Using Spatial Technologies to Assess Risk Factors for Diarrheal Disease Under Environmental Variability in Bangladesh: A Machine Learning Study
Abstract
1. Introduction
2. Methods
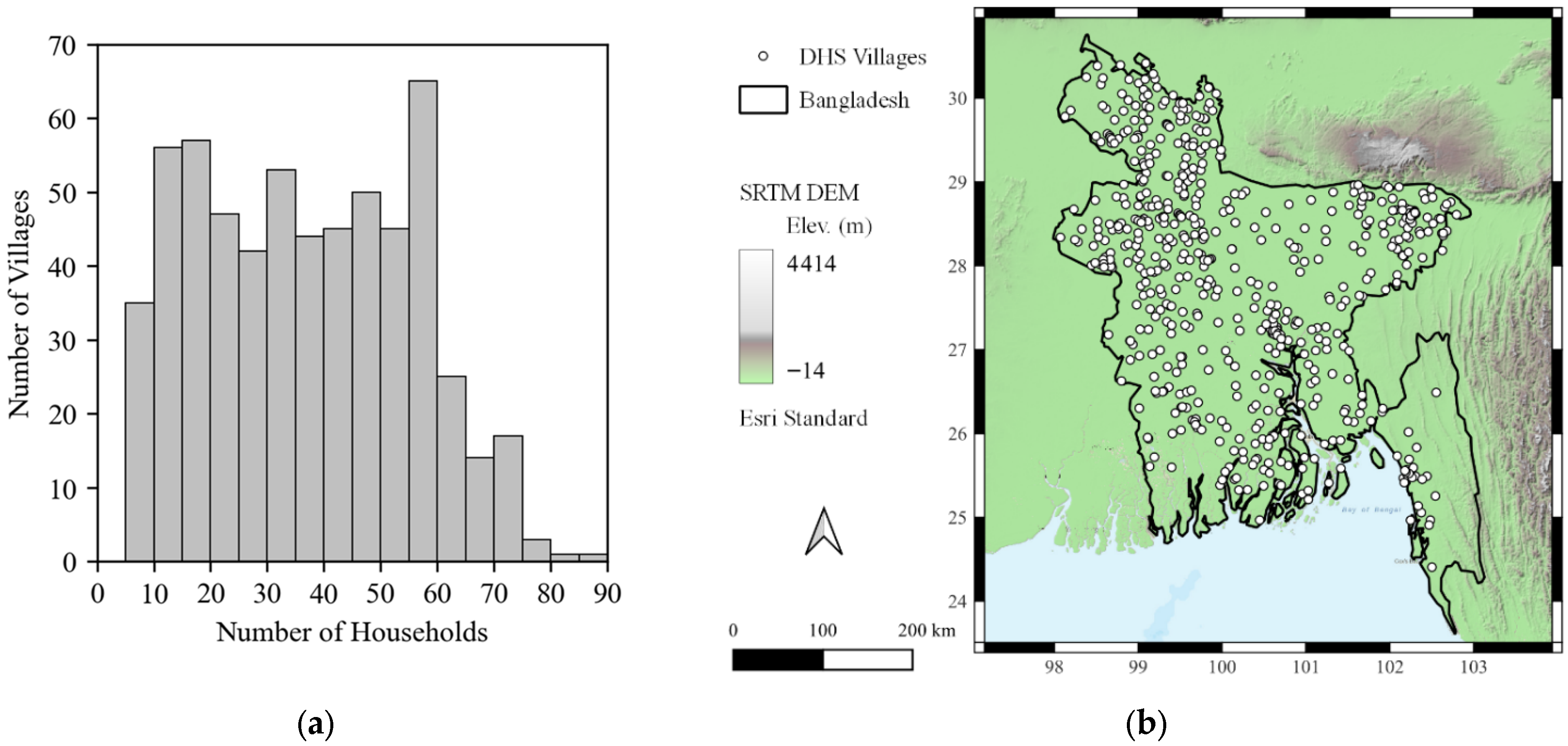
2.1. Data Preparation
2.2. Random Forest Classifier Models
3. Results
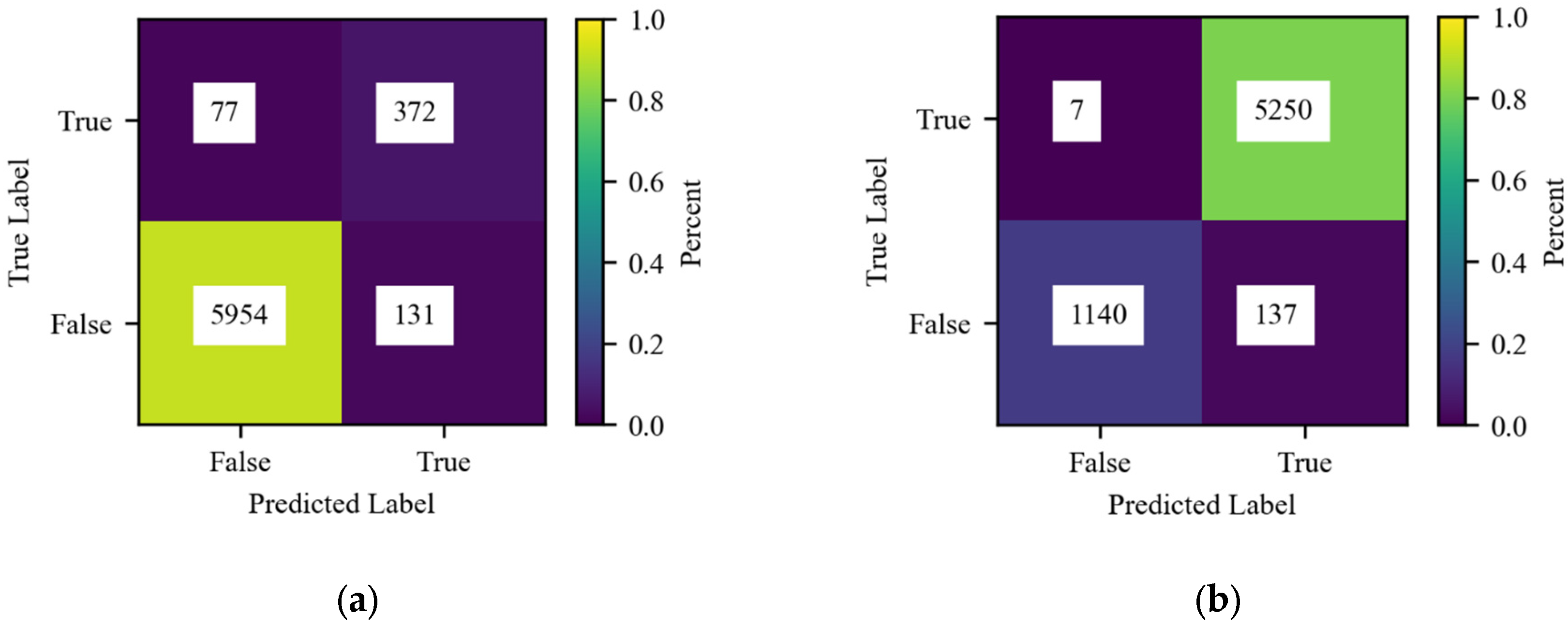
3.1. Model Performance
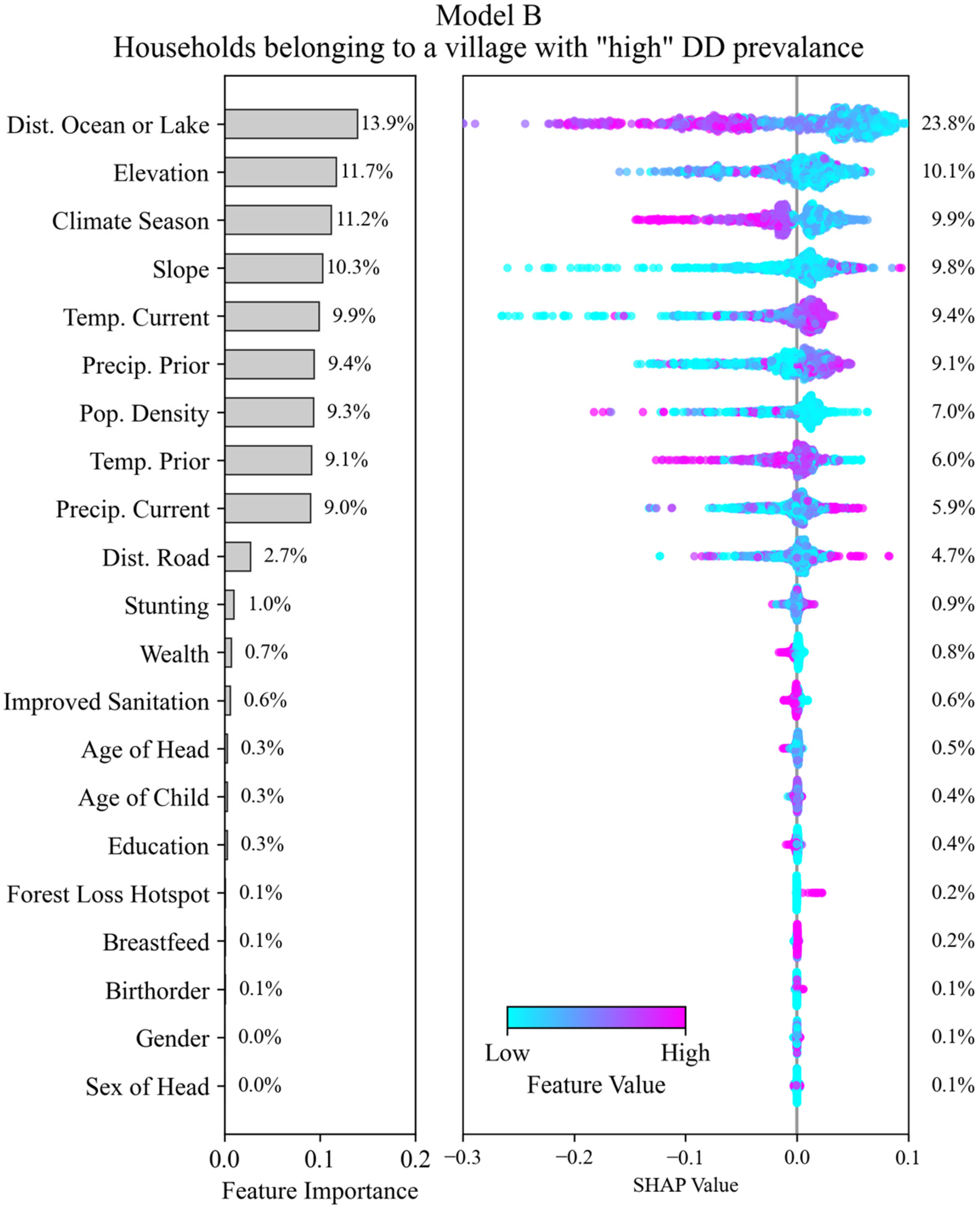
3.2. Interpretation of SHAP Values
3.3. Model A—Prediction of DD Outcomes at the Household Level
3.4. Model B—Prediction of Households Belonging to High or Low DD Occurrence Villages
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DD | Diarrheal Disease. |
| DALYs | Disability-Adjusted Life Years |
| LMICs | Low- and Middle-Income Countries |
| WHO | World Health Organization |
| IPCC | Intergovernmental Panel on Climate Change |
| WASH | Water, Sanitation, and Hygiene |
| DHS | Demographic and Health Surveys |
| HH | Household |
| IDs | Identifiers |
| CHIRPS | Climate Hazards Group InfraRed Precipitation with Stations |
| CHIRTS | Climate Hazards Group InfraRed Temperature with Stations |
| RF | Random Forest |
| SHAP | Shapley Additive Explanations |
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Bakir, H.; Hadi, M.; Jurdi, M. Towards a renewed public health regulatory and surveillance role in water, sanitation and hygiene. East. Mediterr. Health J. 2017, 23, 525–526. [Google Scholar] [CrossRef]
- Hodge, J.; Chang, H.H.; Boisson, S.; Collin, S.M.; Peletz, R.; Clasen, T. Assessing the Association between Thermotolerant Coliforms in Drinking Water and Diarrhea: An Analysis of Individual-Level Data from Multiple Studies. Environ. Health Perspect. 2016, 124, 1560–1567. [Google Scholar] [CrossRef] [PubMed]
