Feasibility and Preliminary Efficacy of Enhanced Midwifery Care to Support Women Experiencing Subclinical Depression: A Pilot Randomised Controlled Trial
Highlights
- Subclinical depression in the perinatal period is common and under-recognized, and may increase risk for later clinical depression and adverse outcomes for mothers and infants.
- This study focuses on women from ethnically diverse communities in South Western Sydney, where barriers to mental health and maternity care are well documented.
- This pilot RCT shows that enhanced midwifery care can be delivered with good fidelity in a hard-to-reach population, underscoring its potential to reduce perinatal mental health inequities.
- The findings provide early, implementation-relevant evidence to inform scalable, integrated models of perinatal mental health support within routine antenatal care.
- The findings of this study reiterate the importance of early identification and proactive support for women with subclinical depressive symptoms, highlighting the need to strengthen early intervention pathways in antenatal care.
- Integrating enhanced midwifery continuity with multidisciplinary support may represent a promising, feasible framework to strengthen engagement among vulnerable groups; adequately powered trials are needed to determine effectiveness and optimise retention.
Abstract
1. Background
2. Methods
2.1. Study Design, Sites, and Participants
2.2. Randomisation and Allocation Concealment
2.3. Intervention and Control Groups
2.4. Data Collection and Outcomes
2.5. Primary Outcome
2.6. Secondary Outcomes
2.7. Sample Size Calculation
2.8. Data Analysis
3. Results
3.1. Participant Characteristics
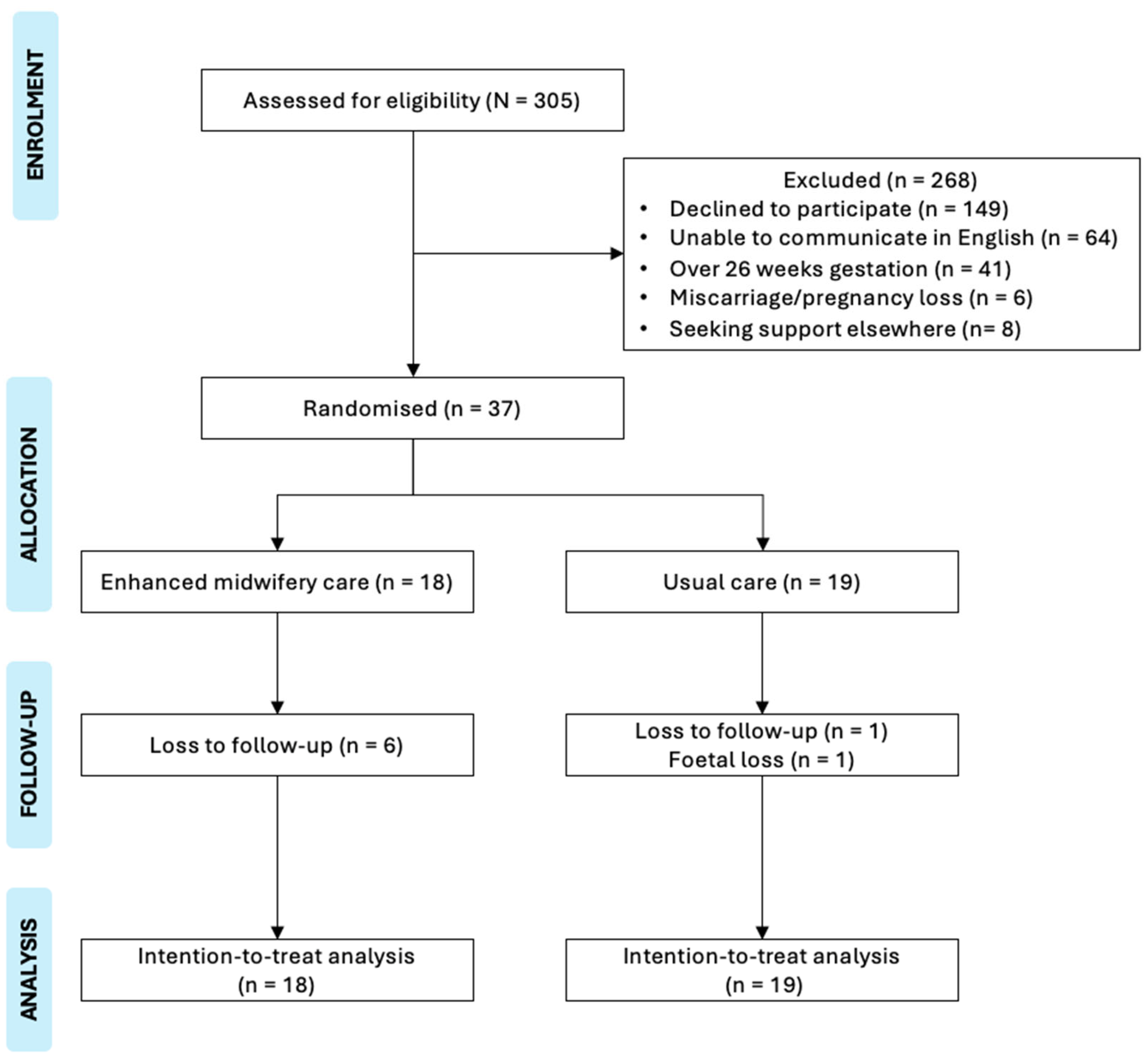
3.2. Feasibility Outcomes
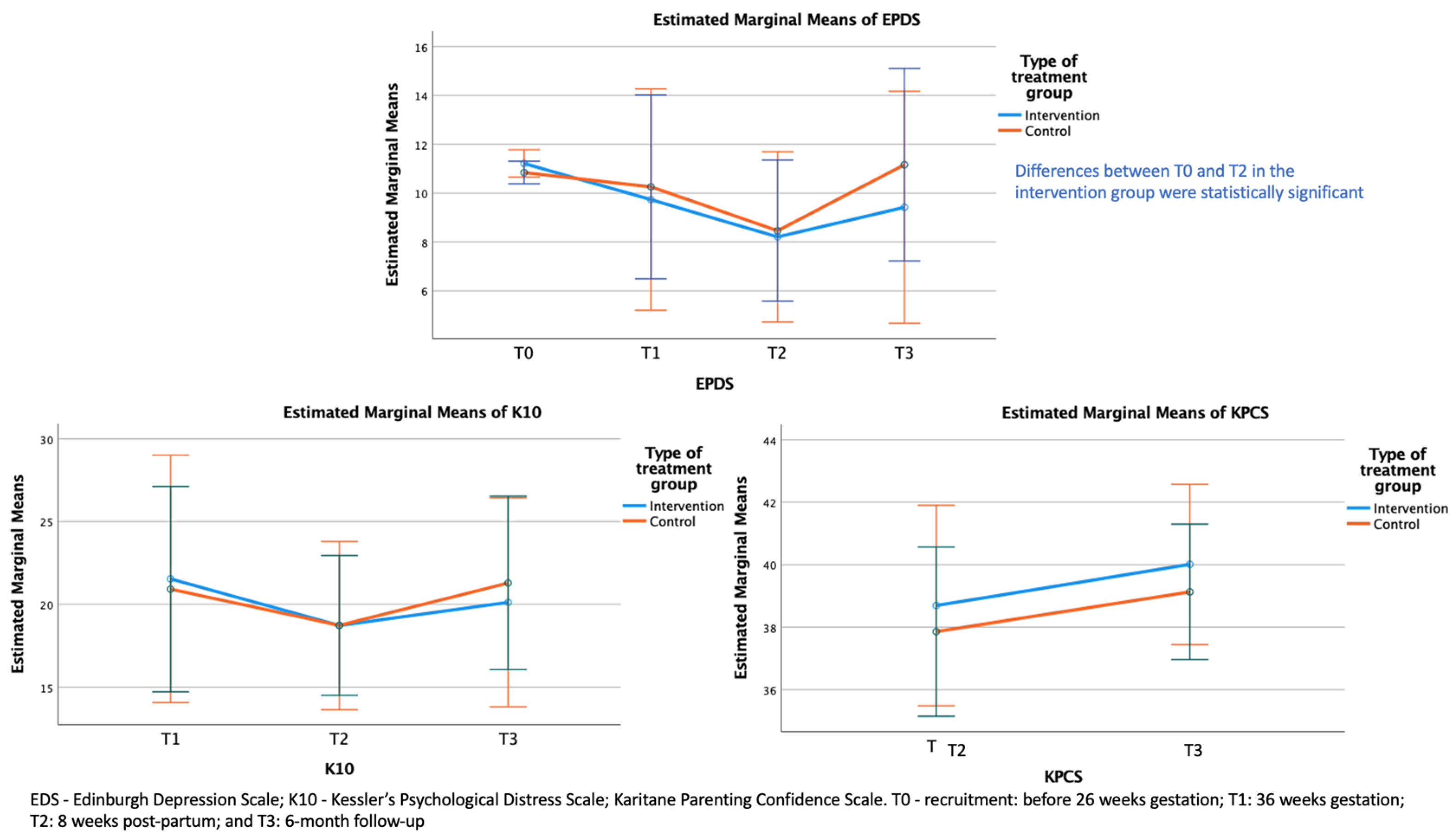
3.3. Findings of the Linear Mixed-Effects Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CALD | Culturally and Linguistically Diverse |
| CFHNs | Child and Family Health Nurses |
| EDS | Edinburgh Depression Scale |
| GPs | General Practitioners |
| ITT | Intention to Treat |
| K10 | Kessler’s Psychological distress |
| KPCS | Karitane Parenting Confidence Scale |
| NSW | New South Wales |
| RCT | Randomised Controlled Trial |
| RM | Research Midwife |
| SPSS | Statistical Package for the Social Sciences |
| SWSLHD | South Western Sydney Local Health District |
References
- Rallis, S.; Skouteris, H.; McCabe, M.; Milgrom, J. The transition to motherhood: Towards a broader understanding of perinatal distress. Women Birth 2014, 27, 68–71. [Google Scholar] [CrossRef]
- Schetter, C.D.; Tanner, L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr. Opin. Psychiatry 2012, 25, 141. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Sun, N.; Jiang, N.; Xu, X.; Gan, Y.; Zhang, J.; Qiu, L.; Yang, C.; Shi, X.; Chang, J. Prevalence and associated factors of antenatal depression: Systematic reviews and meta-analyses. Clin. Psychol. Rev. 2021, 83, 101932. [Google Scholar] [CrossRef] [PubMed]
