Electronic Personal Health Records for Mobile Populations: A Rapid Systematic Literature Review
Abstract
1. Introduction
Rationale
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
2.4. Grey Literature
2.5. Synthesis of Results
2.6. Ethical Review Statement
2.7. Patient and Public Involvement Statement
3. Results
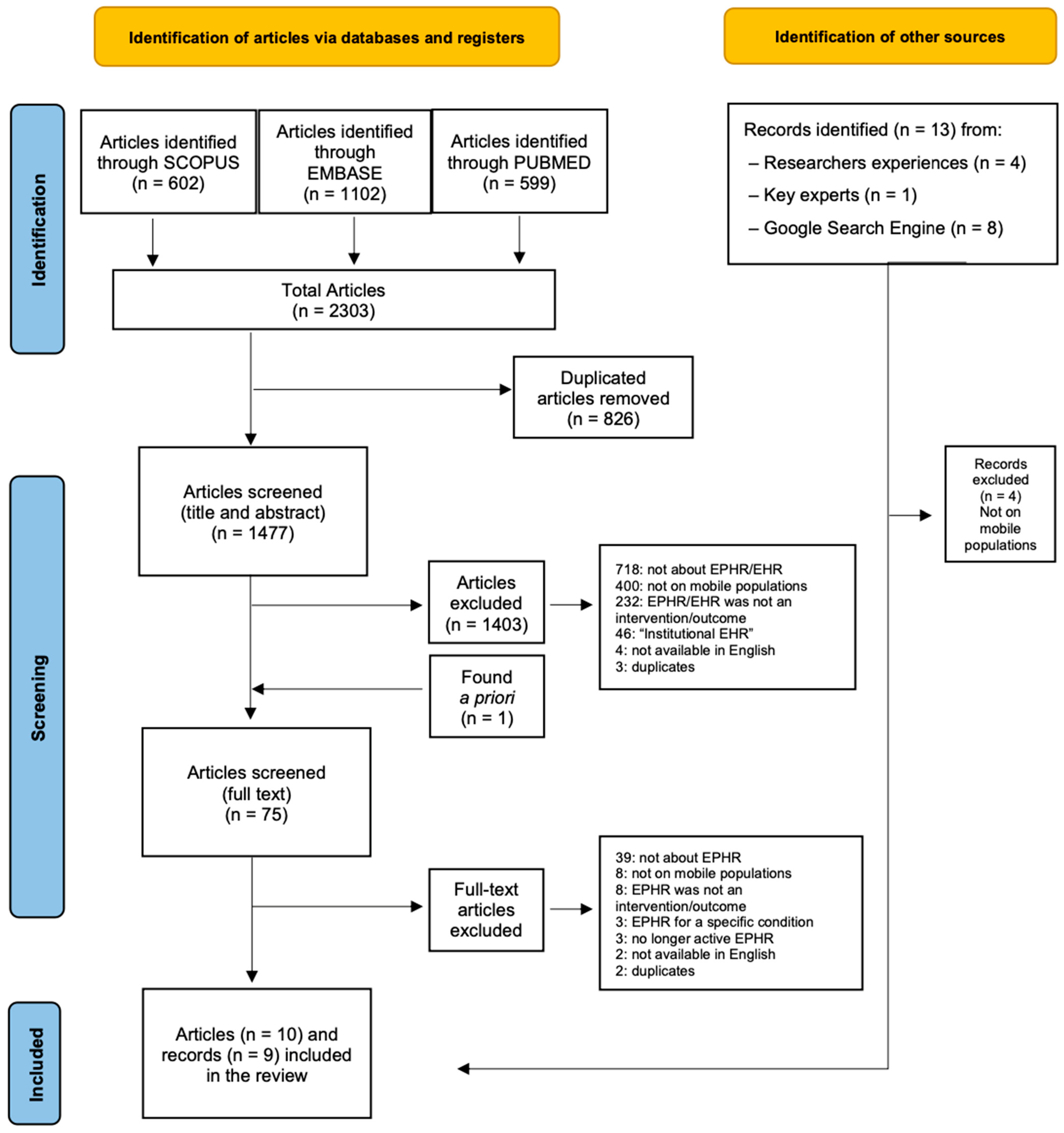
3.1. Literature
3.1.1. Results from Eligible Peer-Reviewed Publications
3.1.2. Results from Grey Literature
3.2. Initiatives
3.2.1. Main Characteristics of the Tools Identified
Mobile Populations
Countries Covered, Stage of Development, and Number of Users
Languages
Tool Description
Partnerships, Ownership, and Funding
3.2.2. Medical Information and Data Management
Health Data Stored in the Tools
Data Entry
Data Sharing
Data Storage, Security, and Offline Accessibility
3.2.3. User Experiences of the Tools Identified (Including Health-Related Outcomes)
3.2.4. User Engagement in Tool Development
4. Discussion
4.1. Discussion of Key Findings
4.1.1. Centralization of Health Records and Other Functionalities
4.1.2. Different Degrees of Patient Autonomy
4.1.3. User-Adoption Remains a Critical Challenge
4.1.4. Data Security Is a Key Priority for EPHRs Creators and Users
4.2. Implications for Research and Practice
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. PRISMA Checklist for Systematic Reviews [68]
| Section and Topic | Item # | Checklist Item | Location Where Item Is Reported |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a systematic review. | p. 1 |
| ABSTRACT | |||
| Abstract | 2 | See the PRISMA 2020 for Abstracts checklist. | p. 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of existing knowledge. | p. 1–4 |
| Objectives | 4 | Provide an explicit statement of the objective(s) or question(s) the review addresses. | p. 4 |
| METHODS | |||
| Eligibility criteria | 5 | Specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses. | p. 4 |
| Information sources | 6 | Specify all databases, registers, websites, organizations, reference lists, and other sources searched or consulted to identify studies. Specify the date when each source was last searched or consulted. | p. 4 |
| Search strategy | 7 | Present the full search strategies for all databases, registers, and websites, including any filters and limits used. | Appendix B |
| Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and if applicable, details of automation tools used in the process. | p. 4 |
| Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators, and if applicable, details of automation tools used in the process. | p. 4–5 |
| Data items | 10a | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g., for all measures, time points, analyses), and if not, the methods used to decide which results to collect. | p. 5 |
| 10b | List and define all other variables for which data were sought (e.g., participant and intervention characteristics, funding sources). Describe any assumptions made about any missing or unclear information. | p. 5 | |
| Study risk of bias assessment | 11 | Specify the methods used to assess risk of bias in the included studies, including details of the tool(s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process. | p. 5 |
| Effect measures | 12 | Specify for each outcome the effect measure(s) (e.g., risk ratio, mean difference) used in the synthesis or presentation of results. | NA |
| Synthesis methods | 13a | Describe the processes used to decide which studies were eligible for each synthesis (e.g., tabulating the study intervention characteristics and comparing against the planned groups for each synthesis (item #5)). | p. 5 |
| 13b | Describe any methods required to prepare the data for presentation or synthesis, such as handling of missing summary statistics, or data conversions. | NA | |
| 13c | Describe any methods used to tabulate or visually display results of individual studies and syntheses. | NA | |
| 13d | Describe any methods used to synthesize results and provide a rationale for the choice(s). If meta-analysis was performed, describe the model(s), method(s) to identify the presence and extent of statistical heterogeneity, and software package(s) used. | p. 5 | |
| 13e | Describe any methods used to explore possible causes of heterogeneity among study results (e.g., subgroup analysis, meta-regression). | NA | |
| 13f | Describe any sensitivity analyses conducted to assess robustness of the synthesized results. | NA | |
| Reporting bias assessment | 14 | Describe any methods used to assess risk of bias due to missing results in a synthesis (arising from reporting biases). | NA |
| Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome. | NA |
| RESULTS | |||
| Study selection | 16a | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram. | p. 5–16 |
| 16b | Cite studies that might appear to meet the inclusion criteria, but which were excluded, and explain why they were excluded. | p. | |
| Study characteristics | 17 | Cite each included study and present its characteristics. | p. 10 |
| Risk of bias in studies | 18 | Present assessments of risk of bias for each included study. | NA |
| Results of individual studies | 19 | For all outcomes, present, for each study (a) a summary of the statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g., confidence/credible interval), ideally using structured tables or plots. | NA |
| Results of syntheses | 20a | For each synthesis, briefly summarize the characteristics and risk of bias among contributing studies. | NA |
| 20b | Present results of all statistical syntheses conducted. If meta-analysis was performed, present for each the summary estimate and its precision (e.g., confidence/credible interval) and measures of statistical heterogeneity. If comparing groups, describe the direction of the effect. | NA | |
| 20c | Present results of all investigations of possible causes of heterogeneity among study results. | NA | |
| 20d | Present results of all sensitivity analyses conducted to assess the robustness of the synthesized results. | NA | |
| Reporting biases | 21 | Present assessments of risk of bias due to missing results (arising from reporting biases) for each synthesis assessed. | NA |
| Certainty of evidence | 22 | Present assessments of certainty (or confidence) in the body of evidence for each outcome assessed. | NA |
| DISCUSSION | |||
| Discussion | 23a | Provide a general interpretation of the results in the context of other evidence. | p. 16 |
| 23b | Discuss any limitations of the evidence included in the review. | p. 16–19 | |
| 23c | Discuss any limitations of the review processes used. | p. 20 | |
| 23d | Discuss implications of the results for practice, policy, and future research. | p. 19 | |
| OTHER INFORMATION | |||
| Registration and protocol | 24a | Provide registration information for the review, including register name and registration number, or state that the review was not registered. | p. 4 |
| 24b | Indicate where the review protocol can be accessed, or state that a protocol was not prepared. | p. 4 | |
| 24c | Describe and explain any amendments to information provided at registration or in the protocol. | NA | |
| Support | 25 | Describe sources of financial or non-financial support for the review, and the role of the funders or sponsors in the review. | p. 21 |
| Competing interests | 26 | Declare any competing interests of review authors. | p. 21 |
| Availability of data, code and other materials | 27 | Report which of the following are publicly available and where they can be found, including template data collection forms, data extracted from the included studies, data used for all analyses, analytic code, and any other materials used in the review. | NA |
Appendix B. Search Queries Used for Each Database
| Pubmed |
|---|
| ((((((((((((((((((((((migrant*[Title/Abstract]) OR (”mobile population*”[Title/Abstract])) OR (refugee*[Title/Abstract])) OR (”asylum seeker*” [Title/Abstract])) OR (”new comer*”[Title/Abstract])) OR (newcomer*[Title/Abstract])) OR (emigrant*[Title/Abstract])) OR (”people on the move”[Title/Abstract]))) OR (”unaccompanied minor*”[Title/Abstract])) OR (”internally displaced*”[Title/Abstract])) OR (”stateless*”[Title/Abstract])) OR (”seasonal worker*”[Title/Abstract])) OR (”temporary foreign worker*”[Title/Abstract])) OR (”international student*”[Title/Abstract])) OR (”medical tourist*”[Title/Abstract])) OR (”expatriate*”[Title/Abstract])) OR (”expat*”[Title/Abstract])) OR (”homeless*”[Title/Abstract])) OR (nomad*[Title/Abstract])) OR (”Emigrants and Immigrants”[Mesh])) OR ((”Refugees”[Mesh]) OR ”Transients and Migrants”[Mesh]) OR (”Medical Tourism”[Mesh]) OR (”Ill-Housed Persons”[Mesh]))AND (((((((((((((((((((((((Electronic Personal Health Record*[Title/Abstract]) OR (Personal Electronic Health Record*[Title/Abstract])) OR (Digital Personal Health Record*[Title/Abstract])) OR (Personal Digital Health Record*[Title/Abstract])) OR (EPHR[Title/Abstract])) OR (Mobile Personal Health Record*[Title/Abstract])) OR (Personal Mobile Health Record*[Title/Abstract])) OR (Digital Patient Held Record*[Title/Abstract])) OR (Electronic Patient Held Record*[Title/Abstract])) OR (Mobile Patient Held Record*[Title/Abstract])) OR (Electronic Personal Medical Record*[Title/Abstract])) OR (Personal