- Demissie, G.D.; Yeshaw, Y.; Aleminew, W.; Akalu, Y. Diarrhea and associated factors among under five children in sub-Saharan Africa: Evidence from demographic and health surveys of 34 sub-Saharan countries. PLoS ONE 2021, 16, e0257522. [Google Scholar] [CrossRef]
- Meki, C.D.; Ncube, E.J.; Voyi, K. Frameworks for mitigating the risk of waterborne diarrheal diseases: A scoping review. PLoS ONE 2022, 17, e0278184. [Google Scholar] [CrossRef]
- Mertens, A.; Balakrishnan, K.; Ramaswamy, P.; Rajkumar, P.; Ramaprabha, P.; Durairaj, N.; Hubbard, A.E.; Khush, R.; Colford, J.M., Jr.; Arnold, B.F. Associations between High Temperature, Heavy Rainfall, and Diarrhea among Young Children in Rural Tamil Nadu, India: A Prospective Cohort Study. Environ. Health Perspect. 2019, 127, 47004. [Google Scholar] [CrossRef]
- Levy, K.; Woster, A.P.; Goldstein, R.S.; Carlton, E.J. Untangling the Impacts of Climate Change on Waterborne Diseases: A Systematic Review of Relationships between Diarrheal Diseases and Temperature, Rainfall, Flooding, and Drought. Environ. Sci. Technol. 2016, 50, 4905–4922. [Google Scholar] [CrossRef]
- Carlton, E.J.; Eisenberg, J.N.S.; Goldstick, J.; Cevallos, W.; Trostle, J.; Levy, K. Heavy Rainfall Events and Diarrhea Incidence: The Role of Social and Environmental Factors. Am. J. Epidemiol. 2014, 179, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Levy, K.; Hubbard, A.E.; Nelson, K.L.; Eisenberg, J.N.S. Drivers of Water Quality Variability in Northern Coastal Ecuador. Environ. Sci. Technol. 2009, 43, 1788–1797. [Google Scholar] [CrossRef]
