Pregnancy Desirability and Motivational Readiness for Postpartum Contraceptive Use: Findings from Population-Based Surveys in Eight Sub-Saharan African Countries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data
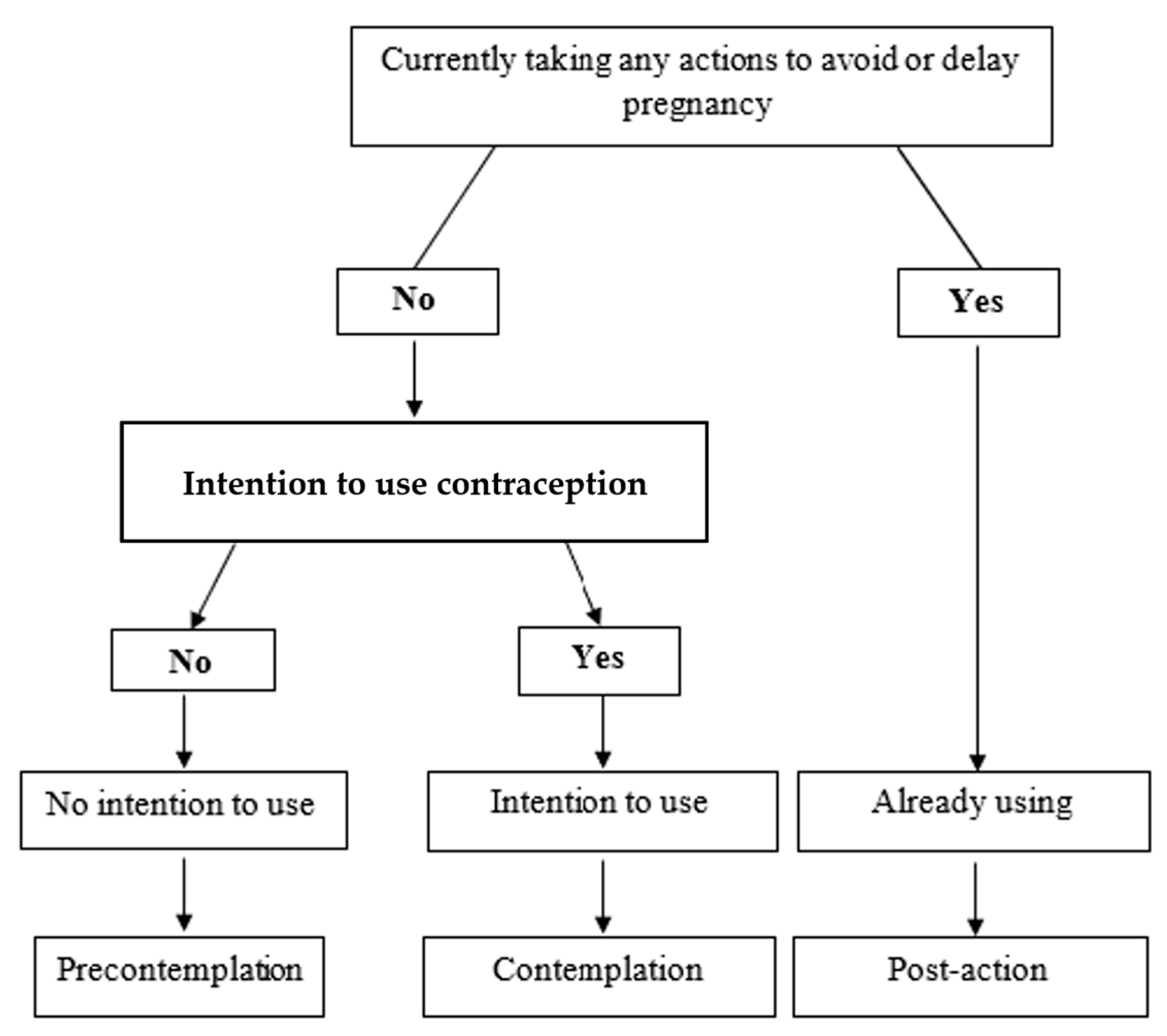
2.2. Outcome Variable
2.3. Exposure Variable
2.4. Covariates
2.5. Analytic Sample
2.6. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Factors Associated with Motivational Readiness for Postpartum Contraceptive Use
3.3. Multinomial Regression Analyses
4. Discussion
4.1. Main Findings and Comparison with Existing Literature
4.2. Strengths and Limitations
4.3. Implications for Public Health
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ESHRE. Why after 50 years of effective contraception do we still have unintended pregnancy? A European perspective. Hum. Reprod. 2018, 33, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Swiatlo, A.; Curtis, S.; Gottfredson, N.; Halpern, C.; Tumlinson, K.; Lich, K.H. Contraceptive Behavior Dynamics and Unintended Pregnancy: A Latent Transition Analysis. Demography 2023, 60, 1089–1113. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, L.A.; Sarnak, D.O.; Karp, C.; Wood, S.N.; Moreau, C.; Kibira, S.P.S.; Makumbi, F. Family Planning Beliefs and Their Association with Contraceptive Use Dynamics: Results from a Longitudinal Study in Uganda. Stud. Fam. Plan. 2021, 52, 241–258. [Google Scholar] [CrossRef]
- Blondel, B.; Beuzelin, M.; Bonnet, C.; Moreau, C. Pregnancy intention and preconception contraceptive behaviors and substandard prenatal care in France. J. Gynecol. Obstet. Hum. Reprod. 2023, 52, 102608. [Google Scholar] [CrossRef] [PubMed]
- Santelli, J.; Rochat, R.; Hatfield-Timajchy, K.; Gilbert, B.C.; Curtis, K.; Cabral, R.; Hirsch, J.S.; Schieve, L. The measurement and meaning of unintended pregnancy. Perspect. Sex. Reprod. Health 2003, 35, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Cleland, J.; Ali, M.M. Reproductive consequences of contraceptive failure in 19 developing countries. Obstet. Gynecol. 2004, 104, 314–320. [Google Scholar] [CrossRef]
- Bearak, J.; Popinchalk, A.; Ganatra, B.; Moller, A.-B.; Tunçalp, Ö.; Beavin, C.; Kwok, L.; Alkema, L. Unintended pregnancy and abortion by income, region, and the legal status of abortion: Estimates from a comprehensive model for 1990–2019. Lancet Glob. Health 2020, 8, e1152–e1161. [Google Scholar] [CrossRef]
