Pediatric Health, Climate Perceptions, and School Absenteeism Across Three Regions of Bangladesh: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Questionnaires
2.3. Physical Examination
2.4. Blood Lead and Hemoglobin Concentration
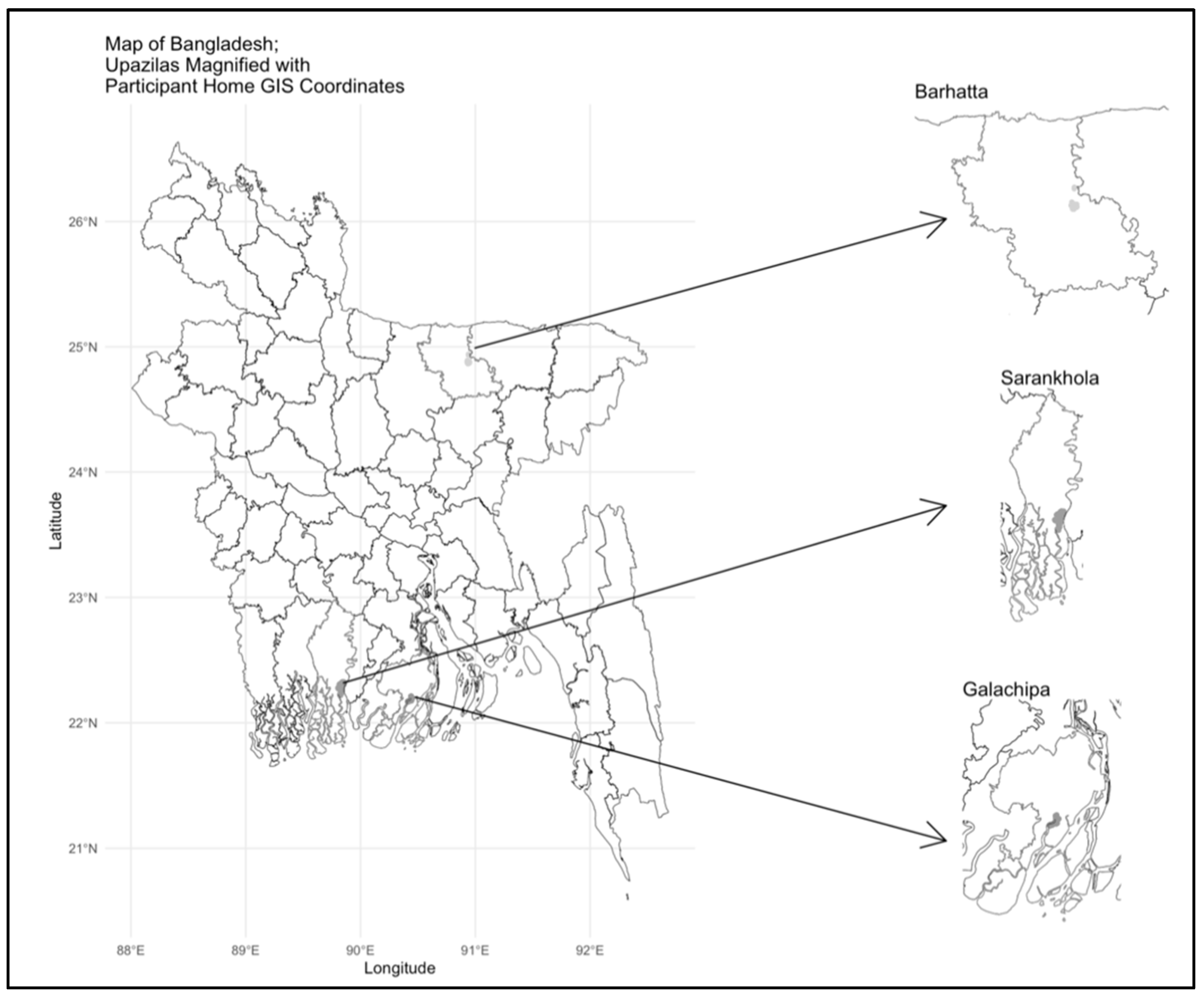
2.5. Water Salinity and GIS Coordinates
2.6. Statistical Analysis
3. Results
3.1. General Characteristics of the Study Population
3.2. Climate and Health-Related Perceptions
3.3. Household Water Salinity
3.4. School Absenteeism
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DCH | Dhaka Community Hospital |
| EEG | Electroencephalography |
| GIS | Geographic Information System |
| SD | Standard Deviation |
| PEFR | Peak Expiratory Flow Rate |
| WHO | World Health Organization |
References
- Zhao, Q.; Yu, P.; Mahendran, R.; Huang, W.; Gao, Y.; Yang, Z.; Ye, T.; Wen, B.; Wu, Y.; Li, S.; et al. Global climate change and human health: Pathways and possible solutions. Eco-Environ. Health 2022, 1, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Shivanna, K.R. Climate change and its impact on biodiversity and human welfare. Proc. Indian Natl. Sci. Acad. 2022, 88, 160–171. [Google Scholar] [CrossRef]
- Sheffield, P.E.; Landrigan, P.J. Global climate change and children’s health: Threats and strategies for prevention. Environ. Health Perspect. 2011, 119, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Hellden, D.; Andersson, C.; Nilsson, M.; Ebi, K.L.; Friberg, P.; Alfven, T. Climate change and child health: A scoping review and an expanded conceptual framework. Lancet Planet. Health 2021, 5, e164–e175. [Google Scholar] [CrossRef]
- Aithal, S.S.; Sachdeva, I.; Kurmi, O.P. Air quality and respiratory health in children. Breathe 2023, 19, 230040. [Google Scholar] [CrossRef] [PubMed]
- Grant, L.; Vanderkelen, I.; Gudmundsson, L.; Fischer, E.; Seneviratne, S.I.; Thiery, W. Global emergence of unprecedented lifetime exposure to climate extremes. Nature 2025, 641, 374–379. [Google Scholar] [CrossRef]
- Proulx, K.; Daelmans, B.; Baltag, V.; Banati, P. Climate change impacts on child and adolescent health and well-being: A narrative review. J. Glob. Health 2024, 14, 04061. [Google Scholar] [CrossRef]
- Mielke, H.W.; Gonzales, C.R.; Powell, E.T.; Laidlaw, M.A.S. Lead in Air, Soil, and Blood: Pb Poisoning in a Changing World. Int. J. Environ. Res. Public Health 2022, 19, 9500. [Google Scholar] [CrossRef]
- Wolfe, M.K.; McDonald, N.C.; Arunachalam, S.; Baldauf, R.; Valencia, A. Impact of School Location on Children’s Air Pollution Exposure. J. Urban Aff. 2020, 43, 1118–1134. [Google Scholar] [CrossRef]
- Roche, I.V.; Ubalde-Lopez, M.; Daher, C.; Nieuwenhuijsen, M.; Gascon, M. The Health-Related and Learning Performance Effects of Air Pollution and Other Urban-Related Environmental Factors on School-Age Children and Adolescents-A Scoping Review of Systematic Reviews. Curr. Environ. Health Rep. 2024, 11, 300–316. [Google Scholar] [CrossRef]