- Kulinkina, A.V.; Mohan, V.R.; Francis, M.R.; Kattula, D.; Sarkar, R.; Plummer, J.D.; Ward, H.; Kang, G.; Balraj, V. Seasonality of water quality and diarrheal disease counts in urban and rural settings in south India. Sci. Rep. 2016, 6, 20521. [Google Scholar] [CrossRef] [PubMed]
- Kraay, A.N.M.; Man, O.; Levy, M.C.; Levy, K.; Ionides, E.; Eisenberg, J.N.S. Understanding the Impact of Rainfall on Diarrhea: Testing the Concentration-Dilution Hypothesis Using a Systematic Review and Meta-Analysis. Environ. Health Perspect. 2020, 128, 126001. [Google Scholar] [CrossRef] [PubMed]
- Herrera, D.; Ellis, A.; Fisher, B.; Golden, C.D.; Johnson, K.; Mulligan, M.; Pfaff, A.; Treuer, T. Upstream watershed condition predicts rural children’s health across 35 developing countries. Nat. Commun. 2017, 8, 811. [Google Scholar] [CrossRef]
- Kattula, D.; Francis, M.R.; Kulinkina, A.V.; Sarkar, R.; Mohan, V.R.; Babji, S.; Ward, H.D.; Kang, G.; Balraj, V.; Naumova, E.N. Environmental predictors of diarrhoeal infection for rural and urban communities in south India in children and adults. Epidmeiol. Infect. 2015, 143, 3036–3047. [Google Scholar] [CrossRef]
- Gong, L.; Hou, S.; Su, B.; Miao, K.; Zhang, N.; Liao, W.; Zhong, S.; Wang, Z.; Yang, L.; Huang, C. Short-term effects of moderate and severe floods on infectious diarrheal diseases in Anhui Province, China. Sci. Total Environ. 2019, 675, 420–428. [Google Scholar] [CrossRef]
- Busby, J.; Smith, T.G.; Krishnan, N.; Wight, C.; Vallejo-Gutierrez, S. In harm’s way: Climate security vulnerability in Asia. World Dev. 2018, 112, 88–118. [Google Scholar] [CrossRef]