- Gipson, J.D.; Muntifering, C.J.; Chauwa, F.K.; Taulo, F.; Tsui, A.O.; Hindin, M.J. Assessing the importance of gender roles in couples’ home-based sexual health services in Malawi. Afr. J. Reprod. Health 2010, 14, 61–71. [Google Scholar]
- Cheng, D.; Schwarz, E.B.; Douglas, E.; Horon, I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception 2009, 79, 194–198. [Google Scholar] [CrossRef]
- Jang, M.; Molino, A.R.; Ribeiro, M.V.; Mariano, M.; Martins, S.S.; Caetano, S.C.; Surkan, P.J. Maternal Pregnancy Intention and Developmental Outcomes in Brazilian Preschool-Aged Children. J. Dev. Behav. Pediatr. 2021, 42, e15–e23. [Google Scholar] [CrossRef]
- Wildsmith, E.; Guzzo, K.B.; Hayford, S.R. Repeat unintended, unwanted and seriously mistimed childbearing in the United States. Perspect. Sex Reprod. Health 2010, 42, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Okonofua, F. Abortion and maternal mortality in the developing world. J. Obstet. Gynaecol. Can. 2006, 28, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Bearak, J.M.; Popinchalk, A.; Beavin, C.; Ganatra, B.; Moller, A.-B.; Tunçalp, Ö.; Alkema, L. Country-specific estimates of unintended pregnancy and abortion incidence: A global comparative analysis of levels in 2015–2019. BMJ Glob. Health 2022, 7, e007151. [Google Scholar] [CrossRef] [PubMed]
- Molla, W.; Hailemariam, S.; Mengistu, N.; Madoro, D.; Bayisa, Y.; Tilahun, R.; Wudneh, A.; Ayele, G.M. Unintended pregnancy and associated factors during COVID-19 pandemic in Ethiopia: Community-based cross-sectional study. Women’s Health 2022, 18, 17455057221118170. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, S.; Clark, G.L.; McGill, S.; Cuñado, J. The effect of past health events on intentions to purchase insurance: Evidence from 11 countries. J. Econ. Psychol. 2019, 74, 102204. [Google Scholar] [CrossRef]
- Weinstein, N.D. Effects of personal experience on self-protective behavior. Psychol. Bull. 1989, 105, 31–50. [Google Scholar] [CrossRef] [PubMed]
- Millstein, S.G.; Halpern-Felsher, B.L. Perceptions of risk and vulnerability. J. Adolesc. Health 2002, 31, 10–27. [Google Scholar] [CrossRef]
- Batyra, E. Contraceptive use behavior change after an unintended birth in Colombia and Peru. Int. Perspect. Sex. Reprod. Health 2020, 46, 9–19. [Google Scholar] [CrossRef]
- Khan, M.N.; Harris, M.; Loxton, D. Modern contraceptive use following an unplanned birth in Bangladesh: An analysis of national survey data. Int. Perspect. Sex. Reprod. Health 2020, 46, 77–87. [Google Scholar] [CrossRef]