- Ogbo, F.A.; Eastwood, J.; Hendry, A.; Jalaludin, B.; Agho, K.E.; Barnett, B.; Page, A. Determinants of antenatal depression and postnatal depression in Australia. BMC Psychiatry 2018, 18, 49. [Google Scholar] [CrossRef] [PubMed]
- Firth, A.D.; Haith-Cooper, M. Vulnerable migrant women and postnatal depression: A case of invisibility in maternity services? Br. J. Midwifery 2018, 26, 78–84. [Google Scholar] [CrossRef][Green Version]
- Rogers, A.; Obst, S.; Teague, S.J.; Rossen, L.; Spry, E.A.; Macdonald, J.A.; Sunderland, M.; Olsson, C.A.; Youssef, G.; Hutchinson, D. Association between maternal perinatal depression and anxiety and child and adolescent development: A meta-analysis. JAMA Pediatr. 2020, 174, 1082–1092. [Google Scholar] [CrossRef]
- Lee, Y.-L.; Tien, Y.; Bai, Y.-S.; Lin, C.-K.; Yin, C.-S.; Chung, C.-H.; Sun, C.-A.; Huang, S.-H.; Huang, Y.-C.; Chien, W.-C. Association of postpartum depression with maternal suicide: A nationwide population-based study. Int. J. Environ. Res. Public Health 2022, 19, 5118. [Google Scholar] [CrossRef]
- Productivity Commission. The Cost of Perinatal Depression and Anxiety in Australia. 2019. Available online: https://assets.pc.gov.au/__data/assets/pdf_file/0017/250811/sub752-mental-health-attachment.pdf (accessed on 11 January 2024).