Electronic Medical Record*[Title/Abstract])) OR (Digital Personal Medical Record*[Title/Abstract])) OR (Personal Digital Medical Record*[Title/Abstract])) OR (Mobile Personal Medical Record*[Title/Abstract])) OR (Personal Mobile Medical Record*[Title/Abstract])) OR (Mobile health record*[Title/Abstract])) OR (Personal Health Platform*[Title/Abstract])) OR (Patient-Controlled Health Record*[Title/Abstract])) OR (Electronic Patient Portal*[Title/Abstract])) OR (Patient Portal*[Title/Abstract]) OR (Telemedicine[Title/Abstract]) OR (eHealth[Title/Abstract]) OR (mHealth[Title/Abstract]) OR (digital health platform[Title/Abstract]) OR (health information system[Title/Abstract]) OR (health information exchange[Title/Abstract])) OR (”Electronic Health Records”[Mesh])) OR (”Telemedicine”[Mesh])) |
| Total items: 599 |
| Scopus |
|---|
| (TITLE-ABS-KEY (“Electronic Personal Health Record” OR “Personal Electronic Health Record” OR “Digital Personal Health Record” OR “Personal Digital Health Record” OR “EPHR” OR “Mobile Personal Health Record” OR “Personal Mobile Health Record” OR “Digital Patient Held Record” OR “Electronic Patient Held Record” OR “Mobile Patient Held Record” OR “Electronic Personal Medical Record” OR “Personal Electronic Medical Record” OR “Digital Personal Medical Record” OR “Personal Digital Medical Record” OR “Mobile Personal Medical Record” OR “Personal Mobile Medical Record” OR “Telemedicine” OR “Health information system” OR “Mobile health record” OR “eHealth” OR “mHealth” OR “Personal Health Platform” OR “Health Information Exchange” OR “Patient-Controlled Health Record” OR “Digital Health Platform” OR “Patient Portal”)) AND (TITLE-ABS-KEY (“migrant*” OR “mobile population*” OR “refugee*” OR “asylum seeker” OR “Internally displaced person*” OR “New comer*” OR “Newcomer*” OR “Emigrant*” OR “person on the move” OR “People on the move” OR “Stranded” OR “Unaccompanied minor” OR “Internally displaced*” OR “Stateless person” OR “Seasonal worker*” OR “Temporary Foreign Worker*” OR “International student*” OR “Medical tourist*” OR “Expat*” OR “Homeless*” OR “Nomad*”)) |
| Total items: 602 |
| Embase |
|---|
| (‘electronic personal health record’:ab,kw,ti OR ‘personal electronic health record’:ab,kw,ti OR ‘digital personal health record’:ab,kw,ti OR ‘personal digital health record’:ab,kw,ti OR ‘ephr’:ab,kw,ti OR ‘mobile personal health record’:ab,kw,ti OR ‘personal mobile health record’:ab,kw,ti OR ‘patient held record’:ab,kw,ti OR ‘electronic patient held record’:ab,kw,ti OR ‘mobile patient held record’:ab,kw,ti OR ‘electronic personal medical record’:ab,kw,ti OR ‘personal electronic medical record’:ab,kw,ti OR ‘digital personal medical record’:ab,kw,ti OR ‘personal digital medical record’:ab,kw,ti OR ‘mobile personal medical record’:ab,kw,ti OR ‘personal mobile medical record’:ab,kw,ti OR ‘telemedicine’:ab,kw,ti OR ‘health information system’:ab,kw,ti OR ‘mobile health record’:ab,kw,ti OR ‘ehealth’:ab,kw,ti OR ‘mhealth’:ab,kw,ti OR ‘personal health platform’:ab,kw,ti OR ‘health information exchange’:ab,kw,ti OR ‘patient-controlled health record’:ab,kw,ti OR ‘digital health platform’:ab,kw,ti OR ‘patient portal’:ab,kw,ti OR ‘telemedicine’/exp OR ‘electronic medical record’/exp OR ‘mhealth’/exp OR ‘telehealth’/exp) AND (‘migrant*’:ab,kw,ti OR ‘mobile population*’:ab,kw,ti OR ‘refugee*’:ab,kw,ti OR ‘asylum seeker’:ab,kw,ti OR ‘internally displaced person*’:ab,kw,ti OR ‘new comer*’:ab,kw,ti OR ‘newcomer*’:ab,kw,ti OR ‘emigrant*’:ab,kw,ti OR ‘person on the move’:ab,kw,ti OR ‘people on the move’:ab,kw,ti OR ‘stranded’:ab,kw,ti OR ‘unaccompanied minor’:ab,kw,ti OR ‘internally displaced*’:ab,kw,ti OR ‘stateless person’:ab,kw,ti OR ‘seasonal worker*’:ab,kw,ti OR ‘temporary foreign worker*’:ab,kw,ti OR ‘international student*’:ab,kw,ti OR ‘medical tourist*’:ab,kw,ti OR ‘expat*’:ab,kw,ti OR ‘homeless*’:ab,kw,ti OR ‘nomad*’:ab,kw,ti OR ‘statelessness’/exp OR ‘homeless person’/exp OR ‘migrant’/exp OR ‘refugee’/exp OR ‘asylum seeker’/exp OR ‘medical tourism’/exp) |
| Total items: 1102 |
| Studies Retrieved from Handsearching References |
|---|
| van de Vijver S, Tensen P, Asiki G, Requena-Méndez A, Heidenrijk M, Stronks K, Cobelens F, Bont J, Agyemang C. Digital health for all: How digital health could reduce inequality and increase universal health coverage. Digit Health. 2023 Jul 7;9:20552076231185434. doi: 10.1177/20552076231185434. |
| Total items: 1 |
| Grey Literature |
|---|
| Google Search Engine: 1 Via key experts: 1 Via experiences: 5 |
| Total items: 7 |
References
- Fundamentals of Migration. Available online: https://www.iom.int/fundamentals-migration (accessed on 3 January 2025).
