Social Inequities in Cardiovascular Disease Risk Factors at Multiple Levels Persist Among Mothers in Texas
Abstract
1. Introduction
2. Materials and Methods
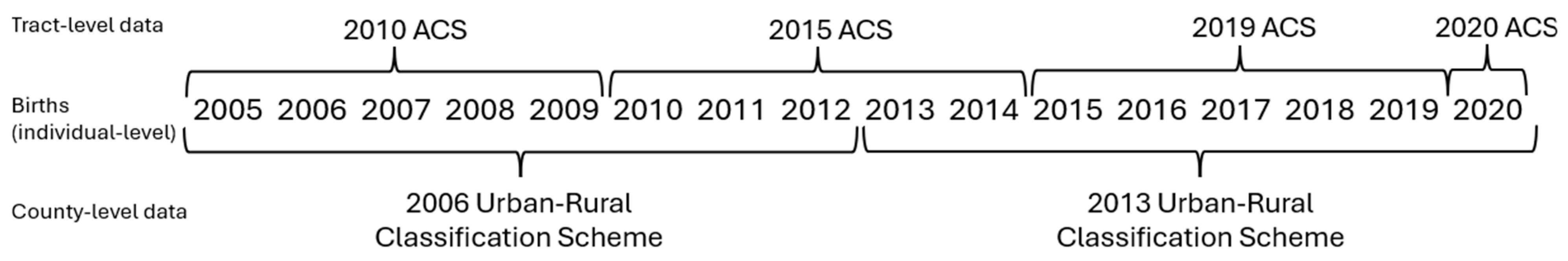
2.1. Data
2.2. Variables
2.3. Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mehta, C.M.; Arnett, J.J.; Palmer, C.G.; Nelson, L.J. Established adulthood: A new conception of ages 30 to 45. Am. Psychol. 2020, 75, 431–444. [Google Scholar] [CrossRef] [PubMed]
- Heart Disease Facts. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/heartdisease/facts.htm (accessed on 14 October 2022).
- Barnes, A.S. Emerging modifiable risk factors for cardiovascular disease in women: Obesity, physical activity, and sedentary behavior. Tex. Heart Inst. J. 2013, 40, 293–295. [Google Scholar] [PubMed]
- Curtin, S.C.; Tejada-Vera, B.; Bastian, B.A.; National Center for Health Statistics (U.S.). Deaths: Leading Causes for 2021. Natl. Vital Stat. Rep. 2024, 73, 38. [Google Scholar] [CrossRef]
- Arora, S.; Stouffer, G.A.; Kucharska-Newton, A.M.; Qamar, A.; Vaduganathan, M.; Pandey, A.; Porterfield, D.; Blankstein, R.; Rosamond, W.D.; Bhatt, D.L.; et al. Twenty Year Trends and Sex Differences in Young Adults Hospitalized with Acute Myocardial Infarction: The ARIC Community Surveillance Study. Circulation 2019, 139, 1047–1056. [Google Scholar] [CrossRef]
- Cooper, R.; Cutler, J.; Desvigne-Nickens, P.; Fortmann, S.P.; Friedman, L.; Havlik, R.; Hogelin, G.; Marler, J.; McGovern, P.; Morosco, G.; et al. Trends and Disparities in Coronary Heart Disease, Stroke, and Other Cardiovascular Diseases in the United States: Findings of the National Conference on Cardiovascular Disease Prevention. Circulation 2000, 102, 3137–3147. [Google Scholar] [CrossRef]
- Shah, N.S.; Lloyd-Jones, D.M.; O’Flaherty, M.; Capewell, S.; Kershaw, K.; Carnethon, M.; Khan, S.S. Trends in Cardiometabolic Mortality in the United States, 1999–2017. JAMA 2019, 322, 780. [Google Scholar] [CrossRef]
- Kurian, A.K.; Cardarelli, K.M. Racial and ethnic differences in cardiovascular disease risk factors: A systematic review. Ethn. Dis. 2007, 17, 143–152. [Google Scholar]
- Safford, M.M.; Brown, T.M.; Muntner, P.M.; Durant, R.W.; Glasser, S.; Halanych, J.H.; Shikany, J.M.; Prineas, R.J.; Samdarshi, T.; Bittner, V.A.; et al. Association of Race and Sex with Risk of Incident Acute Coronary Heart Disease Events. JAMA 2012, 308, 1768. [Google Scholar] [CrossRef]
- Virani, S.S.; Brautbar, A.; Davis, B.C.; Nambi, V.; Hoogeveen, R.C.; Sharrett, R.; Coresh, J.; Mosley, T.H.; Morrisett, J.D.; Catellier, D.J.; et al. Associations Between Lipoprotein(a) Levels and Cardiovascular Outcomes in Black and White Subjects: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2012, 125, 241–249. [Google Scholar] [CrossRef]
- Thomas, A.J.; Eberly, L.E.; Davey Smith, G.; Neaton, J.D.; Stamler, J. Race/ethnicity, income, major risk factors, and cardiovascular disease mortality. Am. J. Public Health 2005, 95, 1417–1423. [Google Scholar] [CrossRef]
- Singh, G.K.; Siahpush, M.; Azuine, R.E.; Williams, S.D. Widening Socioeconomic and Racial Disparities in Cardiovascular Disease Mortality in the United States, 1969–2013. Int. J. MCH Aids. 2015, 3, 106–118. [Google Scholar] [CrossRef]
- Flegal, K.M. Prevalence and Trends in Obesity Among US Adults, 1999–2008. JAMA 2010, 303, 235. [Google Scholar] [CrossRef]
