Abstract
The World Health Organization (WHO) recommends exclusive breastfeeding for the first six months after birth to ensure child health and survival. Antenatal care provides an opportunity to educate pregnant women on optimal breastfeeding practices. A cluster-randomized control trial in Ghana examined the impact of group antenatal care on breastfeeding knowledge and practice. The study enrolled 1761 pregnant women from 14 health facilities in Ghana. The intervention group (n = 877) received eight group sessions, while the control group (n = 884) received individual, routine care. Data were collected at baseline and post intervention. Pearson’s chi-square test was performed to examine categorical data, while odds ratios were calculated using separate logistic regression models to examine differences between the intervention and control groups over time. Women enrolled in group antenatal care had higher odds of following WHO recommendations to exclusively breastfeed for the first six months (odds ratio [OR]: 3.6, 95% confidence interval [95% CI]: 2.1, 6.3) and waiting to introduce solid food until six months of age (OR: 3.1, 95% CI: 1.5, 6.9). Our results found that women who participated in group antenatal care were more likely to follow the recommendations for exclusive breastfeeding developed by the WHO.
1. Background
Antenatal care (ANC) is one of the most utilized preventive maternal healthcare services with an impact on lowering the rates of maternal mortality and morbidity (MMR), along with the reduction in stillbirths and perinatal deaths [1]. The World Health Organization (WHO) outlined a comprehensive global guideline for ANC practice covering various areas, including breastfeeding as a preventive measure for both mother and baby [1]. Proper nutrition is essential for infants to achieve optimal growth and development, and breastfeeding exclusively is considered one of the most cost-effective and convenient ways to ensure child health and survival [2]. WHO and the United Nations International Children’s Emergency Fund (UNICEF) recommend that breastfeeding begin within one hour of birth. Infants should be exclusively breastfed for the first six months (with no other liquids or food, including water) and should additionally continue breastfeeding until two years of age or beyond while also introducing appropriate and safe solid (complementary) foods [3]. According to WHO, breastmilk is safe and clean, requires no preparation, even in environments with poor sanitation and unsafe drinking water, and contains all the essential nutrients and antibodies to protect against childhood illnesses [2]. This makes breastmilk the ideal food for infants for the first six months up to the second year of life [4]. Optimal breastfeeding is the best source of nutrition for the newborn and the cornerstone for establishing healthy growth and development for children [5,6]. It has beneficial effects on a child’s cognitive development, protection against obesity, respiratory tract illnesses, bronchial asthma, type 2 diabetes, cholesterol regulation, and reduction in diarrhea problems [2,7,8,9]. Infants who are not breastfed are 6 to 10 times more likely to die in the early months than those who are exclusively breastfed [10]. Breastfeeding is a potential measure to annually save the lives of 2.7 million from stunting, wasting, overweight, and underweight [10,11]. Undernutrition contributes to 45% of all infant deaths globally [10,11]. The majority of these deaths are accounted for by low- and middle-income countries (LMICs) in the sub-Saharan Africa (SSA) region and southern Asia [2,11], where exclusive breastfeeding (EBF) is practiced sub-optimally, with less than half of infants under 6 months exclusively breastfeeding [2]. Additionally, access to clean water, adequate sanitation, and essential health and social services are often limited in SSA [4,12].
1.1. Antenatal Care and Breastfeeding
Addressing the health and practical benefits and importance of exclusive breastfeeding remains essential for healthcare research and practice. There is mounting evidence that ANC interventions, alone or in combination with intrapartum and postpartum support, can increase breastfeeding initiation, duration, and exclusivity through the provision of adequate information [13,14,15]. Studies have shown that only a fraction of clients receive adequate breastfeeding counseling during pregnancy [16]. Additional studies have identified inappropriate communication [17], lack of knowledge [4,12], outdated health facilities and cultural practices [12], and healthcare provider (HCP) shortage (lack of skilled birth attendants) [18,19] as barriers leading to little time spent on client counseling [20,21], and oversights in providing the required support to mothers for improving breastfeeding practices [22,23].
1.2. Group Antenatal Care and Breastfeeding
Breastfeeding can be challenging, particularly in the first moments after birth. However, having the right policies, programs, and people in place provides a strong support network for mothers. The group antenatal care (GANC) intervention was based on the Health Literacy Skills Framework [24]. An initial feasibility study [25] was conducted using this framework to assess and tailor the implementation of GANC in Ghana. Studies have shown that social and professional support and follow-up improve breastfeeding practices among mothers [26,27,28]. The holistic and patient-centered nature of group antenatal care (GANC) makes it possible to provide comprehensive ANC that can culturally tailor counseling and support toward breastfeeding. Implementing GANC in LMICs is relatively new, with only a handful of studies examining whether GANC affects breastfeeding. This study examines the impact of GANC on breastfeeding knowledge and practices among mothers in Ghana.