- The International Organization for Migration. World Migration Report 2024; The International Organization for Migration: Grand Sacconai, Switzerland, 2024. [Google Scholar]
- UNHCR. UNHCR Global Trends Report 2023; UNHCR: Geneva, Switzerland, 2024. [Google Scholar]
- Abubakar, I.; Aldridge, R.W.; Devakumar, D.; Orcutt, M.; Burns, R.; Barreto, M.L.; Dhavan, P.; Fouad, F.M.; Groce, N.; Guo, Y.; et al. The UCL–Lancet Commission on Migration and Health: The Health of a World on the Move. Lancet 2018, 392, 2606–2654. [Google Scholar] [CrossRef] [PubMed]
- Binagwaho, A.; Mathewos, K. The Right to Health. Health Hum. Rights 2023, 25, 133–135. [Google Scholar]
- Chiesa, V.; Chiarenza, A.; Mosca, D.; Rechel, B. Health Records for Migrants and Refugees: A Systematic Review. Health Policy 2019, 123, 888–900. [Google Scholar] [CrossRef] [PubMed]
- Chiarenza, A.; Dauvrin, M.; Chiesa, V.; Baatout, S.; Verrept, H. Supporting Access to Healthcare for Refugees and Migrants in European Countries under Particular Migratory Pressure. BMC Health Serv. Res. 2019, 19, 513. [Google Scholar] [CrossRef]
- Winters, M.; Rechel, B.; de Jong, L.; Pavlova, M. A Systematic Review on the Use of Healthcare Services by Undocumented Migrants in Europe. BMC Health Serv. Res. 2018, 18, 30. [Google Scholar] [CrossRef]
- Alonso, V.; Santos, J.V.; Pinto, M.; Ferreira, J.; Lema, I.; Lopes, F.; Freitas, A. Health Records as the Basis of Clinical Coding: Is the Quality Adequate? A Qualitative Study of Medical Coders’ Perceptions. HIM J. 2020, 49, 28–37. [Google Scholar] [CrossRef]
- Suphanchaimat, R.; Kantamaturapoj, K.; Putthasri, W.; Prakongsai, P. Challenges in the Provision of Healthcare Services for Migrants: A Systematic Review through Providers’ Lens. BMC Health Serv. Res. 2015, 15, 390. [Google Scholar] [CrossRef]
- Kerr, G.; Kulshreshtha, N.; Greenfield, G.; Li, E.; Beaney, T.; Hayhoe, B.W.J.; Car, J.; Clavería, A.; Collins, C.; Espitia, S.M.; et al. Features and Frequency of Use of Electronic Health Records in Primary Care across 20 Countries: A Cross-Sectional Study. Public Health 2024, 233, 45–53. [Google Scholar] [CrossRef]
- GSMA. GSMA Annual Report 2023; GSMA: Atlanta, GA, USA, 2024. [Google Scholar]
- UNESCO. The UNESCO Courier Stories of Migration; UNESCO: Paris, France, 2021. [Google Scholar]
- Unwin, T.; Ghimire, A.; Yeoh, S.-G.; Lorini, M.R.; Harindranath, G.H. Uses of Digital Technologies by Nepali Migrants and Their Families; UNESCO: Paris, France, 2021. [Google Scholar]
- Benson, J.; Brand, T.; Christianson, L.; Lakeberg, M. Localisation of Digital Health Tools Used by Displaced Populations in Low and Middle-Income Settings: A Scoping Review and Critical Analysis of the Participation Revolution. Confl. Health 2023, 17, 20. [Google Scholar] [CrossRef]
- van de Vijver, S.; Tensen, P.; Asiki, G.; Requena-Méndez, A.; Heidenrijk, M.; Stronks, K.; Cobelens, F.; Bont, J.; Agyemang, C. Digital Health for All: How Digital Health Could Reduce Inequality and Increase Universal Health Coverage. Digit. Health 2023, 9, 20552076231185434. [Google Scholar] [CrossRef]
- Ashworth, H.; Ebrahim, S.; Ebrahim, H.; Bhaiwala, Z.; Chilazi, M. A Free, Open-Source, Offline Digital Health System for Refugee Care. JMIR Med. Inform. 2022, 10, e33848. [Google Scholar] [CrossRef] [PubMed]
- Zenner, D.; Méndez, A.R.; Schillinger, S.; Val, E.; Wickramage, K. Health and Illness in Migrants and Refugees Arriving in Europe: Analysis of the Electronic Personal Health Record System. J. Travel Med. 2022, 29, taac035. [Google Scholar] [CrossRef] [PubMed]
- Markle Foundation. Connecting Americans to Their Healthcare: Final Report—Working Group on Policies for Electronic Information Sharing Between Doctors and Patients; Markle Foundation: New York, NY, USA, 2004. [Google Scholar]
- Essén, A.; Scandurra, I.; Gerrits, R.; Humphrey, G.; Johansen, M.A.; Kierkegaard, P.; Koskinen, J.; Liaw, S.-T.; Odeh, S.; Ross, P.; et al. Patient Access to Electronic Health Records: Differences across Ten Countries. Health Policy Technol. 2018, 7, 44–56. [Google Scholar] [CrossRef]
