Association of Parental Oral Health Knowledge and Self-Efficacy with Early Childhood Caries and Oral Health Quality of Life in Texas Schoolchildren
Abstract
1. Introduction
2. Materials and Methods
2.1. Recruitment and Sample
2.1.1. School Inclusion Criteria
2.1.2. Parent–Child Dyad Inclusion Criteria
2.1.3. Child Exclusion Criteria
2.2. Study Measures
2.2.1. Primary Outcomes
2.2.2. Child and Parent Sociodemographics
2.2.3. Child Anthropometric Measurements
2.2.4. Exposure Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- A significant association was found between parental oral health self-efficacy for their child and child active dental caries prevalence and OHQoL.
- No associations were noted for parental oral health knowledge and child active dental caries prevalence and OHQoL.
- Future research is needed to understand the mechanisms by which parental psychosocial factors influence child dental caries-related behaviors and caries risk to design and inform theory-driven behavioral interventions for dental caries prevention in young children.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OHRQoL | Oral health-related quality of life |
| ICDAS | International Caries Detection and Assessment System |
| ECOHIS | Early Childhood Oral Health Impact Scale |
| DFS/dfs | Decayed and filled surfaces in permanent and primary teeth |
| DFT/dft | Decayed and filled permanent and primary teeth |
| SCT | Social Cognitive Theory |
References
- Centers for Disease Control and Prevention. Oral Conditions–Healthy People 2030. Available online: https://odphp.health.gov/healthypeople/objectives-and-data/browse-objectives/oral-conditions (accessed on 30 January 2025).
- Huang, G.; Cao, G.; Liu, J.; Liu, M. Global trends in incidence of caries in permanent teeth of children aged 5 through 14 years, 1990 through 2019. J. Am Dent. Assoc. 2024, 155, 667–678.e21. [Google Scholar] [CrossRef] [PubMed]
- Pitts, N.B.; Twetman, S.; Fisher, J.; Marsh, P.D. Understanding Dental Caries as a Non-Communicable Disease. Br. Dent. J. 2021, 231, 749–753. [Google Scholar] [CrossRef] [PubMed]
- US. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General; National Institute of Dental and Craniofacial Research, National Institutes of Health: Bethesda, MD, USA, 2000. Available online: https://www.nidcr.nih.gov/sites/default/files/2017-10/hck1ocv.%40www.surgeon.fullrpt.pdf (accessed on 30 January 2025).
- Fleming, E.; Afful, J. Prevalence of Total and Untreated Dental Caries Among Youth: United States, 2015–2016; NCHS Data Brief No 307; National Center for Health Statistics: Hyattsville, MD, USA, 2018. Available online: https://www.cdc.gov/nchs/products/databriefs/db307.htm (accessed on 29 January 2025).
- Texas Department of State Health Services. Dental Health Data and Reporting. Texas DSHS. 2019. Available online: https://www.dshs.texas.gov/dental-health/dental-health-data-reporting (accessed on 29 January 2025).
- Do, L.G.; Spencer, A. Oral Health-Related Quality of Life of Children by Dental Caries and Fluorosis Experience. J. Public Health Dent. 2007, 67, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.M.; McGrath, C.P.; King, N.M.; Lo, E.C. Oral Health-Related Quality of Life in Hong Kong Preschool Children. Caries Res. 2011, 45, 370–376. [Google Scholar] [CrossRef]
