Characteristics of Community-Dwelling Older People Who Are Less Likely to Respond to Mail Surveys Under Infection Countermeasures for New Strains of Coronavirus: The Takasaki Study
Abstract
1. Introduction
2. Materials and Methods
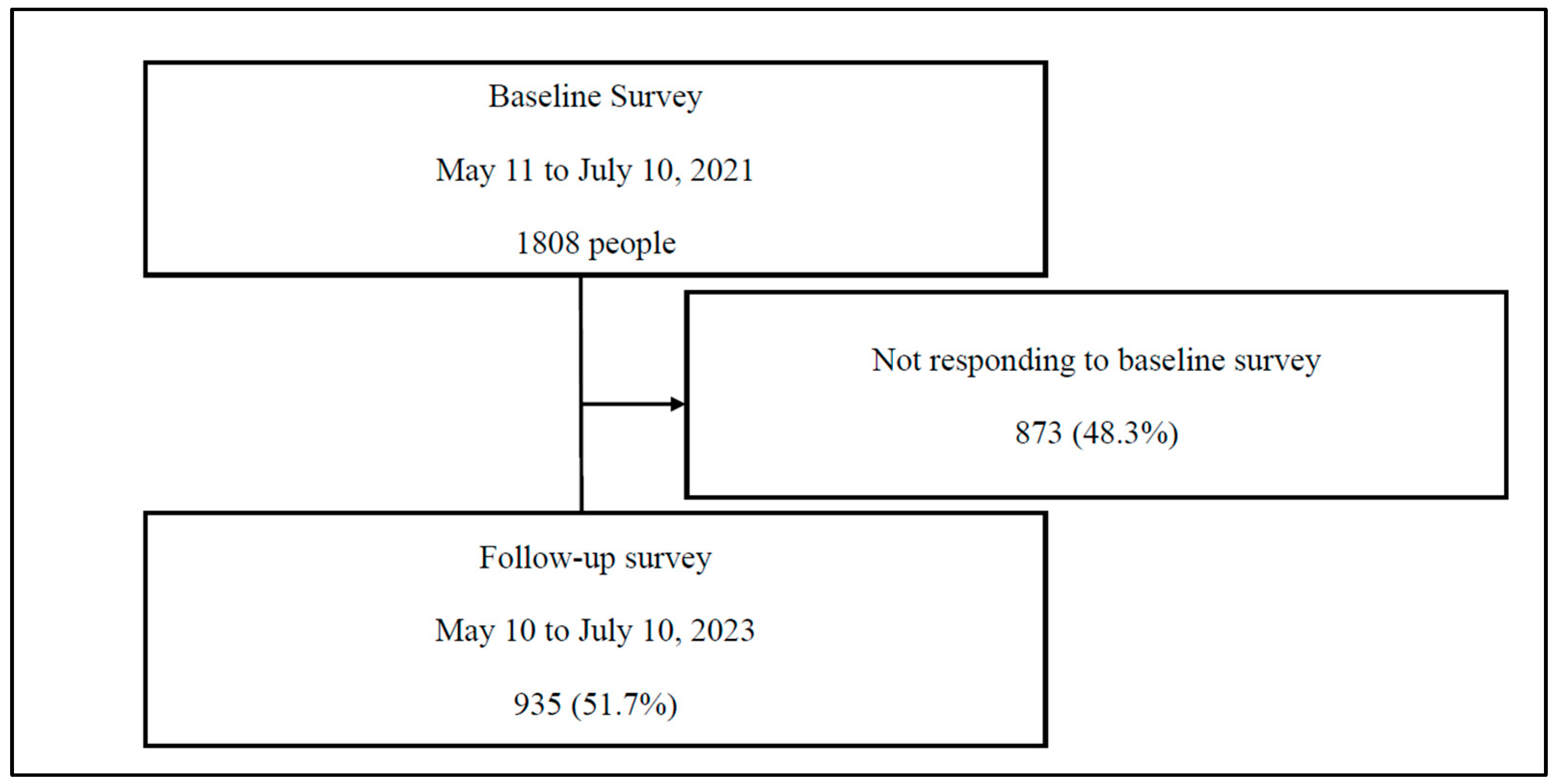
2.1. Study Design and Participants
2.2. Measurements
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Internal Affairs and Communications Statistics Bureau Home Page: Statistical Topics No. 142 Japan’s Older Adults Seen from Statistics—In Honor of “Respect for the Aged Day”. Available online: https://www.stat.go.jp/data/topics/pdf/topics142.pdf (accessed on 25 January 2025).