- Ebi, K.L. Managing climate change risks is imperative for human health. Nat. Rev. Nephrol. 2022, 18, 74–75. [Google Scholar] [CrossRef]
- Anderko, L.; Chalupka, S.; Du, M.; Hauptman, M. Climate Change’s Reproductive and Children’s Health: A Review of Risks, Exposures, and Impacts. Pediatr. Res. 2020, 87, 414–419. [Google Scholar] [CrossRef]
- Kearney, C.A.; Ellis, K.; Arcaina, V.J. Climate Change Injustice and School Attendance and Absenteeism: Proximal and Distal Ecological Links. Front. Educ. 2024, 9, 1455430. [Google Scholar] [CrossRef]
- Hrabok, M.; Delorme, A.; Agyapong, V.I.O. Threats to Mental Health and Well-Being Associated with Climate Change. J. Anxiety Disord. 2020, 76, 102295. [Google Scholar] [CrossRef]
- Lawrence, D.; Dawson, V.; Houghton, S.; Goodsell, B.; Sawyer, M.G. Impact of Mental Disorders on Attendance at School. Aust. J. Educ. 2019, 63, 5–21. [Google Scholar] [CrossRef]
- Das, P. Child Labour, Seasonal Migration and School Exclusion: A Sad Story of Tribal Girls in Rural India. J. Rural. Dev. 2021, 39, 504–518. [Google Scholar] [CrossRef]
- Fernandez, S.; Arce, G.; Garcia-Alaminos, A.; Cazcarro, I.; Arto, I. Climate change as a veiled driver of migration in Bangladesh and Ghana. Sci. Total Environ. 2024, 922, 171210. [Google Scholar] [CrossRef] [PubMed]
- Jihan, M.A.T.; Popy, S.; Kayes, S.; Rasul, G.; Maowa, A.S.; Rahman, M.M. Climate change scenario in Bangladesh: Historical data analysis and future projection based on CMIP6 model. Sci. Rep. 2025, 15, 7856. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.A. Social and legal barriers to improving human rights of climate change displaced people in Bangladesh. J. Interrupted Stud. 2019, 2, 103–117. [Google Scholar] [CrossRef]
- Chowdhury, M.R.K.; Khan, H.T.A.; Rashid, M.; Kabir, R.; Islam, S.; Shariful Islam, M.; Kader, M. Differences in risk factors associated with single and multiple concurrent forms of undernutrition (stunting, wasting or underweight) among children under 5 in Bangladesh: A nationally representative cross-sectional study. BMJ Open 2021, 11, e052814. [Google Scholar] [CrossRef] [PubMed]
- Jibon, M.J.N.; Ruku, S.; Islam, A.; Khan, M.N.; Mallick, J.; Bari, A.; Senapathi, V. Impact of climate change on vector-borne diseases: Exploring hotspots, recent trends and future outlooks in Bangladesh. Acta Trop. 2024, 259, 107373. [Google Scholar] [CrossRef]
- Kumar, S.; Islam, R.; Akash, P.B.; Rahman, M.; Rahman, M.M.; Hossain, M.M. Lead (Pb) Contamination in Agricultural Products and Human Health Risk Assessment in Bangladesh. Water Air Soil Pollut. 2022, 233, 257. [Google Scholar] [CrossRef]
- Voss, M.; Nyström, C.; Nilsson, M.; Rigó, A.; Lundqvist, A. The Missing Middle of Childhood. Glob. Health Action 2023, 16, 2242196. [Google Scholar] [CrossRef]