- Feeney, O.; Werner-Felmayer, G.; Siipi, H.; Frischhut, M.; Zullo, S.; Barteczko, U.; Øystein Ursin, L.; Linn, S.; Felzmann, H.; Krajnović, D.; et al. European Electronic Personal Health Records Initiatives and Vulnerable Migrants: A Need for Greater Ethical, Legal and Social Safeguards. Dev. World Bioeth. 2020, 20, 27–37. [Google Scholar] [CrossRef]
- Damen, D.J.; Schoonman, G.G.; Maat, B.; Habibović, M.; Krahmer, E.; Pauws, S. Patients Managing Their Medical Data in Personal Electronic Health Records: Scoping Review. J. Med. Internet Res. 2022, 24, e37783. [Google Scholar] [CrossRef]
- Brands, M.R.; Gouw, S.C.; Beestrum, M.; Cronin, R.M.; Fijnvandraat, K.; Badawy, S.M. Patient-Centered Digital Health Records and Their Effects on Health Outcomes: Systematic Review. J. Med. Internet Res. 2022, 24, e43086. [Google Scholar] [CrossRef]
- Matlin, S.A.; Hanefeld, J.; Corte-Real, A.; da Cunha, P.R.; de Gruchy, T.; Manji, K.N.; Netto, G.; Nunes, T.; Şanlıer, İ.; Takian, A.; et al. Digital Solutions for Migrant and Refugee Health: A Framework for Analysis and Action. Lancet Reg. Health—Eur. 2025, 50, 101190. [Google Scholar] [CrossRef]
- Buford, A.; Ashworth, H.C.; Ezzeddine, F.L.; Dada, S.; Nguyen, E.; Ebrahim, S.; Zhang, A.; Lebovic, J.; Hamvas, L.; Prokop, L.J.; et al. Systematic Review of Electronic Health Records to Manage Chronic Conditions among Displaced Populations. BMJ Open 2022, 12, e056987. [Google Scholar] [CrossRef]
- Joseph, L.; Lavis, A.; Greenfield, S.; Boban, D.; Humphries, C.; Jose, P.; Jeemon, P.; Manaseki-Holland, S. Systematic Review on the Use of Patient-Held Health Records in Low-Income and Middle-Income Countries. BMJ Open 2021, 11, e046965. [Google Scholar] [CrossRef]
- Ballout, G.; Al-Shorbaji, N.; Abu-Kishk, N.; Turki, Y.; Zeidan, W.; Seita, A. UNRWA’s Innovative e-Health for 5 Million Palestine Refugees in the Near East. BMJ Innov. 2018, 4, 128–134. [Google Scholar] [CrossRef]
- Saleh, S.; Arnaout, N.E.; Faulkner, J.R.; Sayegh, M.H. Sijilli: A Mobile Electronic Health Records System for Refugees in Low-Resource Settings. Lancet Glob. Health 2019, 7, e1168–e1169. [Google Scholar] [CrossRef]
- Narla, N.P.; Surmeli, A.; Kivlehan, S.M. Agile Application of Digital Health Interventions during the COVID-19 Refugee Response. Ann. Glob. Health 2020, 86, 135. [Google Scholar] [CrossRef] [PubMed]
- Nasir, S.; Goto, R.; Kitamura, A.; Alafeef, S.; Ballout, G.; Hababeh, M.; Kiriya, J.; Seita, A.; Jimba, M. Dissemination and Implementation of the E-MCHHandbook, UNRWA’s Newly Released Maternal and Child Health Mobile Application: A Cross-Sectional Study. BMJ Open 2020, 10, e034885. [Google Scholar] [CrossRef] [PubMed]
- Saleh, S.; El Arnaout, N.; Abdouni, L.; Jammoul, Z.; Hachach, N.; Dasgupta, A. Sijilli: A Scalable Model of Cloud-Based Electronic Health Records for Migrating Populations in Low-Resource Settings. J. Med. Internet Res. 2020, 22, e18183. [Google Scholar] [CrossRef] [PubMed]
- Surmeli, A.; Narla, N.P.; Shields, A.J.; Atun, R. Leveraging Mobile Applications in Humanitarian Crisis to Improve Health: A Case of Syrian Women and Children Refugees in Turkey. J. Glob. Health Rep. 2020, 4, e2020099. [Google Scholar] [CrossRef]
- Meyer, C.L.; Surmeli, A.; Hoeflin Hana, C.; Narla, N.P. Perceptions on a Mobile Health Intervention to Improve Maternal Child Health for Syrian Refugees in Turkey: Opportunities and Challenges for End-User Acceptability. Front. Public Health 2022, 10, 1025675. [Google Scholar] [CrossRef]
- Shrestha, A.; Alawa, J.; Ashworth, H.; Essar, M.Y. Innovation Is Needed in Creating Electronic Health Records for Humanitarian Crises and Displaced Populations. Front. Digit. Health 2022, 4, 939168. [Google Scholar] [CrossRef]
- Seita, A.; Ballout, G.; Albeik, S.; Salameh, Z.; Zeidan, W.; Shah, S.; Atallah, S.; Horino, M. Leveraging Digital Health Data to Transform the United Nations Systems for Palestine Refugees for the Post Pandemic Time. Health Syst. Reform 2024, 10, 2378505. [Google Scholar] [CrossRef]
- HealthEmove Your Personal Health Record. Available online: https://healthemove.org (accessed on 6 January 2025).