2. Method
This study was a cluster-randomized control trial conducted from July 2019 to May 2022 in the Eastern Region of Ghana using 14 matched-pair health facilities in four [4] districts. These facilities provide focused antenatal services to people within the catchment area. The trial was registered with ClinicalTrials.gov on 25 July 2019 (RCT: NCT04033003). The protocol for this trial can be found elsewhere [29].
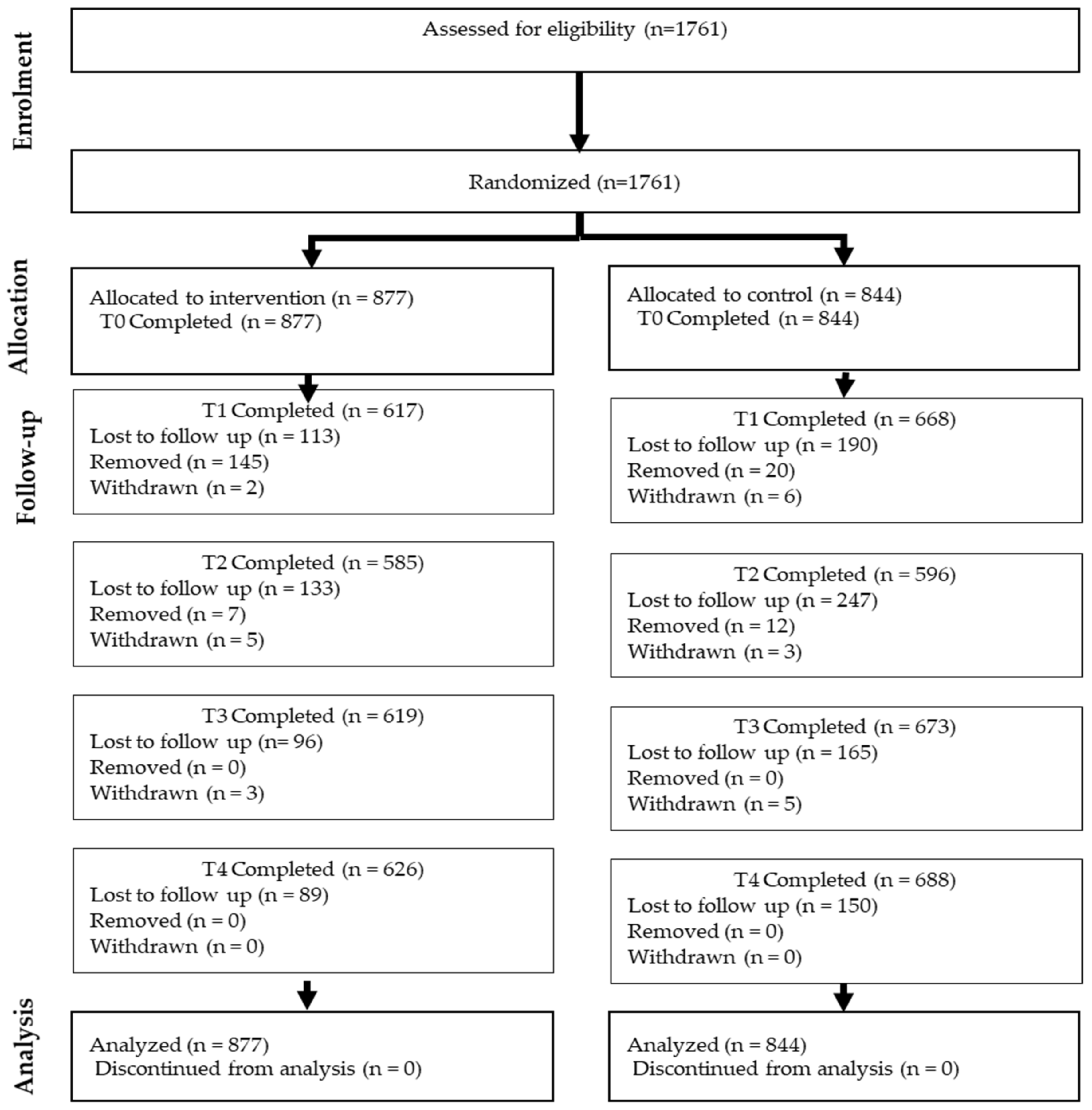
The study setting includes four districts within the Eastern Region of Ghana: Akwapim North, Yilo Krobo, Nswam-Adoagyiri, and Lower Manya Krobo. Intervention and control sites covered distinct catchment communities to prevent the overlap of study participants. The study used purposive sampling to identify pregnant women who enrolled in ANC at the randomized facilities within the selected region of Ghana. Randomization was achieved using a matched-pair method based on the number of deliveries and average gestation at the time of ANC enrollment at each facility. The nbpMatching package from R software (version 1.5.0; R Foundation for Statistical Computing) was used to complete the matching and randomization process [30]. A sample size of about 100 women per facility was calculated at 80% power with an intraclass correlation coefficient of 0.01 [31]. To account for attrition, 120 women per facility were recruited [29]. Pregnant women who attended any of the 14 selected facilities with a gestation of less than 20 weeks, over 15 years old, spoke any of the following languages: English, Ewe, Dangme, Ga, or Akan, and consented to participate in the study were offered the opportunity to participate in the study. A trained research assistant (RA) then provided a detailed explanation of the study and obtained informed consent. Those with high-risk pregnancies requiring specialist care were excluded. Figure 1 shows the flow of participants through the different stages of the study.