- Flegal, K.M.; Carroll, M.D.; Kit, B.K.; Ogden, C.L. Prevalence of Obesity and Trends in the Distribution of Body Mass Index Among US Adults, 1999–2010. JAMA 2012, 307, 491. [Google Scholar] [CrossRef] [PubMed]
- Pearson-Stuttard, J.; Guzman-Castillo, M.; Penalvo, J.L.; Rehm, C.D.; Afshin, A.; Danaei, G.; Kypridemos, C.; Gaziano, T.; Mozaffarian, D.; Capewell, S.; et al. Modeling Future Cardiovascular Disease Mortality in the United States: National Trends and Racial and Ethnic Disparities. Circulation 2016, 133, 967–978. [Google Scholar] [CrossRef]
- Obesity is a Common, Serious, and Costly Disease. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/obesity/data/adult.html (accessed on 14 October 2022).
- Kwan, T.W.; Wong, S.S.; Hong, Y.; Kanaya, A.M.; Khan, S.S.; Hayman, L.L.; Shah, S.H.; Welty, F.K.; Deedwania, P.C.; Kaliq, A.; et al. Epidemiology of Diabetes and Atherosclerotic Cardiovascular Disease Among Asian American Adults: Implications, Management, and Future Directions: A Scientific Statement from the American Heart Association. Circulation 2023, 148, 74–94. [Google Scholar] [CrossRef]
- Gordon, N.P.; Lin, T.Y.; Rau, J.; Lo, J.C. Aggregation of Asian-American subgroups masks meaningful differences in health and health risks among Asian ethnicities: An electronic health record based cohort study. BMC Public Health 2019, 19, 1551. [Google Scholar] [CrossRef] [PubMed]
- Chernov, C.; Wang, L.; Thorpe, L.E.; Isla, N.; Freeman, A.; Trinh-Shevrin, C.; Kanchi, R.; Perlman, S.E. Cardiovascular Disease Risk Factors Among Immigrant and US-Born Adults in New York City. Public Health Rep. 2022, 137, 537–547. [Google Scholar] [CrossRef]
- Gil-González, D.; Carrasco-Portiño, M.; Vives-Cases, C.; Agudelo-Suárez, A.A.; Castejón Bolea, R.; Ronda-Pérez, E. Is health a right for all? An umbrella review of the barriers to health care access faced by migrants. Ethn. Health 2015, 20, 523–541. [Google Scholar] [CrossRef] [PubMed]
- Clough, J.; Lee, S.; Chae, D.H. Barriers to Health Care among Asian Immigrants in the United States: A Traditional Review. J. Health Care Poor Underserved 2013, 24, 384–403. [Google Scholar] [CrossRef]
- Wafula, E.G.; Snipes, S.A. Barriers to Health Care Access Faced by Black Immigrants in the US: Theoretical Considerations and Recommendations. J. Immigr. Minor. Health 2014, 16, 689–698. [Google Scholar] [CrossRef]
- Langellier, B.A.; Garza, J.R.; Glik, D.; Prelip, M.L.; Brookmeyer, R.; Roberts, C.K.; Peters, A.; Ortega, A.N. Immigration Disparities in Cardiovascular Disease Risk Factor Awareness. J. Immigr. Minor. Health 2012, 14, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.T.; Echeverria, S.E.; DuPont-Reyes, M.J.; Vasquez, E.; Murillo, R.; Gonzalez, T.; Rodriguez, F. Educational Attainment and Prevalence of Cardiovascular Health (Life’s Simple 7) in Asian Americans. Int. J. Environ. Res. Public Health 2021, 18, 1480. [Google Scholar] [CrossRef]
- Cubbin, C.; Hadden, W.C.; Winkleby, M.A. Neighborhood context and cardiovascular disease risk factors: The contribution of material deprivation. Ethn. Dis. 2001, 11, 687–700. [Google Scholar]
- Unger, E.; Diez-Roux, A.V.; Lloyd-Jones, D.M.; Mujahid, M.S.; Nettleton, J.A.; Bertoni, A.; Badon, S.E.; Ning, H.; Allen, N.B. Association of neighborhood characteristics with cardiovascular health in the multi-ethnic study of atherosclerosis. Circ. Cardiovasc. Qual. Outcomes 2014, 7, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Correa, A.; Greer, S.; Sims, M. Assessing neighborhood-level effects on disparities in cardiovascular diseases. Circulation 2015, 131, 124–127. [Google Scholar] [CrossRef]