- Kramer, P.F.; Feldens, C.A.; Ferreira, S.H.; Bervian, J.; Rodrigues, P.H.; Peres, M.A. Exploring the Impact of Oral Diseases and Disorders on Quality of Life of Preschool Children. Community Dent. Oral Epidemiol. 2013, 41, 327–335. [Google Scholar] [CrossRef]
- Krisdapong, S.; Prasertsom, P.; Rattanarangsima, K.; Sheiham, A. Associations Between Perceived Needs for Dental Treatment, Oral Health-Related Quality of Life, and Oral Diseases in School-Aged Thai Children. Community Dent. Oral Epidemiol. 2014, 42, 323–332. [Google Scholar] [CrossRef]
- Ramos-Jorge, J.; Alencar, B.M.; Pordeus, I.A.; Soares, M.E.; Marques, L.S.; Ramos-Jorge, M.L.; Paiva, S.M. Impact of Dental Caries on Quality of Life Among Preschool Children: Emphasis on the Type of Tooth and Stages of Progression. Eur. J. Oral Sci. 2015, 123, 88–95. [Google Scholar] [CrossRef]
- Fleming, P. Timetable for Oral Prevention in Childhood—A Current Opinion. Prog. Orthod. 2015, 16, 27. [Google Scholar] [CrossRef]
- Lynch, R.J. The Primary and Mixed Dentition, Post-Eruptive Enamel Maturation, and Dental Caries: A Review. Int. Dent. J. 2013, 63 (Suppl. S2), 3–13. [Google Scholar] [CrossRef]
- Pujar, P.; Subbareddy, V.V. Evaluation of the Tooth Brushing Skills in Children Aged 6–12 Years. Eur. Arch. Paediatr. Dent. 2013, 14, 213–219. [Google Scholar] [CrossRef]
- Krol, D.M.; Whelan, K.; The Section on Oral Health. Maintaining and Improving the Oral Health of Young Children. Pediatrics 2023, 151, e2022060417. [Google Scholar] [CrossRef] [PubMed]
- Chuang, R.J.; Byrd-Williams, C.; Yamal, J.M.; Johnson, K.; Kelder, S.; Nelson, S.; Mofleh, D.; Sharma, S.V. Design for a Cluster Randomized Controlled Trial to Evaluate the Effects of the CATCH Healthy Smiles School-Based Oral Health Promotion Intervention Among Elementary School Children. Contemp. Clin. Trials Commun. 2022, 30, 101033. [Google Scholar] [CrossRef]
- Sharma, S.V.; Kelder, S.; Yamal, J.M.; Chuang, R.J.; Byrd-Williams, C.; Bona, G.; Bajaj, N.; Brito, F.; Neumann, A.S. Development and Feasibility Testing of CATCH Healthy Smiles, an Oral Health Promotion Intervention for Prevention of Dental Caries Among Elementary School Children. J. Sch. Health 2022, 92, 20–30. [Google Scholar] [CrossRef]
- Ekstrand, K.R.; Gimenez, T.; Ferreira, F.R.; Mendes, F.M.; Braga, M.M. The International Caries Detection and Assessment System–ICDAS: A Systematic Review. Caries Res. 2018, 52, 406–419. [Google Scholar] [CrossRef]
- Pahel, B.T.; Rozier, R.G.; Slade, G.D. Parental Perceptions of Children’s Oral Health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2007, 5, 6. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Child and Teen BMI Categories. BMI. Available online: https://www.cdc.gov/bmi/child-teen-calculator/bmi-categories.html (accessed on 30 January 2025).
- Finlayson, T.L.; Siefert, K.; Ismail, A.I.; Delva, J.; Sohn, W. Reliability and Validity of Brief Measures of Oral Health-Related Knowledge, Fatalism, and Self-Efficacy in Mothers of African American Children. Pediatr. Dent. 2005, 27, 422–428. [Google Scholar]
- de Silva-Sanigorski, A.; Ashbolt, R.; Green, J.; Calache, H.; Keith, B.; Riggs, E.; Waters, E. Parental Self-Efficacy and Oral Health-Related Knowledge Are Associated with Parent and Child Oral Health Behaviors and Self-Reported Oral Health Status. Community Dent. Oral Epidemiol. 2013, 41, 345–352. [Google Scholar]
- Centers for Disease Control and Prevention. FastStats–Oral and Dental Health. Available online: https://www.cdc.gov/nchs/fastats/dental.htm (accessed on 30 January 2025).