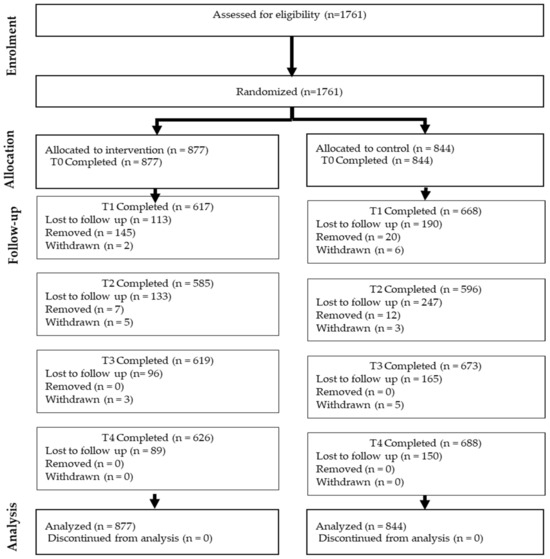
Figure 1.
Flow diagram of the progress through the phases of a parallel randomized trial of two groups (Participants lost to follow-up at T1, T2, or T3 remain eligible to complete surveys at subsequent timepoints.).
2.1. Group Antenatal Care Intervention
The group antenatal care intervention occurred in seven randomized health facilities. A comprehensive individual assessment was conducted at the initial visit, followed by the eight group sessions. The sessions follow the eight contact visits recommended by WHO [1], which is currently practiced in Ghana. Each session lasted approximately 60–90 min. A midwife led the sessions in groups of 12–14 pregnant women. The sessions comprised evidence-based discussions and participatory learning activities tailored to pregnancy, delivery, and postpartum and newborn health, including breastfeeding. All discussions were guided by a validated Facilitator’s Guide for Antenatal Care [25]. Women enrolled in the control groups received individual antenatal care (IANC) per the standard of care for focused antenatal care.
2.2. Data Collection
Research assistants used password-encrypted tablets to collect data from pregnant women at various time points: Time 0: baseline (immediately following the consent process); Time 1: 34 weeks gestation—3 weeks post-delivery; Time 2: 6–12 weeks postpartum; Time 3: 5 to 8 months postpartum; Time 4: 11 to 14 months postpartum. At Times 0 and 1, questions on breastfeeding knowledge and intention were asked.
2.3. Data Analysis
Participants’ baseline demographic data were summarized using descriptive statistics and analyzed using bivariate statistical tests to compare the baseline characteristics of the participants between the GANC intervention and IANC control groups. Two sample t-tests were used to compare age and wealth index, while the Mann–Whitney Wilcoxon test was used to compare the number of previous pregnancies. Chi-squared tests were used to compare categorical data. Logistic regression models adjusted for clustering to test the differences in participants’ knowledge about the appropriate time to start breastfeeding a baby, the age at which to give additional fluids other than breastmilk, and the introduction of solid food between the two groups over time. The potential covariates were the study arms (GANC vs. IANC) and time (T0 vs. T1). Education and parity were also included to control for potential confounding.
3. Results
Table 1, the demographic table, presents the baseline characteristics of the participants. The majority of the participants (56%) were in the 25–34 age group. In terms of education, 10% of the participants and 16% of their partners reported tertiary education. Ninety-three (93%) of the participants were Christians, and 20% of the participants were experiencing their first pregnancy. The demographics were evenly distributed between the two study arms.

Table 1.
Demographic Table.
Table 2 compares the percentage increase in mothers’ knowledge of the appropriate age at which to introduce fluids other than breast milk to infants between the intervention group (GANC) and the control group (IANC). At baseline, the estimated percentage of women choosing 6 months or older to introduce fluids other than breastmilk was similar for the two groups: 81% of the women in IANC and 82.6% in GANC. At Time 1, while this percentage increased for both groups, the percentage rose more sharply in the GANC than the IANC (p < 0.0001). The estimated percentage of participants reporting the ideal time to introduce fluids other than breastmilk at or after 6 months of age increased from 81% to 89% in the IANC and 82% to 97% in the GANC.

Table 2.
