Fear of COVID-19 and PTSD: The Protective Function of Problem-Solving Appraisals in Mental Health
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Context
2.2. Participants and Procedure
2.3. Instruments
2.4. Ethics
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ammar, A.; Chtourou, H.; Boukhris, O.; Trabelsi, K.; Masmoudi, L.; Brach, M.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M. COVID-19 home confinement negatively impacts social participation and life satisfaction: A worldwide multicenter study. Int. J. Environ. Res. Public Health 2020, 17, 6237. [Google Scholar] [CrossRef]
- Padmanabhanunni, A. Psychological distress in the time of COVID-19: The relationship between anxiety, hopelessness, and depression and the mediating role of sense of coherence. Traumatology 2022, 28, 376–382. [Google Scholar] [CrossRef]
- Cooper, S.; Kramers-Olen, A.L. University students’ mental health and emotional wellbeing during the COVID-19 pandemic and ensuing lockdown. South Afr. J. Psychol. 2021, 51, 229–243. [Google Scholar] [CrossRef]
- Chu, Y.-H.; Li, Y.-C. The Impact of Online Learning on Physical and Mental Health in University Students during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2966. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.-Y.; Schleider, J.L.; Nelson, B.D.; Richmond, L.L.; Eaton, N.R. Gender and Racial/Ethnic Disparities in Undergraduate and Graduate Students’ Mental Health and Treatment Use Amid the COVID-19 Pandemic. Adm. Policy Ment. Health Ment. Health Serv. Res. 2023, 50, 552–562. [Google Scholar] [CrossRef] [PubMed]
- Theurel, A.; Witt, A. Identifying Barriers to Mental Health Help-Seeking in French University Students during the COVID-19 Pandemic. Creative Educ. 2022, 13, 437–449. [Google Scholar] [CrossRef]
- Thomeer, M.B.; Moody, M.D.; Yahirun, J. Racial and Ethnic Disparities in Mental Health and Mental Health Care During The COVID-19 Pandemic. J. Racial Ethn. Health Disparities 2023, 10, 961–976. [Google Scholar] [CrossRef] [PubMed]
- Philippe, T.J.; Sikder, N.; Jackson, A.; Koblanski, M.E.; Liow, E.; Pilarinos, A.; Vasarhelyi, K. Digital Health Interventions for Delivery of Mental Health Care: Systematic and Comprehensive Meta-Review. JMIR Ment. Health 2022, 9, e35159. [Google Scholar] [CrossRef] [PubMed]
- Sinha, C.; Meheli, S.; Kadaba, M. Understanding Digital Mental Health Needs and Usage With an Artificial Intelligence-Led Mental Health App (Wysa) During the COVID-19 Pandemic: Retrospective Analysis. JMIR Form. Res. 2023, 7, e41913. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Robinson, E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2021, 136, 603–609. [Google Scholar] [CrossRef]
