Exploring Family Typologies and Health Outcomes in a Dutch Primary Care Population of Children Living in Urban Cities in the Netherlands: A Latent Class Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Child and Family Demographics
2.3. Social and Physical Environmental Factors
- (1)
- Physical environment includes data such as the distance to roads and green areas, air quality, and noise pollution.
- (2)
- Housing stock includes data such as residential area, housing vacancy, and overcrowding.
- (3)
- Facilities stock includes proximity data, such as the distance to healthcare, education, and hospitality service providers.
- (4)
- Social cohesion includes aspects such as population density and diversity of life stages.
- (5)
- Nuisance and insecurity, which include violent crimes, vandalism, public disturbances, and experienced nuisance and insecurity [30].
2.4. Health Outcomes
2.5. Statistical Analysis
2.6. Latent Class Analysis
2.7. Logistic Regression Analyses
3. Results
3.1. LCA Class Interpretation
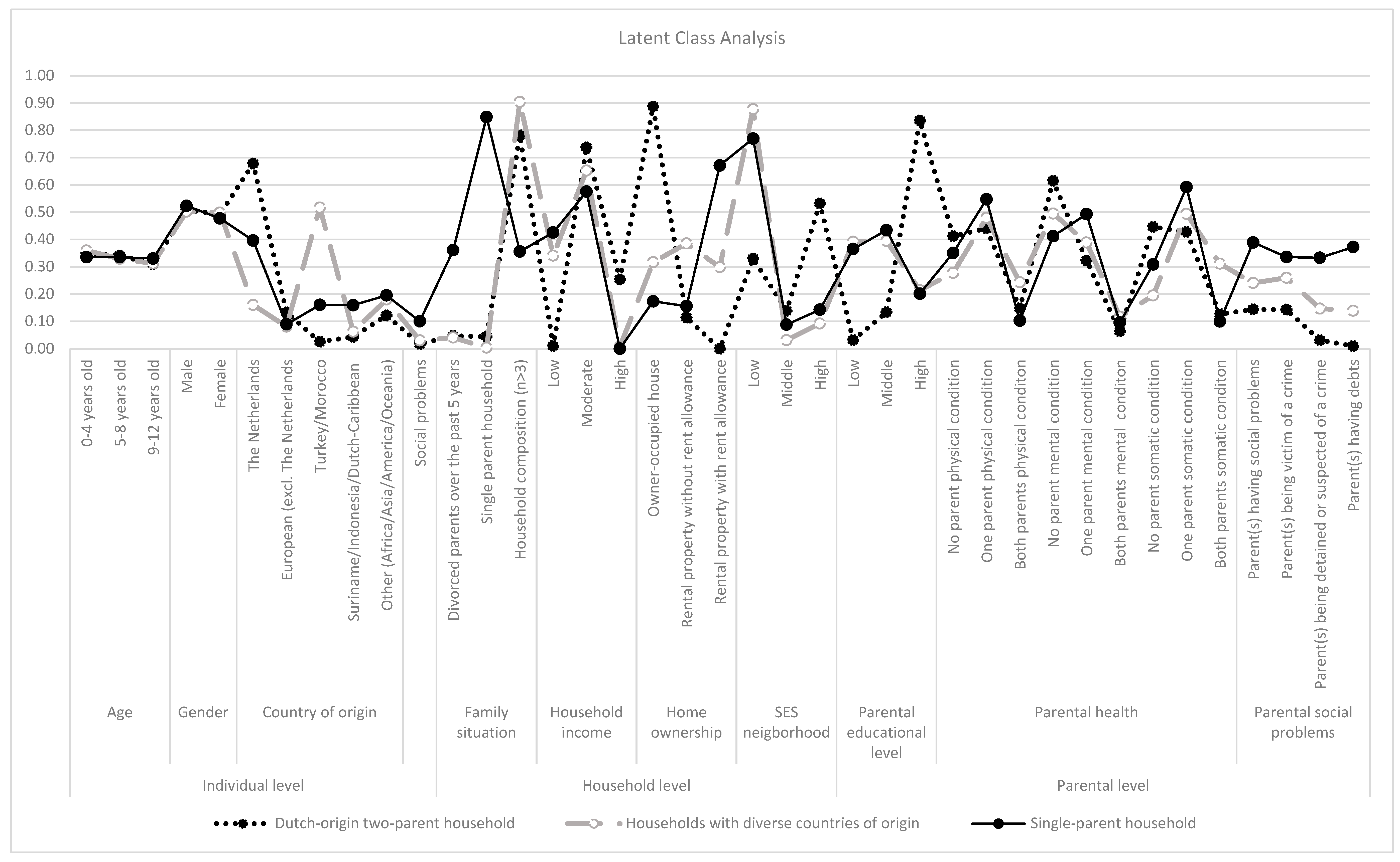
3.1.1. Class 1: ‘Dutch-Origin Two-Parent Household’ (n = 7267 [50% of Total Study Population])
3.1.2. Class 2: ‘Households with Diverse Countries of Origin’ (n = 4313 [29.7% of Total Study Population])
3.1.3. Class 3: ‘Single-Parent Household’ (n = 2967 [20.4% of Total Study Population])
3.2. Social and Physical Environment
3.3. Child Health-Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SES | Socioeconomic status |
| LCA | Latent class analysis |
| ACEs | Adverse childhood experiences |
| GP | General practitioner |
| ELAN | Extramural LUMC Academic Network |
Appendix A
| Child and Family Demographics | Definition | Categories | Data Source * |
|---|---|---|---|
| Individual dimension | |||
| Age | Categorical age of the child in years, calculated on 1 January 2018. | 0–4 years old 5–8 years old 9–12 years old | SSD |
| Gender | Gender of the child as stated at birth. | Male Female | SSD |
| Country of origin | Based on the child’s birthplace and the birthplaces of the child’s parents. An individual is categorized as ‘Dutch’ if both the person and their parents were born in the Netherlands. If the mother’s country of birth differs from the Netherlands, this country determines the classification. If the father was born in a country other than the Netherlands but the mother was born in the Netherlands, then the father’s country of birth determines the classification. If both parents were born outside the Netherlands, the mother’s country of birth is used as the determining factor. Categorized based on SSD and adjusted to frequent countries of origin in the Netherlands to fit the study population [1]. Based on the historical background of Dutch colonization, we combined Surinam, Indonesia, and the Dutch-Caribbean. | The Netherlands Europe (excluding the Netherlands) Turkey/Morocco Surinam/Indonesia/Dutch-Caribbean Other (Africa/Asia/America/Oceania) | SSD |
| Social problems | Social problems as registered by the GP in 2018 and 2019. Including problems with food/water, medical issues, with police or justice, due to violence, with family, with work/education, with housing, with partner/relation, with finances, and social problems. Included ICPC codes: Z04, Z04.01, Z04.02, Z04.03, Z04.04, Z04.05, Z24, Z27, Z28, Z29 Z29.01, Z29.02, Z29.03 Z16, Z16.01, Z16.02, Z16.03, Z18, Z19, Z20, Z21, Z21.01, Z21.02, Z22, Z23 Z12, Z12.01, Z12.02, Z13, Z13.01, Z13.02, Z13.03, Z14, Z15 | No Yes | ELAN |
| Household dimension | |||
| Family situation | One or both parents have been divorced in 2015–2019, or there was a shift from a two-parent household to a single-parent household. In 2018 it was registered as a single-parent household. If the registered household type includes two adults with children, an individual is considered as living in a two-parent household. This does not have to include one’s biological parents or married adults. The registered household composition refers to the number of persons registered at a home address at the same time in 2018. | Divorced parents over the past 5 years Single-parent household Household composition (n > 3) | SSD |
| Household income | Categorized household income based on percentage groups of standardized disposable income for private households at the start of 2018; <10th percentile is classified as low, 10th–90th percentile is classified as moderate, and >90th percentile is classified as high. | Low Moderate High | SSD |
| Home ownership | Home ownership of the home one lives in, in 2018. | Owner-occupied house Rental property without rent allowance Rental property with rent allowance | SSD |
| Socioeconomic Status (SES) neighborhood | Mean neighborhood SES of the neighborhood one lives in, measured by the SES-WOA score 2019 [63]. | Low Middle High | SSD |
| Parental dimension ** | |||
| Parental educational level | Highest registered educational level achieved in 2018 by either the mother or father, according to the International Standard Classification of Education. Low included primary school and junior high school. Middle included senior high school and MBO. High included HBO and WO. | Low Middle High Missing | SSD |