- Ministry of Health, Labor and Welfare. Healthy Life Expectancy in 2022 (Reiwa 4). Available online: https://www.mhlw.go.jp/content/10904750/001363069.pdf (accessed on 25 January 2025).
- Lewis, S.; Ewald, L.; Duber, H.C.; Mokdad, A.H.; Gakidou, E. Determinants of Unmet Healthcare Needs During the Final Stage of the COVID-19 Pandemic: Insights From a 21-Country Online Survey. Int. J. Public Health 2024, 69, 1607639. [Google Scholar] [CrossRef] [PubMed]
- Na, L. Characteristics of community-dwelling older individuals who delayed care during the COVID-19 pandemic. Arch. Gerontol. Geriatr. 2022, 101, 104710. [Google Scholar] [CrossRef] [PubMed]
- Sands, L.P.; Albert, S.M.; Suitor, J.J. Understanding and addressing older adults’ needs during COVID-19. Innov. Aging 2020, 4, igaa019. [Google Scholar] [CrossRef] [PubMed]
- Steinman, M.A.; Perry, L.; Perissinotto, C.M. Meeting the care needs of older adults isolated at home during the COVID-19 pandemic. JAMA Intern. Med. 2020, 180, 819–820. [Google Scholar] [CrossRef]
- Li, W.; Frydman, J.L.; Li, Y.; Liu, B. Characterizing delayed care among US older adults by self-rated health during the COVID-19 pandemic. Prev. Med. 2022, 164, 107308. [Google Scholar] [CrossRef]
- Jones, A.N.; Power, M.C. Pre-pandemic factors associated with delayed health care among US older adults during the COVID-19 pandemic. J. Med. Access 2023, 7, 27550834231202860. [Google Scholar] [CrossRef]
- Zhong, S.; Huisingh-Scheetz, M.; Huang, E.S. Delayed medical care and its perceived health impact among US older adults during the COVID-19 pandemic. J. Am. Geriatr. Soc. 2022, 70, 1620–1628. [Google Scholar] [CrossRef]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. The influence of the COVID-19 pandemic on physical activity and new incidence of frailty among initially non-frail older adults in Japan: A follow-up online survey. J. Nutr. Health Aging 2021, 25, 751–756. [Google Scholar] [CrossRef]
- Ataka, T.; Kimura, N.; Eguchi, A.; Matsubara, E. Changes in objectively measured lifestyle factors during the COVID-19 pandemic in community-dwelling older adults. BMC Geriatr. 2022, 22, 326. [Google Scholar] [CrossRef]
- van Der Klei, V.M.G.T.H.; Moens, I.S.; Simons, T.; den Elzen, W.P.J.; Mooijaart, S.P.; Gussekloo, J.; Trompet, S.; Drewes, Y.M.; Drewes, Y.M. The impact of the COVID-19 pandemic on Positive Health among older adults in relation to the complexity of health problems. J. Am. Geriatr. Soc. 2024, 72, 718–728. [Google Scholar] [CrossRef]
- Alonzi, S.; La Torre, A.; Silverstein, M.W. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychol. Trauma 2020, 12 (Suppl. S1), S236–S238. [Google Scholar] [CrossRef] [PubMed]