- Fernández, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Picco, S.; Pedreira, M.E. Psychological distress and mental health trajectories during the COVID-19 pandemic in Argentina: A longitudinal study. Sci. Rep. 2022, 12, 5632. [Google Scholar] [CrossRef]
- Duong, C.D. The impact of fear and anxiety of COVID-19 on life satisfaction: Psychological distress and sleep disturbance as mediators. Personal. Individ. Differ. 2021, 178, 110869. [Google Scholar] [CrossRef]
- Duong, T.V.; Nguyen, M.H.; Lai, C.-F.; Chen, S.-C.; Dadaczynski, K.; Okan, O.; Lin, C.-Y. COVID-19-related fear, stress and depression in school principals: Impacts of symptoms like COVID-19, information confusion, health-related activity limitations, working hours, sense of coherence and health literacy. Ann. Med. 2022, 54, 2064–2077. [Google Scholar] [CrossRef]
- Abuhammad, S.; Khabour, O.F.; Alomari, M.A.; Alzoubi, K.H. Depression, stress, anxiety among jordanian people during COVID-19 pandemic: A survey-based study. Inform. Med. Unlocked 2022, 30, 100936. [Google Scholar] [CrossRef]
- Islam, M.R.; Nahar, Z.; Hossain, M.S.; Hossain, M.J.; Shahriar, M.; Islam, S.M.A.; Bhuiyan, M.A. Prevalence and associated factors for elevated fear and depressive symptoms among the private service holders in Bangladesh during the COVID-19 pandemic: A cross-sectional study. Health Sci. Rep. 2022, 5, e795. [Google Scholar] [CrossRef]
- Padmanabhanunni, A.; Pretorius, T.B.; Bouchard, J.-P.; Stiegler, N. Facing your fear of COVID-19: Resilience as a protective factor against burnout in South African teachers. Ann. Médico-Psychol. 2023, 181, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Ji, B.; Liu, Y.; Zhang, J.; Liu, Q.; Ge, Y.; Xie, Y.; Liu, C. The prevalence of psychological stress in student populations during the COVID-19 epidemic: A systematic review and meta-analysis. Sci. Rep. 2022, 12, 12118. [Google Scholar] [CrossRef] [PubMed]
- Parvar, S.Y.; Ghamari, N.; Pezeshkian, F.; Shahriarirad, R. Prevalence of anxiety, depression, stress, and perceived stress and their relation with resilience during the COVID-19 pandemic, a cross-sectional study. Health Sci. Rep. 2022, 5, e460. [Google Scholar] [CrossRef] [PubMed]
- Pressley, T.; Ha, C.; Learn, E. Teacher stress and anxiety during COVID-19: An empirical study. Sch. Psychol. 2021, 36, 367. [Google Scholar] [CrossRef]
- Knowles, K.A.; Olatunji, B.O. Specificity of trait anxiety in anxiety and depression: Meta-analysis of the State-Trait Anxiety Inventory. Clin. Psychol. Rev. 2020, 82, 101928. [Google Scholar] [CrossRef]