- Bandura, A. Social-Cognitive Theory, 7th ed.; Psychology Press: London, UK, 2010; p. 20. ISBN 9781315793177. [Google Scholar]
- Hooley, M.; Skouteris, H.; Boganin, C.; Satur, J.; Kilpatrick, N. Parental Influence and the Development of Dental Caries in Children Aged 0–6 Years: A Systematic Review of the literature. J. Dent. 2012, 40, 873–885. [Google Scholar] [CrossRef]
- Smith, S.R.; Kroon, J.; Schwarzer, R.; Hamilton, K. Parental Social-Cognitive Correlates of Preschoolers’ Oral Hygiene Behavior: A Systematic Review and Meta-Analysis. Soc. Sci. Med. 2020, 264, 113322. [Google Scholar] [CrossRef]
- Hevel, D.J.; Henshaw, M.; Endrighi, R.; Adams, W.G.; Heeren, T.; Jankowski, A.; Borrelli, B. The Differential Predictive Utility of Two Caregiver-Targeted Self-Efficacy Measures to Promote Oral Health of Underserved Children. Health Psychol. 2023, 42, 735–745. [Google Scholar] [CrossRef]
- Wilson, A.R.; Mulvahill, M.J.; Tiwari, T. The Impact of Maternal Self-Efficacy and Oral Health Beliefs on Early Childhood Caries in Latino Children. Front Public Health. 2017, 5, 228. [Google Scholar] [CrossRef]
- Zhao, J.; Shi, H.; Wang, J.; Huang, R.; Liu, Y.; Zhang, Y.; Jiang, N.; Wang, T.; Wang, J.; Xu, X. Association of oral health knowledge, self-efficacy and behaviours with oral health-related quality of life in Chinese primary school children: A cross-sectional study. BMJ Open. 2022, 12, e062170. [Google Scholar] [CrossRef]
- Rimal, R.N. Closing the Knowledge-Behavior Gap in Health Promotion: The Mediating Role of Self-Efficacy. Health Commun. 2000, 12, 219–237. [Google Scholar] [CrossRef] [PubMed]
- Yamal, J.M.; Mofleh, D.; Chuang, R.J.; Wang, M.; Johnson, K.; Garcia-Quintana, A.; Titiloye, T.; Nelson, S.; Sharma, S.V. Training Protocol and Calibration of the International Caries Detection and Assessment System in a School-Based Clinical Trial of Elementary School-Age Children. J. Public Health Dent. 2024, 85, 13–20. [Google Scholar] [CrossRef] [PubMed]

| Overall (N = 1084) | No Active Lesions a (N = 529) | Active Lesions a (N = 554) | p Value | |
|---|---|---|---|---|
| Child age | ||||
| Mean (SD) | 5.46 (0.554) | 5.46 (0.536) | 5.45 (0.570) | 0.578 |
| Median [Q1, Q3] | 5.00 [5.00, 6.00] | 5.00 [5.00, 6.00] | 5.00 [5.00, 6.00] | |
| Child gender | ||||
| Female | 546 (51.4%) | 270 (52.5%) | 276 (50.4%) | 0.52 |
| Male | 517 (48.6%) | 244 (47.5%) | 272 (49.6%) | |
| Child ethnicity | ||||