Percentage increase in giving fluids and solid food at six months or more by group.
A similar increase was also seen for the age at which mothers began feeding solid food to babies. At baseline, the estimated percentage of women choosing 6 months or older as the appropriate age to start giving babies solid food was about 90% for both groups. At T1, while the percentage rose for both groups, the increase was significantly greater in the GANC, where 98% of the women were estimated to choose 6 months or older, compared to 95% in the IANC (p < 0.0001).
Table 3, the model summary, presents the results of the study with three different outcomes, showing the odds ratios, p-values, and 95% confidence intervals for various factors.

Table 3.
Model Summary.
3.1. Outcome 1: Knowledge on Initiation of Breastfeeding
Overall, no significant differences were seen between the two groups (OR = 1.0, 95% CI = 0.8, 1.3). There is an overall time effect where the initiation of breastfeeding was significantly lower at T1 compared to T0 (OR: 0.75, 95%: 0.7, 0.9), suggesting that women in GANC have the highest likelihood of initiating breastfeeding early. Tertiary-educated women had the highest probability of initiating breastfeeding within 30 min of delivery compared to less-educated women. The odds of early breastfeeding initiation are significantly lower for primary education (OR: 0.55, 95% CI: 0.37, 0.81), junior high (OR: 0.59, 95% CI: 0.42, 0.84), and secondary education (OR: 0.58, 95% CI: 0.4, 0.83).
3.2. Outcome 2: Best Time to Start Giving Fluids Other than Breastmilk
Mothers enrolled in GANC had greater odds of reporting exclusive breastfeeding as compared to IANC over time (p-value ≤ 0.0001). They reported the introduction of fluids other than breastmilk at 6 months or later (OR: 3.6, 95% CI: 2.1, 6.3). The results also found a significant effect due to parity and education. First-time mothers were more likely to introduce fluids before the recommended six months (OR: 0.52, 95% CI: 0.4, 0.7). In terms of education, women reporting a tertiary education had the highest likelihood of waiting to give baby fluids until 6 months or later compared to those with lower education such as primary (OR: 0.32, 95% CI: 0.2, 0.6), junior high (OR: 0.35, 95% CI: 0.2, 0.6), and secondary education (OR: 0.47, 95% I: 0.3, 0.8).
3.3. Outcome 3: Best Time to Start Giving Solid Food to Babies
Over time, mothers enrolled in GANC had greater odds of giving solids to babies at 6 months or later compared to IANC (p-value = 0.003). In addition, the odds of opting to introduce solids at or after 6 months are lower among first-time mothers (OR: 0.69, 95% CI: 0.4, 0.9). Also, women with tertiary education had higher odds of waiting until at least 6 months of age to introduce solid foods than women with less education: primary (OR: 0.14, 95% CI: 0.1, 0.4); junior high (OR: 0.18, 95% CI: 0.1, 0.5); secondary (OR: 0.3, 95% CI: 0.1, 0.8).
4. Discussion
The current study examined the impact of GANC on breastfeeding knowledge and practices among mothers in Ghana. Group antenatal care is an innovative approach to care with reports of higher patient and provider satisfaction rates and lower maternal and infant mortality and morbidity rates [1,32,33,34,35]. Mothers’ knowledge and practices play key roles in the process of breastfeeding [36]. Breastfeeding is a critical practice that is part of a complex intervention for improving maternal and infant health but lacks evidence regarding the effects of group care interventions [37]. Behavioral change interventions such as GANC have shown to be effective in increasing breastfeeding knowledge, leading to better practice behaviors [38]. Breastfeeding interventions delivered in combination with health services and group contexts double exclusive breastfeeding practice [39].
Our study results reveal that GANC improved optimal timing for introducing fluids and complementary foods. This indicates that apart from the statistical significance, this result is a clinically important finding that aligns with the WHO recommendation of exclusively breastfeeding for the first six months without other liquids or food, including water [2]. Compelling data indicates that breastfeeding protects against pneumonia and diarrhea, the primary causes of infant mortality [6,40], leading to approximately 50% reduction in diarrheal episodes and 33% of respiratory illnesses [4].
Studies have shown that women receiving individualized antenatal care have poor breastfeeding knowledge and practices compared to GANC [20,21]. Factors contributing to these issues include inadequate breastfeeding counseling during pregnancy [16], ineffective communication and support [17], outdated health facilities and cultural practices [12], and healthcare provider (HCP) shortage (lack of skilled birth attendants) usually leading to little time spent on client counseling [18,19]. Breastfeeding education and counseling through GANC have been associated with increased breastfeeding knowledge [41,42]. The support provided and garnered from GANC increases rates and improves breastfeeding practices among mothers [43]. These findings emphasize that knowledge and support from GANC increase: (1) the mother’s psychological well-being, self-confidence, motivation, intention, competence, and autonomy to breastfeed exclusively [42,44,45,46]; (2) timely initiation and exclusive breastfeeding [47,48,49]; (3) higher breastfeeding rates [50,51]; and (4) breastfeeding sustenance up to two years [52]. Improving breastfeeding knowledge not only helps to achieve better infant health [41] but also leads to cost savings (reduction in health expenditure) due to fewer infections and diseases caused by poor breastfeeding practices [53] and reduced costs in purchasing baby foods [54,55].