- Pretorius, T.B.; Padmanabhanunni, A. Anxiety in Brief: Assessment of the Five-Item Trait Scale of the State-Trait Anxiety Inventory in South Africa. Int. J. Environ. Res. Public Health 2023, 20, 5697. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, T.B.; Padmanabhanunni, A. Toward a Positive Life beyond COVID-19: Problem-Solving Appraisal as a Resistance Resource in the Relationship between Stress and Well-Being in Students. Healthcare 2023, 11, 350. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Hui, W.; Lan, X.; Wei, J.; Hu, Y.; Li, R.; Zhang, Z.; Yuan, S.; Jiao, Z. A follow-up study of post-traumatic stress disorder of SARS patients after discharge. Chin. J. Rehabil. Med. 2006, 21, 1003–1004. [Google Scholar]
- Kaputu-Kalala-Malu, C.; Musalu, E.M.; Walker, T.; Ntumba-Tshitenge, O.; Ahuka-Mundeke, S. PTSD, depression and anxiety in Ebola virus disease survivors in Beni town, Democratic Republic of the Congo. BMC Psychiatry 2021, 21, 1–342. [Google Scholar] [CrossRef]
- Yuan, K.; Gong, Y.-M.; Liu, L.; Sun, Y.-K.; Tian, S.-S.; Wang, Y.-J.; Zhong, Y.; Zhang, A.-Y.; Su, S.-Z.; Liu, X.-X.; et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: A meta-analysis and systematic review. Mol. Psychiatry 2021, 26, 4982–4998. [Google Scholar] [CrossRef] [PubMed]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef]
- Yunitri, N.; Chu, H.; Kang, X.L.; Jen, H.-J.; Pien, L.-C.; Tsai, H.-T.; Kamil, A.R.; Chou, K.-R. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: A meta-analysis. Int. J. Nurs. Stud. 2022, 126, 104136. [Google Scholar] [CrossRef]
- Idoiaga, N.; Legorburu, I.; Ozamiz-Etxebarria, N.; Lipnicki, D.M.; Villagrasa, B.; Santabárbara, J. Prevalence of Post-Traumatic Stress Disorder (PTSD) in University Students during the COVID-19 Pandemic: A Meta-Analysis Attending SDG 3 and 4 of the 2030 Agenda. Sustainability 2022, 14, 7914. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2022. [Google Scholar]
- Sun, R.; Zhou, X. Differences in posttraumatic stress disorder networks between young adults and adolescents during the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 2023, 15, S29. [Google Scholar] [CrossRef]
- Lazarus, R.S. Stress and Emotion: A New Synthesis; Springer publishing Company: Berlin/Heidelberg, Germany, 2006. [Google Scholar]
- Ali, A.; Khan, A.A.; Abbas, S.; Khan, A.S.; Ullah, E. Cognitive appraisal, Coping, Stress and Fear Contracting COVID-19 in Working People in Pakistan. J. Ration.-Emotive Cogn.-Behav. Ther. 2022, 40, 663–682. [Google Scholar] [CrossRef]
- Padmanabhanunni, A.; Wiid, C. From fear to fortitude: Differential vulnerability to PTSD among South African university students. Traumatology 2022, 28, 167–174. [Google Scholar] [CrossRef]