| Parental health | Health condition as registered by the GP in 2016–2019. Physical health conditions: diabetes, cancer, heart failure, coronary heart disease, stroke, rheumatism, migraine, chronic obstructive pulmonary disease (COPD), asthma, dementia, hypertensive heart disease, colitis ulcerosa, (head) trauma, thyroid disorder, stomach ulcer, sexually transmitted infections/HIV, eczema, osteoporosis, miscarriage, abortion, osteoarthritis, parkinson’s disease, epilepsy, chronic neck and back pain. Included ICPC-codes: T90, T90.01, T90.02, A79, B72, B72.01, B72.02, B73, D74, D75, D76, D77, D77.01, D77.02, D77.03, D77.04, L71, L71.01, L71.02, N74, R84, R85, S77, S77.01, S77.02, S77.03, S77.04, T71, U75, U76, U77, W72, X75, X76, X76.01, X77, X77.01, X77.02, Y77, Y78, Y78.01, Y78.02, Y78.03, K78, k79, K79.01, K79.02, K80, K80.01, K80.02, K80.03, K74, K74.01, K74.02, K75, K76, K76.01, K76.02, K89, K90, K90.01, K90.02, K90.03, K86, K87, L88, L88.01, L88.02, N89, R91, R91.01, R91.02, R95, R96, R96.02, P70, P70.01, P70.02, D93,D94, D94.01, D94.01, D85, D86, D86.01, D88-D91, D91.01, D91.02, D91.03, D98, D98.01, D98.02, D98.03, A80, A81, A82, N79, N80, N80.01, N80.02, N80.03, N80.04, N81, L76, L76.01, L76.02, L76.03, L76.04, L76.05 , L76.06, L76.07, L76.08, T81, T85, T86, X70, X71, X73, X74, X74.01, X90, X91, Y70-Y72, Y76, B90, B90.01, B90.02, S86, S86.01, S86.02, S88.01, S88.02, S88.03, S88.04, S87, S88, S89, S90, S91, W80, W82, W83, N87, N87.01, L89, L90, L91, N88, L83, L83.01, L84, L84.01, L84.02, L86, L86.01 Mental health conditions: suicide attempts, burnout/stress, mood disorder, anxiety disorder, substance abuse, personality disorder, psychotic disorder, attention-deficit hyperactivity disorder (ADHD)/behavioral disorder, autism spectrum disorder (ASD), eating disorder. Included ICPC-codes: P77, P77.01, P77.02, P78, P02, P06, P06.01, P07, P03, P73, P73.02, P76, P76.01, P76.02, P01, P02.01, P74, P74.01, P74.02, P79, P79.01, P79.02, P15, P15.01, P15.02, P15.03, P15.05, P15.06, P16, P17, P18, P19, P19.01, P19.02, P80, P80.01, P80.02, P72, P98, P21, P22, P23, P04, P99, P99.01, P99.02, T06, T06.01, T06.02 Somatic health condition: headache, generalized fatigue/pain, irritable bowel syndrome (IBS), abdominal pain, neck and back Pain. Included ICPC codes: D01, D02, D04, D06, Y02, N01, N02, N90, L01, L02, L03, D93, A01, A04, A04.01 | No parent physical condition One parent’s physical condition Both parents’ physical condition No parent mental condition One parent’s mental condition Both parents’ mental condition No parent somatic condition One parent’s somatic condition Both parents’ somatic condition | ELAN |
| Parental social problems | One or both parents have social problems as registered by the GP in 2016–2019. Including problems with food/water, medical issues, with police or justice, due to violence, with family, with work/education, with housing, with partner/relation, with finances and social problems. Included ICPC codes: Z04, Z04.01, Z04.02, Z04.03, Z04.04, Z04.05, Z24, Z27, Z28, Z29 Z29.01, Z29.02, Z29.03 Z16, Z16.01, Z16.02, Z16.03, Z18, Z19, Z20, Z21, Z21.01, Z21.02, Z22, Z23 Z12, Z12.01, Z12.02, Z13, Z13.01, Z13.02, Z13.03, Z14, Z15 One or both parents were registered as a victim of any criminal act (e.g., theft of belongings to sexual assault) reported to the police in 2015–2019. One or both parents were detained or suspected of a crime in 2015–2019. Based on registration of debt restructuring and/or delayed health insurance payments for more than six months for one or both parents in 2015–2019. | Parent(s) have social problems Parent(s) being victims of a crime Parent(s) being detained or suspected of a crime Parent(s) having debts | ELAN SSD SSD SSD |
| Social and Physical Environmental Factors | Definition | Categories * | Data Source ** |
|---|---|---|---|
| Physical environment | Includes proximity to highway, main road, railroad, high voltage, transmission tower, wind turbines, green environment, dunes, open nature, water, agricultural, shops, industry, offices, semi built up, and earthquake risk, heat stress, noise pollution, flood risk, air quality, accidents, car density, and shop vacancy. | Large negative deviation Negative deviation Small negative deviation Average | Livability Index |
| Nuisance and insecurity | Includes violent crimes, destruction, disturbances, and nuisance and insecurity. | Large negative deviation Negative deviation Average Small positive deviation/Positive deviation | Livability Index |
| Social cohesion | Includes diversity of life stages, population density, mutation rate of persons, household development, and social cohesion. | Large negative deviation Negative deviation Small negative deviation Average | Livability Index |
| Facilities | Includes distance to education, catering industry, culture, shops, healthcare, train station, and facility density, and job accessibility. | Small negative deviation/Average Small positive deviation Positive deviation Large positive deviation | Livability Index |
| Housing | Includes surface area of homes, proximity to monuments, building height, housing vacancy, construction period, private rental, owner-occupied homes, overcrowding, and construction type. | Large negative deviation Negative deviation Small negative deviation Average | Livability Index |