- Barber, S.; Hickson, D.A.; Wang, X.; Sims, M.; Nelson, C.; Diez-Roux, A.V. Neighborhood Disadvantage, Poor Social Conditions, and Cardiovascular Disease Incidence Among African American Adults in the Jackson Heart Study. Am. J. Public Health 2016, 106, 2219–2226. [Google Scholar] [CrossRef] [PubMed]
- Hines, A.L.; Albert, M.A.; Blair, J.P.; Crews, D.C.; Cooper, L.A.; Long, D.L.; Carson, A.P. Neighborhood Factors, Individual Stressors, and Cardiovascular Health Among Black and White Adults in the US: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. JAMA Netw. Open 2023, 6, e2336207. [Google Scholar] [CrossRef]
- Chi, G.C.; Hajat, A.; Bird, C.E.; Cullen, M.R.; Griffin, B.A.; Miller, K.A.; Shih, R.A.; Stefanick, M.L.; Vedal, S.; Whitsel, E.A.; et al. Individual and Neighborhood Socioeconomic Status and the Association between Air Pollution and Cardiovascular Disease. Environ. Health Perspect. 2016, 124, 1840–1847. [Google Scholar] [CrossRef]
- Do, D.P.; Zheng, C. A marginal structural modeling strategy investigating short and long-term exposure to neighborhood poverty on BMI among U.S. black and white adults. Health Place 2017, 46, 201–209. [Google Scholar] [CrossRef]
- Fan, J.X.; Wen, M.; Li, K. Associations between obesity and neighborhood socioeconomic status: Variations by gender and family income status. SSM Popul. Health 2020, 10, 100529. [Google Scholar] [CrossRef]
- Mendez, D.D.; Thorpe, R.J.; Amutah, N.; Davis, E.M.; Walker, R.E.; Chapple-McGruder, T.; Bodnar, L. Neighborhood racial composition and poverty in association with pre-pregnancy weight and gestational weight gain. SSM Popul. Health 2016, 2, 692–699. [Google Scholar] [CrossRef] [PubMed]
- Ford, P.B.; Dzewaltowski, D.A. Neighborhood deprivation, supermarket availability, and BMI in low-income women: A multilevel analysis. J. Community Health 2011, 36, 785–796. [Google Scholar] [CrossRef]
- Sheehan, C.M.; Cantu, P.A.; Powers, D.A.; Margerison-Zilko, C.E.; Cubbin, C. Long-term neighborhood poverty trajectories and obesity in a sample of california mothers. Health Place 2017, 46, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.R.; Ommerborn, M.J.; Hickson, D.A.; Grooms, K.N.; Sims, M.; Taylor, H.A.; Albert, M.A. Neighborhood disadvantage, neighborhood safety and cardiometabolic risk factors in African Americans: Biosocial associations in the Jackson Heart study. PLoS ONE 2013, 8, e63254. [Google Scholar] [CrossRef] [PubMed]
- Schiff, M.D.; Mair, C.F.; Barinas-Mitchell, E.; Brooks, M.M.; Méndez, D.D.; Naimi, A.I.; Reeves, A.; Hedderson, M.; Janssen, I.; Fabio, A. Longitudinal profiles of neighborhood socioeconomic vulnerability influence blood pressure changes across the female midlife period. Health Place 2023, 82, 103033. [Google Scholar] [CrossRef]
- Karriker-Jaffe, K.J.; Liu, H.; Johnson, R.M. Racial/ethnic differences in associations between neighborhood socioeconomic status, distress, and smoking among U.S. adults. J. Ethn. Subst. Abus. 2016, 15, 73–91. [Google Scholar] [CrossRef]
- Health Disparities in Rural Women. The American College of Obstetricians and Gynecologists. 2014. Available online: https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2014/02/health-disparities-in-rural-women (accessed on 13 October 2022).