- Li, J.-B.; Yang, A.; Dou, K.; Wang, L.-X.; Zhang, M.-C.; Lin, X.-Q. Chinese public’s knowledge, perceived severity, and perceived controllability of COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: A national survey. BMC Public Health 2020, 20, 1589. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, M.; Güler, A. Coronavirus anxiety, fear of COVID-19, hope and resilience in healthcare workers: A moderated mediation model study. Health Psychol. Rep. 2021, 9, 388–397. [Google Scholar] [CrossRef] [PubMed]
- Prasetyo, Y.T.; Castillo, A.M.; Salonga, L.J.; Sia, J.A.; Seneta, J.A. Factors affecting perceived effectiveness of COVID-19 prevention measures among Filipinos during Enhanced Community Quarantine in Luzon, Philippines: Integrating Protection Motivation Theory and extended Theory of Planned Behavior. Int. J. Infect. Dis. 2020, 99, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Heppner, P. The problem Solving Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1988. [Google Scholar]
- de la Fuente, A.; Chang, E.C.; Cardeñoso, O.; Chang, O.D. Examining coping strategies used by Spanish female social work students: Evidence for the importance of social problem-solving abilities. Soc. Work Educ. 2019, 38, 314–329. [Google Scholar] [CrossRef]
- Thompson, D.; Bhatt, R.; Watson, K. Physical activity problem-solving inventory for adolescents: Development and initial validation. Pediatr. Exerc. Sci. 2013, 25, 448–467. [Google Scholar] [CrossRef] [PubMed]
- Heppner, P.P.; Witty, T.E.; Dixon, W.A. Problem-Solving Appraisal and Human Adjustment: A Review of 20 Years of Research Using the Problem Solving Inventory. Couns. Psychol. 2004, 32, 344–428. [Google Scholar] [CrossRef]
- Bélanger, C.; Laporte, L.; Sabourin, S.; Wright, J. The Effect of Cognitive-Behavioral Group Marital Therapy on Marital Happiness and Problem Solving Self-Appraisal. Am. J. Fam. Ther. 2015, 43, 103–118. [Google Scholar] [CrossRef]
- Tabancalı, E.; Öngel, G. Examining the Relationship between High School Students’ Lifelong Learning Tendencies and Problem Solving Self-Appraisal. Eur. Educ. Res. 2022, 5, 297–312. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Zsido, A.N.; Teleki, S.A.; Csokasi, K.; Rozsa, S.; Bandi, S.A. Development of the short version of the spielberger state—Trait anxiety inventory. Psychiatry Res. 2020, 291, 113223. [Google Scholar] [CrossRef]
- Makhubela, M. Assessing psychological stress in South African university students: Measurement validity of the perceived stress scale (PSS-10) in diverse populations. Curr. Psychol. 2022, 41, 2802–2809. [Google Scholar] [CrossRef]
- Heppner, P.P.; Petersen, C.H. The development and implications of a personal problem-solving inventory. J. Couns. Psychol. 1982, 29, 66–75. [Google Scholar] [CrossRef]
- Heppner, P.P.; Pretorius, T.B.; Wei, M.; Lee, D.-g.; Wang, Y.-W. Examining the Generalizability of Problem-Solving Appraisal in Black South Africans. J. Couns. Psychol. 2002, 49, 484–498. [Google Scholar] [CrossRef]