| Health Outcomes | Definition | Categories * | Data Source ** |
|---|---|---|---|
| Number of Health conditions | Categorized number of health conditions as included within physical, mental, and somatic health conditions as registered by the GP in 2018–2019. | No condition One condition Multiple conditions | ELAN |
| Physical health condition | Had a physical health condition as registered by the GP in 2018–2019. Including: endocrine disorders (thyroid disorder, diabetes, or rheumatism), cancer, sexually transmitted infections/HIV, cardiac diseases (heart failure, coronary heart disease, or hypertensive heart disease), asthma, chronic obstructive pulmonary disease (COPD), eczema (including Psoriasis), migraine, Diseases Dutch National Immunization Program, (head) trauma, epilepsy, lower respiratory tract infection. Included ICPC-codes: T90, T90.01, T90.02, L88, L88.01, L88.02, A79, B72, B72.01, B72.02, B73, D75, D76, D77, D77.01, D77.02, D77.03, D77.04, L71, L71.01, L71.01, N74, R84, R85, S77, T71, U75, U76, U77, W72, S77.02, S77.03, S77.04, X75, X76, X76.01, X77, X77.01, X77.02, Y78.01, Y78.02, Y78.03, Y77, Y78, W82, W83, X70, X71, X73, X74, X74.01, B90.01, B90.02, X90, X91, Y70, Y71, Y72, Y76, B90, K78, K79.01, K79.02, K80.01, K80.02, K80.03, K79, K80, K74, K74.01, K74.02, K76.01, K76.02, K75, K76, K86, K87, R96, R96.01, R96.02, S86, S86.01, S86.02, S88.01, S88.02, S88.03, S88.04, S87, S88, S89, S90, S91, N89, A80, A81, A82, N79, N80, N80.01, N80.02, N80.03, N80.04, N81, N88, R78, R81, R81.01 R83, R83.01, A71, A74, D71, N70, N70.01, N70.02, N72, R71, R91, R91.01, R91.02, R95 | No Yes | ELAN |
| Mental health condition | Had a mental health condition as registered by the GP in 2018–2019. Including: externalizing behavioral disorder (behavioral issues and attention-deficit hyperactivity disorder (ADHD), Substance abuse), internalizing behavioral disorder (mood disorder or anxiety disorder), other mental disorders (burnout, stress, personality disorder, autism spectrum disorder (ASD), or eating disorder). Included ICPC-codes: P15, P15.01, P15.02, P15.03, P15.05, P15.06, P19.01, P19.02, P16, P17, P18, P19, P21, P22, P23, P04, P03, P76, P76.01, P76.02, P73.02, P73, P74, P79, P79.01, P79.02, P74.01, P74.02, P02.01, P01, P72, P98, P80, P80.01, P80.02, P99.01,T06, T06.01, T06.02,P99.02, P99, P78, P78, P02, P06, P06.01, P07 | No Yes | ELAN |
| Somatic health condition | Had a somatic health condition as registered by the GP in 2018–2019. Including: headache disorders, (chronic) neck and back pain, generalized fatigue/pain, overweight/obesity, gastrointestinal conditions (including irritable bowel syndrome (IBS) and abdominal pain). Included ICPC-codes: N01, N02, N90, L01, L02, L03, L83, L83.01, L84, L84.01, L84.02, L86.01, L86, A01, A04, A04.01, T82, T83, D93, D94, D94.01, D94.02, D85, D86, D86.01, D88-D91, D91.01, D91.02, D91.03, D98, D98.01, D98.02, D98.03, D01, D02, D04, D06, Y02 | No Yes | ELAN |
| Healthcare expenditure | Total healthcare costs between 2018 and 2019. Includes all costs associated with the Health Insurance Act (e.g., GP costs and hospital care costs), excluding youth care costs. | ≥0 ≤560 >€560 ≤€950 >€950 ≤€1772 >€1772 Missings | SSD |
| GP visits | Total number of GP visits during 2018–2019. Excluding repeat prescriptions, flu vaccines, internal consultations, mail processing, notes, and missed appointments. | 0 visits 1–3 visits 4–6 visits 7 or more visits | ELAN |
| In contact with (inpatient or outpatient) youth care | Children to whom, during (part of) the reporting periods, one or more forms of assistance or care were provided under the Youth Act, such as support for psychological or parenting problems, or who received services and support through the Dutch Youth Protection Services. The juvenile court decides on a child protection measure to eliminate any threats to the safe development of a child, such as an unsafe family environment. This decision follows an investigation by the Council for Child Protection [4]. Included years: 2018–2019. | No Yes | SSD |
| Number of Class | Akaike Information Criterion (AIC) | Bayesian Information Criterion (BIC) | G-Square | Chi-Square Goodness of Fit | Residual Degrees of Freedom | Log Likelihood | Entropy |
|---|---|---|---|---|---|---|---|
| 1 | 384,962.3 | 385,182.3 | 115,321.10 | 1,315,665,127 | 14,518 | −192,452.20 | - |
| 2 | 363,567.3 | 364,014.8 | 94,622.32 | 380,063,330 | 14,488 | −181,724.60 | 0.80 |
| 3 | 357,324.1 | 357,999.2 | 88,696.10 | 419,886,409 | 14,458 | −178,573.10 | 0.82 |
| 4 | 354,395.4 | 355,298.1 | 85,886.72 | 115,893,466 | 14,428 | −177,078.70 | 0.79 |
| 5 | 352,336.7 | 353,466.9 | 83,912.73 | 45,522,607 | 14,398 | −176,019.30 | 0.76 |
| 6 | 350,727.8 | 352,085.5 | 82,563.98 | 35,120,814 | 14,368 | −175,184.90 | 0.75 |
| Class 1 | Class 2 | Class 3 | Total Study Population | |
|---|---|---|---|---|
| Social and physical environmental factors | N (%) | N (%) | N (%) | N (%) |
| Physical environment | ||||
| Large negative deviation | 639 (8.8%) | 2196 (50.9%) | 1094 (36.9%) | 3569 (24.5%) |
| Negative deviation | 1059 (14.6%) | 1356 (31.4%) | 914 (30.8%) | 3487 (24.0%) |
| Small negative deviation | 2352 (32.4%) | 625 (14.5%) | 673 (22.7%) | 3854 (26.5%) |
| Average | 3217 (44.3%) | 136 (3.2%) | 286 (9.6%) | 3637 (25.0%) |