- IPCC. Climate Change 2023: Synthesis Report; IPCC: Geneva, Switzerland, 2023; pp. 35–115. Available online: https://www.ipcc.ch/report/ar6/syr/downloads/report/IPCC_AR6_SYR_LongerReport.pdf (accessed on 2 January 2025).
- United Nations. World Population Prospects 2024: Summary of Results; United Nations: New York, NY, USA, 2024; p. 80. Available online: https://population.un.org/wpp/assets/Files/WPP2024_Summary-of-Results.pdf (accessed on 2 January 2025).
- Muhammad, F.; Chowdhury, M.; Arifuzzaman, M.; Chowdhury, A.A. Public Health Problems in Bangladesh: Issues and challenges. South East Asia J. Public Health 2016, 6, 11–16. [Google Scholar] [CrossRef]
- Sultana, M.; Mahumud, R.A.; Sarker, A.R. Emerging Patterns of Mortality and Morbidity in District Level Hospitals in Bangladesh. Ann. Public Heal Res. 2015, 2, 1027. [Google Scholar]
- Harris, A.M.; Chowdhury, F.; Begum, Y.A.; Khan, A.I.; Faruque, A.S.G.; Svennerholm, A.-M.; Harris, J.B.; Ryan, E.T.; Cravioto, A.; Calderwood, S.B.; et al. Shifting Prevalence of Major Diarrheal Pathogens in Patients Seeking Hospital Care during Floods in 1998, 2004, and 2007 in Dhaka, Bangladesh. Am. J. Trop. Med. Hyg. 2008, 79, 708. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, B.S.; Harris, J.B.; Khan, A.I.; Larocque, R.C.; Sack, D.A.; Malek, M.A.; Faruque, A.S.G.; Qadri, F.; Calderwood, S.B.; Luby, S.P.; et al. Diarrheal epidemics in Dhaka, Bangladesh, during three consecutive floods: 1988, 1998, and 2004. Am. J. Trop. Med. Hyg. 2006, 74, 1067–1073. [Google Scholar] [CrossRef]