- Khan, Z.; Vowles, Z.; Fernandez Turienzo, C.; Barry, Z.; Brigante, L.; Downe, S.; Easter, A.; Harding, S.; McFadden, A.; Montgomery, E. Targeted health and social care interventions for women and infants who are disproportionately impacted by health inequalities in high-income countries: A systematic review. Int. J. Equity Health 2023, 22, 131. [Google Scholar] [CrossRef]
- Sharma, S.; Jegadeesh, G.; Raynes-Greenow, C.; Gordon, A.; Gunawardhana, G.; Muscat, D.M. How have interventions targeting pregnant women from refugee, migrant and culturally and linguistically diverse backgrounds living in high-income countries been developed or tailored to meet community needs? A systematic scoping review of stillbirth-related literature. BMC Pregnancy Childbirth 2025, 25, 103. [Google Scholar]
- NSW Health. SAFE START Strategic Policy. 2010. Available online: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2010_016.pdf (accessed on 12 February 2023).
- Cox, J.; Holden, J. Perinatal Mental Health: A Guide to the Edinburgh Postnatal Depression Scale (EPDS); Royal College of Psychiatrists: London, UK, 2003; Available online: https://psycnet.apa.org/record/2004-14522-000 (accessed on 23 February 2023).
- Highet, N.J.; The Expert Working Group and Expert Subcommittees. Mental Health Care in the Perinatal Period: Australian Clinical Practice Guideline; Centre of Perinatal Excellence (COPE): Melbourne, VIC, Australia, 2023; Available online: https://www.cope.org.au/uploads/images/Health-professionals/COPE_2023_Perinatal_Mental_Health_Practice_Guideline.pdf (accessed on 11 March 2023).
- Matthey, S.; Phillips, J.; White, T.; Glossop, P.; Hopper, U.; Panasetis, P.; Petridis, A.; Larkin, M.; Barnett, B. Routine psychosocial assessment of women in the antenatal period: Frequency of risk factors and implications for clinical services. Arch. Women’s Ment. Health 2004, 7, 223–229. [Google Scholar] [CrossRef]
- Noonan, M.; Jomeen, J.; Galvin, R.; Doody, O. Survey of midwives’ perinatal mental health knowledge, confidence and attitudes and learning needs. Women Birth 2018, 31, e358–e366. [Google Scholar] [CrossRef] [PubMed]
- Austin, M. Marce International Society position statement on psychosocial assessment and depression screening in perinatal women. Best Pract. Res. Clin. Obstet. Gynaecol. 2014, 28, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Austin, M. Antental screening and early intervention for ‘perinatal’ distress, depression and anxiety: Where to from here? Arch. Women’s Ment. Health 2004, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Dong, V.; Montgomery, A.; Adily, P.; Eastwood, J. Antenatal depression risk under the NSW SAFE START Strategic Policy: Who is missing out on universal screening? J. Paediatr. Child Health 2023, 59, 906–911. [Google Scholar] [CrossRef]
- Wohler, Y.; Dantas, J.A. Barriers accessing mental health services among culturally and linguistically diverse (CALD) immigrant women in Australia: Policy implications. J. Immigr. Minor. Health 2017, 19, 697–701. [Google Scholar] [CrossRef]
- Cibralic, S.; Pickup, W.; Diaz, A.M.; Kohlhoff, J.; Karlov, L.; Stylianakis, A.; Schmied, V.; Barnett, B.; Eapen, V. The impact of midwifery continuity of care on maternal mental health: A narrative systematic review. Midwifery 2023, 116, 103546. [Google Scholar] [CrossRef]
- Homer, C.; Brodie, P.; Sandall, J.; Leap, N. Midwifery Continuity of Care; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Sandall, J.; Soltani, H.; Gates, S.; Shennan, A.; Devane, D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst. Rev. 2016, 2016, CD004667. [Google Scholar] [CrossRef]
- Kildea, S.; Simcock, G.; Liu, A.; Elgbeili, G.; Laplante, D.P.; Kahler, A.; Austin, M.-P.; Tracy, S.; Kruske, S.; Tracy, M.; et al. Continuity of midwifery carer moderates the effects of prenatal maternal stress on postnatal maternal wellbeing: The Queensland flood study. Arch. Women’s Ment. Health 2018, 21, 203–214. [Google Scholar] [CrossRef]
- Bradford, B.F.; Wilson, A.N.; Portela, A.; McConville, F.; Fernandez Turienzo, C.; Homer, C.S. Midwifery continuity of care: A scoping review of where, how, by whom and for whom? PLOS Global Public Health 2022, 2, e0000935. [Google Scholar] [CrossRef]