- HERA Digital Health. Available online: https://heradigitalhealth.org/ (accessed on 10 January 2025).
- RedSafe, a Digital Humanitarian Platform. Available online: https://www.icrc.org/en/redsafe (accessed on 7 January 2025).
- 4th RedSafe Kiosk Opens. Available online: https://www.icrc.org/en/document/4th-redsafe-kiosk-opens-zimbabwe (accessed on 7 January 2025).
- JICA. Jordan: UNRWA’s Electronic MCH Handbook Application for Palestine Refugees; JICA: Tokyo, Japan, 2017. [Google Scholar]
- My Personal Health Bank—Health Data Today Healthcare Tomorrow. Available online: https://www.mypersonalhealthbank.com (accessed on 8 January 2025).
- My Personal Health Bank Usage Statistics. Available online: https://www.linkedin.com/posts/my-personal-health-bank_patientempowerment-healthdata-mypersonalhealthbank-activity-6995336497310658560-tysJ/ (accessed on 8 January 2025).
- Novel Measurements for Performance Improvement Challenge My Personal Health Bank. Available online: https://solve.mit.edu/solutions/63213 (accessed on 8 January 2025).
- RedSafe—Apps No Google Play. Available online: https://play.google.com/store/apps/details?id=org.icrc.dhp&hl=pt_PT (accessed on 7 January 2025).
- Borsari, L.; Stancanelli, G.; Guarenti, L.; Grandi, T.; Leotta, S.; Barcellini, L.; Borella, P.; Benski, A.C. An Innovative Mobile Health System to Improve and Standardize Antenatal Care Among Underserved Communities: A Feasibility Study in an Italian Hosting Center for Asylum Seekers. J. Immigr. Minor. Health 2018, 20, 1128–1136. [Google Scholar] [CrossRef]
- Brotherton, T.; Brotherton, S.; Ashworth, H.; Kadambi, A.; Ebrahim, H.; Ebrahim, S. Development of an Offline, Open-Source, Electronic Health Record System for Refugee Care. Front. Digit. Health 2022, 4, 847002. [Google Scholar] [CrossRef]
- Rossano, V.; Roselli, T.; Berni, F. A Healthcare System to Support Well-Being of Migrants: The Project Prevenzione 4.0; IADIS: Lisbon, Portugal, 2020; pp. 355–358. [Google Scholar]
- Lyles, C.R.; Tieu, L.; Sarkar, U.; Kiyoi, S.; Sadasivaiah, S.; Hoskote, M.; Ratanawongsa, N.; Schillinger, D. A Randomized Trial to Train Vulnerable Primary Care Patients to Use a Patient Portal. J. Am. Board. Fam. Med. 2019, 32, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Khader, Y.S.; Laflamme, L.; Schmid, D.; El-Halabi, S.; Khdair, M.A.; Sengoelge, M.; Atkins, S.; Tahtamouni, M.; Derrough, T.; El-Khatib, Z. Children Immunization App (CImA) Among Syrian Refugees in Zaatari Camp, Jordan: Protocol for a Cluster Randomized Controlled Pilot Trial Intervention Study. JMIR Res. Protoc. 2019, 8, e13557. [Google Scholar] [CrossRef] [PubMed]
- UCRAID (Ukrainian Citizen and Refugee Electronic Support in Respiratory Diseases, Allergy, Immunology and Dermatology) Action Plan—Bousquet—2023—Allergy—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/10.1111/all.15855 (accessed on 7 February 2025).
- Salah, A.; Alobid, S.; Jalalzai, S.; Junger, D.; Burgert, O. Univie: An App for Managing Digital Health Data of Refugees. In Digital Health and Informatics Innovations for Sustainable Health Care Systems; IOS Press: Amsterdam, The Netherlands, 2024; pp. 195–199. [Google Scholar]
- Palestinian Ministry of Health. Overview of the MCHHB in Palestine; Palestinian Ministry of Health: Al-Bireh, Palestine, 2012. [Google Scholar]
- Tensen, P.; van Dormolen, S.; van de Vijver, S.J.M.; van de Pavert, M.L.; Agyemang, C.O. Healthcare Providers Intentions to Use an Electronic Personal Health Record for Undocumented Migrants: A Qualitative Exploration Study in The Netherlands. Glob. Public Health 2025, 20, 2445840. [Google Scholar] [CrossRef] [PubMed]
- Building Health Systems That Are Inclusive for Refugees and Migrants. Available online: https://www.who.int/europe/activities/building-health-systems-that-are-inclusive-for-refugees-and-migrants (accessed on 20 January 2025).