- Kanan, A.H.; Pirotti, F. A Comparative Assessment of Land Use-Land Cover Dynamics Between Bangladesh and Indian Sundarbans From 1975–2020: A Geospatial and Statistical-Based Approach. Int. Arch. Photogramm. Remote Sens. Spat. Inf. Sci. 2022, 43, 625–632. [Google Scholar] [CrossRef]
- Moniruzzam, M.; Roy, A.; Bhatt, C.M.; Gupta, A.; An, N.T.T.; Hassan, M. Impact Analysis of Urbanization on Land Use Land Cover Change for Khulna City, Bangladesh Using Temporal Landsat Imagery. Int. Arch. Photogramm. Remote Sens. Spat. Inf. Sci. 2018, 42, 757–760. [Google Scholar] [CrossRef]
- Uddin, I.M.; Endres, K.; Parvin, T.; Bhuyian, M.S.I.; Zohura, F.; Masud, J.; Monira, S.; Hasan, M.T.; Biswas, S.K.; Sultana, M.; et al. Food Hygiene and Fecal Contamination on the Household Compound are Associated with Increased Pediatric Diarrhea in Urban Bangladesh (CHoBI7 Program). Am. J. Trop. Med. Hyg. 2023, 108, 524–529. [Google Scholar] [CrossRef]
- Wu, J.; van Geen, A.; Ahmed, K.M.; Alam, Y.A.J.; Culligan, P.J.; Escamilla, V.; Feighery, J.; Ferguson, A.S.; Knappett, P.; Mailloux, B.J.; et al. Increase in diarrheal disease associated with arsenic mitigation in Bangladesh. PLoS ONE 2011, 6, e29593. [Google Scholar] [CrossRef] [PubMed]
- Goel, V.; Bell, G.J.; Sridhar, S.; Islam, M.S.; Yunus, M.; Ali, M.T.; Khan, M.A.; Alam, M.N.; Faruque, A.; Kabir, M.M.; et al. Considering Alternate Pathways of Drinking-Water Contamination: Evidence of Risk Substitution from Arsenic Mitigation Programs in Rural Bangladesh. Int. J. Environ. Res. Public Health 2020, 17, 5372. [Google Scholar] [CrossRef]