- Hopewell, S.; Chan, A.W.; Collins, G.S.; Hróbjartsson, A.; Moher, D.; Schulz, K.F.; Tunn, R.; Aggarwal, R.; Berkwits, M.; Berlin, J.A.; et al. CONSORT 2025 Statement: Updated guideline for reporting randomised trials. BMJ. 2025, 388, e081123. [Google Scholar] [CrossRef]
- Kianersi, S.; Luetke, M.; Ludema, C.; Valenzuela, A.; Rosenberg, M. Use of research electronic data capture (REDCap) in a COVID-19 randomized controlled trial: A practical example. BMC Med. Res. Methodol. 2021, 21, 175. [Google Scholar] [CrossRef]
- Gamble, J.; Creedy, D.; Moyle, W.; Webster, J.; McAllister, M.; Dickson, P. Effectiveness of a Counseling Intervention after a Traumatic Childbirth: A Randomized Controlled Trial. Birth 2005, 32, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Matthey, S.; Kavanagh, D.J.; Howie, P.; Barnett, B.; Charles, M. Prevention of postnatal distress or depression: An evaluation of an intervention at preparation for parenthood classes. J. Affect. Disord. 2004, 79, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Reading, R. Child and family outcomes of a long-term nurse home visitation programme: A randomised controlled trial. Child Care Health Dev. 2011, 37, 755–756. [Google Scholar] [CrossRef]
- Milani, H.S.M.D.M.P.H.; Azargashb, E.P.; Beyraghi, N.M.D.; Defaie, S.M.D.; Asbaghi, T.M.D. Effect of Telephone-Based Support on Postpartum Depression: A Randomized Controlled Trial. Int. J. Fertil. Steril. 2015, 9, 247–253. [Google Scholar]
- Oommen, H.; Rantanen, A.; Kaunonen, M.; Tarkka, M.-T.; Salonen, A.H. Social support provided to Finnish mothers and fathers by nursing professionals in the postnatal ward. Midwifery 2011, 27, 754–761. [Google Scholar] [CrossRef]
- Grote, N.K.; Katon, W.J.; Lohr, M.J.; Carson, K.; Curran, M.; Galvin, E.; Russo, J.E.; Gregory, M. Culturally relevant treatment services for perinatal depression in socio-economically disadvantaged women: The design of the MOMCare study. Contemp. Clin. Trials 2014, 39, 34–49. [Google Scholar] [CrossRef]
- Matthey, S.; Fisher, J.; Rowe, H. Using the Edinburgh postnatal depression scale to screen for anxiety disorders: Conceptual and methodological considerations. J. Affect. Disord. 2013, 146, 224–230. [Google Scholar] [CrossRef]
- Matthey, S. Using the Edinburgh Postnatal Depression Scale to screen for anxiety disorders. Depress. Anxiety 2008, 25, 926–931. [Google Scholar] [CrossRef]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.-L.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Črnčec, R.; Barnett, B.; Matthey, S. Karitane Parenting Confidence Scale; Sydney South West Area Health Service: Liverpool, UK, 2008. [Google Scholar]
- Chakraborty, H.; Gu, H. A mixed model approach for intent-to-treat analysis in longitudinal clinical trials with missing values. RTI Press 2009, 2–9. [Google Scholar] [CrossRef]
- Marshall, S.; Xu, H.; Taki, S.; Laird, Y.; Love, P.; Wen, L.M.; Rissel, C. Engagement, satisfaction, retention and behavioural outcomes of linguistically diverse mothers and infants participating in an Australian early obesity prevention trial. Health Promot. J. Aust. 2022, 33, 350–360. [Google Scholar] [CrossRef]
- Frew, P.M.; Saint-Victor, D.S.; Isaacs, M.B.; Kim, S.; Swamy, G.K.; Sheffield, J.S.; Edwards, K.M.; Villafana, T.; Kamagate, O.; Ault, K. Recruitment and retention of pregnant women into clinical research trials: An overview of challenges, facilitators, and best practices. Clin. Infect. Dis. 2014, 59 (Suppl. S7), S400–S407. [Google Scholar] [CrossRef]
- Khanlari, S.; Eastwood, J.; Barnett, B.; Naz, S.; Ogbo, F.A. Psychosocial and obstetric determinants of women signalling distress during Edinburgh Postnatal Depression Scale (EPDS) screening in Sydney, Australia. BMC Pregnancy Childbirth 2019, 19, 407. [Google Scholar] [CrossRef]
- South Western Sydney Local Health District. Engaging Culturally and Linguistically Diverse (CALD) Communities in Health Research. Available online: https://www.swslhd.health.nsw.gov.au/pdfs/cald.pdf (accessed on 25 January 2023).