| Nuisance and insecurity | ||||
| Large negative deviation | 612 (8.4%) | 1963 (45.5%) | 1110 (37.4%) | 3685 (25.3%) |
| Negative deviation | 1127 (15.5%) | 1565 (36.3%) | 913 (30.8%) | 3605 (24.8%) |
| Average | 2337 (32.2%) | 623 (14.4%) | 724 (24.4%) | 3684 (25.3%) |
| Small positive deviation/Positive deviation | 3191 (43.9%) | 162 (3.8%) | 220 (7.4%) | 3573 (24.6%) |
| Social cohesion | ||||
| Large negative deviation | 789 (10.9%) | 2159 (50.1%) | 1192 (40.2%) | 4140 (28.5%) |
| Negative deviation | 1712 (23.6%) | 1622 (37.6%) | 1121 (37.8%) | 4455 (30.6%) |
| Small negative deviation | 1464 (20.1%) | 307 (7.1%) | 386 (13.0%) | 2157 (14.8%) |
| Average | 3302 (45.4%) | 225 (5.2%) | 268 (9.0%) | 3795 (26.1%) |
| Facilities | ||||
| Small negative deviation/Average | 2227 (30.6%) | 763 (17.7%) | 565 (19.0%) | 3555 (24.4%) |
| Small positive deviation | 1650 (22.7%) | 1041 (24.1%) | 730 (24.6%) | 3421 (23.5%) |
| Positive deviation | 1847 (25.4%) | 1325 (30.7%) | 988 (33.3%) | 4160 (28.6%) |
| Large positive deviation | 1543 (21.2%) | 1184 (27.5%) | 684 (23.1%) | 3411 (23.4%) |
| Housing | ||||
| Large negative deviation | 695 (9.6%) | 1914 (44.4%) | 958 (32.3%) | 3567 (24.5%) |
| Negative deviation | 1096 (15.1%) | 1630 (37.8%) | 1120 (37.7%) | 3846 (26.4%) |
| Small negative deviation | 2315 (31.9%) | 573 (13.3%) | 595 (20.1%) | 3483 (23.9%) |
| Average | 3161 (43.5%) | 196 (4.5%) | 294 (9.9%) | 3651 (25.1%) |
| Class 1 | Class 2 | Class 3 | Total Study Population | |
|---|---|---|---|---|
| Child health outcomes | N (%) | N (%) | N (%) | N (%) |
| Number of health conditions | ||||
| No condition | 3928 (54.1%) | 2082 (48.3%) | 1397 (47.1%) | 7407 (50.9%) |
| One condition | 2234 (30.7%) | 1481 (34.3%) | 975 (32.9%) | 4690 (32.2%) |
| Multiple conditions | 1105 (15.2%) | 975 (32.9%) | 595 (20.1%) | 2450 (16.8%) |
| Physical health condition | ||||
| No | 4843 (66.6%) | 2686 (62.3%) | 1865 (62.9%) | 9394 (64.6%) |
| Yes | 2424 (33.4%) | 1627 (37.7%) | 1102 (37.1%) | 5153 (35.4%) |
| Mental health condition | ||||
| No | 6597 (90.8%) | 3991 (92.5%) | 2605 (87.8%) | 13,193 (90.7%) |
| Yes | 670 (9.2%) | 322 (7.5%) | 362 (12.2%) | 1354 (9.3%) |
| Somatic health condition | ||||
| No | 6182 (85.1%) | 3463 (80.3%) | 2395 (80.7%) | 12,040 (82.8%) |
| Yes | 1085 (14.9%) | 850 (19.7%) | 572 (19.3%) | 2507 (17.2%) |
| Healthcare expenditure | ||||
| ≥0 ≤560 | 2230 (30.7%) | 763 (17.7%) | 621 (20.9%) | 3614 (24.8%) |
| >€560 ≤€950 | 1891 (26.0%) | 1013 (23.5%) | 709 (23.9%) | 3613 (24.8%) |
| >€950 ≤€1772 | 1635 (22.5%) | 1208 (28.0%) | 793 (26.7%) | 3636 (25.0%) |
| >€1772 | 1473 (20.3%) | 1316 (30.5%) | 840 (28.3%) | 3629 (24.9%) |
| Missings | 38 (0.5%) | 13 (0.3%) | 4 (0.1%) | 55 (0.4%) |
| GP visits | ||||
| 0 visits | 3114 (42.9%) | 1376 (31.9%) | 979 (33.0%) | 5469 (37.6%) |
| 1–3 visits | 2059 (28.3%) | 1293 (30.0%) | 849 (28.6%) | 4201 (28.9%) |
| 4–6 visits | 1120 (15.4%) | 822 (19.1%) | 525 (17.7%) | 2467 (17.0%) |
| 7 or more visits | 974 (13.4%) | 822 (19.1%) | 614 (20.7%) | 2410 (16.6%) |
| In contact with youth care | ||||
| No | 6357 (87.5%) | 3744 (86.8%) | 2066 (69.6%) | 12,167 (83.6%) |
| Yes | 910 (12.5%) | 569 (13.2%) | 901 (30.4%) | 2380 (16.4%) |
References
- Hakulinen, C.; Mok, P.L.H.; Horsdal, H.T.; Pedersen, C.B.; Mortensen, P.B.; Agerbo, E.; Webb, R.T. Parental income as a marker for socioeconomic position during childhood and later risk of developing a secondary care-diagnosed mental disorder examined across the full diagnostic spectrum: A national cohort study. BMC Med. 2020, 18, 323. [Google Scholar] [CrossRef]
- Santini, Z.I.; Koyanagi, A.; Stewart-Brown, S.; Perry, B.D.; Marmot, M.; Koushede, V. Cumulative risk of compromised physical, mental and social health in adulthood due to family conflict and financial strain during childhood: A retrospective analysis based on survey data representative of 19 European countries. BMJ Glob. Health 2021, 6, e004144. [Google Scholar] [CrossRef]
- Andersen, S.H. Association of Youth Age at Exposure to Household Dysfunction with Outcomes in Early Adulthood. JAMA Netw. Open 2021, 4, e2032769. [Google Scholar] [CrossRef]
- Vaalavuo, M.; Niemi, R.; Suvisaari, J. Growing up unequal? Socioeconomic disparities in mental disorders throughout childhood in Finland. SSM Popul. Health 2022, 20, 101277. [Google Scholar] [CrossRef]
- van Minde, M.R.C.; de Kroon, M.L.A.; Sijpkens, M.K.; Raat, H.; Steegers, E.A.P.; Bertens, L.C.M. Associations between Socio-Economic Status and Unfavorable Social Indicators of Child Wellbeing; a Neighbourhood Level Data Design. Int. J. Environ. Res. Public. Health 2021, 18, 12661. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Applying Neurobiological and Socio-Behavioral Sciences from Prenatal Through Early Childhood Development: A Health Equity Approach. Vibrant and Healthy Kids: Aligning Science, Practice, and Policy to Advance Health Equity; Negussie, Y., Geller, A., DeVoe, J.E., Eds.; National Academies Press (US): Washington, DC, USA, 2019. [Google Scholar]
- Kruk, K.E. Parental income and the dynamics of health inequality in early childhood—Evidence from the UK. Health Econ. 2013, 22, 1199–1214. [Google Scholar] [CrossRef]