While our study identified positive relationships between higher levels of education and multiparity to better breastfeeding knowledge, other studies have reported that mothers have several reasons for engaging in various breastfeeding behaviors: facility delivery [56], good health status [5], vaginal delivery [26,56], partner knowledge [56], and employment status [5,26,28,56,57] reflect other reasons that facilitate exclusive breastfeeding among mothers. Some major barriers to exclusive breastfeeding, such as poor knowledge (mostly related to myths and misconceptions) [27,57], lack or improper counseling by healthcare providers [21], and lack of a partner, family, or professional support [27], were comprehensively addressed by the broad scope and impact of GANC [42,44,46,47,48,49]. This underscores the importance of using effective intervention service delivery techniques, such as GANC, to intensify counseling and support and address the diversity and complexities around maternal breastfeeding behavior for improving child health and survival.
Strengths and Limitations
Participants were not blinded to the study. However, facilities within each matched pair randomized to either intervention or control were far apart, preventing any possibility of contamination. Participant selection was purposive at the study sites; however, randomization was implemented at the facility level to address potential issues related to generalization. Participant follow-up for this study ended at fourteen months. Additional data will be needed to assess the long-term adherence to continued breastfeeding at two years and its effects on maternal and newborn health outcomes.
The cluster-randomized design has many strengths, including evaluating effectiveness under conditions of actual use and the possibility of generalizing results to clinical practices similar to those in this trial. This design maintains the rigor and internal validity of an RCT while enhancing external validity through essential methodological features.
5. Conclusions
Group antenatal care has the potential to be a significant intervention in promoting better breastfeeding practices. Tackling maternal and infant health issues is complex for low-resourced areas. The provision of GANC is one strategy for managing the complexities around maternal healthcare and improving the health and well-being of mothers and their children. Future research should continue to explore the long-term effects of GANC on breastfeeding practices and maternal–infant health, as well as identify the most effective components of the program to further enhance its impact. Findings from our study can support policymakers and stakeholders in the SSA region to consider the implementation of GANC to improve maternal health and improve practices such as breastfeeding.
Author Contributions
T.N.L. contributed to the drafting and substantial revisions of the manuscript. J.W. contributed to the conception and design of the trial and manuscript revisions. B.G. contributed to the data analysis, interpretation drafting, and substantial manuscript revisions. V.A.K., V.E.A.A., R.Z. and E.A. contributed to the data acquisition, interpretation, manuscript conception, and substantial revisions. C.M. contributed to the manuscript’s conception, design, interpretation, and substantial revisions. J.R.L. contributed to the conception, design, data interpretation, drafting, and substantial manuscript revisions. All authors have read and agreed to the published version of the manuscript.
Funding
The National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (RO1HD096277) funded this study.
Institutional Review Board Statement
Ethical approval was received from the Institutional Review Boards of the University of Michigan (HUM#00161464) and the Ghana Health Service Ethical Review Committee (GHS-ERC: 016/04/19).
Informed Consent Statement
All study participants signed or thumb-printed an informed consent form for inclusion before participation. Anonymity was maintained, as participants were not obliged to provide personal information.
Data Availability Statement
Data are available in the Deep Blue repository of the University of Michigan at https://deepblue.lib.umich.edu/data (accessed on 27 November 2024).
Acknowledgments
The authors acknowledge the efforts and contributions of participants, research assistants, and everyone involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- WHO. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience; World Health Organization: Geneva, Switzerland, 2016; Available online: https://apps.who.int/iris/bitstream/handle/10665/250796/97892415?sequence=1 (accessed on 28 October 2023).
- WHO. Breastfeeding. 2024. Available online: https://www.who.int/health-topics/breastfeeding (accessed on 12 May 2024).
- WHO; UNICEF. Ten Steps to Successful Breastfeeding. 2018. Available online: https://www.who.int/teams/nutrition-and-food-safety/food-and-nutrition-actions-in-health-systems/ten-steps-to-successful-breastfeeding (accessed on 12 May 2024).
- UNICEF. From the First Hour of Life|UNICEF. 2016. Available online: https://www.unicef.org/reports/first-hour-life (accessed on 11 May 2024).