- Kabir, M.I.; Rahman, M.B.; Smith, W.; Lusha, M.A.; Azim, S.; Milton, A.H. Knowledge and perception about climate change and human health: Findings from a baseline survey among vulnerable communities in Bangladesh. BMC Public Health 2016, 16, 266. [Google Scholar] [CrossRef]
- Patel, A.A.; Ciccone, O.; Njau, A.; Shanungu, S.; Grollnek, A.K.; Fredrick, F.; Hodgeman, R.; Sideridis, G.D.; Kapur, K.; Harini, C.; et al. A pediatric epilepsy diagnostic tool for use in resource-limited settings: A pilot study. Epilepsy Behav. 2016, 59, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Tairou, F.; Nawaz, S.; Tahita, M.C.; Herrera, S.; Faye, B.; Tine, R.C.K. Malaria prevention knowledge, attitudes, and practices (KAP) among adolescents living in an area of persistent transmission in Senegal: Results from a cross-sectional study. PLoS ONE 2022, 17, e0274656. [Google Scholar] [CrossRef] [PubMed]
- Asher, M.I.; Keil, U.; Anderson, H.R.; Beasley, R.; Crane, J.; Martinez, F.; Mitchell, E.A.; Pearce, N.; Sibbald, B.; Stewart, A.W.; et al. International Study of Asthma and Allergies in Childhood (ISAAC): Rationale and methods. Eur. Respir. J. 1995, 8, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.M.; Khan, S.J.; Tanni, K.N.; Roy, T.; Chisty, M.A.; Islam, M.R.; Rumi, M.; Sakib, M.S.; Quader, M.A.; Bhuiyan, M.N.; et al. Knowledge, Attitude, and Practices towards Dengue Fever among University Students of Dhaka City, Bangladesh. Int. J. Environ. Res. Public Health 2022, 19, 4023. [Google Scholar] [CrossRef]
- Rahman, M.A.; Renzaho, A.M.N.; Kundu, S.; Awal, M.A.; Ashikuzzaman, M.; Fan, L.; Ahinkorah, B.O.; Okyere, J.; Kamara, J.K.; Mahumud, R.A. Prevalence and factors associated with chronic school absenteeism among 207,107 in-school adolescents: Findings from cross-sectional studies in 71 low-middle and high-income countries. PLoS ONE 2023, 18, e0283046. [Google Scholar] [CrossRef]
- UNICEF Regional Office for South Asia. Rising to the Challenge: Youth Perspectives on Climate Change and Education in Bangladesh; UNICEF: Kathmandu, Nepal, 2021. [Google Scholar]
- Neri, A.J.; Roy, J.; Jarrett, J.; Pan, Y.; Dooyema, C.; Caldwell, K.; Umar-Tsafe, N.T.; Olubiyo, R.; Brown, M.J. Analysis of a novel field dilution method for testing samples that exceed the analytic range of point-of-care blood lead analyzers. Int. J. Environ. Health Res. 2014, 24, 418–428. [Google Scholar] [CrossRef][Green Version]
- Scheelbeek, P.F.D.; Chowdhury, M.A.H.; Haines, A.; Alam, D.S.; Hoque, M.A.; Butler, A.P.; Khan, A.E.; Mojumder, S.K.; Blangiardo, M.; Elliott, P.; et al. Drinking Water Salinity and Raised Blood Pressure: Evidence from a Cohort Study in Coastal Bangladesh. Environ. Health Perspect. 2017, 125, 057007. [Google Scholar] [CrossRef]
- Ahmed, K.J.; Haq, S.M.A.; Bartiaux, F. The nexus between extreme weather events, sexual violence, and early marriage: A study of vulnerable populations in Bangladesh. Popul. Environ. 2019, 40, 303–324. [Google Scholar] [CrossRef]