- Cameron, N.A.; Molsberry, R.; Pierce, J.B.; Perak, A.M.; Grobman, W.A.; Allen, N.B.; Greenland, P.; Lloyd-Jones, D.M.; Khan, S.S. Pre-Pregnancy Hypertension Among Women in Rural and Urban Areas of the United States. J. Am. Coll. Cardiol. 2020, 76, 2611–2619. [Google Scholar] [CrossRef]
- Harrington, R.A.; Califf, R.M.; Balamurugan, A.; Brown, N.; Benjamin, R.M.; Braund, W.E.; Hipp, J.; Konig, M.; Sanchez, E.; Maddox, K.E.J. Call to Action: Rural Health: A Presidential Advisory from the American Heart Association and American Stroke Association. Circulation 2020, 141, e615–e644. [Google Scholar] [CrossRef]
- Macintyre, S.; Ellaway, A.; Cummins, S. Place effects on health: How can we conceptualise, operationalise and measure them? Soc. Sci. Med. 2002, 55, 125–139. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Kuh, D. Life course epidemiology. J. Epidemiol. Community Health 2003, 57, 778–783. [Google Scholar] [CrossRef]
- Krieger, N. Theories for social epidemiology in the 21st century: An ecosocial perspective. Int. J. Epidemiol. 2001, 30, 668–677. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, K.K.; Huang, X.; Cameron, N.A.; Petito, L.C.; Joseph, J.; Landon, M.B.; Grobman, W.A.; Khan, S.S. Rural-urban disparities in pregestational and gestational diabetes in pregnancy: Serial, cross-sectional analysis of over 12 million pregnancies. BJOG 2024, 131, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Tennessee Department of Health. Annual Summary Report 2020. Tennessee Pregnancy Assessment Monitoring System (PRAMS). Available online: https://www.tn.gov/content/dam/tn/health/documents/PRAMS-Summary-Report-2020.pdf (accessed on 24 February 2025).
- Gallagher, A.; Liu, J.; Probst, J.C.; Martin, A.B.; Hall, J.W. Maternal obesity and gestational weight gain in rural versus urban dwelling women in South Carolina. J. Rural. Health 2013, 29, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Dunkel Schetter, C.; Schafer, P.; Lanzi, R.G.; Clark-Kauffman, E.; Raju, T.N.K.; Hillemeier, M.M. Shedding Light on the Mechanisms Underlying Health Disparities Through Community Participatory Methods: The Stress Pathway. Perspect. Psychol. Sci. 2013, 8, 613–633. [Google Scholar] [CrossRef]
- Seguin, R.; Connor, L.; Nelson, M.; LaCroix, A.; Eldridge, G. Understanding barriers and facilitators to healthy eating and active living in rural communities. J. Nutr. Metab. 2014, 2014, 146502. [Google Scholar] [CrossRef] [PubMed]
- Beeber, L.S.; Perreira, K.M.; Schwartz, T. Supporting the Mental Health of Mothers Raising Children in Poverty. How Do We Target Them for Intervention Studies? Ann. N. Y. Acad. Sci. 2008, 1136, 86–100. [Google Scholar] [CrossRef]
- Cassells, R.C.; Evans, G.W. Ethnic Variation in Poverty and Parenting Stress. In Parental Stress and Early Child Development; Deater-Deckard, K., Panneton, R., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 15–45. [Google Scholar] [CrossRef]
- Haghighat, N.; Hu, M.; Laurent, O.; Chung, J.; Nguyen, P.; Wu, J. Comparison of birth certificates and hospital-based birth data on pregnancy complications in Los Angeles and Orange County, California. BMC Pregnancy Childbirth 2016, 16, 93. [Google Scholar] [CrossRef]
- Bodnar, L.M.; Abrams, B.; Bertolet, M.; Gernand, A.D.; Parisi, S.M.; Kimes, K.P.; Lash, T.L. Validity of birth certificate-derived maternal weight data. Paediatr. Perinat. Epidemiol. 2014, 28, 203–212. [Google Scholar] [CrossRef]