- Mitra, A.R.; Fergusson, N.A.; Lloyd-Smith, E.; Wormsbecker, A.; Foster, D.; Karpov, A.; Crowe, S.; Haljan, G.; Chittock, D.R.; Kanji, H.D.; et al. Baseline characteristics and outcomes of patients with COVID-19 admitted to intensive care units in Vancouver, Canada: A case series. CMAJ 2020, 192, E694–E701. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.Y.S.; Zhang, D.; Sit, R.W.S.; Yip, B.H.K.; Chung, R.Y.N.; Wong, C.K.M.; Chan, D.C.C.; Sun, W.; Kwok, K.O.; Mercer, S.W.; et al. Impact of COVID-19 on loneliness, mental health, and health service utilisation: A prospective cohort study of older adults with multimorbidity in primary care. Br. J. Gen. Pract. 2020, 70, e817–e824. [Google Scholar] [CrossRef]
- Vannini, P.; Gagliardi, G.P.; Kuppe, M.; Dossett, M.L.; Donovan, N.J.; Gatchel, J.R.; Quiroz, Y.T.; Premnath, P.Y.; Amariglio, R.; Sperling, R.A.; et al. Stress, resilience, and coping strategies in a sample of community-dwelling older adults during COVID-19. J. Psychiatr. Res. 2021, 138, 176–185. [Google Scholar] [CrossRef]
- Whitehead, B.R. COVID-19 as a stressor: Pandemic expectations, perceived stress, and negative affect in older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, e59–e64. [Google Scholar] [CrossRef]
- Koizumi, S.; Ohta, A.; Kamei, M. Homebound older adults who live independently in rural Japan: Prevalence and contributing factors during the COVID-19 pandemic. Prev. Med. Rep. 2024, 39, 102640. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, T.; Saida, K.; Tanaka, S.; Murayama, A. Rapid response: Impact of the COVID-19 pandemic on frailty in the elderly citizen; corona-frailty. BMJ 2020, 369, m1543. [Google Scholar]
- Shinohara, T.; Saida, K.; Tanaka, S.; Murayama, A. Do lifestyle measures to counter COVID-19 affect frailty rates in elderly community dwelling? Protocol for cross-sectional and cohort study. BMJ Open 2020, 10, e040341. [Google Scholar] [CrossRef]
- Tanaka, S.; Saida, K.; Murayama, A.; Higuchi, D.; Shinohara, T. Associated factors of new subjective cognitive decline complaints after a 6-month period among community-dwelling older adults during the COVID-19 pandemic in Japan. Psychogeriatrics 2023, 23, 136–140. [Google Scholar] [CrossRef]
- Tanaka, S.; Murayama, A.; Higuchi, D.; Saida, K.; Shinohara, T. Relationship between consistent subjective cognitive decline and occurrence of falls six months later. Arch. Gerontol. Geriatr. 2023, 104, 104841. [Google Scholar] [CrossRef]
- Murayama, A.; Higuchi, D.; Saida, K.; Tanaka, S.; Shinohara, T. Fall risk prediction for community-dwelling older adults: Analysis of assessment scale and evaluation items without actual measurement. Int. J. Environ. Res. Public Health 2024, 21, 224. [Google Scholar] [CrossRef] [PubMed]
- Gunma Prefectural Office: Temporary Press Conference on Requests for Priority Measures Such as Prevention of Spread (May 12). Available online: https://www.pref.gunma.jp/site/chiji/22640.html (accessed on 25 January 2025).
- Ministry of Health, Labor and Welfare. Response to the Novel Coronavirus Infection After Shift to Category 5 Infectious Disease. Available online: https://www.mhlw.go.jp/stf/corona5rui.html (accessed on 25 January 2025).