- Fotso, J.C.; Izugbara, C.; Saliku, T.; Ochako, R. Unintended pregnancy and subsequent use of modern contraceptive among slum and non-slum women in Nairobi, Kenya. BMC Pregnancy Childbirth 2014, 14, 224. [Google Scholar] [CrossRef]
- Bakibinga, P.; Matanda, D.J.; Ayiko, R.; Rujumba, J.; Muiruri, C.; Amendah, D.; Atela, M. Pregnancy history and current use of contraception among women of reproductive age in Burundi, Kenya, Rwanda, Tanzania and Uganda: Analysis of demographic and health survey data. BMJ Open 2016, 6, e009991. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, L.A.; Karp, C.; Magalona, S.; Shiferaw, S.; Seme, A.; Ahmed, S. Exploring Multiple Measures of Pregnancy Preferences and Their Relationship with Postpartum Contraceptive Uptake Using Longitudinal Data from PMA Ethiopia. Stud. Fam. Plan. 2023, 54, 467–486. [Google Scholar] [CrossRef] [PubMed]
- Boydell, V.; Galavotti, C. Getting Intentional about Intention to Use: A Scoping Review of Person-Centered Measures of Demand. Stud. Fam. Plan. 2022, 53, 61–132. [Google Scholar] [CrossRef] [PubMed]
- Tsui, A.O.; McDonald-Mosley, R.; Burke, A.E. Family Planning and the Burden of Unintended Pregnancies. Epidemiol. Rev. 2010, 32, 152–174. [Google Scholar] [CrossRef] [PubMed]
- Kruglanski, A.W.; Chernikova, M.; Rosenzweig, E.; Kopetz, C. On motivational readiness. Psychol. Rev. 2014, 121, 367. [Google Scholar] [CrossRef] [PubMed]
- Norcross; Krebs, P.M.; Prochaska, J.O. Stages of change. J. Clin. Psychol. 2011, 67, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Woo, M.C.; Ferrara, G.; Puerto-Torres, M.; Gillipelli, S.R.; Elish, P.; Muniz-Talavera, H.; Gonzalez-Ruiz, A.; Armenta, M.; Barra, C.; Diaz-Coronado, R. Stages of change: Strategies to promote use of a Pediatric Early Warning System in resource-limited pediatric oncology centers. Cancer Med. 2023, 12, 15358–15370. [Google Scholar] [CrossRef]
- Buchmann, M.; Jordan, S.; Loer, A.M.; Finger, J.D.; Domanska, O.M. Motivational readiness for physical activity and health literacy: Results of a cross-sectional survey of the adult population in Germany. BMC Public Health 2023, 23, 331. [Google Scholar] [CrossRef]
- Martinasek, M.; Tamulevicius, N.; Gibson-Young, L.; McDaniel, J.; Moss, S.J.; Pfeffer, I.; Lipski, B. Predictors of Vaping Behavior Change in Young Adults Using the Transtheoretical Model: A Multi-Country Study. Tob. Use Insights 2021, 14, 1179173x20988672. [Google Scholar] [CrossRef]