- Sarker, I.; Karim, M.R.; S, E.B.; Hasan, M. Dengue fever mapping in Bangladesh: A spatial modeling approach. Health Sci. Rep. 2024, 7, e2154. [Google Scholar] [CrossRef]
- Abdullah, A.S.M.; Dalal, K.; Yasmin, M.; Ussatayeva, G.; Halim, A.; Biswas, A. Perceptions and practices on newborn care and managing complications at rural communities in Bangladesh: A qualitative study. BMC Pediatr. 2021, 21, 168. [Google Scholar] [CrossRef] [PubMed]
- Wang, M. Iron Deficiency and Other Types of Anemia in Infants and Children. Am. Fam. Physician 2016, 93, 270–278. [Google Scholar]
- Aksu, T.; Unal, S. Iron Deficiency Anemia in Infancy, Childhood, and Adolescence. Turk. Arch. Pediatr. 2023, 58, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Bi, P.; Hiller, J.E. Climate change and disability-adjusted life years. J. Environ. Health 2007, 70, 32–36. [Google Scholar]
- Weeda, L.J.Z.; Bradshaw, C.J.A.; Judge, M.A.; Saraswati, C.M.; Le Souef, P.N. How climate change degrades child health: A systematic review and meta-analysis. Sci. Total Environ. 2024, 920, 170944. [Google Scholar] [CrossRef] [PubMed]
- Hoque, D.M.; Rahman, M.; Billah, S.M.; Savic, M.; Karim, A.Q.; Chowdhury, E.K.; Hossain, A.; Musa, S.A.; Kumar, H.; Malhotra, S.; et al. An assessment of the quality of care for children in eighteen randomly selected district and sub-district hospitals in Bangladesh. BMC Pediatr. 2012, 12, 197. [Google Scholar] [CrossRef]
- Islam, S.; Khan, M.A.S.; Badal, M.F.A.; Khan, M.Z.I.; Gozal, D.; Hasan, M.J. Clinical and hematological profiles of children with dengue residing in a non-endemic zone of Bangladesh. PLoS Neglected Trop. Dis. 2022, 16, e0010847. [Google Scholar] [CrossRef]
- Guo, Y.; Gasparrini, A.; Armstrong, B.; Li, S.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; de Sousa Zanotti Stagliorio Coelho, M.; Leone, M.; Pan, X.; et al. Global variation in the effects of ambient temperature on mortality: A systematic evaluation. Epidemiology 2014, 25, 781–789. [Google Scholar] [CrossRef]
- Rocque, R.J.; Beaudoin, C.; Ndjaboue, R.; Cameron, L.; Poirier-Bergeron, L.; Poulin-Rheault, R.A.; Fallon, C.; Tricco, A.C.; Witteman, H.O. Health effects of climate change: An overview of systematic reviews. BMJ Open 2021, 11, e046333. [Google Scholar] [CrossRef]
- Kabir, M.I.; Rahman, M.B.; Smith, W.; Lusha, M.A.; Milton, A.H. Climate change and health in Bangladesh: A baseline cross-sectional survey. Glob. Health Action 2016, 9, 29609. [Google Scholar] [CrossRef] [PubMed]
- Hossain, B.; Shi, G.; Ajiang, C.; Sarker, M.N.I.; Sohel, M.S.; Sun, Z.; Yang, Q. Climate change induced human displacement in Bangladesh: Implications on the livelihood of displaced riverine island dwellers and their adaptation strategies. Front. Psychol. 2022, 13, 964648. [Google Scholar] [CrossRef] [PubMed]