- Yamada, M.; Arai, H. Predictive value of frailty scores for healthy life expectancy in community-dwelling older Japanese adults. J. Am. Med. Dir. Assoc. 2015, 16, 1002.e7–1002.e11. [Google Scholar] [CrossRef]
- Shinohara, T.; Saida, K.; Tanaka, S.; Murayama, A. Actual frailty conditions and lifestyle changes in community-dwelling older adults affected by coronavirus disease 2019 countermeasures in Japan: A cross-sectional study. Sage Open Nurs. 2021, 7, 23779608211025117. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, D.; Yoshida, T.; Watanabe, Y.; Yamada, Y.; Miyachi, M.; Kimura, M. Validation of the Kihon Checklist and the frailty screening index for frailty defined by the phenotype model in older Japanese adults. BMC Geriatr. 2022, 22, 478. [Google Scholar] [CrossRef]
- Satake, S.; Arai, H. The revised Japanese version of the Cardiovascular Health Study criteria (revised J-CHS criteria). Geriatr. Gerontol. Int. 2020, 20, 992–993. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, M.L.; Coppinger, T.; McCarthy, A.L. The role of nutrition and physical activity in frailty: A review. Clin. Nutr. ESPEN 2020, 35, 1–11. [Google Scholar] [CrossRef]
- Shimada, H.; Makizako, H.; Lee, S.; Doi, T.; Lee, S.; Tsutsumimoto, K.; Harada, K.; Hotta, R.; Bae, S.; Nakakubo, S.; et al. Impact of cognitive frailty on daily activities in older persons. J. Nutr. Health Aging 2016, 20, 729–735. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Doi, T.; Yoshida, D.; Anan, Y.; Tsutsumimoto, K.; Uemura, K.; Liu-Ambrose, T.; Park, H.; Lee, S.; et al. Physical frailty predicts incident depressive symptoms in elderly people: Prospective findings from the Obu Study of Health Promotion for the Elderly. J. Am. Med. Dir. Assoc. 2015, 16, 194–199. [Google Scholar] [CrossRef]
- Shinohara, T.; Saida, K.; Tanaka, S.; Murayama, A. Association between frailty and changes in lifestyle and physical or psychological conditions among older adults affected by the coronavirus disease 2019 countermeasures in Japan. Geriatr. Gerontol. Int. 2021, 21, 39–42. [Google Scholar] [CrossRef]
- Tierney, N.; Cook, D.; McBain, M.; Fay, C.; O’Hara-Wild, M.; Hester, J.; Smith, L.; Heiss, A. Package “naniar”. Available online: https://cran.r-project.org/web/packages/naniar/naniar.pdf (accessed on 27 September 2024).
- Van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- van Buuren, S.; Groothuis-Oudshoorn, K.; Vink, G.; Schouten, R.; Robitzsch, A.; Rockenschaub, P.; Doove, L.; Jolani, S.; Moreno-Betancur, M. Package “mice”. Available online: https://cran.r-project.org/web/packages/mice/mice.pdf (accessed on 27 September 2024).
- White, I.R.; Royston, P.; Wood, A.M. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 2011, 30, 377–399. [Google Scholar] [CrossRef] [PubMed]
- Harrell, F.E.; Lee, K.L.; Califf, R.M.; Pryor, D.B.; Rosati, R.A. Regression modelling strategies for improved prognostic prediction. Stat. Med. 1984, 3, 143–152. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Maruta, J.; Kurozumi, H.; Uchida, K.; Akada, S.; Inoue, K. Longitudinal changes in anxiety and depression and their ameliorating lifestyle factors among community-dwelling older adults during the COVID-19 pandemic. Arch. Gerontol. Geriatr. Plus 2024, 1, 100036. [Google Scholar] [CrossRef]
- Murayama, A.; Higuchi, D.; Saida, K.; Tanaka, S.; Shinohara, T. Risk factors for falls in community-dwelling older adults during the novel coronavirus pandemic in Japan: A prospective cohort study. Int. J. Environ. Res. Public Health 2024, 21, 1603. [Google Scholar] [CrossRef]
- World Health Organization. WHO to Identify Pathogens That Could Cause Future Outbreaks and Pandemics. Available online: https://www.who.int/news/item/21-11-2022-who-to-identify-pathogens-that-could-cause-future-outbreaks-and-pandemics (accessed on 27 September 2024).