- Pretorius, T.B.; Heyns, P.M.; Broekmann, N.C. The effect of a computer-assisted career guidance system on the career development of South African students. S. Afr. J. Psychol. 1991, 21, 119–123. [Google Scholar] [CrossRef]
- Spielberger, C.D. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis; Prentice Hall: Englewood Cliffs, NJ, USA, 2010. [Google Scholar]
- Ashbaugh, A.R.; Houle-Johnson, S.; Herbert, C.; El-Hage, W.; Brunet, A. Psychometric Validation of the English and French Versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). PLoS ONE 2016, 11, e0161645. [Google Scholar] [CrossRef] [PubMed]
- Bridgland, V.M.E.; Moeck, E.K.; Green, D.M.; Swain, T.L.; Nayda, D.M.; Matson, L.A.; Hutchison, N.P.; Takarangi, M.K.T. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 2021, 16, e0240146. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Hu, T.; Hu, B.; Jin, C.; Wang, G.; Xie, C.; Chen, S.; Xu, J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020, 274, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hitchcock, C.; Ellis, A.A.; Williamson, P.; Nixon, R.D.V. The Prospective Role of Cognitive Appraisals and Social Support in Predicting Children’s Posttraumatic Stress. J. Abnorm. Child Psychol. 2015, 43, 1485–1492. [Google Scholar] [CrossRef]
- Kirby, L.D.; Qian, W.; Adiguzel, Z.; Afshar Jahanshahi, A.; Bakracheva, M.; Orejarena Ballestas, M.C.; Cruz, J.F.A.; Dash, A.; Dias, C.; Ferreira, M.J.; et al. Appraisal and coping predict health and well-being during the COVID-19 pandemic: An international approach. Int. J. Psychol. 2022, 57, 49–62. [Google Scholar] [CrossRef]
- Ehlers, A.; Clark, D.M. A cognitive model of posttraumatic stress disorder. Behav. Res. Ther. 2000, 38, 319–345. [Google Scholar] [CrossRef]
- Halligan, S.L.; Michael, T.; Clark, D.M.; Ehlers, A. Posttraumatic Stress Disorder Following Assault: The Role of Cognitive Processing, Trauma Memory, and Appraisals. J. Consult. Clin. Psychol. 2003, 71, 419–431. [Google Scholar] [CrossRef]
- Maren, S.; Holmes, A. Stress and Fear Extinction. Neuropsychopharmacology 2016, 41, 58–79. [Google Scholar] [CrossRef]
- Nagarajan, R.; Krishnamoorthy, Y.; Basavarachar, V.; Dakshinamoorthy, R. Prevalence of post-traumatic stress disorder among survivors of severe COVID-19 infections: A systematic review and meta-analysis. J. Affect. Disord. 2022, 299, 52–59. [Google Scholar] [CrossRef]
- Padmanabhanunni, A. Trauma nation: Exposure to traumatic events among South African university students. J. Community Psychol. 2020, 48, 1853–1862. [Google Scholar] [CrossRef]