| Black or African American | 212 (22.6%) | 110 (24.2%) | 102 (21.2%) | 0.358 b |
| Mexican American, Latino, or Hispanic | 663 (70.8%) | 315 (69.4%) | 347 (72.0%) | |
| White, Caucasian, or Anglo | 42 (4.5%) | 23 (5.1%) | 19 (3.9%) | |
| Asian | 7 (0.7%) | 2 (0.4%) | 5 (1.0%) | |
| Other | 13 (1.4%) | 4 (0.8%) | 9 (1.9%) | |
| Parent age | ||||
| Mean (SD) | 33.1 (7.75) | 33.5 (7.63) | 32.7 (7.86) | 0.114 |
| Median [Q1, Q3] | 32.0 [28.0, 37.0] | 32.0 [28.0, 38.0] | 32.0 [27.0, 37.0] | |
| Parent gender | ||||
| Female | 784 (88.3%) | 390 (90.7%) | 394 (86.0%) | 0.039 * |
| Male | 104 (11.7%) | 40 (9.3%) | 64 (14.0%) | |
| Parent ethnicity | ||||
| Black or African American | 191 (21.8%) | 95 (22.4%) | 96 (21.1%) | 0.009 b |
| Mexican American, Latino, or Hispanic | 638 (72.6%) | 307 (72.4%) | 330 (72.7%) | |
| White, Caucasian, or Anglo | 29 (3.3%) | 19 (4.5%) | 10 (2.2%) | |
| Asian | 9 (1.0%) | 1 (0.2%) | 8 (1.8%) | |
| Other | 12 (1.4%) | 2 (0.5%) | 10 (2.2%) | |
| Language spoken at home | ||||
| Only English | 284 (29.6%) | 144 (30.7%) | 140 (28.6%) | 0.388 |
| More English than another | 125 (13.0%) | 66 (14.1%) | 59 (12.1%) | |
| Both English and another | 148 (15.4%) | 71 (15.1%) | 77 (15.7%) | |
| More another than English | 107 (11.2%) | 43 (9.2%) | 63 (12.9%) | |
| Only another | 295 (30.8%) | 145 (30.9%) | 150 (30.7%) | |
| Parent education | ||||
| Never attended school or only attended kindergarten | 47 (5.3%) | 20 (4.6%) | 27 (5.9%) | 0.588 |
| Grades 1 through 8 (elementary) | 103 (11.5%) | 52 (12.0%) | 51 (11.1%) | |
| Grades 9 through 11 (some high school) | 131 (14.7%) | 59 (13.6%) | 72 (15.7%) | |
| Grades 12 or GED (high school graduate) | 337 (37.7%) | 170 (39.3%) | 167 (36.4%) | |
| College 1 year to 3 years (some college or technical school) | 205 (23.0%) | 94 (21.7%) | 111 (24.2%) | |
| College 4 years or more (college graduate) | 70 (7.7%) | 38 (8.8%) | 31 (6.8%) | |
| Parent employment status | ||||
| Employed for wages | 351 (42.8%) | 181 (45.6%) | 170 (40.2%) | 0.627 b |
| Self-employed | 56 (6.8%) | 26 (6.5%) | 30 (7.1%) | |
| Out of work for less than 1 year | 30 (3.7%) | 12 (3.0%) | 18 (4.3%) | |
| Out of work for more than 1 year | 45 (5.5%) | 20 (5.0%) | 25 (5.9%) | |
| Homemaker | 274 (33.4%) | 128 (32.2%) | 145 (34.3%) | |
| Employed in seasonal labor | 24 (2.9) | 11 (2.8%) | 13 (3.1%) | |
| Retired | 3 (0.4%) | 0 (0%) | 3 (0.7%) | |
| Unable to work | 38 (4.6%) | 19 (4.8%) | 19 (4.5%) | |