- Bronfenbrenner, U.; Morris, P.A. The Bioecological Model of Human Development. In Handbook of Child Psychology: Theoretical Models of Human Development, 6th ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2006; Volume 1, pp. 793–828. [Google Scholar]
- Zhang, H.; Lee, Z.X.; White, T.; Qiu, A. Parental and social factors in relation to child psychopathology, behavior, and cognitive function. Transl. Psychiatry 2020, 10, 80. [Google Scholar] [CrossRef]
- Bøe, T.; Serlachius, A.S.; Sivertsen, B.; Petrie, K.J.; Hysing, M. Cumulative effects of negative life events and family stress on children’s mental health: The Bergen Child Study. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 1–9. [Google Scholar] [CrossRef]
- Vermeiren, A.P.; Willeboordse, M.; Oosterhoff, M.; Bartelink, N.; Muris, P.; Bosma, H. Socioeconomic multi-domain health inequalities in Dutch primary school children. Eur. J. Public Health 2018, 28, 610–616. [Google Scholar] [CrossRef]
- Reiss, F. Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Soc. Sci. Med. 2013, 90, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; McLanahan, S. Family Structure Transitions and Child Development:Instability, Selection, and Population Heterogeneity. Am. Sociol. Rev. 2015, 80, 738–763. [Google Scholar] [CrossRef]
- Evans, G.W.; Kantrowitz, E. Socioeconomic Status and Health: The Potential Role of Environmental Risk Exposure. Annu. Rev. Public Health 2002, 23, 303–331. [Google Scholar] [CrossRef]
- WHO Regional Office for Europe. Environmental Health Inequalities in Europe; Second assessment report; WHO Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Houweling, T.A.J.; Grünberger, I. Intergenerational transmission of health inequalities: Towards a life course approach to socioeconomic inequalities in health—A review. J. Epidemiol. Community Health 2024, 78, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Raat, H.; You, Y.; Santos, S.; van Grieken, A.; Wang, H.; Yang-Huang, J. Change in neighborhood socioeconomic status and childhood weight status and body composition from birth to adolescence. Int. J. Obes. 2024, 48, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Subiza-Pérez, M.; García-Baquero, G.; Fernández-Somoano, A.; Riaño, I.; González, L.; Delgado-Saborit, J.M.; Guxens, M.; Fossati, S.; Vrijheid, M.; Fernandes, A.; et al. Social inequalities, green and blue spaces and mental health in 6–12 years old children participating in the INMA cohort. Health Place 2023, 83, 103104. [Google Scholar] [CrossRef] [PubMed]
- Cronin, C.E.; Gran, B.K. The importance of environment: Neighborhood characteristics and parent perceptions of child health. J. Child Health Care 2018, 22, 658–669. [Google Scholar] [CrossRef]
- Franzini, L.; Elliott, M.N.; Cuccaro, P.; Schuster, M.; Gilliland, M.J.; Grunbaum, J.A.; Franklin, F.; Tortolero, S.R. Influences of Physical and Social Neighborhood Environments on Children’s Physical Activity and Obesity. Am. J. Public Health 2009, 99, 271–278. [Google Scholar] [CrossRef]
- Kolthof, H.; Kikkert, M.; Dekker, J. Multiproblem or multirisk families. A broad review of the literature. J. Child. Adolesc. Behav. 2014, 2, 2. [Google Scholar]
- Ardesch, F.H.; Meulendijk, M.C.; Kist, J.M.; Vos, R.C.; Vos, H.M.M.; Kiefte-de Jong, J.C.; Spruit, M.; Bruijnzeels, M.A.; Bussemaker, M.J.; Numans, M.E.; et al. The introduction of a data-driven population health management approach in the Netherlands since 2019: The Extramural LUMC Academic Network data infrastructure. Health Policy 2023, 132, 104769. [Google Scholar] [CrossRef]
- Kist, J.M.; Vos, H.M.M.; Vos, R.C.; Mairuhu, A.T.A.; Struijs, J.N.; Vermeiren, R.; van Peet, P.G.; van Os, H.J.A.; Ardesch, F.H.; Beishuizen, E.D.; et al. Data Resource Profile: Extramural Leiden University Medical Center Academic Network (ELAN). Int. J. Epidemiol. 2024, 53, dyae099. [Google Scholar] [CrossRef]
- Lamberts, H.; Hofmans-Okkes, I. The core of computer based patient records in family practice: Episodes of care classified with ICPC. Int. J. Biomed. Comput. 1996, 42, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Bakker, B.F.M.; van Rooijen, J.; van Toor, L. The System of social statistical datasets of Statistics Netherlands: An integral approach to the production of register-based social statistics. Stat. J. IAOS 2014, 30, 411–424. [Google Scholar] [CrossRef]
- Leefbarometer Meting 2018: Data.Overheid. 2018. Available online: https://data.overheid.nl/dataset/leefbaarometer-meting-2018 (accessed on 17 January 2025).
- Haag, G.D. Den Haag in Cijfers. 2018. Available online: https://denhaag.incijfers.nl/viewer?workspace_guid=48401fff-221b-40fc-830d-f94d24836a0e (accessed on 17 March 2025).
- Leiden, G. Leiden in Cijfers. 2018. Available online: https://leiden.incijfers.nl (accessed on 17 March 2025).
- van Rossem, L.; Hafkamp-de Groen, E.; Jaddoe, V.W.; Hofman, A.; Mackenbach, J.P.; Raat, H. The role of early life factors in the development of ethnic differences in growth and overweight in preschool children: A prospective birth cohort. BMC Public Health 2014, 14, 722. [Google Scholar] [CrossRef] [PubMed]
- Leefbaarometer—Online Informatie Over de Leefbaarheid in Alle Buurten en Wijken: Ministerie van Binnenlandse Zaken en Koninkrijksrelaties. Available online: https://www.leefbaarometer.nl/page/FAQ (accessed on 17 January 2025).