- Ha, B.T.T.; Jayasuriya, R.; Owen, N. Increasing male involvement in family planning decision making: Trial of a social-cognitive intervention in rural Vietnam. Health Educ. Res. 2005, 20, 548–556. [Google Scholar] [CrossRef]
- Grimley, D.M.; Riley, G.E.; Bellis, J.M.; Prochaska, J.O. Assessing the Stages of Change and Decision-Making for Contraceptive Use for the Prevention of Pregnancy, Sexually Transmitted Diseases, and Acquired Immunodeficiency Syndrome. Health Educ. Q. 1993, 20, 455–470. [Google Scholar] [CrossRef] [PubMed]
- Peipert, J.F.; Zhao, Q.; Meints, L.; Peipert, B.J.; Redding, C.A.; Allsworth, J.E. Adherence to dual-method contraceptive use. Contraception 2011, 84, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Boise, R.; Petersen, R.; Curtis, K.M.; Aalborg, A.; Yoshida, C.K.; Cabral, R.; Ballentine, J.M. Reproductive health counseling at pregnancy testing: A pilot study. Contraception 2003, 68, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Godin, G.; Lambert, L.-D.; Owen, N.; Nolin, B.; Prud’homme, D. Stages of motivational readiness for physical activity: A comparison of different algorithms of classification. Br. J. Health Psychol. 2004, 9, 253–267. [Google Scholar] [CrossRef]
- Ross, J.A.; Winfrey, W.L. Contraceptive use, intention to use and unmet need during the extended postpartum period. Int. Fam. Plan. Perspect. 2001, 27, 20–27. [Google Scholar] [CrossRef]
- Negash, W.D.; Eshetu, H.B.; Asmamaw, D.B. Intention to use contraceptives and its correlates among reproductive age women in selected high fertility sub-Saharan Africa countries: A multilevel mixed effects analysis. BMC Public Health 2023, 23, 257. [Google Scholar] [CrossRef]
- Odimegwu, C.; Phiri, M.; Tapera, T.; Simona, S. Patterns and correlates of intention to use contraceptives among fecund sexually active women in developing countries. Glob. Health Action 2023, 16, 2255043. [Google Scholar] [CrossRef]
- Sedgh, G.; Ashford, L.S.; Hussain, R. Unmet Need for Contraception in Developing Countries: Examining Women’s Reasons for Not Using a Method; Guttmacher Institute: New York, NY, USA, 2016. [Google Scholar]
- Hernandez, N.D.; Chandler, R.; Nava, N.; Tamler, I.; Daley, E.M.; Baldwin, J.A.; Buhi, E.R.; O’Rourke, K.; Romero-Daza, N.; Grilo, S. Young adult US-born Latina women’s thoughts, feelings and beliefs about unintended pregnancy. Cult. Health Sex. 2020, 22, 920–936. [Google Scholar]