- Kemp, R.L.; Moore, B.H. Local Governments in the United States: An Overview of Cities and Counties. Bus. Public. Adm. Stud. 2011, 6, 48. [Google Scholar]
| Distribution | Risk Factor Prevalence 1 | |||||
|---|---|---|---|---|---|---|
| N | % | Diabetes | Hypertension | Obesity | Smoking | |
| Overall | 2,089,588 | 100.0% | 1.1% | 1.9% | 25.9% | 3.0% |
| Individual-level | ||||||
| Age | ||||||
| 30–35 years | 1,508,945 | 72.2% | 1.0% | 1.5% | 25.3% | 3.1% |
| 36–40 years | 497,650 | 23.8% | 1.6% | 2.5% | 27.3% | 2.6% |
| 41–45 years | 82,993 | 4.0% | 2.2% | 3.8% | 28.2% | 2.4% |
| Race/Ethnicity | ||||||
| Asian/Pacific Islander | 172,379 | 8.2% | 0.9% | 0.8% | 7.5% | 0.5% |
| Black | 214,449 | 10.3% | 1.3% | 4.2% | 37.2% | 3.8% |
| Hispanic, U.S.-born | 381,628 | 18.3% | 1.8% | 2.2% | 39.5% | 2.5% |
| Hispanic, immigrant | 486,085 | 23.3% | 1.5% | 1.3% | 24.8% | 0.5% |
| White | 835,047 | 40.0% | 0.7% | 1.7% | 21.2% | 5.0% |
| Marital status | ||||||
| Married | 1,640,361 | 78.5% | 1.0% | 1.7% | 24.0% | 2.0% |
| Not married | 449,227 | 21.5% | 1.5% | 2.5% | 32.9% | 6.5% |
| Educational attainment | ||||||
| Did not complete high school | 335,035 | 16.0% | 1.9% | 1.7% | 30.0% | 2.8% |
| High school graduate or GED | 352,839 | 16.9% | 1.6% | 2.3% | 31.5% | 5.2% |
| Some college | 368,679 | 17.6% | 1.3% | 2.4% | 34.7% | 5.6% |
| College graduate | 1,033,035 | 49.4% | 0.7% | 1.5% | 19.5% | 1.4% |
| Tract-level * (SD = standard deviation) | ||||||
| % Poor | ||||||
| <1 SD from the mean | 314,531 | 15.1% | 0.7% | 1.3% | 16.5% | 1.8% |
| Within 1 SD of the mean | 1,496,999 | 71.6% | 1.1% | 1.9% | 26.4% | 3.3% |
| >1 SD from the mean | 278,058 | 13.3% | 1.8% | 2.1% | 33.9% | 2.6% |
| % Black or African American | ||||||
| <1 SD from the mean | 0 | 0.0% | -- | -- | -- | -- |
| Within 1 SD of the mean | 1,850,450 | 88.6% | 1.1% | 1.8% | 25.2% | 3.0% |
| >1 SD from the mean | 239,138 | 11.4% | 1.4% | 2.7% | 31.5% | 3.2% |
| % Hispanic or Latino | ||||||
| <1 SD from the mean | 238,032 | 11.4% | 0.7% | 1.5% | 18.2% | 3.5% |
| Within 1 SD of the mean | 1,457,237 | 69.7% | 1.1% | 1.9% | 25.0% | 3.3% |
| >1 SD from the mean | 394,319 | 18.9% | 1.7% | 1.8% | 34.0% | 1.7% |
| County-level urban/rural status | ||||||
| Large metropolitan | 1,556,324 | 74.5% | 1.1% | 1.8% | 23.6% | 2.3% |
| Medium or small metropolitan | 402,790 | 19.3% | 1.2% | 2.0% | 31.6% | 4.2% |
| Nonmetropolitan | 130,474 | 6.2% | 1.6% | 2.8% | 35.2% | 7.5% |
| Fixed Effects | % Poor, Unadjusted | % Poor, Adjusted | % Black/African American, Unadjusted | % Black/African American, Adjusted | % Hispanic/ Latino, Unadjusted | % Hispanic/ Latino, Adjusted |
|---|---|---|---|---|---|---|
| Age | -- | 1.09 (1.09–1.10) * | -- | 1.09 (1.09–1.10) * | -- | 1.09 (1.09–1.10) * |
| Race/ethnicity | -- | -- | -- | |||
| Asian/Pacific Islander | 1.44 (1.36–1.53) * | 1.49 (1.41–1.58) * | 1.47 (1.39–1.56) * | |||
| Black | 1.62 (1.54–1.70) * | 1.71 (1.62–1.80) * | 1.68 (1.60–1.76) * | |||
| Hispanic, U.S.-born | 1.98 (1.90–2.06) * | 2.06 (1.98–2.15) * | 1.91 (1.84–1.99) * | |||
| Hispanic, immigrant | 1.33 (1.27–1.38) * | 1.42 (1.36–1.49) * | 1.31 (1.26–1.37) * | |||
| White | 1.00 | 1.00 | 1.00 | |||
| Marital status | -- | -- | -- | |||
| Married | 1.00 | 1.00 | 1.00 | |||
| Not married | 1.00 (0.97–1.02) | 1.01 (0.98–1.04) | 1.00 (0.97–1.03) | |||
| Educational attainment | -- | -- | -- | |||
| <High school | 1.90 (1.80–1.96) * | 1.99 (1.91–2.08) * | 1.91 (1.83–2.00) * | |||