| Parent income | ||||
| Less than 10,000 | 176 (26.9%) | 83 (25.6%) | 92 (27.9%) | 0.915 |
| 10,001 to 15,000 | 85 (13.0%) | 39 (12.0%) | 46 (13.9%) | |
| 15,001 to 20,000 | 67 (10.2%) | 35 (10.8%) | 32 (9.7%) | |
| 20,001 to 25,000 | 69 (10.5%) | 37 (11.4%) | 32 (9.7%) | |
| 25,001 to 35,000 | 102 (15.6%) | 49 (15.1%) | 53 (16.1%) | |
| 35,001 to 50,000 | 93 (14.2%) | 47 (14.5%) | 46 (13.9%) | |
| 50,001 to 75,000 or greater | 63 (9.6%) | 34 (10.5%) | 29 (8.8%) | |
| Household members | ||||
| Mean (SD) | 4.89 (1.73) | 4.88 (1.73) | 4.91 (1.74) | 0.832 |
| Median [Q1, Q3] | 5.00 [4.00, 6.00] | 5.00 [4.00, 6.00] | 5.00 [4.00, 6.00] | |
| Assistance programs | ||||
| No | 166 (18.8%) | 64 (15.0%) | 102 (22.4%) | 0.00624 |
| Yes | 719 (81.2%) | 364 (85.0%) | 354 (77.6%) | |
| Child BMI | ||||
| Underweight | 30 (2.8%) | 14 (2.7%) | 16 (2.9%) | 0.758 |
| Healthy weight | 633 (59.7%) | 299 (58.3%) | 334 (61.2%) | |
| Overweight | 190 (17.9%) | 97 (18.9%) | 92 (16.8%) | |
| Obese | 207 (19.5%) | 103 (20.1%) | 104 (19.0%) | |
| Child QOL (ECOHIS) | ||||
| Mean (SD) | 2.61 (3.84) | 1.97 (2.84) | 3.24 (4.55) | <0.001 * |
| Median [Q1, Q3] | 1.00 [0, 3.00] | 1.00 [0, 2.00] | 2.00 [0, 4.00] | |
| Parent QOL (ECOHIS) | ||||
| Mean (SD) | 1.12 (2.04) | 0.760 (1.46) | 1.48 (2.43) | <0.001 * |
| Median [Q1, Q3] | 0 [0, 2.00] | 0 [0, 1.00] | 0 [0, 2.00] | |
| Missed school days | ||||
| Mean (SD) | 0.47 (1.16) | 0.419 (0.989) | 0.519 (1.30) | 0.542 |
| Median [Q1, Q3] | 0 [0, 0] | 0 [0, 0] | 0 [0, 0] | |
| Child’s brushing frequency | ||||
| Never | 6 (0.8%) | 3 (0.8%) | 3 (0.8%) | 0.842 b |
| Less than once a week | 6 (0.8%) | 2 (0.6%) | 4 (1.1%) | |
| At least once a week but not everyday | 51 (7.2%) | 23 (6.4%) | 28 (7.9%) | |
| Once a day | 280 (39.3%) | 140 (39.1%) | 139 (39.4%) | |
| More than once a day | 369 (51.8%) | 190 (53.1%) | 179 (50.7%) | |
| Child’s last dentist visit | ||||
| In the last year | 541 (76.5%) | 304 (84.7%) | 236 (68.0%) | <0.001 * |
| More than 1 year ago but less than 2 years ago | 67 (9.5%) | 17 (4.7%) | 50 (14.4%) | |
| More than 2 years ago | 39 (5.5%) | 15 (4.2%) | 24 (6.9%) | |
| Never have been | 60 (8.5%) | 23 (6.4%) | 37 (10.7%) | |
| Parental knowledge score | ||||
| Mean (SD) | 4.18 (0.765) | 4.24 (0.784) | 4.12 (0.742) | 0.00326 * |
| Median [Q1, Q3] | 4.17 [3.83, 5.00] | 4.33 [4.00, 5.00] | 4.00 [3.67, 4.83] | |
| Parental self-efficacy score | ||||