- Admasu, M.A.; Cione, E. Breastfeeding knowledge, attitude, and practice and related determinants among maternal in Gondar, Ethiopia: Cross-sectional study. Int. J. Nutr. Food Sci. 2016, 5, 25. [Google Scholar] [CrossRef][Green Version]
- Ogbo, F.A.; Agho, K.; Ogeleka, P.; Woolfenden, S.; Page, A.; Eastwood, J.; Global Child Health Research Interest Group. Infant feeding practices and diarrhoea in sub-Saharan African countries with high diarrhoea mortality. PLoS ONE 2017, 12, e0171792. [Google Scholar] [CrossRef] [PubMed]
- Couto, G.R.; Dias, V.; de Jesus Oliveira, J. Benefits of Exclusive Breastfeeding: An Integrative Review. Nurs. Pract. Today 2020, 7, 245–254. Available online: https://publish.kne-publishing.com/index.php/NPT/article/view/4034 (accessed on 12 May 2024).
- North, K.; Gao, M.; Allen, G.; Lee, A.C. Breastfeeding in a Global Context: Epidemiology, Impact, and Future Directions. Clin. Ther. 2022, 44, 228–244. [Google Scholar] [CrossRef] [PubMed]
- Picó, C.; Palou, M.; Pomar, C.A.; Palou, A. Chapter 2—Benefits of breastfeeding in infant health: A role for milk signaling peptides. In Molecular Nutrition: Mother and Infant; Vinciguerra, M., Sanchez, P.C., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 29–56. Available online: https://www.sciencedirect.com/science/article/pii/B9780128138625000025 (accessed on 12 May 2024).
- WHO. Infant and Young Child Feeding. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding (accessed on 12 May 2024).
- UNICEF; WHO; WB. The UNICEF/WHO/WB Joint Child Malnutrition Estimates (JME) Group Released New Data for 2021. 2021. Available online: https://www.who.int/news/item/06-05-2021-the-unicef-who-wb-joint-child-malnutrition-estimates-group-released-new-data-for-2021 (accessed on 12 May 2024).
- UNICEF. Capture the Moment|UNICEF. 2018. Available online: https://www.unicef.org/reports/capture-moment (accessed on 11 May 2024).
- Habtewold, T.D.; Sharew, N.T.; Alemu, S.M. Evidence on the effect of gender of newborn, antenatal care and postnatal care on breastfeeding practices in Ethiopia: A meta-analysis andmeta-regression analysis of observational studies. BMJ Open 2019, 9, e023956. [Google Scholar] [CrossRef] [PubMed]
- Lassi, Z.S.; Rind, F.; Irfan, O.; Hadi, R.; Das, J.K.; Bhutta, Z.A. Impact of Infant and Young Child Feeding (IYCF) Nutrition Interventions on Breastfeeding Practices, Growth and Mortality in Low- and Middle-Income Countries: Systematic Review. Nutrients 2020, 12, 722. [Google Scholar] [CrossRef]
- Wouk, K.; Tully, K.P.; Labbok, M.H. Systematic Review of Evidence for Baby-Friendly Hospital Initiative Step 3: Prenatal Breastfeeding Education. J. Hum. Lact. 2017, 33, 50–82. [Google Scholar] [CrossRef]
- Mallick, L.; Benedict, R.K.; Wang, W. Facility readiness and counseling during antenatal care and the relationship with early breastfeeding in Haiti and Malawi. BMC Pregnancy Childbirth 2020, 20, 325. [Google Scholar] [CrossRef]
- Patil, D.S.; Pundir, P.; Dhyani, V.S.; Krishnan, J.B.; Parsekar, S.S.; D’Souza, S.M.; Ravishankar, N.; Renjith, V. A mixed-methods systematic review on barriers to exclusive breastfeeding. Nutr. Health 2020, 26, 323–346. [Google Scholar] [CrossRef]
- UN. Global Multidimensional Poverty Index 2019: Illuminating Inequalities. 2019. Available online: https://ora.ox.ac.uk/objects/uuid:f0b62a48-e028-473a-9c86-44822ba46427 (accessed on 11 May 2024).
- WHO. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: Executive Summary. 2019. Available online: https://iris.who.int/handle/10665/327596 (accessed on 13 June 2024).