| High school graduate/GED | 1.69 (1.63–1.76) * | 1.76 (1.69–1.83) * | 1.72 (1.65–1.79) * | |||
| Some college | 1.52 (1.47–1.58) * | 1.56 (1.50–1.62) * | 1.72 (1.65–1.79) * | |||
| College graduate | 1.00 | 1.00 | 1.00 | |||
| % Poor | 1.90 (1.76–1.94) * | 1.39 (1.33–1.46) * | -- | -- | -- | -- |
| % Poor 2 | 0.68 (0.65–0.72) * | 0.80 (0.80–0.85) * | ||||
| % Black or African American | -- | -- | 1.02 (1.00–1.08) | 0.99 (0.95–1.04) | -- | -- |
| % Black or African American 2 | 1.06 (1.01–1.12) ^ | 1.04 (0.99–1.09) | ||||
| % Hispanic or Latino | -- | -- | -- | -- | 2.02 (1.90–2.18) * | 1.46 (1.36–1.58) * |
| % Hispanic or Latino 2 | 0.70 (0.61–0.71) * | 0.80 (0.72–0.83) * | ||||
| Urban/rural status | -- | -- | -- | |||
| Large metropolitan | 1.00 | 1.00 | 1.00 | |||
| Medium/small metropolitan | 0.90 (0.87–0.94) * | 0.99 (0.95–1.04) | 0.97 (0.92–1.01) | |||
| Nonmetropolitan | 1.24 (1.16–1.31) * | 1.32 (1.24–1.40) * | 1.35 (1.27–1.43) * | |||
| Time | -- | -- | -- | |||
| Years 2005–2009 | 0.85 (0.81–0.88) * | 0.84 (0.81–0.87) * | 0.84 (0.81–0.87) * | |||
| Years 2010–2014 | 0.97 (0.94–1.00) | 0.97 (0.94–1.00) | 0.97 (0.94–1.00) ^ | |||
| Years 2015–2020 | 1.00 | 1.00 | 1.00 | |||
| Random effect | 0.25 | 0.19 | 0.38 | 0.22 | 0.27 | 0.20 |
| Fit statistics | ||||||
| −2 log likelihood | 257,431 | 252,130 | 258,368 | 252,361 | 257,442 | 252,187 |
| AIC | 257,439 | 252,164 | 258,376 | 252,395 | 257,450 | 252,221 |
| BIC | 257,467 | 252,285 | 258,404 | 252,516 | 257,479 | 252,342 |
| Fixed Effects | % Poor, Unadjusted | % Poor, Adjusted | % Black/African American, Unadjusted | % Black/African American, Adjusted | % Hispanic/ Latino, Unadjusted | % Hispanic/ Latino, Adjusted |
|---|---|---|---|---|---|---|
| Age | -- | 1.11 (1.10–1.11) * | -- | 1.11 (1.10–1.11) * | -- | 1.11 (1.10–1.11) * |
| Race/ethnicity | -- | -- | -- | |||
| Asian/Pacific Islander | 0.51 (0.49–0.54) * | 0.52 (0.49–0.55) * | 0.52 (0.49–0.55) * | |||
| Black | 2.11 (2.04–2.17) * | 2.09 (2.02–2.16) * | 2.12 (2.05–2.18) * | |||
| Hispanic, U.S.-born | 1.03 (1.00–1.06) | 1.08 (1.04–1.11) * | 1.03 (1.00–1.06) | |||
| Hispanic, immigrant | 0.57 (0.55–0.59) * | 0.60 (0.58–0.62) * | 0.58 (0.56–0.60) * | |||
| White | 1.00 | 1.00 | 1.00 | |||
| Marital status | -- | -- | -- | |||
| Married | 1.00 | 1.00 | 1.00 | |||
| Not married | 1.15 (1.12–1.17) * | 1.15 (1.13–1.18) * | 1.16 (1.13–1.18) * | |||
| Educational attainment | -- | -- | -- | |||
| <High school | 1.25 (1.20–1.30) * | 1.26 (1.22–1.31) * | 1.27 (1.22–1.31) * | |||
| High school graduate/GED | 1.33 (1.29–1.37) * | 1.35 (1.31–1.39) * | 1.34 (1.30–1.38) * | |||
| Some college | 1.32 (1.28–1.36) * | 1.33 (1.29–1.37) * | 1.32 (1.29–1.36) * | |||
| College graduate | 1.00 | 1.00 | 1.00 | |||
| % Poor | 1.39 (1.34–1.46) * | 1.29 (1.24–1.34) * | -- | -- | -- | -- |
| % Poor 2 | 0.78 (0.74–0.81) * | 0.82 (0.79–0.85) * | ||||
| % Black or African American | -- | -- | 1.20 (1.16–1.25) * | 1.13 (1.09–1.17) * | -- | -- |
| % Black or African American 2 | 0.99 (0.96–1.03) | 0.95 (0.91–0.98) + | ||||
| % Hispanic or Latino | -- | -- | -- | -- | 1.57 (1.47–1.70) * | 1.57 (1.48–1.67) * |
| % Hispanic or Latino 2 | 0.65 (0.61–0.69) * | 0.67 (0.62–0.71) * | ||||
| Urban/rural status | -- | -- | -- | |||
| Large metropolitan | 1.00 | 1.00 | 1.00 | |||
| Medium/small metropolitan | 1.10 (1.06–1.14) * | 1.18 (1.14–1.23) * | 1.19 (1.14–1.23) * | |||
| Nonmetropolitan | 1.49 (1.42–1.57) * | 1.63 (1.55–1.71) * | 1.63 (1.56–1.72) * | |||