- Rerolle, F.; Arnold, B.F.; Benmarhnia, T. Excess risk in infant mortality among populations living in flood-prone areas in Bangladesh: A cluster-matched cohort study over three decades, 1988 to 2017. Proc. Natl. Acad. Sci. USA 2023, 120, e2218789120. [Google Scholar] [CrossRef] [PubMed]
- Haque, F.; Lampe, F.C.; Hajat, S.; Stavrianaki, K.; Hasan, S.M.T.; Faruque, A.S.G.; Ahmed, T.; Jubayer, S.; Kelman, I. Impacts of climate change on diarrhoeal disease hospitalisations: How does the global warming targets of 1.5–2 degrees C affect Dhaka, Bangladesh? PLoS Neglected Trop. Dis. 2024, 18, e0012139. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, Q.D.; Saha, N.C.; Alam, M.B.; Hoque, S.A.; Islam, A.; Chowdhury, R.N.; Hussain, M.E.; Chowdhury, Y.S.; Hossain, S.; Chowdhury, M.A.; et al. Prevalence of epilepsy in Bangladesh: Results from a national household survey. Epilepsia Open 2020, 5, 526–536. [Google Scholar] [CrossRef]
- Karim, T.; Das, M.C.; Muhit, M.; Badawi, N.; Khandaker, G.; Mohammad, S.S. Improving epilepsy control among children with cerebral palsy in rural Bangladesh: A prospective cohort-based study. BMJ Open 2022, 12, e052578. [Google Scholar] [CrossRef]
| Children in Three Study Sites (n = 300) | |||
|---|---|---|---|
| Characteristics | Barhatta (n = 100) | Galachipa (n = 100) | Sarankhola (n = 100) |
| Age (years) | 8.7 ± 1.9 | 8.8 ± 2.1 | 9.1 ± 1.8 |
| Sex | |||
| Male | 44 | 43 | 48 |
| Female | 56 | 57 | 52 |
| BMI (kg/m2) | 14.0 ± 2.8 | 15.1 ± 2.2 | 14.4 ± 1.7 |
| Mid-Upper Arm Circumference (cm) | 18.2 ± 2.6 | 18.5 ± 2.5 | 18.1 ± 2.2 |
| Education Level | |||
| No Institutional Education | 4 | 0 | 2 |
| Primary Level (Class 1–5) | 90 | 88 | 89 |
| Secondary Level (Class 6–10) | 4 | 7 | 9 |
| Other/Not Applicable | 2 | 5 | 0 |
| Education Status by Age | |||
| Any Schooling | |||
| Ages 6–8 | 45 (93.8%) | 42 (89.4%) | 33 (97.1%) |
| Ages 9–10 | 30 (93.8%) | 26 (100%) | 43 (100%) |
| Ages 11–12 | 19 (95.0%) | 27 (100%) | 22 (95.7%) |
| Head of Household Sex | |||
| Male | 94 | 93 | 94 |
| Head of Household Occupation | |||
| Farmer | 39 | 16 | 8 |
| Day Labor | 29 | 34 | 61 |
| Service Holder | 15 | 16 | 14 |
| Small Businessman | 13 | 32 | 14 |
| Housewife | 2 | 2 | 2 |
| Unemployed | 2 | 0 | 1 |
| Head of Household Occupation by Sex | |||
| Male | |||
| Farmer | |||
| Day Labor | 38 (40.4%) | 16 (17.2%) | 8 (8.5%) |
| Service Holder | 27 (28.7%) | 32 (34.4%) | 59 (62.8%) |
| Small Businessman | 14 (14.9%) | 14 (15.1%) | 13 (13.8%) |
| Unemployed | 13 (13.8%) | 31 (33.3%) | 13 (13.8%) |
| Female | 2 (2.1%) | 0 (0%) | 1 (1.1%) |
| Farmer | |||
| Day Labor | 1 (16.7%) | 0 (0%) | 0 (0%) |
| Service Holder | 2 (33.3%) | 2 (28.6%) | 2 (33.3%) |
| Small Businesswoman | 1 (16.7%) | 2 (28.6%) | 1 (16.7%) |
| Housewife | 0 (0%) | 1 (14.3%) | 1 (16.7%) |
| Unemployed | 2 (33.3%) | 2 (28.6%) | 2 (33.3%) |
| 0 (0%) | 0 (0%) | 0 (0%) | |
| Household Monthly Income (Thousands BDT), median (IQR) | 20.0 (15.0, 20.0) | 14.5 (10.0, 18.0) | 10.0 (9.0, 15.0) |