- Bock, J.G.; Haque, Z.; McMahon, K.A. Displaced and Dismayed: How ICTs Are Helping Refugees and Migrants, and How We Can Do Better. Inf. Technol. Dev. 2020, 26, 670–691. [Google Scholar] [CrossRef]
- Radu, I.; Scheermesser, M.; Spiess, M.R.; Schulze, C.; Händler-Schuster, D.; Pehlke-Milde, J. Digital Health for Migrants, Ethnic and Cultural Minorities and the Role of Participatory Development: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 6962. [Google Scholar] [CrossRef]
- Gonzalez, C.; Early, J.; Gordon-Dseagu, V.; Mata, T.; Nieto, C. Promoting Culturally Tailored mHealth: A Scoping Review of Mobile Health Interventions in Latinx Communities. J. Immigr. Minor. Health 2021, 23, 1065–1077. [Google Scholar] [CrossRef]
- Jang, Y.; Yoon, J.; Park, N.S. Source of Health Information and Unmet Healthcare Needs in Asian Americans. J. Health Commun. 2018, 23, 652–660. [Google Scholar] [CrossRef]
- Kaihlanen, A.-M.; Virtanen, L.; Buchert, U.; Safarov, N.; Valkonen, P.; Hietapakka, L.; Hörhammer, I.; Kujala, S.; Kouvonen, A.; Heponiemi, T. Towards Digital Health Equity—A Qualitative Study of the Challenges Experienced by Vulnerable Groups in Using Digital Health Services in the COVID-19 Era. BMC Health Serv. Res. 2022, 22, 188. [Google Scholar] [CrossRef]
- Liem, A.; Natari, R.B.; Jimmy; Hall, B.J. Digital Health Applications in Mental Health Care for Immigrants and Refugees: A Rapid Review. Telemed. e-Health 2021, 27, 3–16. [Google Scholar] [CrossRef]
- Whitehead, L.; Talevski, J.; Fatehi, F.; Beauchamp, A. Barriers to and Facilitators of Digital Health Among Culturally and Linguistically Diverse Populations: Qualitative Systematic Review. J. Med. Internet Res. 2023, 25, e42719. [Google Scholar] [CrossRef]
- Alencar, A. Technology Can Be Transformative for Refugees, but It Can Also Hold Them Back. Available online: https://www.migrationpolicy.org/article/digital-technology-refugees (accessed on 4 February 2025).
- Taylor, D. Home Office Illegally Seized Phones of 2,000 Asylum Seekers, Court Rules; The Guardian: Kings Place, UK, 25 March.
- Tondo, L.; Hawkins, A. Croatian Police Accused of Burning Asylum Seekers’ Phones and Passports; The Guardian: Kings Place, UK.
- BBC. Europe Migrants: Austria to Seize Migrants’ Phones in Asylum Clampdown 2018. In BBC News; BBC: Portland Place, UK, 20 April.
- Mancini, T.; Sibilla, F.; Argiropoulos, D.; Rossi, M.; Everri, M. The Opportunities and Risks of Mobile Phones for Refugees’ Experience: A Scoping Review. PLoS ONE 2019, 14, e0225684. [Google Scholar] [CrossRef]
- European Parliament. Directorate General for Parliamentary Research Services. In Blockchain and the General Data Protection Regulation: Can Distributed Ledgers Be Squared with European Data Protection Law? Publications Office: Luxembourg, 2019. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
| No. | Authorship (Year) | Title | Publication | Methodology | EPHR |
|---|---|---|---|---|---|
| 1 | Ballout, G. et al. (2018) [27] | UNRWA’s innovative e-Health for 5 million Palestine refugees in the Near East | Original article | NA | e-MCH Handbook |
| 2 | Saleh, S. et al. (2019) [28] | Sijilli: a mobile electronic health records system for refugees in low-resource settings | Comment | NA | Sijilli |
| 3 | Narla, N. et al. (2020) [29] | Agile application of digital health interventions during the COVID-19 refugee response | Viewpoint | Exploratory evaluation | HERA App |
| 4 | Nasir, S. et al. (2020) [30] | Dissemination and implementation of the e-MCH Handbook, UNRWA’s newly released maternal and child health mobile application: a cross-sectional study | Original article | Cross-sectional study design | e-MCH Handbook |
| 5 | Saleh, S. et al. (2020) [31] | Sijilli: A scalable model of cloud-based electronic health records for migrating populations in low-resource settings | Viewpoint | NA | Sijilli |
| 6 | Surmeli, A. et al. (2020) [32] | Leveraging mobile applications in humanitarian crisis to improve health: A case of Syrian women and children refugees in Turkey | Report | NA | HERA App |
| 7 | Meyer, C. et al. (2022) [33] | Perceptions on a mobile health intervention to improve maternal child health for Syrian refugees in Turkey: Opportunities and challenges for end-user acceptability | Original article | Qualitative study | HERA App |
| 8 | Shrestha, A. et al. (2022) [34] | Innovation is needed in creating electronic health records for humanitarian crises and displaced populations | Opinion paper | NA | Sijilli |
| 9 | Vijver, S. et al. (2023) [16] | Digital health for all: How digital health could reduce inequality and increase universal health coverage | Viewpoint | NA | HealthEmove |
| 10 | Seita, A. et al. (2024) [35] | Leveraging digital health data to transform the United Nations Systems for Palestine refugees for the post pandemic time | Original article | Qualitative study | e-MCH Handbook |