- Ferro, M.A.; Lipman, E.L.; Van Lieshout, R.J.; Gorter, J.W.; Shanahan, L.; Boyle, M.; Georgiades, K.; Timmons, B. Multimorbidity in Children and Youth Across the Life-course (MY LIFE): Protocol of a Canadian prospective study. BMJ Open 2019, 9, e034544. [Google Scholar] [CrossRef]
- van den Akker, M.; Dieckelmann, M.; Hussain, M.A.; Bond-Smith, D.; Muth, C.; Pati, S.; Saxena, S.; Silva, D.; Skoss, R.; Straker, L.; et al. Children and adolescents are not small adults: Toward a better understanding of multimorbidity in younger populations. J. Clin. Epidemiol. 2022, 149, 165–171. [Google Scholar] [CrossRef]
- Weller, B.E.; Bowen, N.K.; Faubert, S.J. Latent Class Analysis: A Guide to Best Practice. J. Black Psychol. 2020, 46, 287–311. [Google Scholar] [CrossRef]
- Ashiabi, G.S.; O’Neal, K.K. Child Social Development in Context:An Examination of Some Propositions in Bronfenbrenner’s Bioecological Theory. Sage Open 2015, 5, 2158244015590840. [Google Scholar] [CrossRef]
- Vandeleur, D.M.; Cunningham, M.M.; Palermo, T.M.; Groenewald, C.B. Association of Neighborhood Characteristics and Chronic Pain in Children and Adolescents in the United States. Clin. J. Pain 2024, 40, 174–181. [Google Scholar] [CrossRef]
- Gelormino, E.; Melis, G.; Marietta, C.; Costa, G. From built environment to health inequalities: An explanatory framework based on evidence. Prev. Med. Rep. 2015, 2, 737–745. [Google Scholar] [CrossRef]
- Weitoft, G.R.; Hjern, A.; Haglund, B.; Rosén, M. Mortality, severe morbidity, and injury in children living with single parents in Sweden: A population-based study. Lancet 2003, 361, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Rattay, P.; von der Lippe, E.; Lampert, T.; Ergebnisse der KiGGS Study Group. Gesundheit von Kindern und Jugendlichen in Eineltern-, Stief- und Kernfamilien. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 2014, 57, 860–868. [Google Scholar] [CrossRef]
- Lanza-León, P.; Cantarero-Prieto, D. The Loud Silent Side of Single Parenthood in Europe: Health and Socio-Economic Circumstances from a Gender Perspective. J. Fam. Econ. Issues 2024, 46, 479–491. [Google Scholar] [CrossRef]
- Grüning Parache, L.; Vogel, M.; Meigen, C.; Kiess, W.; Poulain, T. Family structure, socioeconomic status, and mental health in childhood. Eur. Child Adolesc. Psychiatry 2024, 33, 2377–2386. [Google Scholar] [CrossRef]
- Miguel, P.M.; Pereira, L.O.; Silveira, P.P.; Meaney, M.J. Early environmental influences on the development of children’s brain structure and function. Dev. Med. Child. Neurol. 2019, 61, 1127–1133. [Google Scholar] [CrossRef] [PubMed]
- Björkenstam, E.; Björkenstam, C.; Jablonska, B.; Kosidou, K. Cumulative exposure to childhood adversity, and treated attention deficit/hyperactivity disorder: A cohort study of 543 650 adolescents and young adults in Sweden. Psychol. Med. 2018, 48, 498–507. [Google Scholar] [CrossRef] [PubMed]
- Lindström, M.; Rosvall, M. Parental separation/divorce in childhood and tobacco smoking in adulthood: A population-based study. Scand. J. Public. Health 2020, 48, 657–666. [Google Scholar] [CrossRef]
- Webster, E.M. The Impact of Adverse Childhood Experiences on Health and Development in Young Children. Glob. Pediatr. Health 2022, 9, 2333794x221078708. [Google Scholar] [CrossRef]
- Ma, J.; Lee, S.J.; Grogan-Kaylor, A. Adverse Childhood Experiences and Spanking Have Similar Associations with Early Behavior Problems. J. Pediatr. 2021, 235, 170–177. [Google Scholar] [CrossRef]
- De Bellis, M.D.; Zisk, A. The biological effects of childhood trauma. Child. Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 185–222. [Google Scholar] [CrossRef] [PubMed]
- Liao, H.; Yan, C.; Ma, Y.; Wang, J. Impact of Adverse Childhood Experiences on Older Adult Poverty: Mediating Role of Depression. Front. Public. Health 2021, 9, 749640. [Google Scholar] [CrossRef]
- Motoc, I.; Hoogendijk, E.O.; Timmermans, E.J.; Deeg, D.; Penninx, B.W.J.H.; Huisman, M. Social and physical neighbourhood characteristics and 10-year incidence of depression and anxiety in older adults: Results from the Longitudinal Aging Study Amsterdam. Soc. Sci. Med. 2023, 327, 115963. [Google Scholar] [CrossRef]
- Singer, M.; Bulled, N.; Ostrach, B.; Mendenhall, E. Syndemics and the biosocial conception of health. Lancet 2017, 389, 941–950. [Google Scholar] [CrossRef]
- Slagboom, M.N.; Crone, M.R.; Reis, R. Exploring syndemic vulnerability across generations: A case study of a former fishing village in the Netherlands. Soc. Sci. Med. 2022, 295, 113122. [Google Scholar] [CrossRef]
- Nicholson, J.M.; Lucas, N.; Berthelsen, D.; Wake, M. Socioeconomic inequality profiles in physical and developmental health from 0–7 years: Australian National Study. J. Epidemiol. Community Health 2012, 66, 81–87. [Google Scholar] [CrossRef]
- Russell, J.; Grant, C.C.; Morton, S.M.B. Multimorbidity in Early Childhood and Socioeconomic Disadvantage: Findings From a Large New Zealand Child Cohort. Acad. Pediatr. 2020, 20, 619–627. [Google Scholar] [CrossRef]
- Bouthoorn, S.H.; Wijtzes, A.I.; Jaddoe, V.W.V.; Hofman, A.; Raat, H.; van Lenthe, F.J. Development of socioeconomic inequalities in obesity among Dutch pre-school and school-aged children. Obesity 2014, 22, 2230–2237. [Google Scholar] [CrossRef]
- Rod, N.H.; Bengtsson, J.; Elsenburg, L.K.; Taylor-Robinson, D.; Rieckmann, A. Hospitalisation patterns among children exposed to childhood adversity: A population-based cohort study of half a million children. Lancet Public Health 2021, 6, e826–e835. [Google Scholar] [CrossRef]
- Cheng, T.L.; Johnson, S.B.; Goodman, E. Breaking the Intergenerational Cycle of Disadvantage: The Three Generation Approach. Pediatrics 2016, 137, e20152467. [Google Scholar] [CrossRef]
- Ellis, W.R.; Dietz, W.H. A New Framework for Addressing Adverse Childhood and Community Experiences: The Building Community Resilience Model. Acad. Pediatr. 2017, 17, S86–S93. [Google Scholar] [CrossRef]
- Ellis, W.; Dietz, W.H.; Chen, K.-L.D. Community Resilience: A Dynamic Model for Public Health 3.0. J. Public Health Manag. Pract. 2022, 28, S18–S26. [Google Scholar] [CrossRef]
- Bontje, M.C.A.; de Ronde, R.W.; Dubbeldeman, E.M.; Kamphuis, M.; Reis, R.; Crone, M.R. Parental engagement in preventive youth health care: Effect evaluation. Child. Youth Serv. Rev. 2021, 120, 105724. [Google Scholar] [CrossRef]
- Wicki, W.; Künzle, R.; Müller, M.; Ziegele, U.; Stadelmann, K.; Gschwind, K. Tasks and impact of school social work in Switzerland as perceived by teachers, principals and school social workers—A multilevel analysis. Int. J. Sch. Soc. Work. 2020, 5, 1–18. [Google Scholar] [CrossRef]
- Isaksson, C.; Sjöström, S. Looking for ‘social work’ in school social work. Eur. J. Soc. Work. 2016, 20, 1–12. [Google Scholar] [CrossRef]
- FitzGerald, C.; Hurst, S. Implicit bias in healthcare professionals: A systematic review. BMC Med. Ethics 2017, 18, 19. [Google Scholar] [CrossRef] [PubMed]
- Tang, E.; de Haan, A.D.; Kuiper, C.H.Z.; Harder, A.T. Family-centred practice and family outcomes in residential youth care: A systematic review. Child Fam. Soc. Work. 2024, 29, 598–614. [Google Scholar] [CrossRef]
- CBS. Sociaal-Economische Status; Scores Per Wijk en Buurt, Regio-Indeling. 2021. Available online: https://opendata.cbs.nl/#/CBS/nl/dataset/85163NED/table (accessed on 13 February 2024).