- Phillips, E.; Stoltzfus, R.J.; Michaud, L.; Pierre, G.L.F.; Vermeylen, F.; Pelletier, D. Do mobile clinics provide high-quality antenatal care? A comparison of care delivery, knowledge outcomes and perception of quality of care between fixed and mobile clinics in central Haiti. BMC Pregnancy Childbirth 2017, 17, 361. [Google Scholar] [CrossRef]
- Rurangirwa, A.A.; Mogren, I.; Ntaganira, J.; Govender, K.; Krantz, G. Quality of antenatal care services in Rwanda: Assessing practices of health care providers. BMC Health Serv. Res. 2018, 18, 865. [Google Scholar] [CrossRef]
- Magoma, M.; Requejo, J.; Merialdi, M.; Campbell, O.M.; Cousens, S.; Filippi, V. How much time is available for antenatal care consultations? Assessment of the quality of care in rural Tanzania. BMC Pregnancy Childbirth 2011, 11, 64. [Google Scholar] [CrossRef] [PubMed]
- von Both, C.; Fleβa, S.; Makuwani, A.; Mpembeni, R.; Jahn, A. How much time do health services spend on antenatal care? Implications for the introduction of the focused antenatal care model in Tanzania. BMC Pregnancy Childbirth 2006, 6, 22. [Google Scholar] [CrossRef] [PubMed]
- Squiers, L.; Peinado, S.; Berkman, N.; Boudewyns, V.; McCormack, L. The Health Literacy Skills Framework. J. Health Commun. 2012, 17 (Suppl. 3), 30–54. [Google Scholar] [CrossRef]
- Lori, J.R.; Munro, M.L.; Chuey, M.R. Use of a facilitated discussion model for antenatal care to improve communication. Int. J. Nurs. Stud. 2016, 54, 84–94. [Google Scholar] [CrossRef]
- Awoke, N.; Tekalign, T.; Lemma, T. Predictors of optimal breastfeeding practices in Worabe town, Silte zone, South Ethiopia. PLoS ONE 2020, 15, e0232316. [Google Scholar] [CrossRef] [PubMed]
- Dukuzumuremyi, J.P.C.; Acheampong, K.; Abesig, J.; Luo, J. Knowledge, attitude, and practice of exclusive breastfeeding among mothers in East Africa: A systematic review. Int. Breastfeed J. 2020, 15, 70. [Google Scholar] [CrossRef]
- Ejie, I.L.; Eleje, G.U.; Chibuzor, M.T.; Anetoh, M.U.; Nduka, I.J.; Umeh, I.B.; Ogbonna, B.O.; Ekwunife, O.I. A systematic review of qualitative research on barriers and facilitators to exclusive breastfeeding practice in sub-Saharan African countries. Int. Breastfeed J. 2021, 16, 44. [Google Scholar] [CrossRef] [PubMed]
- Lori, J.R.; Williams, J.E.; Kukula, V.A.; Apetorgbor, V.E.; Awini, E.A.; Amankwah, G.; Zielinski, R.; Lockhart, N.; James, K.H.; Moyer, C.A. Group Antenatal Care in Ghana: Protocol for a Cluster Randomized Controlled Trial. JMIR Res. Protoc. 2022, 11, e40828. [Google Scholar] [CrossRef]
- Beck, C.; Lu, B.; Greevy, R. nbpMatching: Functions for Optimal Non-Bipartite Matching. 2024. Available online: https://cran.r-project.org/web/packages/nbpMatching/ (accessed on 19 November 2024).
- Rotondi, M.; Donner, A. Sample size estimation in cluster randomized trials: An evidence-based perspective. Comput. Stat. Data Anal. 2012, 56, 1174–1187. [Google Scholar] [CrossRef]
- AWHONN. Respectful Maternity Care Framework and Evidence-Based Clinical Practice Guideline. J. Obstet. Gynecol. Neonatal Nurs. 2022, 51, e3–e54. [Google Scholar] [CrossRef]
- WHO. The Prevention and Elimination of Disrespect and Abuse During Facility-Based Childbirth; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- WHO. WHO Recommendations on Intrapartum Care for a Positive Childbirth Experience; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- WHO. Strategies Towards Ending Preventable Maternal Mortality (EPMM); World Health Organization: Geneva, Switzerland, 2021; 44p, Available online: https://iris.who.int/handle/10665/153544 (accessed on 2 October 2023).