| No. | Authorship (Month, Year) | Title | Publication Type | EPHR Tool |
|---|---|---|---|---|
| 1 | HealthEmove (n.d.) [36] | Your Personal Health Record | Official website HealthEmove | HealthEmove |
| 2 | Hera Digital Health (n.d.) [37] | HERA Digital Health | Official website HERA Digital Health | HERA App |
| 3 | ICRC (n.d.) [38] | RedSafe, a Digital Humanitarian Platform | Official website ICRC | RedSafe |
| 4 | ICRC (February, 2022) [39] | Fourth RedSafe kiosk opens in Zimbabwe | News release on the official website ICRC | RedSafe |
| 5 | JICA (August, 2017) [40] | Jordan: UNRWA’s electronic MCH handbook application for Palestine refugees (Issue 20) | Technical brief | e-MCH Handbook |
| 6 | My Personal Health Bank (n.d.) [41] | My Personal Health Bank | Official website of My Personal Health Bank | My Personal Health Bank |
| 7 | My Personal Health Bank (n.d.) [42] | Usage statistics | LinkedIn post | My Personal Health Bank |
| 8 | MIT-solve (August, 2022) [43] | Novel measurement for performance improvement challenge My Personal Health Bank | Application MIT-solve | My Personal Health Bank |
| 9 | Play Store (May, 2024) [44] | Play Store: RedSafe | App download | RedSafe |
| Tool Name | Initiated/Owned by | Mobile Population | Current Countries | Stage of Development | Number of Users (Month, Year) a | Languages | Tool Description | Application Type |
|---|---|---|---|---|---|---|---|---|
| Tools from the scientific literature | ||||||||
| e-MCH Handbook | UNRWA and JICA # | Palestine refugees # | Jordan, Gaza, Lebanon, Westbank, Syria # | Application since 2017 # | 254,586 registered users (July 2023) and 22,000 active users (June 2023) # | Arabic # | mHealth application with PHR | Smartphone app # |
| HERA App | HERA Digital Health & | Syrian refugees # | Turkey # | Application since 2018. In 2020 field tests were performed # | >3000 refugee families in Turkish pilot study (n.d.) & | Arabic, Turkish, English #, Pashto and Dari & | Humanitarian platform with ‘digital vault’ | Smartphone and web-app # |
| Sijilli | American University of Beirut and Epic Health Systems # | Syrian refugees # | Lebanon # | Launched 2018 # | >10,000 users (2022) # | English and Arabic # | EHR with user-portal and USB-stick | NA |
| HealthEmove | Initiative: Amsterdam Health & Technology Institute; software: Patients Know Best 5.0.18 & | Refugees # and People on the move & | Netherlands & | Application since 2023 # | NA | 22 languages & | EPHR | Web-app & |
| Tools from the grey literature | ||||||||
| My personal Health Bank | University of Southern Denmark, University of Dodoma and Muhimbili University & | People in developing countries and people on the move & | Tanzania & | Feasibility study from June 2022 until February 2023 | 4969 patients included (June 2022) & (31) a | English, Kiswahili & | EPHR | Web-app & |
| RedSafe | International Committee of the Red Cross & | People affected by conflict, migration and other humanitarian crisis & | Honduras, Guatemala, El Salvador, Mexico, USA, Costa Rica, Panama, Zimbabwe, South Africa, Botswana, Malawi, Mozambique, Eswatini, Lesotho, Switzerland, Zambia *,& | Launched in May 2021 & | 32,000 downloads (February 2022) & | English, Spanish and Portuguese & | Humanitarian platform with ‘digital vault’ | Smartphone and web-app & |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tensen, P.; Gaifém, F.; Paul, S.K.; Wekesah, F.M.; Acheampong, P.R.; Nikolajsen, M.B.; Kirk, U.B.; Owusu-Dabo, E.; Kallestrup, P.; Agyemang, C.; et al. Electronic Personal Health Records for Mobile Populations: A Rapid Systematic Literature Review. Int. J. Environ. Res. Public Health 2025, 22, 488. https://doi.org/10.3390/ijerph22040488
Tensen P, Gaifém F, Paul SK, Wekesah FM, Acheampong PR, Nikolajsen MB, Kirk UB, Owusu-Dabo E, Kallestrup P, Agyemang C, et al. Electronic Personal Health Records for Mobile Populations: A Rapid Systematic Literature Review. International Journal of Environmental Research and Public Health. 2025; 22(4):488. https://doi.org/10.3390/ijerph22040488
Chicago/Turabian StyleTensen, Paulien, Francisca Gaifém, Simeon Kintu Paul, Frederick Murunga Wekesah, Princess Ruhama Acheampong, Maria Bach Nikolajsen, Ulrik Bak Kirk, Ellis Owusu-Dabo, Per Kallestrup, Charles Agyemang, and et al. 2025. "Electronic Personal Health Records for Mobile Populations: A Rapid Systematic Literature Review" International Journal of Environmental Research and Public Health 22, no. 4: 488. https://doi.org/10.3390/ijerph22040488
APA StyleTensen, P., Gaifém, F., Paul, S. K., Wekesah, F. M., Acheampong, P. R., Nikolajsen, M. B., Kirk, U. B., Owusu-Dabo, E., Kallestrup, P., Agyemang, C., & van de Vijver, S. (2025). Electronic Personal Health Records for Mobile Populations: A Rapid Systematic Literature Review. International Journal of Environmental Research and Public Health, 22(4), 488. https://doi.org/10.3390/ijerph22040488