| Time | -- | -- | -- | |||
| Years 2005–2009 | 0.74 (0.72–0.76) * | 0.75 (0.72–0.77) * | 0.74 (0.72–0.77) * | |||
| Years 2010–2014 | 0.88 (0.86–0.90) * | 0.89 (0.87–0.91) * | 0.89 (0.86–0.91) * | |||
| Years 2015–2020 | 1.00 | 1.00 | 1.00 | |||
| Random effect | 0.26 | 0.17 | 0.24 | 0.18 | 0.27 | 0.17 |
| Fit statistics | ||||||
| −2 log likelihood | 382,566 | 370,654 | 382,409 | 370,731 | 382,694 | 370,606 |
| AIC | 382,574 | 370,688 | 382,417 | 370,765 | 382,702 | 370,640 |
| BIC | 382,603 | 370,809 | 382,445 | 370,886 | 382,730 | 370,760 |
| Fixed Effects | % Poor, Unadjusted | % Poor, Adjusted | % Black/African American, Unadjusted | % Black/African American, Adjusted | % Hispanic/ Latino, Unadjusted | % Hispanic/ Latino, Adjusted |
|---|---|---|---|---|---|---|
| Age | -- | 1.03 (1.03–1.03) * | -- | 1.03 (1.03–1.03) * | -- | 1.03 (1.03–1.03) * |
| Race/ethnicity | -- | -- | -- | |||
| Asian/Pacific Islander | 0.33 (0.33–0.34) * | 0.33 (0.33–0.34) * | 0.34 (0.33–0.34) * | |||
| Black | 1.74 (1.72–1.76) * | 1.73 (1.71–1.75) * | 1.74 (1.72–1.76) * | |||
| Hispanic, U.S.-born | 1.72 (1.70–1.74) * | 1.73 (1.71–1.75) * | 1.70 (1.68–1.71) * | |||
| Hispanic, immigrant | 0.81 (0.80–0.82) * | 0.81 (0.81–0.82) * | 0.80 (0.79–0.81) * | |||
| White | 1.00 | 1.00 | 1.00 | |||
| Marital status | -- | -- | -- | |||
| Married | 1.00 | 1.00 | 1.00 | |||
| Not married | 1.02 (1.01–1.03) * | 1.02 (1.01–1.03) * | 1.02 (1.01–1.03) * | |||
| Educational attainment | -- | -- | -- | |||
| <High school | 1.41 (1.39–1.43) * | 1.42 (1.40–1.43) * | 1.41 (1.39–1.43) * | |||
| High school graduate/GED | 1.36 (1.34–1.37) * | 1.36 (1.35–1.37) * | 1.36 (1.35–1.37) * | |||
| Some college | 1.54 (1.53–1.56) * | 1.54 (1.53–1.56) * | 1.54 (1.53–1.56) * | |||
| College graduate | 1.00 | 1.00 | 1.00 | |||
| % Poor | 1.30 (1.28–1.33) * | 1.24 (1.22–1.26) * | -- | -- | -- | -- |
| % Poor 2 | 0.86 (0.84–0.87) * | 0.88 (0.86–0.89) * | ||||
| % Black or African American | -- | -- | 1.07 (1.04–1.09) * | 1.13 (1.11–1.16) * | -- | -- |
| % Black or African American 2 | 1.02 (1.00–1.05) | 0.95 (0.93–0.97) * | ||||
| % Hispanic or Latino | -- | -- | -- | -- | 1.32 (1.27–1.37) * | 1.34 (1.30–1.39) * |
| % Hispanic or Latino 2 | 0.94 (0.91–0.98) + | 0.85 (0.82–0.88) * | ||||
| Urban/rural status | -- | -- | -- | |||
| Large metropolitan | 1.00 | 1.00 | 1.00 | |||
| Medium/small metropolitan | 1.28 (1.25–1.31) * | 1.40 (1.37–1.44) * | 1.29 (1.26–1.32) * | |||
| Nonmetropolitan | 1.49 (1.45–1.54) * | 1.61 (1.56–1.66) * | 1.58 (1.54–1.63) * | |||
| Time | -- | -- | -- | |||
| Years 2005–2009 | 0.74 (0.73–0.75) * | 0.74 (0.73–0.75) * | 0.74 (0.73–0.75) * | |||
| Years 2010–2014 | 0.86 (0.85–0.86) * | 0.86 (0.85–0.86) * | 0.86 (0.85–0.86) * | |||
| Years 2015–2020 | 1.00 | 1.00 | 1.00 | |||
| Random effect | 0.29 | 0.16 | 0.35 | 0.18 | 0.29 | 0.16 |
| Fit statistics | ||||||
| −2 log likelihood | 2,285,395 | 2,213,221 | 2,286,169 | 2,213,688 | 2,284,944 | 2,213,103 |
| AIC | 2,285,403 | 2,213,255 | 2,286,177 | 2,213,722 | 2,284,952 | 2,213,137 |
| BIC | 2,285,432 | 2,213,376 | 2,286,205 | 2,213,843 | 2,284,980 | 2,213,258 |
| Fixed Effects | % Poor, Unadjusted | % Poor, Adjusted | % Black/African American, Unadjusted | % Black/African American, Adjusted | % Hispanic/ Latino, Unadjusted | % Hispanic/ Latino, Adjusted |
|---|---|---|---|---|---|---|
| Age | -- | 0.99 (0.99–0.99) * | -- | 0.99 (0.99–0.99) * | -- | 0.99 (0.99–0.99) * |