- Colombara, D.; Khalil, I.; Rao, P.; Troeger, C.; Forouzanfar, M.H.; Riddle, M.S.; Mokdad, A.H. Chronic Health Consequences of Acute Enteric Infections in the Developing World. Am. J. Gastroenterol. Suppl. 2016, 3, 4–11. [Google Scholar] [CrossRef]
- Akter, J.; Islam, M.R.; Akter, S.; Rahman, M.M.; Hossain, F.; Anam, M.R.; Alam, M.A.; Sultana, P.; Rashid, S. Equity in access to safely managed sanitation and prevalence of diarrheal diseases in Bangladesh: A national and sub-national analysis. BMC Infect. Dis. 2022, 22, 871. [Google Scholar] [CrossRef]
- Kamal, M.; Tewabe, T.; Tsheten, T. Individual and community-level factors associated with under-five diarrhea in Bangladesh: Evidence from Demographic and Health Survey 2014. Curr. Ther. Res. Clin. Exp. 2022, 97, 100686. [Google Scholar] [CrossRef]
- Mall, R.K.; Srivastava, R.K.; Banerjee, T.; Mishra, O.P.; Bhatt, D.; Sonkar, G. Disaster Risk Reduction Including Climate Change Adaptation Over South Asia: Challenges and Ways Forward. Int. J. Disaster Risk Sci. 2019, 10, 14–27. [Google Scholar] [CrossRef]
- DHS. The DHS Program—Bangladesh: Standard DHS, 2022 Dataset. Available online: https://dhsprogram.com/data/dataset/Bangladesh_Standard-DHS_2022.cfm?flag=0 (accessed on 2 January 2025).
- Alamgir, M.; Shahid, S.; Hazarika, M.K.; Nashrrullah, S.; Harun, S.B.; Shamsudin, S. Analysis of Meteorological Drought Pattern During Different Climatic and Cropping Seasons in Bangladesh. JAWRA J. Am. Water Resour. Assoc. 2015, 51, 794–806. [Google Scholar] [CrossRef]
- Perez-Haydrich, C.; Warren, J.L.; Burgert, C.R.; Emch, M.E. Guidelines on the Use of DHS GPS Data. Available online: https://dhsprogram.com/publications/publication-SAR8-Spatial-Analysis-Reports.cfm (accessed on 2 January 2025).