- Hoorelbeke, K.; Koster, E.H.W.; Demeyer, I.; Loeys, T.; Vanderhasselt, M.-A. Effects of Cognitive Control Training on the Dynamics of (Mal)Adaptive Emotion Regulation in Daily Life. Emotion 2016, 16, 945–956. [Google Scholar] [CrossRef]
- Conklin, L.R.; Cassiello-Robbins, C.; Brake, C.A.; Sauer-Zavala, S.; Farchione, T.J.; Ciraulo, D.A.; Barlow, D.H. Relationships among adaptive and maladaptive emotion regulation strategies and psychopathology during the treatment of comorbid anxiety and alcohol use disorders. Behav. Res. Ther. 2015, 73, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Nikčević, A.V.; Marino, C.; Kolubinski, D.C.; Leach, D.; Spada, M.M. Modelling the contribution of the Big Five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. J. Affect. Disord. 2021, 279, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Heppner, M.J.; Lee, D.-g.; Paul Heppner, P.; McKinnon, L.C.; Multon, K.D.; Gysbers, N.C. The role of problem-solving appraisal in the process and outcome of career counseling. J. Vocat. Behav. 2004, 65, 217–238. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Amaya, M.; Szalacha, L.A.; Hoying, J.; Taylor, T.; Bowersox, K. Feasibility, Acceptability, and Preliminary Effects of the COPE Online Cognitive-Behavioral Skill-Building Program on Mental Health Outcomes and Academic Performance in Freshmen College Students: A Randomized Controlled Pilot Study. J. Child Adolesc. Psychiatr. Nurs. 2015, 28, 147–154. [Google Scholar] [CrossRef] [PubMed]
- de la Fuente, A.; Chang, E.C.; Cardeñoso, O.; Chang, O.D. The psychological impact of social problem solving under stress in adults: Debased life satisfaction, heightened depressed mood, or both? Personal. Individ. Differ. 2019, 146, 46–52. [Google Scholar] [CrossRef]
| Variables and Indices | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Fear of COVID-19 | |||||||
| 2. Problem-solving appraisal | 0.12 * | ||||||
| 3. Re-experiencing | 0.28 ** | 0.35 ** | |||||
| 4. Avoidance | 0.26 ** | 0.28 ** | 0.66 ** | ||||
| 5. Negative alterations | 0.26 ** | 0.51 ** | 0.12 ** | −0.59 ** | |||
| 6. Hyper-arousal | 00.26 ** | 0.43 ** | 0.67 ** | −0.54 ** | 0.80 ** | ||
| 7. Anxiety | 0.20 ** | 0.48 ** | −0.54 ** | 0.48 ** | 0.65 ** | 0.59 ** | |
| Mean | 17.4 | 97.8 | 9.5 | 4.3 | 13.5 | 11.2 | 12.4 |
| SD | 6.5 | 20.3 | 5.5 | 2.6 | 7.5 | 6.0 | 4.1 |
| Skewness | 0.35 | −0.08 | 0.04 | −0.21 | 0.02 | 0.02 | 0.03 |
| Kurtosis | −0.44 | −0.05 | −0.95 | −1.18 | −1.04 | −0.91 | −0.88 |
| Alpha | 0.87 | 0.89 | 0.89 | 0.89 | 0.88 | 0.82 | 0.88 |
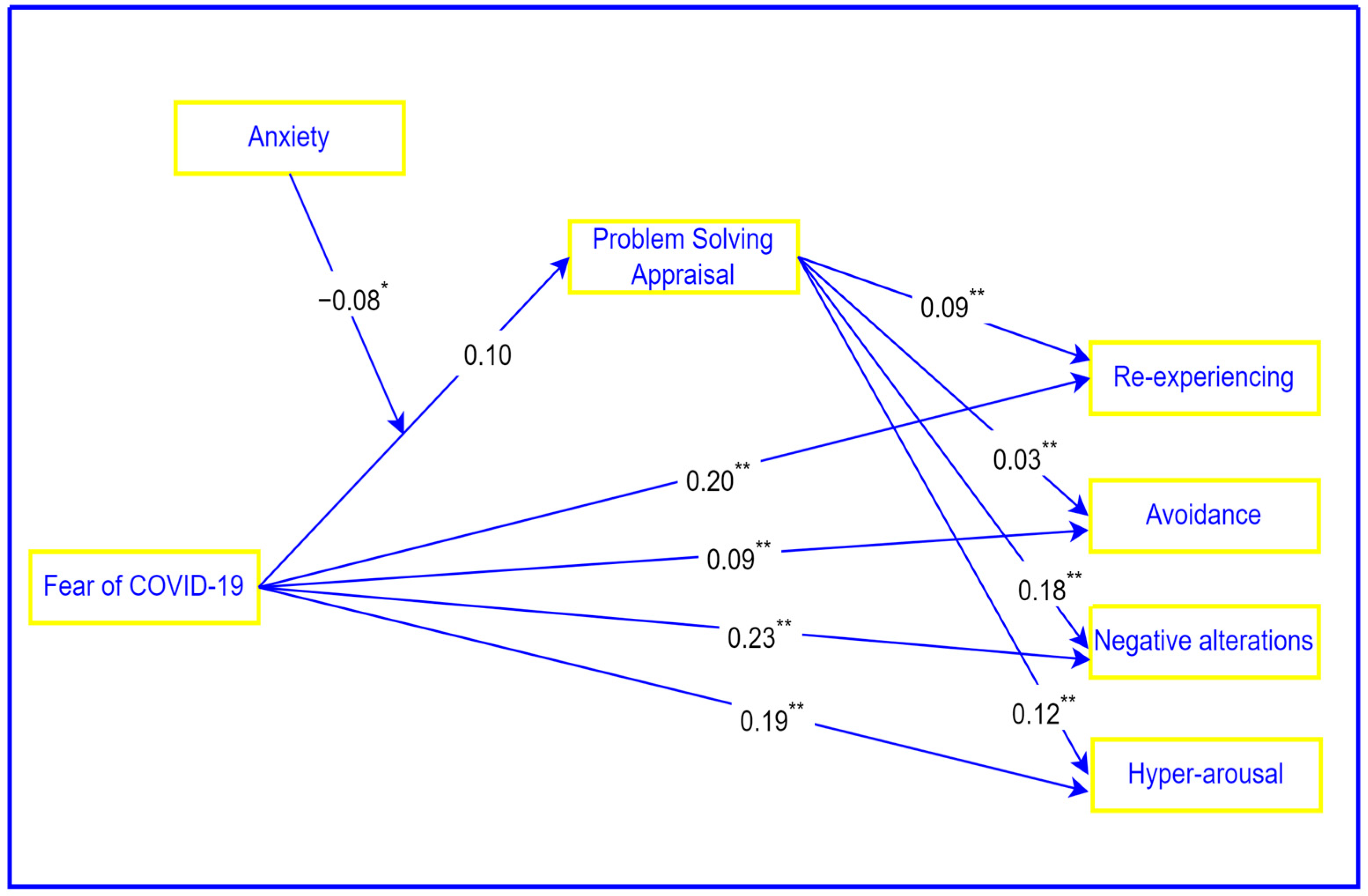
| Effect | Beta | SE | p | 95% CI | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Fear of COVID-19—re-experiencing | 0.20 | 0.04 | 0.000 | 0.12 | 0.29 |
| Fear of COVID-19—avoidance | 0.09 | 0.02 | 0.000 | 0.05 | 0.13 |