- Chen, Z.; Cong, Z. Age differences in experiencing negative impacts of the COVID-19 pandemic: A latent class analysis. Int. J. Disaster Risk Reduct. 2023, 96, 103957. [Google Scholar] [CrossRef]
- Sugaya, N.; Yamamoto, T.; Uchiumi, C. A 2-year longitudinal study examining the change in psychosocial factors under the COVID-19 pandemic in Japan. Sci. Data 2024, 11, 544. [Google Scholar] [CrossRef]
- Katori, T. Japan’s healthcare delivery system: From its historical evolution to the challenges of a super-aged society. Glob. Health Med. 2024, 6, 6–12. [Google Scholar] [CrossRef]
- Weber, P.; Birkholz, L.; Straub, R.; Kohler, S.; Helsper, N.; Dippon, L.; Pfeifer, K.; Rütten, A.; Semrau, J. The limitations and potentials of evaluating economic aspects of community-based health promotion: A critical review. Appl. Health Econ. Health Policy 2024, 22, 165–179. [Google Scholar] [CrossRef]
- Su, Y.; Hamatani, M.; Yuki, M.; Ogawa, N.; Kawahara, K. Frailty and social isolation before and during the coronavirus disease 2019 pandemic among older adults: A path analysis. J. Adv. Nurs. 2024, 80, 1902–1913. [Google Scholar] [CrossRef] [PubMed]
- Hamatani, M.; Su, Y.; Yuki, M.; Ogawa, N.; Kawahara, K. Depressive symptoms associated with infection prevention measures and daily lifestyle habit characteristics among Japanese community-dwelling older adults during the COVID-19 pandemic. Jpn. J. Nurs. Sci. 2024, 21, e12575. [Google Scholar] [CrossRef] [PubMed]
- Tokumitsu, K.; Sugawara, N.; Tabuchi, T.; Yasui-Furukori, N. Real-world predictors of changes in fear of COVID-19 in the Japanese general population: A large-scale internet-based cohort study with 20,712 participants. BMC Psychiatry 2024, 24, 435. [Google Scholar] [CrossRef] [PubMed]
| Overall | Responding Group | Non-Responding Group | t-Value | χ2 | p-Value | |
|---|---|---|---|---|---|---|
| (n = 935) | (n = 330) | (n = 605) | ||||
| Age, mean ± standard deviation | 79.09 ± 6.16 | 79.37 ± 5.44 | 78.95 ± 6.52 | 1.009 | 0.313 | |
| Sex, (male/female), n (%) | 238(25.4)/697(74.6) | 71(21.5)/259(78.5) | 167(27.6)/438(72.4) | 3.856 | 0.041 | |
| Living arrangement, (living together/alone), n (%) | 622(66.5)/313(33.5) | 256(77.6)/74(22.4) | 366(60.5)/239(39.5) | 27.21 | <0.001 | |
| Fall history, (presence/absence), n (%) | 112(12.0)/823(88.0) | 38(11.5)/292(88.5) | 74(12.2)/531(87.8) | 0.047 | 0.833 | |
| Comorbidity, (presence/absence), n (%) | 611(65.3)/324(34.7) | 186(56.4)/144(43.6) | 425(70.2)/180(29.8) | 17.57 | <0.001 | |
| Long-term care insurance, (use/not use), n (%) | 187(20.0)/748(80.0) | 54(16.4)/276(83.6) | 133(22.0)/472(78.0) | 3.871 | 0.040 | |
| FSI (score), mean ± standard deviation | 1.31 ± 1.13 | 1.19 ± 1.08 | 1.38 ± 1.16 | −2.529 | 0.014 |
| No. | Questions | Overall (n = 935) | Responding Group (n = 330) | Non-Responding Group (n = 605) | χ2 | p-Value |
|---|---|---|---|---|---|---|
| Q1 | Have you lost 2–3 kg or more in the past 6 months? (score: 0/1), n (%) | 111(11.9)/824(88.1) | 35(10.6)/295(89.4) | 76(12.6)/529(87.4) | 0.605 | 0.399 |
| Q2 | Do you think you walk slower than before? (score: 0/1), n (%) | 526(56.3)/409(43.7) | 176(53.3)/154(46.7) | 350(57.9)/255(42.1) | 1.592 | 0.190 |