| Race/ethnicity | -- | -- | -- | |||
| Asian/Pacific Islander | 0.16 (0.15–0.17) * | 0.16 (0.15–0.17) * | 0.16 (0.15–0.17) * | |||
| Black | 0.42 (0.41–0.44) * | 0.41 (0.40–0.43) * | 0.42 (0.41–0.43) * | |||
| Hispanic, U.S.-born | 0.25 (0.25–0.26) * | 0.25 (0.25–0.26) * | 0.28 (0.27–0.28) * | |||
| Hispanic, immigrant | 0.04 (0.04–0.04) * | 0.04 (0.04–0.04) * | 0.04 (0.04–0.04) * | |||
| White | 1.00 | 1.00 | 1.00 | |||
| Marital status | -- | -- | -- | |||
| Married | 1.00 | 1.00 | 1.00 | |||
| Not married | 2.95 (2.89–3.00) * | 2.94 (2.89–3.00) * | 2.99 (2.94–3.05) * | |||
| Educational attainment | -- | -- | -- | |||
| <High school | 4.99 (4.83–5.15) * | 5.02 (4.87–5.19) * | 5.20 (5.03–5.37) * | |||
| High school graduate/GED | 3.84 (3.75–3.94) * | 3.85 (3.75–3.95) * | 3.94 (3.85–4.05) * | |||
| Some college | 3.24 (3.16–3.32) * | 3.28 (3.20–3.36) * | 3.34 (3.26–3.42) * | |||
| College graduate | 1.00 | 1.00 | 1.00 | |||
| % Poor | 1.19 (1.14–1.24) * | 1.19 (1.14–1.23) * | -- | -- | -- | -- |
| % Poor 2 | 0.83 (0.79–0.87) * | 0.83 (0.80–0.86) * | ||||
| % Black or African American | -- | -- | 0.99 (0.94–1.04) | 1.13 (1.09–1.18) * | -- | -- |
| % Black or African American 2 | 1.06 (1.01–1.11) ^ | 0.92 (0.89–0.96) * | ||||
| % Hispanic or Latino | -- | -- | -- | -- | 1.25 (1.16–1.36) * | 1.72 (1.62–1.83) * |
| % Hispanic or Latino 2 | 0.59 (0.54–0.64) * | 0.47 (0.44–0.50) * | ||||
| Urban/rural status | -- | -- | -- | |||
| Large metropolitan | 1.00 | 1.00 | 1.00 | |||
| Medium/small metropolitan | 1.66 (1.59–1.73) * | 1.73 (1.66–1.80) * | 2.01 (1.93–2.09) * | |||
| Nonmetropolitan | 2.35 (2.24–2.50) * | 2.49 (2.38–2.61) * | 2.56 (2.44–2.68) * | |||
| Time | -- | -- | -- | |||
| Years 2005–2009 | 1.43 (1.39–1.46) * | 1.43 (1.40–1.46) * | 1.44 (1.40–1.47) * | |||
| Years 2010–2014 | 1.29 (1.26–1.31) * | 1.29 (1.26–1.31) * | 1.29 (1.27–1.32) * | |||
| Years 2015–2020 | 1.00 | 1.00 | 1.00 | |||
| Random effect | 1.03 | 0.29 | 1.05 | 0.29 | 0.93 | 0.25 |
| Fit statistics | ||||||
| −2 log likelihood | 525,279 | 458,737 | 525,330 | 458,744 | 524,716 | 457,971 |
| AIC | 525,287 | 458,771 | 525,338 | 458,778 | 524,724 | 458,005 |
| BIC | 525,315 | 458,892 | 525,367 | 458,899 | 524,752 | 458,125 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cubbin, C.; La Frinere-Sandoval, Q.N.B.; Widen, E.M. Social Inequities in Cardiovascular Disease Risk Factors at Multiple Levels Persist Among Mothers in Texas. Int. J. Environ. Res. Public Health 2025, 22, 404. https://doi.org/10.3390/ijerph22030404
Cubbin C, La Frinere-Sandoval QNB, Widen EM. Social Inequities in Cardiovascular Disease Risk Factors at Multiple Levels Persist Among Mothers in Texas. International Journal of Environmental Research and Public Health. 2025; 22(3):404. https://doi.org/10.3390/ijerph22030404
Chicago/Turabian StyleCubbin, Catherine, Quynh Nhu (Natasha) B. La Frinere-Sandoval, and Elizabeth M. Widen. 2025. "Social Inequities in Cardiovascular Disease Risk Factors at Multiple Levels Persist Among Mothers in Texas" International Journal of Environmental Research and Public Health 22, no. 3: 404. https://doi.org/10.3390/ijerph22030404
APA StyleCubbin, C., La Frinere-Sandoval, Q. N. B., & Widen, E. M. (2025). Social Inequities in Cardiovascular Disease Risk Factors at Multiple Levels Persist Among Mothers in Texas. International Journal of Environmental Research and Public Health, 22(3), 404. https://doi.org/10.3390/ijerph22030404






