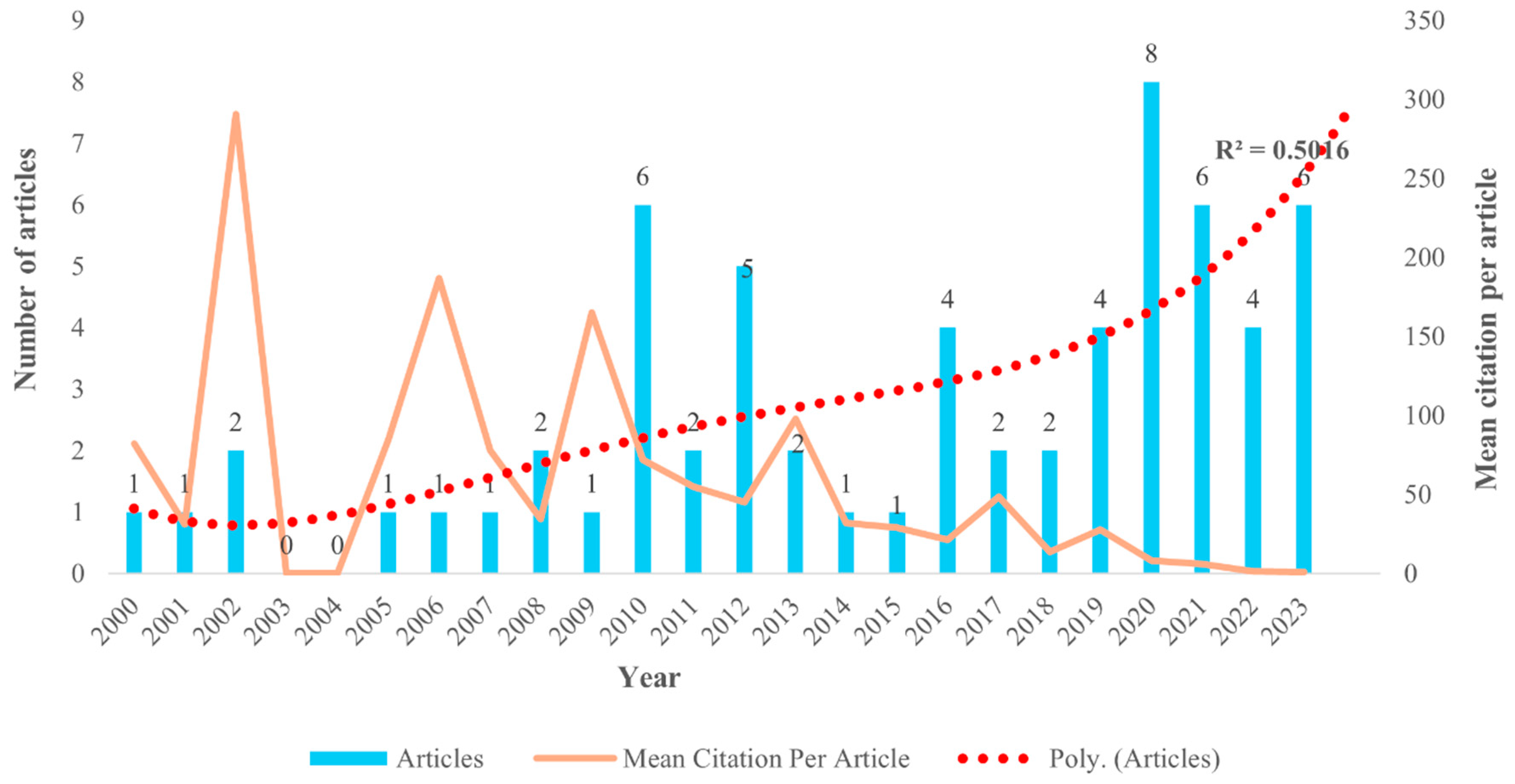
| Category | Description | Results |
|---|---|---|
| Main Information about Data | ||
| Timespan | 2000:2023 | |
| Sources (journals, books, etc.) | 45 | |
| Documents (articles) | 63 | |
| Annual growth rate for articles | 8.1 | |
| Average age per document | 8.65 | |
| Average citations per document (article) | 43.4 | |
| References | 2835 | |
| Document Contents | ||
| Keywords plus (ID) | 604 | |
| Author’s keywords (DE) | 215 | |
| Authors | ||
| Authors | 277 | |
| Authors of single-authored documents | 4 | |
| Author Collaboration | ||
| Single-authored documents | 4 | |
| Co-authors per document | 4.62 | |
| International co-authorships, % | 20.63 | |
| Document Type(s) | ||
| Journal articles | 63 |
| S/N | Article | DOI | Study Population | Local Citations (LC) | Global Citations (GC) | LC/GC Ratio (%) |
|---|---|---|---|---|---|---|
| 1 | Brossoit et al. [46] | https://doi.org/10.1037/ocp0000139 | Construction workers in the US | 5 | 50 | 10 |
| 2 | Kling et al. [60] | https://doi.org/10.1093/sleep/33.5.611 | * Cross-section of the Canadian working population | 5 | 70 | 7.41 |
| 3 | Barnes and Wagner [45] | https://doi.org/10.1037/a0015320 | Mining workers in the US | 4 | 165 | 2.42 |
| 4 | Nakata [77] | https://doi.org/10.1111/j.1365-2869.2011.00910.x | * Male employees in Tokyo | 3 | 48 | 6.25 |
| 5 | Powell and Copping [81] | https://doi.org/10.1061/(ASCE)CO.1943-7862.0000211 | Construction workers in Canada | 3 | 57 | 5.27 |
| 6 | Wilson et al. [94] | https://doi.org/10.1016/j.aap.2017.09.023 | Nurses in Saudi Arabia | 2 | 52 | 3.85 |
| 7 | Rosekind et al. [85] | https://doi.org/10.1097/JOM.0b013e3181c78c30 | * Employees across different industries in the US | 2 | 266 | 0.75 |
| 8 | Kessler et al. [59] | https://doi.org/10.5665/sleep.1884 | * Employees across different industries in the US | 2 | 72 | 2.78 |
| S/N | Article | Journal | DOI | Study Population | Total Citations (TC) | TC per Year |
|---|---|---|---|---|---|---|
| 1 | Léger et al. [63] | Sleep | https://doi.org/10.1093/sleep/25.6.621 | * Cross-section of the French working population | 386 | 16.78 |
| 2 | Rosekind et al. [85] | Journal of Workplace and Environmental Medicine | https://doi.org/10.1097/JOM.0b013e3181c78c30 | * Employees across different industries in the US | 266 | 17.73 |
| 3 | Melamed and Oksenberg [39] | Sleep | https://doi.org/10.1093/sleep/25.3.315 | * Employees across different industrial plants in Israel | 195 | 8.48 |
| 4 | Léger et al. [64] | Sleep | https://doi.org/10.1093/sleep/29.2.171 | * Cross-section of the French working population | 187 | 9.84 |
| 5 | Sneddon et al. [87] | Safety Science | https://doi.org/10.1016/j.ssci.2012.05.027 | Drilling personnel in the UK | 166 | 13.83 |
| 6 | Barnes and Wagner [45] | J Appl Psychol | https://doi.org/10.1037/a0015320 | Mining workers in the United States | 165 | 10.31 |
| 7 | Sabbagh-Ehrlich et al. [86] | Injury Prev | https://doi.org/10.1136/ip.2004.007682 | Truck drivers in Israel | 85 | 4.25 |
| 8 | Linton and Bryngelsson [67] | J Occup Rehabil | https://doi.org/10.1023/A:1009408204694 | * Employees across different industries in Sweden | 82 | 3.28 |