| Country | Survey Year | Response/Completion Rates (%) | Females Interviewed | Sample | Subregion |
|---|---|---|---|---|---|
| Ethiopia | 2018 | 98.6 | 7429 | 1428 | East Africa |
| Kenya | 2018 | 99.1 | 5720 | 1057 | East Africa |
| Uganda | 2018 | 96.8 | 4225 | 1186 | East Africa |
| Burkina Faso | 2019 | 97.7 | 3388 | 797 | West Africa |
| Côte d’Ivoire | 2018 | 98.1 | 2738 | 740 | West Africa |
| Ghana | 2017 | 98.1 | 4154 | 736 | West Africa |
| Niger | 2017 | 97.0 | 3020 | 900 | West Africa |
| Nigeria | 2018 | 98.1 | 11,106 | 2644 | West Africa |
| Characteristics | Country (Survey Year) | |||||||
|---|---|---|---|---|---|---|---|---|
| Burkina Faso (2019) | Côte d’Ivoire (2018) | Ethiopia (2018) | Ghana (2017) | Kenya (2018) | Niger (2018) | Nigeria (2018) | Uganda (2018) | |
| Number of women (n) | 886 | 745 | 1552 | 736 | 1057 | 1085 | 2644 | 1186 |
| All women (%) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Stage of change of contraceptive readiness | ||||||||
| Precontemplation (no intention to use) | 16.70 | 25.45 | 19.51 | 28.23 | 11.74 | 48.21 | 34.53 | 11.97 |
| Contemplation (intention to use) | 48.37 | 49.59 | 43.06 | 33.31 | 20.86 | 26.12 | 38.88 | 46.92 |
| Post-action (already using) | 35.56 | 24.96 | 37.43 | 38.45 | 67.40 | 25.68 | 26.60 | 41.15 |
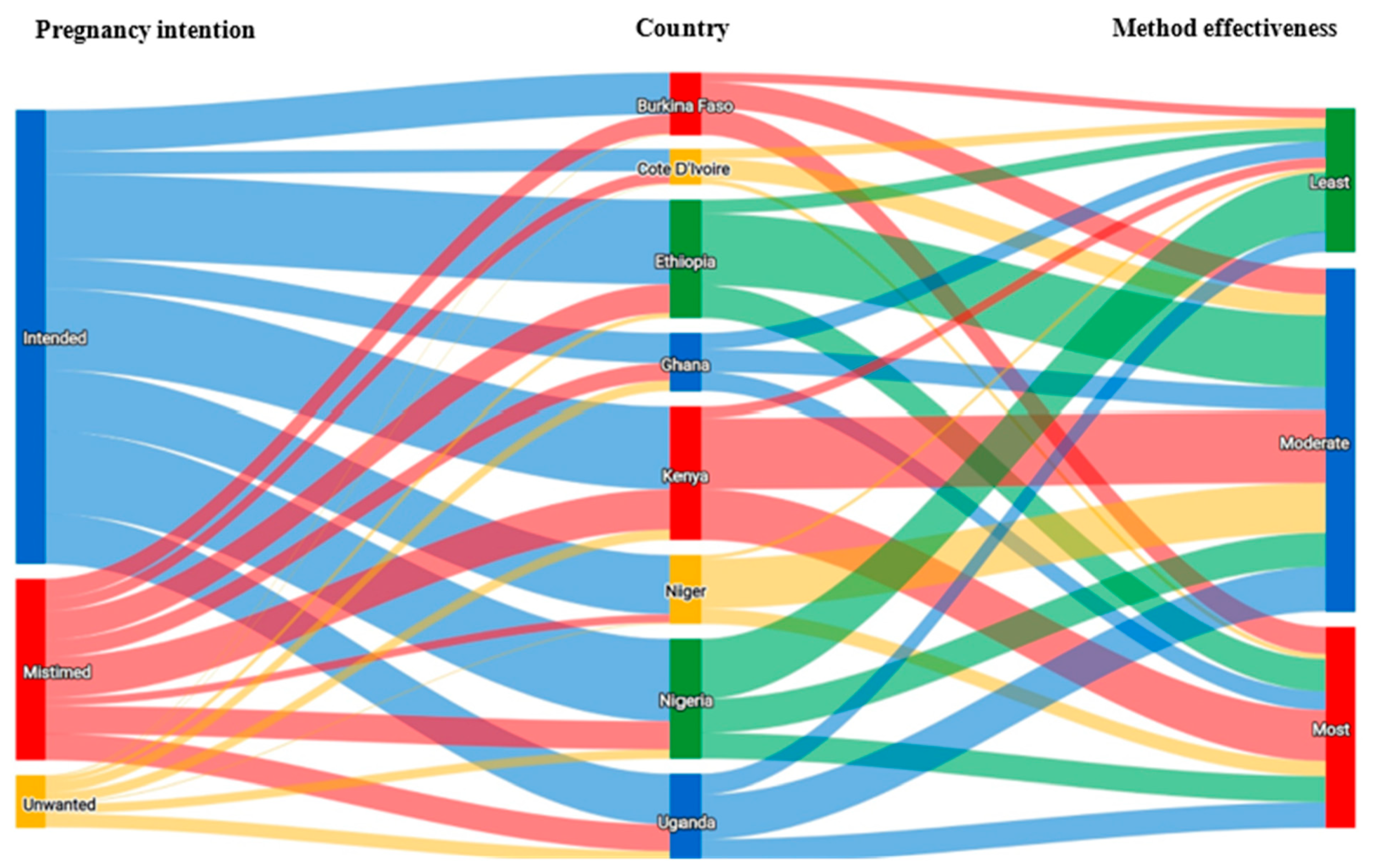
| Pregnancy intention | ||||||||
| Intended | 69.41 | 66.02 | 65.68 | 55.12 | 55.74 | 90.90 | 75.56 | 53.78 |
| Mistimed | 29.37 | 31.76 | 27.09 | 26.58 | 33.60 | 8.99 | 18.28 | 32.13 |
| Unwanted | 1.22 | 2.22 | 7.23 | 18.31 | 10.66 | 0.61 | 6.16 | 14.10 |
| Age, years | ||||||||
| 15–24 | 38.81 | 33.82 | 29.96 | 27.75 | 38.06 | 38.45 | 25.50 | 39.19 |
| 24–34 | 42.79 | 47.17 | 51.20 | 49.76 | 47.46 | 42.98 | 51.35 | 43.91 |
| 35–49 | 18.4 | 19.01 | 18.84 | 22.49 | 14.48 | 18.58 | 23.16 | 16.91 |
| Parity | ||||||||
| Low | 42.59 | 44.43 | 42.84 | 53.68 | 56.44 | 37.22 | 42.24 | 40.13 |
| Average | 26.25 | 32.39 | 26.46 | 28.20 | 27.41 | 27.42 | 34.47 | 29.13 |
| High | 31.17 | 32.39 | 30.70 | 18.12 | 16.15 | 35.36 | 23.30 | 30.74 |
| Marital status | ||||||||
| Not married or in union | 5.45 | 12.57 | 4.33 | 11.43 | 17.31 | 3.32 | 4.66 | 14.21 |
| Currently married or in union | 94.55 | 87.43 | 95.67 | 88.57 | 82.69 | 96.68 | 95.34 | 85.79 |
| Highest level of education | ||||||||