- Mandemakers, J.; Leidelmeijer, K.; Burema, F.; Halbersma, R.; Middeldorp, M.; Veldkamp, J. Instrumentontwikkeling Leefbarometer 3.0; Atlas Research: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Wong, R.S.; Tung, K.T.S.; Rao, N.; Chan, K.L.; Fu, K.W.; Yam, J.C.; Tso, W.W.Y.; Wong, W.H.S.; Lum, T.Y.S.; Wong, I.C.K.; et al. Using Latent Class Analyses to Examine Health Disparities among Young Children in Socially Disadvantaged Families during the COVID-19 Pandemic. Int. J. Environ. Res. Public. Health 2022, 19, 7893. [Google Scholar] [CrossRef] [PubMed]
- Petersen, K.J.; Qualter, P.; Humphrey, N. The Application of Latent Class Analysis for Investigating Population Child Mental Health: A Systematic Review. Front. Psychol. 2019, 10, 1214. [Google Scholar] [CrossRef] [PubMed]
| Class 1 | Class 2 | Class 3 | Total Study Population | |
|---|---|---|---|---|
|
Dutch-origin two-parent household (n = 7267) | Households with diverse countries of origin (n = 4313) |
Single-parent household (n = 2967) |
n (%) (n = 14,547) | |
| Estimated class population shares | 49.2 | 29.5 | 21.3 | |
| Predicted by modal posterior probability | 50.0 | 29.7 | 20.4 | |
| Individual level | ||||
| Age 3 ** | ||||
| 0–4 years old | 35.0 | 35.9 | 33.5 | 5087 (35.0) |
| 5–8 years old | 34.1 | 32.9 | 33.5 | 4889 (33.6) |
| 9–12 years old | 30.9 | 31.2 | 33.0 | 4571 (31.4) |
| Gender 3 ** | ||||
| Male | 50.8 | 50.2 | 52.3 | 7410 (50.9) |
| Female | 49.2 | 49.8 | 47.7 | 7137 (49.1) |
| Country of origin 3 ** | ||||
| Netherlands | 67.8 | 16.0 | 39.6 | 6762 (46.5) |
| European (other than the Netherlands) | 13.3 | 8.1 | 8.9 | 1571 (10.8) |
| Turkey/Morocco | 2.6 | 51.7 | 16.0 | 2899 (19.9) |
| Suriname/Indonesia/Dutch-Caribbean | 4.3 | 6.2 | 15.9 | 1068 (7.3) |
| Other(Africa/Asia/America/Oceania) | 12.1 | 18.0 | 19.5 | 2247 (15.4) |
| Social problems 3 | 1.7 | 3.0 | 10.0 | 561 (3.9) |
| Household level | ||||
| Family situation | ||||
| Divorced parents over the past 5 years 6 | 4.7 | 4.1 | 36.1 | 1629 (11.2) |
| Single parent household 3 ** | 4.4 | 0.3 | 84.8 | 2961 (20.4) |
| Household composition (n > 3) 3 ** | 78.1 | 90.4 | 35.6 | 10607 (72.9) |
| Household income 3 ** | ||||
| Low | 1.0 | 34.0 | 42.5 | 2852 (19.6) |
| Moderate | 73.7 | 65.2 | 57.5 | 9851 (67.7) |
| High | 25.4 | 0.7 | 0 | 1844 (12.7) |
| Home ownership 3 * | ||||
| Owner-occupied house | 88.6 | 31.7 | 17.3 | 8234 (56.6) |
| Rental property without rent allowance | 11.4 | 38.5 | 15.6 | 2950 (20.3) |
| Rental property with rent allowance | 0 | 29.8 | 67.1 | 3363 (23.1) |
| SES neighborhood 4 * | ||||
| Low | 33.0 | 87.7 | 76.9 | 8511 (58.5) |
| Middle | 13.8 | 3.1 | 8.8 | 1395 (9.6) |
| High | 53.2 | 9.2 | 14.3 | 4641 (31.9) |
| Parental level | ||||
| Parental educational level 5 ** | ||||
| Low | 3.2 | 39.2 | 36.5 | 2770 (19.0) |
| Middle | 13.3 | 39.5 | 43.4 | 3634 (25.0) |
| High | 83.5 | 21.4 | 20.1 | 6763 (46.5) |
| Missing | 1380 (9.5) | |||
| Parental health ** | ||||
| No parent physical condition 7 | 41.1 | 27.8 | 35.1 | 5223 (35.9) |
| One parent physical condition 7 | 44.1 | 47.9 | 54.7 | 6905 (47.5) |
| Both parents physical condition 7 | 14.8 | 24.3 | 10.2 | 2419 (16.6) |
| No parent mental condition 7 | 61.5 | 49.5 | 41.2 | 7797 (53.6) |
| One parent mental condition 7 | 32.2 | 38.9 | 49.3 | 5499 (37.8) |
| Both parents mental condition 7 | 6.3 | 11.7 | 9.6 | 1251 (8.6) |
| No parent somatic condition 7 | 44.6 | 19.5 | 30.9 | 4983 (34.3) |
| One parent somatic condition 7 | 42.8 | 49.4 | 59.2 | 7012 (48.2) |
| Both parents somatic condition 7 | 12.7 | 31.1 | 10.0 | 2552 (17.5) |
| Parental social problems | ||||
| Parent(s) having social problems 7 ** | 14.4 | 24.0 | 38.9 | 3268 (22.5) |
| Parent(s) being victim of a crime 6 | 14.3 | 26.0 | 33.5 | 3177 (21.8) |
| Parent(s) being detained or suspected of a crime 6 | 3.1 | 14.7 | 33.3 | 1886 (13.0) |
| Parent(s) having debts 6 ** | 0.9 | 13.9 | 37.2 | 1818 (12.5) |
| Class 2 | Class 3 | |||||
| Social and physical environmental factors | OR | 95% CI | p | OR | 95% CI | p |
| Physical environment | ||||||
| Intercept | 1.26 | [1.17–1.36] | <0.001 | 0.68 | [0.62–0.74] | <0.001 |
| Large negative deviation | 1.00 | 1.00 | ||||
| Negative deviation | 0.75 | [0.67–0.83] | <0.001 | 0.88 | [0.78–1.00] | 0.048 |
| Small negative deviation | 0.60 | [0.54–0.66] | <0.001 | 0.85 | [0.76–0.96] | 0.008 |
| Average | 0.06 | [0.06–0.07] | <0.001 | 0.18 | [0.15–0.20] | <0.001 |
| Nuisance and insecurity | ||||||
| Intercept | 3.21 | [2.93–3.51] | <0.001 | 1.81 | [1.64–2.00] | <0.001 |
| Large negative deviation | 1.00 | 1.00 | ||||
| Negative deviation | 0.43 | [0.38–0.49] | <0.001 | 0.45 | [0.39–0.51] | <0.001 |
| Average | 0.08 | [0.07–0.09] | <0.001 | 0.17 | [0.15–0.19] | <0.001 |
| Small positive deviation/Positive deviation | 0.02 | [0.01–0.02] | <0.001 | 0.04 | [0.03–0.05] | <0.001 |
| Social cohesion | ||||||
| Intercept | 2.74 | [2.52–2.97] | <0.001 | 1.51 | [1.38–1.65] | <0.001 |
| Large negative deviation | 1.00 | 1.00 | ||||