- Morrell, C.J.; Sutcliffe, P.; Booth, A.; Stevens, J.; Scope, A.; Stevenson, M.; Harvey, R.; Bessey, A.; Cantrell, A.; Dennis, C.-L. A systematic review, evidence synthesis and meta-analysis of quantitative and qualitative studies evaluating the clinical effectiveness, the cost-effectiveness, safety and acceptability of interventions to prevent postnatal depression. Health Technol. Assess. 2016, 20, 1–414. [Google Scholar] [CrossRef]
- D’haenens, F.; Van Rompaey, B.; Swinnen, E.; Dilles, T.; Beeckman, K. The effects of continuity of care on the health of mother and child in the postnatal period: A systematic review. Eur. J. Public Health 2020, 30, 749–760. [Google Scholar] [CrossRef]
- Barr, K.R.; Nguyen, T.A.; Pickup, W.; Cibralic, S.; Mendoza Diaz, A.; Barnett, B.; Eapen, V. Perinatal continuity of care for mothers with depressive symptoms: Perspectives of mothers and clinicians. Front. Psychiatry 2024, 15, 1385120. [Google Scholar] [CrossRef]
| Variables | Intervention Group (N = 18) n (%) | Control Group (N = 19) n (%) | p-Value |
|---|---|---|---|
| Mother’s age in years, mean (SD) | 29.1 (7.1) | 30.6 (6.0) | 0.501 |
| Number of weeks pregnant, mean (SD) | 18.4 (4.5) | 19.3 (3.5) | 0.514 |
| Country of birth | 0.618 | ||
| Australia | 10 (55.6) | 9 (47.4) | |
| Other | 8 (44.4) | 10 (52.6) | |
| Ethnicity | 0.632 | ||
| Caucasian | 6 (33.3) | 5 (26.3) | |
| Non-Caucasian | 11 (61.1) | 13 (68.4) | |
| Missing/Undisclosed | 1 (5.6) | 1 (5.3) | |
| Language spoken at home | 0.800 | ||
| English | 13 (72.2) | 16 (84.2) | |
| Other | 5 (27.8) | 3 (15.8) | |
| CALD status * | 0.632 | ||
| No | 6 (33.3) | 5 (26.3) | |
| Yes | 11 (61.1) | 13 (68.4) | |
| Missing/Undisclosed | 1 (5.6) | 1 (5.3) | |
| Indigenous status | 0.604 a | ||
| No | 17 (94.4) | 16 (84.2) | |
| Yes | 1 (5.6) | 3 (15.8) | |
| Smoking status | 1.000 a | ||
| No | 17 (94.4) | 18 (94.7) | |
| Yes | 1 (5.6) | 1 (5.3) | |
| EDS at baseline, mean (SD) | 11.11 (0.83) | 10.84 (0.77) | 0.313 |
| K10 at baseline, mean (SD) | 19.50 (8.31) | 19.63 (10.42) | 0.973 |
| Outcomes | β | SE | p-Value | |
|---|---|---|---|---|
| EDS | Intercept | 16.42 | 4.34 | 0.001 |
| Treatment (Reference = Control) | −0.02 | 1.63 | 0.992 | |
| Time (Ref = T0) | ||||
| T1 | −1.50 | 1.39 | 0.283 | |
| T2 | −2.77 | 1.36 | 0.045 | |
| T3 | −1.14 | 1.39 | 0.414 | |
| Time (Ref = T0) × Treatment (Ref = Control) | ||||
| Time (T1) × Treatment (Intervention) | −1.15 | 2.08 | 0.581 | |
| Time (T2) × Treatment (Intervention) | −1.34 | 2.10 | 0.524 | |