| Reported Health Conditions in Child | |||
| Asthma | 6 | 1 | 21 |
| Dengue | 1 | 2 | 2 |
| Epilepsy | 2 | 1 | 17 |
| Rash | 6 | 2 | 48 |
| Children in Three Study Sites (n = 300) | |||
|---|---|---|---|
| Variable | Barhatta (n = 100) | Galachipa (n = 100) | Sarankhola (n = 100) |
| Height (cm) | 127.2 ± 13.3 | 125.5 ± 14.2 | 126.5 ± 10.8 |
| Weight (kg) | 23.1 ± 7.7 | 24.3 ± 7.4 | 23.5 ± 5.9 |
| PEFR Min-Max, L/min | 130–330 | 80–380 | 50–390 |
| PEFR Mean (SD), L/min | 219.5 ± 45.3 | 196.4 ± 49.9 | 234.2 ± 51.9 |
| Blood Lead, Median (Min-Max) (µg/dL) | 4.60 (<LOD − 36.4) | 1.65 (<LOD − 9.3) | 1.65 (<LOD − 12.7) |
| Hemoglobin Concentration (g %) | 12.8 ± 1.0 | 13.1 ± 1.6 | 11.0 ± 1.5 |
| Children in Three Study Sites (n = 300) | |||
|---|---|---|---|
| Exposure Question | Barhatta (n = 100) | Galachipa (n = 100) | Sarankhola (n = 100) |
| Main Source of Drinking Water | |||
| Shallow | 98 | 0 | 0 |
| Deep Tubewell | 2 | 99 | 22 |
| Supplied Water Through Pipe | 0 | 1 | 5 |
| Crude Pond Water | 0 | 0 | 13 |
| Refined Pond Water | 0 | 0 | 15 |
| Rainwater | 0 | 0 | 38 |
| Other | 0 | 0 | 7 |
| Closest Place of Healthcare Services | |||
| Government Hospital | 0 | 90 | 93 |
| Community Clinic | 3 | 9 | 6 |
| NGO Healthcare Clinic | 97 | 0 | 0 |
| Village Doctor | 0 | 1 | 0 |
| Pharmacy | 0 | 0 | 1 |
| Have Access to Government Healthcare Facility | |||
| District Hospital | 0 | 0 | 1 |
| Upazila Health Complex | 94 | 100 | 77 |
| Union Health Center | 1 | 0 | 17 |
| Community Clinic | 5 | 74 | 4 |
| Have Health Education Program in School | 10 | 98 | 93 |
| Have Access to Community Clinic | 6 | 77 | 8 |
| Faced Any Natural Calamity | |||
| Flood | 86 | 100 | 40 |
| Drought | 11 | 77 | 16 |
| Cyclone | 1 | 100 | 100 |
| Tidal Wave | 0 | 2 | 29 |
| River Erosion | 0 | 4 | 7 |
| Ever Became Homeless due to Natural Calamity in Last 10 Years | 4 | 41 | 78 |
| Heard of Climate Change | 32 | 100 | 100 |
| Source of Hearing Climate Change | |||
| Newspaper | 3 | 14 | 2 |
| Radio | 0 | 1 | 5 |
| Television | 15 | 82 | 83 |
| Neighbor | 6 | 56 | 44 |
| Health worker | 9 | 86 | 30 |
| School teacher | 0 | 59 | 18 |
| Perceived Type of Climate Change | |||
| Excessive temperature | 31 | 100 | 93 |
| Excessive cold | 0 | 73 | 3 |
| Change in pattern of precipitation | 1 | 93 | 18 |
| Cyclone/Tidal wave | 0 | 27 | 94 |
| Frequent flood | 1 | 82 | 3 |
| Water logging | 0 | 2 | 4 |
| Perceived Reasons for Climate Change | |||
| Deforestation | 28 | 100 | 97 |
| Industrial effluent | 1 | 37 | 21 |
| Population growth | 3 | 78 | 34 |
| Black smoke of vehicles | 1 | 13 | 46 |
| Excessive carbon emissions to the atmosphere | 0 | 8 | 4 |
| Quick urbanization and change in livelihood | 0 | 0 | 3 |
| Children in Three Study Sites (n = 300) | |||
|---|---|---|---|
| Water Use | Barhatta (n = 100) | Galachipa (n = 100) | Sarankhola (n = 100) |
| Drinking Water Salinity (ppt) | |||