- Hamze, L.; Mao, J.; Reifsnider, E. Knowledge and attitudes towards breastfeeding practices: A cross-sectional survey of postnatal mothers in China. Midwifery 2019, 74, 68–75. [Google Scholar] [CrossRef]
- McFadden, A.; Siebelt, L.; Marshall, J.L.; Gavine, A.; Girard, L.C.; Symon, A.; MacGillivray, S. Counselling interventions to enable women to initiate and continue breastfeeding: A systematic review and meta-analysis. Int. Breastfeed J. 2019, 14, 42. [Google Scholar] [CrossRef] [PubMed]
- Sudarmi; Rumintang, B.I.; Anggraeni, N.P.D.A.; Halimatussyaadiah, S. Integrated antenatal care services with breastfeeding counseling practices to improve pregnant women’s knowledge, skills and readiness for exclusive breastfeeding. Bali Med. J. 2023, 12, 1147–1151. [Google Scholar] [CrossRef]
- Olufunlayo, T.F.; Roberts, A.A.; MacArthur, C.; Thomas, N.; Odeyemi, K.A.; Price, M.; Jolly, K. Improving exclusive breastfeeding in low and middle-income countries: A systematic review. Matern. Child Nutr. 2019, 15, e12788. [Google Scholar] [CrossRef]
- Troeger, C.; Blacker, B.F.; Khalil, I.A.; Rao, P.C.; Cao, S.; Zimsen, S.R.; Albertson, S.B.; Deshpande, A.; Farag, T.; Abebe, Z.; et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1211–1228. [Google Scholar] [CrossRef] [PubMed]
- Auger, S.J.; Verbiest, S.; Spickard, J.V.; Simán, F.M.; Colindres, M. Participatory group prenatal education using photonovels: Evaluation of a lay health educator model with low-income Latinas. J. Particip. Med. 2015, 7, e13. [Google Scholar] [PubMed]
- Risisky, D.; Chan, R.L.; Zigmont, V.A.; Asghar, S.M.; DeGennaro, N. Examining Delivery Method and Infant Feeding Intentions between Women in Traditional and Non-Traditional Prenatal Care. Matern. Child Health J. 2018, 22, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Andersson, E.; Christensson, K.; Hildingsson, I. Mothers’ satisfaction with group antenatal care versus individual antenatal care—A clinical trial. Sex Reprod. Healthc. 2013, 4, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Gray, H.L.; Rancourt, D.; Masho, S.; Stern, M. Comparing Group Versus Individual Prenatal Care on Breastfeeding Practice and Motivational Factors. J. Perinat. Neonatal Nurs. 2024, 38, 385–393. [Google Scholar] [CrossRef]
- Lori, J.R.; Chuey, M.; Munro-Kramer, M.L.; Ofosu-Darkwah, H.; Adanu, R.M.K. Increasing postpartum family planning uptake through group antenatal care: A longitudinal prospective cohort design. Reprod. Health 2018, 15, 208. [Google Scholar] [CrossRef]
- Trotman, G.; Chhatre, G.; Darolia, R.; Tefera, E.; Damle, L.; Gomez-Lobo, V. The Effect of Centering Pregnancy versus Traditional Prenatal Care Models on Improved Adolescent Health Behaviors in the Perinatal Period. J. Pediatr. Adolesc. Gynecol. 2015, 28, 395–401. [Google Scholar] [CrossRef]
- Picklesimer, A.; Heberlein, E.; Covington-Kolb, S. Group prenatal care: Has its time come? Clin. Obstet. Gynecol. 2015, 58, 380–391. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.; Garnier-Villarreal, M.; Hanson, L. Effectiveness of CenteringPregnancy on Breastfeeding Initiation Among African Americans: A Systematic Review and Meta-analysis. J. Perinat. Neonatal Nurs. 2018, 32, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Sheeder, J.; Weber Yorga, K.; Kabir-Greher, K. A Review of Prenatal Group Care Literature: The Need for a Structured Theoretical Framework and Systematic Evaluation. Matern. Child Health J. 2012, 16, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Chapman, D.J.; Pérez-Escamilla, R. Breastfeeding among minority women: Moving from risk factors to interventions. Adv. Nutr. 2012, 3, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Nicolau, P.; Rodriguez, S.; Maso, P.; Agramunt, S.; Garcia, E.; Sala, A.; Vernet-Tomas, M.; Paya, A. Impact of Group Prenatal Care Support on Breastfeeding Initiation Rates and Other Maternal and Perinatal Outcomes. Obstet. Gynecol. Res. 2018, 1, 38–44. [Google Scholar] [CrossRef]
- Tanner-Smith, E.E.; Steinka-Fry, K.T.; Lipsey, M.W. Effects of CenteringPregnancy group prenatal care on breastfeeding outcomes. J. Midwifery Womens Health 2013, 58, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Jans, S.; Westra, X.; Crone, M.; van den Akker-van, M.E.; Rijnders, M. Long-term cost savings with Centering-based group antenatal care. Midwifery 2023, 126, 103829. [Google Scholar] [CrossRef]
- Hampson, G.; Roberts, S.L.E.; Lucas, A.; Parkin, D. An economic analysis of human milk supplementation for very low birth weight babies in the USA. BMC Pediatr. 2019, 19, 337. [Google Scholar] [CrossRef]
- Zanganeh, M.; Jordan, M.; Mistry, H. A systematic review of economic evaluations for donor human milk versus standard feeding in infants. Matern. Child Nutr. 2021, 17, e13151. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K.Y.; Page, A.; Arora, A.; Ogbo, F.A. Trends and determinants of early initiation of breastfeeding and exclusive breastfeeding in Ethiopia from 2000 to 2016. Int. Breastfeed J. 2019, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Patil, C.L.; Klima, C.S.; Steffen, A.D.; Leshabari, S.C.; Pauls, H.; Norr, K.F. Implementation challenges and outcomes of a randomized controlled pilot study of a group prenatal care model in Malawi and Tanzania. Int. J. Gynaecol. Obstet. 2017, 139, 290–296. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).