- Burgert, C.R.; Colston, J.; Roy, T.; Zachary, B. Geographic Displacement Procedure and Georeferenced Data Release Policy for the Demographic and Health Surveys. Available online: https://dhsprogram.com/publications/publication-SAR7-Spatial-Analysis-Reports.cfm (accessed on 2 January 2025).
- Hansen, M.C.; Potapov, P.V.; Moore, R.; Hancher, M.; Turubanova, S.A.; Tyukavina, A.; Thau, D.; Stehman, S.V.; Goetz, S.J.; Loveland, T.R.; et al. High-Resolution Global Maps of 21st-Century Forest Cover Change. Science 2013, 342, 850–853. [Google Scholar] [CrossRef]
- Funk, C.; Peterson, P.; Landsfeld, M.; Pedreros, D.; Verdin, J.; Shukla, S.; Husak, G.; Rowland, J.; Harrison, L.; Hoell, A.; et al. The climate hazards infrared precipitation with stations—A new environmental record for monitoring extremes. Sci. Data 2015, 2, 150066. [Google Scholar] [CrossRef]
- Bauch, S.C.; Birkenbach, A.M.; Pattanayak, S.K.; Sills, E.O. Public health impacts of ecosystem change in the Brazilian Amazon. Proc. Natl. Acad. Sci. USA 2015, 112, 7414–7419. [Google Scholar] [CrossRef] [PubMed]
- Stekhoven, D.J.; Bühlmann, P. MissForest—Non-parametric missing value imputation for mixed-type data. Bioinformatics 2012, 28, 112–118. [Google Scholar] [CrossRef]
- Louhichi, M.; Nesmaoui, R.; Mbarek, M.; Lazaar, M. Shapley Values for Explaining the Black Box Nature of Machine Learning Model Clustering. Procedia Comput. Sci. 2023, 220, 806–811. [Google Scholar] [CrossRef]
- Rodríguez-Pérez, R.; Bajorath, J. Interpretation of machine learning models using shapley values: Application to compound potency and multi-target activity predictions. J. Comput. Aided Mol. Des. 2020, 34, 1013–1026. [Google Scholar] [CrossRef]
- Gleason, K.M.; Valeri, L.; Shankar, A.H.; Hasan, M.O.S.I.; Quamruzzaman, Q.; Rodrigues, E.G.; Christiani, D.C.; Wright, R.O.; Bellinger, D.C.; Mazumdar, M. Stunting is associated with blood lead concentration among Bangladeshi children aged 2–3 years. Environ. Health 2016, 15, 103. [Google Scholar] [CrossRef] [PubMed]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006; p. 312. [Google Scholar]



| Feature | Description | Type | Scale | Mean (S.D.) a | Aggregation Method b |
|---|---|---|---|---|---|
| Socio-Demographic Features | |||||
| Age of Child | Age of child in months. | Continuous | HH | 29.9 (17.2) | Average |
| Stunting | Height/age standard deviations according to the WHO. | Continuous | HH | −75.5 (213.3) | Average |
| Age of Head | Age of the head of household in years. | Continuous | HH | 41.7 (14.1) | Average |
| Pop. Density | Average population density in 5 km radius. | Continuous | Village | 2814 (6320) | n/a |
| Education | Respondent has higher or secondary education. | Binary | HH | 42% | Prevalence |
| Gender | Gender of child (male). | Binary | HH | 49% | Prevalence |
| Improved Sanitation | Improved sanitation based on WHO definitions. | Binary | HH | 53% | Mode |
| Breastfeed | Respondent is currently breastfeeding. | Binary | HH | 68% | Prevalence |
| Wealth | Respondent is in upper two quintiles of wealth. | Binary | HH | 39% | Prevalence |
| Birth Order | Birth order of child experiencing diarrheal disease. | Categorical (1–5) | HH | 1.2 (0.45) | Mode |
| Sex of Head | Sex of the head of household (male). | Binary | HH | 8% | Prevalence |