| Negative deviation | 0.35 | [0.31–0.39] | <0.001 | 0.43 | [0.39–0.49] | <0.001 |
| Small negative deviation | 0.08 | [0.07–0.09] | <0.001 | 0.18 | [0.15–0.20] | <0.001 |
| Average | 0.03 | [0.02–0.03] | <0.001 | 0.05 | [0.05–0.06] | <0.001 |
| Facilities | ||||||
| Intercept | 0.34 | [0.32–0.37] | <0.001 | 0.25 | [0.23–0.28] | <0.001 |
| Small negative deviation/Average | 1.00 | 1.00 | ||||
| Small positive deviation | 1.84 | [1.64–2.06] | <0.001 | 1.74 | [1.54–1.98] | <0.001 |
| Positive deviation | 2.09 | [1.88–2.33] | <0.001 | 2.11 | [1.87–2.38] | <0.001 |
| Large positive deviation | 2.24 | [2.00–2.51] | <0.001 | 1.75 | [1.54–1.99] | <0.001 |
| Housing | ||||||
| Intercept | 2.75 | [2.53–3.00] | <0.001 | 1.38 | [1.25–1.52] | <0.001 |
| Large negative deviation | 1.00 | 1.00 | ||||
| Negative deviation | 0.54 | [0.48–0.61] | <0.001 | 0.74 | [0.65–0.84] | <0.001 |
| Small negative deviation | 0.09 | [0.08–0.10] | <0.001 | 0.19 | [0.16–0.21] | <0.001 |
| Average | 0.02 | [0.02–0.03] | <0.001 | 0.07 | [0.06–0.08] | <0.001 |
| Child Health Outcomes | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p |
|---|---|---|---|---|---|---|---|---|---|
| Number of health conditions (ref = no condition) | One condition | Multiple conditions | |||||||
| Intercept | 0.57 | [0.54–0.60] | <0.001 | 0.28 | [0.26–0.30] | <0.001 | |||
| Class 1 | 1.00 | 1.00 | |||||||
| Class 2 | 1.25 | [1.15–1.36] | <0.001 | 1.23 | [1.11–1.35] | <0.001 | |||
| Class 3 | 1.23 | [1.11–1.35] | <0.001 | 1.51 | [1.35–1.70] | <0.001 | |||
| Physical health condition (ref = no) | Yes | ||||||||
| Intercept | 0.50 | [0.48–0.53] | <0.001 | ||||||
| Class 1 | 1.00 | ||||||||
| Class 2 | 1.21 | [1.12–1.31] | <0.001 | ||||||
| Class 3 | 1.18 | [1.08–1.29] | <0.001 | ||||||
| Mental health condition (ref = no) | Yes | ||||||||
| Intercept | 0.10 | [0.09–0.11] | <0.001 | ||||||
| Class 1 | 1.00 | ||||||||
| Class 2 | 0.79 | [0.69–0.91] | <0.001 | ||||||
| Class 3 | 1.37 | [1.19–1.57] | <0.001 | ||||||
| Somatic health condition (ref = no) | Yes | ||||||||
| Intercept | 0.18 | [0.16–0.19] | <0.001 | ||||||
| Class 1 | 1.00 | ||||||||
| Class 2 | 1.40 | [1.27–1.54] | <0.001 | ||||||
| Class 3 | 1.36 | [1.22–1.52] | <0.001 | ||||||
| Healthcare expenditure (ref = ≥0 ≤560) | >€560 ≤ €950 | >€950 ≤ €1772 | >€1772 | ||||||
| Intercept | 0.85 | [0.80–0.90] | <0.001 | 0.73 | [0.69–0.78] | <0.001 | 0.66 | [0.62–0.71] | <0.001 |
| Class 1 | 1.00 | 1.00 | 1.00 | ||||||
| Class 2 | 1.57 | [1.40–1.75] | <0.001 | 2.16 | [1.93–2.41] | <0.001 | 2.61 | [2.34–2.92] | <0.001 |
| Class 3 | 1.35 | [1.19–1.52] | <0.001 | 1.74 | [1.54–1.97] | <0.001 | 2.05 | [1.81–2.32] | <0.001 |
| GP visits (ref = 0 visits) | 1–3 visits | 4–6 visits | 7 or more visits | ||||||
| Intercept | 0.66 | [0.63–0.70] | <0.001 | 0.36 | [0.34–0.39] | <0.001 | 0.31 | [0.29–0.34] | <0.001 |
| Class 1 | 1.00 | 1.00 | 1.00 | ||||||
| Class 2 | 1.42 | [1.29–1.56] | <0.001 | 1.66 | [1.49–1.85] | <0.001 | 1.91 | [1.71–2.14] | <0.001 |
| Class 3 | 1.31 | [1.18–1.46] | <0.001 | 1.49 | [1.31–1.69] | <0.001 | 2.01 | [1.77–2.27] | <0.001 |
| In contact with youth care (ref = no) | Yes | ||||||||
| Intercept | 0.14 | [0.13–0.15] | <0.001 | ||||||
| Class 1 | 1.00 | ||||||||
| Class 2 | 1.06 | [0.95–1.19] | 0.296 | ||||||
| Class 3 | 3.05 | [2.74–3.38] | <0.001 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Groenestein, S.F.F.; Crone, M.R.; Dubbeldeman, E.M.; Lottman, S.; Kiefte-de Jong, J.C.; Bussemaker, J.; van der Pas, S. Exploring Family Typologies and Health Outcomes in a Dutch Primary Care Population of Children Living in Urban Cities in the Netherlands: A Latent Class Analysis. Int. J. Environ. Res. Public Health 2025, 22, 1474. https://doi.org/10.3390/ijerph22101474
Groenestein SFF, Crone MR, Dubbeldeman EM, Lottman S, Kiefte-de Jong JC, Bussemaker J, van der Pas S. Exploring Family Typologies and Health Outcomes in a Dutch Primary Care Population of Children Living in Urban Cities in the Netherlands: A Latent Class Analysis. International Journal of Environmental Research and Public Health. 2025; 22(10):1474. https://doi.org/10.3390/ijerph22101474
Chicago/Turabian StyleGroenestein, Samantha F. F., Matty R. Crone, Evelien M. Dubbeldeman, Stijntje Lottman, Jessica C. Kiefte-de Jong, Jet Bussemaker, and Suzan van der Pas. 2025. "Exploring Family Typologies and Health Outcomes in a Dutch Primary Care Population of Children Living in Urban Cities in the Netherlands: A Latent Class Analysis" International Journal of Environmental Research and Public Health 22, no. 10: 1474. https://doi.org/10.3390/ijerph22101474
APA StyleGroenestein, S. F. F., Crone, M. R., Dubbeldeman, E. M., Lottman, S., Kiefte-de Jong, J. C., Bussemaker, J., & van der Pas, S. (2025). Exploring Family Typologies and Health Outcomes in a Dutch Primary Care Population of Children Living in Urban Cities in the Netherlands: A Latent Class Analysis. International Journal of Environmental Research and Public Health, 22(10), 1474. https://doi.org/10.3390/ijerph22101474