| Time (T3) × Treatment (Intervention) | −1.80 | 2.08 | 0.389 | |
| K10 scale | Intercept | 27.04 | 9.19 | 0.007 |
| Treatment (Ref = Control) | −0.58 | 3.20 | 0.856 | |
| Time (Ref = T1) | ||||
| T2 | −1.20 | 1.93 | 0.535 | |
| T3 | 1.06 | 1.97 | 0.593 | |
| Time (Ref = T1) × Treatment (Ref = Control) | ||||
| Time (T2) × Treatment (Intervention) | −1.05 | 3.02 | 0.729 | |
| Time (T3) × Treatment (Intervention) | −1.99 | 2.99 | 0.509 | |
| KPCS | Intercept | 34.30 | 4.65 | <0.001 |
| Treatment (Ref = Control) | 0.87 | 1.58 | 0.584 | |
| Time (Ref = T2) | ||||
| T3 | 1.44 | 1.03 | 0.176 | |
| Time (Ref = T2) × Treatment (Ref = Control) | ||||
| Time (T3) × Treatment (Intervention) | −0.31 | 1.60 | 0.847 | |
| Contrast | Estimate | SE | p-Value |
|---|---|---|---|
| T0–T1 | 2.08 | 1.04 | 0.199 |
| T0–T2 | 3.44 | 1.05 | 0.008 |
| T0–T3 | 2.04 | 1.04 | 0.212 |
| T1–T2 | 1.36 | 1.11 | 0.613 |
| T1–T3 | −0.03 | 1.10 | 1.000 |
| T2–T3 | −1.40 | 1.11 | 0.594 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
John, J.R.; Pickup, W.; Mendoza Diaz, A.; Cibralic, S.; Heys, A.; Schmied, V.; Barnett, B.; Eapen, V. Feasibility and Preliminary Efficacy of Enhanced Midwifery Care to Support Women Experiencing Subclinical Depression: A Pilot Randomised Controlled Trial. Int. J. Environ. Res. Public Health 2025, 22, 1835. https://doi.org/10.3390/ijerph22121835
John JR, Pickup W, Mendoza Diaz A, Cibralic S, Heys A, Schmied V, Barnett B, Eapen V. Feasibility and Preliminary Efficacy of Enhanced Midwifery Care to Support Women Experiencing Subclinical Depression: A Pilot Randomised Controlled Trial. International Journal of Environmental Research and Public Health. 2025; 22(12):1835. https://doi.org/10.3390/ijerph22121835
Chicago/Turabian StyleJohn, James R., Wendy Pickup, Antonio Mendoza Diaz, Sara Cibralic, Aleisha Heys, Virginia Schmied, Bryanne Barnett, and Valsamma Eapen. 2025. "Feasibility and Preliminary Efficacy of Enhanced Midwifery Care to Support Women Experiencing Subclinical Depression: A Pilot Randomised Controlled Trial" International Journal of Environmental Research and Public Health 22, no. 12: 1835. https://doi.org/10.3390/ijerph22121835
APA StyleJohn, J. R., Pickup, W., Mendoza Diaz, A., Cibralic, S., Heys, A., Schmied, V., Barnett, B., & Eapen, V. (2025). Feasibility and Preliminary Efficacy of Enhanced Midwifery Care to Support Women Experiencing Subclinical Depression: A Pilot Randomised Controlled Trial. International Journal of Environmental Research and Public Health, 22(12), 1835. https://doi.org/10.3390/ijerph22121835