| Climate and Geographic Features | |||||
| Precip. Previous | Total precipitation (mm) in month prior to survey. | Continuous | Village | 265.9 (254.9) | |
| Precip. Current | Total precipitation (mm) of month of survey. | Continuous | Village | 286.1 (271.5) | n/a |
| Temp. Previous | Average temperature (°C) of month prior to survey. | Continuous | Village | 30.98 (2.8) | n/a |
| Temp. Current | Average temperature (°C) of month of survey. | Continuous | Village | 30.96 (2.7) | n/a |
| Climate Season | Climate season at time of survey. (1 = dry winter; 2 = pre-monsoon; 3 = monsoon; 4 = post-monsoon). | Categorical (1–4) | Village | 2.4 (0.96) | n/a |
| Dist. Ocean or Lake | Distance (m) to ocean or lake. | Continuous | Village | 248,781 (171,040) | n/a |
| Elevation | Average elevation (m) of the village. | Continuous | Village | 14.22 (11.4) | n/a |
| Slope | Average slope within 5 km radius of village. | Continuous | Village | 0.12 (0.18) | n/a |
| Dist. Road | Distance (m) to nearest road. | Continuous | Village | 2214 (2341) | n/a |
| Forest Loss Hotspot | Village located in a forest loss hotspot. | Binary | Village | 2% | n/a |
| Health Outcome Features | |||||
| DD HH | Child in household has experience diarrheal disease in the past two weeks. | Binary | HH | 7% | Prevalence |
| DD Village | Diarrheal disease experienced in ≥3% village HHs. | Binary | Village | 80% | |
| Dataset | Sample Size |
|---|---|
| Household-Level | 21,779 households |
| Village-Level | 600 villages |
| “Low” DD group | 4257 households in 179 villages |
| “High” DD group | 17,522 households in 421 villages |
| Metric | A | B |
|---|---|---|
| Recall (true positive rate) | 82.9% | 99.9% |
| False positive rate | 2.2% | 10.7% |
| Precision | 74.0% | 97.5% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Heijden, R.; Doran, E.M.B.; King, P.; Brown, K.P.; Rizzo, D.M.; Gleason, K.M. Using Spatial Technologies to Assess Risk Factors for Diarrheal Disease Under Environmental Variability in Bangladesh: A Machine Learning Study. Int. J. Environ. Res. Public Health 2025, 22, 1758. https://doi.org/10.3390/ijerph22111758
van der Heijden R, Doran EMB, King P, Brown KP, Rizzo DM, Gleason KM. Using Spatial Technologies to Assess Risk Factors for Diarrheal Disease Under Environmental Variability in Bangladesh: A Machine Learning Study. International Journal of Environmental Research and Public Health. 2025; 22(11):1758. https://doi.org/10.3390/ijerph22111758
Chicago/Turabian Stylevan der Heijden, Ryan, Elizabeth M. B. Doran, Parker King, Kennedy P. Brown, Donna M. Rizzo, and Kelsey M. Gleason. 2025. "Using Spatial Technologies to Assess Risk Factors for Diarrheal Disease Under Environmental Variability in Bangladesh: A Machine Learning Study" International Journal of Environmental Research and Public Health 22, no. 11: 1758. https://doi.org/10.3390/ijerph22111758
APA Stylevan der Heijden, R., Doran, E. M. B., King, P., Brown, K. P., Rizzo, D. M., & Gleason, K. M. (2025). Using Spatial Technologies to Assess Risk Factors for Diarrheal Disease Under Environmental Variability in Bangladesh: A Machine Learning Study. International Journal of Environmental Research and Public Health, 22(11), 1758. https://doi.org/10.3390/ijerph22111758