| 25th Percentile | 0.10 | 0.30 | 0.05 |
| Median | 0.20 | 0.30 | 0.05 |
| 75th Percentile | 0.50 | 0.30 | 0.06 |
| Cooking Water Salinity (ppt) | |||
| 25th Percentile | 0.10 | 0.30 | 0.05 |
| Median | 0.20 | 0.30 | 0.05 |
| 75th Percentile | 0.43 | 0.30 | 0.10 |
| Perceived Increase in Local Water Salinity (Past 10 Years) | 0 | 89 | 89 |
| Use Same Water Source for Drinking and Bathing/Cooking | 96 | 98 | 46 |
| Children in Three Study Sites (n = 300) | |||
|---|---|---|---|
| Survey Questions | Barhatta (n = 100) | Galachipa (n = 100) | Sarankhola (n = 100) |
| Days Missed School/Classes | |||
| 0 day | 34 | 29 | 31 |
| 1–2 day | 22 | 47 | 33 |
| 3–5 day | 5 | 18 | 26 |
| 6–9 day | 1 | 0 | 5 |
| 10 or more days | 37 | 2 | 3 |
| Reasons for Missed School | |||
| Personal illness | 13 | 36 | 48 |
| Family illness | 1 | 16 | 3 |
| Take care of another person | 1 | 0 | 2 |
| Work responsibilities | 6 | 1 | 0 |
| Menstrual cycle | 0 | 0 | 0 |
| Transportation problems | 0 | 1 | 14 |
| Weather/Climate emergency | 1 | 12 | 25 |
| Unexpected school closure | 39 | 0 | 5 |
| Had to move | 6 | 5 | 4 |
| Climate Change Affect Education | |||
| Unaffected | 58 | 20 | 23 |
| Made school unsafe | 32 | 4 | 17 |
| Impacted journey to school | 6 | 71 | 61 |
| Impacted teacher | 1 | 4 | 1 |
| Impacted school facilities | 0 | 8 | 2 |
| Impacted attendance | 1 | 4 | 4 |
| Family’s ability to afford schooling | 1 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, Y.S.; Afroz, S.; Mow, S.S.; Wang, X.; Sarpy, C.; Islam, M.F.; Husain, M.N.; Hossain, M.S.; Sania, A.R.; Mostofa, M.G.; et al. Pediatric Health, Climate Perceptions, and School Absenteeism Across Three Regions of Bangladesh: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2025, 22, 1639. https://doi.org/10.3390/ijerph22111639
Jung YS, Afroz S, Mow SS, Wang X, Sarpy C, Islam MF, Husain MN, Hossain MS, Sania AR, Mostofa MG, et al. Pediatric Health, Climate Perceptions, and School Absenteeism Across Three Regions of Bangladesh: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2025; 22(11):1639. https://doi.org/10.3390/ijerph22111639
Chicago/Turabian StyleJung, Yoon Sik, Sakila Afroz, Sadia Samad Mow, Xingyan Wang, Caroline Sarpy, Md Fuadul Islam, Md Nazmul Husain, Md Shahadat Hossain, Al Romana Sania, Md Golam Mostofa, and et al. 2025. "Pediatric Health, Climate Perceptions, and School Absenteeism Across Three Regions of Bangladesh: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 22, no. 11: 1639. https://doi.org/10.3390/ijerph22111639
APA StyleJung, Y. S., Afroz, S., Mow, S. S., Wang, X., Sarpy, C., Islam, M. F., Husain, M. N., Hossain, M. S., Sania, A. R., Mostofa, M. G., Quamruzzaman, Q., & Mazumdar, M. (2025). Pediatric Health, Climate Perceptions, and School Absenteeism Across Three Regions of Bangladesh: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 22(11), 1639. https://doi.org/10.3390/ijerph22111639