| Fear of COVID-19—negative alterations | 0.23 | 0.05 | 0.000 | 0.13 | 0.34 |
| Fear of COVID-19—hyper-arousal | 0.19 | 0.05 | 0.000 | 0.11 | 0.28 |
| Problem-solving appraisal—re-experiencing | 0.09 | 0.01 | 0.000 | 0.06 | 0.11 |
| Problem-solving appraisal—avoidance | 0.03 | 0.01 | 0.000 | 0.02 | 0.05 |
| Problem-solving appraisal—negative alterations | 0.18 | 0.02 | 0.000 | 0.15 | 0.21 |
| Problem-solving appraisal—hyper-arousal | 0.12 | 0.01 | 0.000 | 0.09 | 0.15 |
| Outcome Variable | Index | Bootstrapped SE | Bootstrapped 95% CI | |
|---|---|---|---|---|
| LL | UL | |||
| Re-experiencing | −0.007 | 0.003 | −0.013 | −0.002 |
| Avoidance | −0.003 | 0.001 | −0.005 | −0.001 |
| Negative alterations | −0.015 | 0.006 | −0.026 | −0.003 |
| Hyper-arousal | −0.010 | 0.004 | −0.018 | −0.002 |
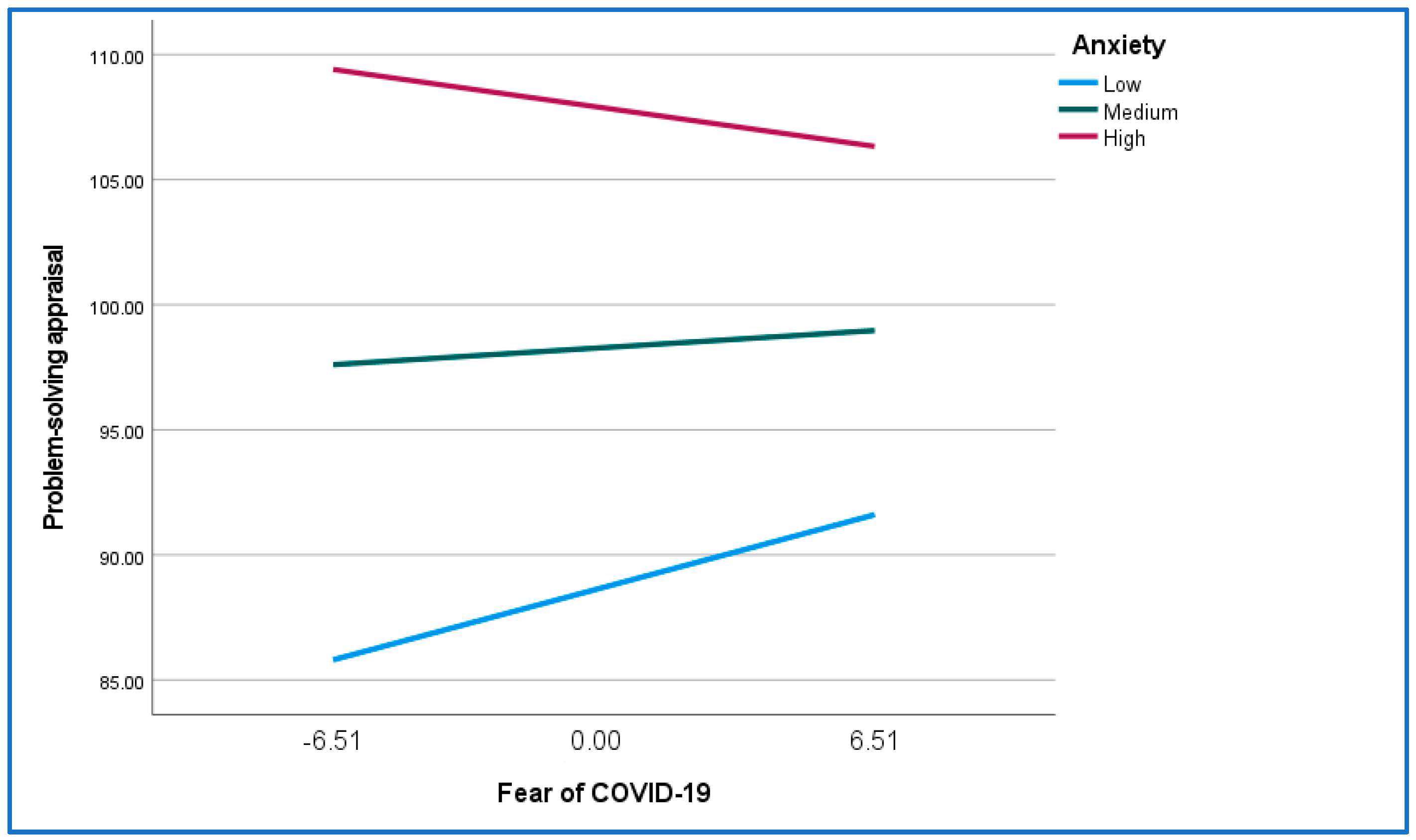
| Anxiety | Effect | SE | 95% Confidence Interval | |
|---|---|---|---|---|
| LL | UL | |||
| Re-experiencing | ||||
| Low anxiety | 0.038 | 0.02 | 0.001 | 0.082 |
| Medium anxiety | 0.009 | 0.01 | −0.012 | 0.040 |
| High anxiety | −0.020 | 0.02 | −0.053 | 0.014 |
| Avoidance | ||||
| Low anxiety | 0.014 | 0.008 | 0.000 | 0.032 |
| Medium anxiety | 0.003 | 0.006 | −0.007 | 0.015 |
| High anxiety | −0.008 | 0.007 | −0.021 | 0.005 |
| Negative alterations | ||||
| Low anxiety | 0.080 | 0.041 | 0.003 | 0.159 |
| Medium anxiety | 0.019 | 0.029 | −0.037 | 0.077 |
| High anxiety | −0.042 | 0.035 | −0.111 | 0.029 |
| Hyper-arousal | ||||
| Low anxiety | 0.054 | 0.028 | −0.001 | 0.112 |
| Medium anxiety | 0.013 | 0.020 | −0.025 | 0.054 |
| High anxiety | −0.028 | 0.023 | −0.075 | 0.019 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Padmanabhanunni, A.; Pretorius, T.B. Fear of COVID-19 and PTSD: The Protective Function of Problem-Solving Appraisals in Mental Health. Int. J. Environ. Res. Public Health 2024, 21, 220. https://doi.org/10.3390/ijerph21020220
Padmanabhanunni A, Pretorius TB. Fear of COVID-19 and PTSD: The Protective Function of Problem-Solving Appraisals in Mental Health. International Journal of Environmental Research and Public Health. 2024; 21(2):220. https://doi.org/10.3390/ijerph21020220
Chicago/Turabian StylePadmanabhanunni, Anita, and Tyrone Brian Pretorius. 2024. "Fear of COVID-19 and PTSD: The Protective Function of Problem-Solving Appraisals in Mental Health" International Journal of Environmental Research and Public Health 21, no. 2: 220. https://doi.org/10.3390/ijerph21020220
APA StylePadmanabhanunni, A., & Pretorius, T. B. (2024). Fear of COVID-19 and PTSD: The Protective Function of Problem-Solving Appraisals in Mental Health. International Journal of Environmental Research and Public Health, 21(2), 220. https://doi.org/10.3390/ijerph21020220