| 9 | Fisman et al. [56] | Infect Control Hosp Epidemiol | https://doi.org/10.1086/510569 | * Employee healthcare workers across the United States and Canada | 78 | 4.33 |
| 10 | Kessler et al. [59] | Sleep | https://doi.org/10.5665/sleep.1884 | * Employees across different industries in the US | 72 | 5.54 |
| 11 | Kling et al. [60] | Sleep | https://doi.org/10.1093/sleep/33.5.611 | * Cross-section of the Canadian working population | 70 | 4.67 |
| 12 | Aderaw et al. [14] | J Trop Med | https://doi.org/10.1155/2011/657275 | Textile factory workers in Ethiopia | 62 | 4.43 |
| 13 | Kao et al. [10] | J Occup Health Psychol | https://doi.org/10.1037/a0039144 | Construction personnel | 58 | 6.44 |
| 14 | Powell and Copping [81] | Journal of Construction Engineering and Management | https://doi.org/10.1061/(ASCE)CO.1943-7862.0000211 | Construction workers in Canada | 57 | 3.8 |
| 15 | Wilson et al. [94] | Accid Anal Prev | https://doi.org/10.1016/j.aap.2017.09.023 | Nurses in Saudi Arabia | 52 | 8.67 |
| 16 | Filtness and Naweed [55] | Applied Ergonomics | https://doi.org/10.1016/j.apergo.2016.10.009 | Train drivers in Australia and New Zealand | 52 | 6.5 |
| 17 | Brossoit et al. [46] | Journal of Workplace Health Psychology | https://doi.org/10.1037/ocp0000139 | Construction personnel in the US | 50 | 8.33 |
| S/N | Sources (Journal Outlets) | Frequency | Zone | Articles per Zone |
|---|---|---|---|---|
| 1 | International Journal of Environmental Research and Public Health | 5 | Zone 1 | 22 |
| 2 | Sleep | 5 | Zone 1 | |
| 3 | Chronobiology International | 3 | Zone 1 | |
| 4 | Journal of Workplace and Environmental Medicine | 3 | Zone 1 | |
| 5 | Journal of Workplace Health Psychology | 3 | Zone 1 | |
| 6 | Journal of Sleep Research | 3 | Zone 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nwaogu, J.M.; Chan, A.P.C.; Naslund, J.A.; Anwer, S. The Interplay Between Sleep and Safety Outcomes in the Workplace: A Scoping Review and Bibliographic Analysis of the Literature. Int. J. Environ. Res. Public Health 2025, 22, 533. https://doi.org/10.3390/ijerph22040533
Nwaogu JM, Chan APC, Naslund JA, Anwer S. The Interplay Between Sleep and Safety Outcomes in the Workplace: A Scoping Review and Bibliographic Analysis of the Literature. International Journal of Environmental Research and Public Health. 2025; 22(4):533. https://doi.org/10.3390/ijerph22040533
Chicago/Turabian StyleNwaogu, Janet Mayowa, Albert P. C. Chan, John A. Naslund, and Shahnawaz Anwer. 2025. "The Interplay Between Sleep and Safety Outcomes in the Workplace: A Scoping Review and Bibliographic Analysis of the Literature" International Journal of Environmental Research and Public Health 22, no. 4: 533. https://doi.org/10.3390/ijerph22040533
APA StyleNwaogu, J. M., Chan, A. P. C., Naslund, J. A., & Anwer, S. (2025). The Interplay Between Sleep and Safety Outcomes in the Workplace: A Scoping Review and Bibliographic Analysis of the Literature. International Journal of Environmental Research and Public Health, 22(4), 533. https://doi.org/10.3390/ijerph22040533