| Mean (SD) | 14.8 (3.50) | 15.2 (3.41) | 14.4 (3.55) | 0.0029 * |
| Median [Q1, Q3] | 15.0 [13.0, 17.0] | 15.0 [13.0, 18.0] | 15.0 [13.0, 17.0] |
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Estimate [95% CI] | p Value | Estimate [95% CI] | p Value | |
| Parental oral knowledge score | −0.45 [−0.81, −0.08] | 0.02 * | −0.19 [−0.6, 0.22] a | 0.37 |
| Parental self-efficacy score | −0.21 [−0.29, −0.14] | <0.01 * | −0.16 [−0.24, −0.09] b | <0.01 * |
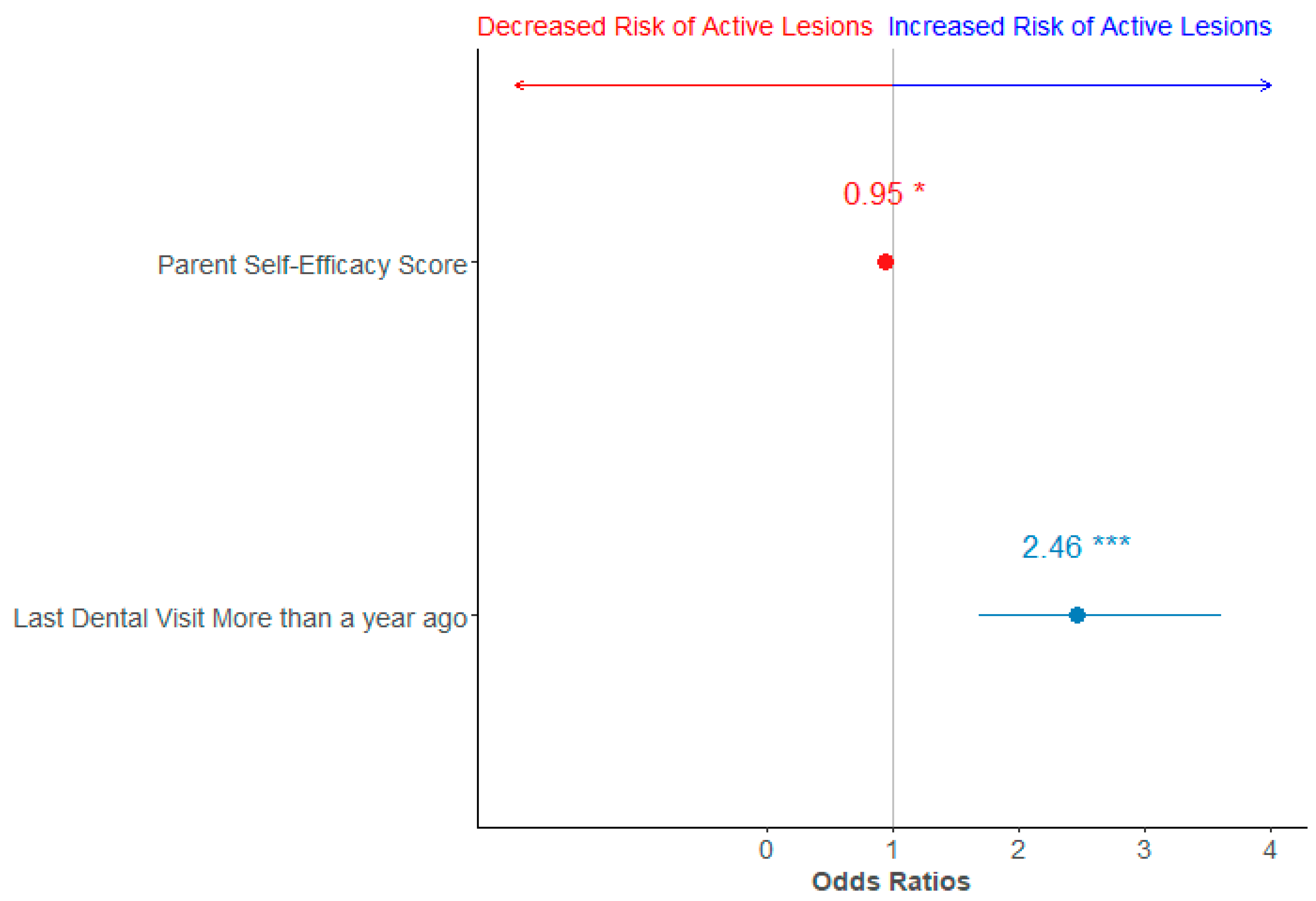
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Odds Ratio [95% CI] | p Value | Odds Ratio [95% CI] | p Value | |
| Parental oral knowledge score | 0.8 [0.66, 0.98] | 0.03 * | 0.91 [0.69, 1.2] a | 0.5 |
| Parental self-efficacy score | 0.93 [0.89, 0.98] | <0.01 * | 0.95 [0.9, 0.99] b | 0.02 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, S.V.; Deason, J.E.; Wang, M.; Garcia-Quintana, A.; Chuang, R.-J.; Johnson, K.; Garner, S.; Kelder, S.; Yamal, J.-M. Association of Parental Oral Health Knowledge and Self-Efficacy with Early Childhood Caries and Oral Health Quality of Life in Texas Schoolchildren. Int. J. Environ. Res. Public Health 2025, 22, 513. https://doi.org/10.3390/ijerph22040513
Sharma SV, Deason JE, Wang M, Garcia-Quintana A, Chuang R-J, Johnson K, Garner S, Kelder S, Yamal J-M. Association of Parental Oral Health Knowledge and Self-Efficacy with Early Childhood Caries and Oral Health Quality of Life in Texas Schoolchildren. International Journal of Environmental Research and Public Health. 2025; 22(4):513. https://doi.org/10.3390/ijerph22040513
Chicago/Turabian StyleSharma, Shreela V., Jeanette E. Deason, Mengxi Wang, Alejandra Garcia-Quintana, Ru-Jye Chuang, Kila Johnson, Shalisa Garner, Steven Kelder, and Jose-Miguel Yamal. 2025. "Association of Parental Oral Health Knowledge and Self-Efficacy with Early Childhood Caries and Oral Health Quality of Life in Texas Schoolchildren" International Journal of Environmental Research and Public Health 22, no. 4: 513. https://doi.org/10.3390/ijerph22040513
APA StyleSharma, S. V., Deason, J. E., Wang, M., Garcia-Quintana, A., Chuang, R.-J., Johnson, K., Garner, S., Kelder, S., & Yamal, J.-M. (2025). Association of Parental Oral Health Knowledge and Self-Efficacy with Early Childhood Caries and Oral Health Quality of Life in Texas Schoolchildren. International Journal of Environmental Research and Public Health, 22(4), 513. https://doi.org/10.3390/ijerph22040513