| Q3 | Do you do physical exercise like walking at least once a week? (score: 0/1), n (%) | 277(29.6)/658(70.4) | 88(26.7)/242(73.3) | 189(31.2)/416(68.8) | 1.928 | 0.155 |
| Q4 | Can you recall what happened 5 min ago? (score: 0/1), n (%) | 844(90.3)/91(9.7) | 302(91.5)/28(8.5) | 542(89.6)/63(10.4) | 0.697 | 0.358 |
| Q5 | Have you felt tired for no reason (in the past 2 weeks)? (score: 0/1), n (%) | 224(24.0)/711(76.0) | 65(19.7)/265(80.3) | 159(26.3)/446(73.7) | 4.726 | 0.025 |
| No. | Questions | Overall | Responding Group | Non-Responding Group | t-Value | p-Value |
|---|---|---|---|---|---|---|
| (n = 935) | (n = 330) | (n = 605) | ||||
| Q1 | Amount of daily movement, mean ± standard deviation | 2.47 ± 0.84 | 2.48 ± 0.85 | 2.47 ± 0.85 | 0.237 | 0.812 |
| Q2 | Leg muscle strength, mean ± standard deviation | 2.31 ± 0.74 | 2.35 ± 0.75 | 2.30 ± 0.75 | 1.057 | 0.291 |
| Q3 | Meal size, mean ± standard deviation | 2.80 ± 0.57 | 2.85 ± 0.57 | 2.76 ±0.58 | 1.725 | 0.085 |
| Q4 | Worry or anxiety, mean ± standard deviation | 2.51 ± 0.74 | 2.54 ± 0.73 | 2.51 ± 0.76 | 0.624 | 0.532 |
| Q5 | Opportunities to talk to people, mean ± standard deviation | 2.27 ± 0.86 | 2.18 ± 0.82 | 2.32 ± 0.89 | −2.458 | 0.014 |
| Independent Variable | Odds Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Sex | 0.84 | 0.67–1.18 | 0.328 |
| Living arrangement (alone) | 2.36 | 1.71–3.27 | <0.001 |
| Comorbidity (presence) | 1.84 | 1.38–2.47 | <0.001 |
| Long-term care insurance (use) | 1.69 | 1.15–2.49 | 0.007 |
| Have you felt tired for no reason (in the past 2 weeks)? (score 1) | 1.57 | 1.10–2.23 | 0.012 |
| Opportunities to talk to people (declining trend) | 1.20 | 1.02–1.42 | 0.029 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murayama, A.; Higuchi, D.; Saida, K.; Tanaka, S.; Shinohara, T. Characteristics of Community-Dwelling Older People Who Are Less Likely to Respond to Mail Surveys Under Infection Countermeasures for New Strains of Coronavirus: The Takasaki Study. Int. J. Environ. Res. Public Health 2025, 22, 437. https://doi.org/10.3390/ijerph22030437
Murayama A, Higuchi D, Saida K, Tanaka S, Shinohara T. Characteristics of Community-Dwelling Older People Who Are Less Likely to Respond to Mail Surveys Under Infection Countermeasures for New Strains of Coronavirus: The Takasaki Study. International Journal of Environmental Research and Public Health. 2025; 22(3):437. https://doi.org/10.3390/ijerph22030437
Chicago/Turabian StyleMurayama, Akihiko, Daisuke Higuchi, Kosuke Saida, Shigeya Tanaka, and Tomoyuki Shinohara. 2025. "Characteristics of Community-Dwelling Older People Who Are Less Likely to Respond to Mail Surveys Under Infection Countermeasures for New Strains of Coronavirus: The Takasaki Study" International Journal of Environmental Research and Public Health 22, no. 3: 437. https://doi.org/10.3390/ijerph22030437
APA StyleMurayama, A., Higuchi, D., Saida, K., Tanaka, S., & Shinohara, T. (2025). Characteristics of Community-Dwelling Older People Who Are Less Likely to Respond to Mail Surveys Under Infection Countermeasures for New Strains of Coronavirus: The Takasaki Study. International Journal of Environmental Research and Public Health, 22(3), 437. https://doi.org/10.3390/ijerph22030437