| None | 68.12 | 53.31 | 48.41 | 20.62 | 5.98 | 71.32 | 27.04 | 10.08 |
| Primary | 15.82 | 28.79 | 36.60 | 19.62 | 47.74 | 17.42 | 18.39 | 60.01 |
| Secondary or higher | 16.06 | 17.90 | 14.99 | 59.76 | 46.28 | 11.26 | 54.57 | 29.92 |
| Fertility intention | ||||||||
| Want no more | 1.89 | 14.56 | 23.94 | 25.35 | 32.03 | 3.96 | 18.01 | 27.53 |
| Wants more | 87.23 | 82.15 | 67.15 | 70.45 | 62.31 | 93.39 | 70.52 | 69.22 |
| Ambivalent | 1.88 | 3.29 | 8.46 | 4.20 | 5.66 | 2.65 | 11.48 | 3.23 |
| Received family-planning counseling | ||||||||
| No | 51.03 | 65.48 | 66.56 | 57.50 | 50.95 | 67.16 | 50.69 | 46.50 |
| Yes | 48.97 | 34.52 | 33.44 | 42.50 | 49.04 | 32.84 | 49.31 | 53.50 |
| Exposure to family-planning mass media | ||||||||
| Not exposed | 36.44 | 46.15 | 61.23 | 24.00 | 7.28 | 49.61 | 31.75 | 20.62 |
| Exposed | 63.56 | 53.85 | 38.77 | 76.01 | 92.72 | 50.39 | 68.25 | 79.38 |
| Household wealth index | ||||||||
| Lowest | 37.85 | 50.12 | 43.01 | 48.42 | 46.16 | 29.62 | 53.64 | 49.69 |
| Average | 37.05 | 18.99 | 20.91 | 20.82 | 18.64 | 35.26 | 14.33 | 21.14 |
| Highest | 25.1 | 30.89 | 36.08 | 30.76 | 35.20 | 35.13 | 32.02 | 29.17 |
| Place of residence | ||||||||
| Rural | 84.14 | 47.00 | 78.97 | 57.68 | 68.69 | 83.88 | 51.66 | 82.95 |
| Urban | 15.86 | 53.00 | 21.03 | 42.32 | 31.32 | 16.12 | 48.34 | 17.05 |
| Burkina Faso | Côte d’Ivoire | Ethiopia | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-contemplation | Con-templation | Post-action | p Value | Pre-contemplation | Con-templation | Post-action | p Value | Pre-contemplation | Con-templation | Post-action | p Value | |
| Number of women (N) | 142 | 429 | 315 | 189 | 369 | 186 | 303 | 668 | 581 | |||
| All women (%) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||
| Pregnancy intention | ||||||||||||
| Intended | 82.57 | 68.47 | 64.74 | 0.037 | 78.52 | 61.97 | 61.32 | 0.01 | 73.03 | 59.77 | 68.64 | 0.002 |
| Mistimed | 15.46 | 30.83 | 33.67 | 20.63 | 35.04 | 36.58 | 22.52 | 29.17 | 27.08 | |||
| Unwanted | 1.96 | 0.70 | 1.59 | 0.85 | 2.98 | 2.10 | 4.44 | 11.06 | 4.28 | |||
| Age, years | ||||||||||||
| 15–24 | 38.30 | 40.86 | 36.25 | 0.40 | 33.29 | 37.33 | 27.41 | 0.006 | 26.38 | 32.82 | 28.54 | 0.0002 |
| 24–34 | 38.82 | 41.16 | 46.80 | 44.54 | 49.62 | 44.98 | 43.22 | 50.54 | 56.13 | |||
| 35–49 | 22.88 | 17.98 | 16.95 | 22.17 | 13.05 | 27.62 | 30.40 | 16.63 | 15.34 | |||
| Parity | ||||||||||||
| Low | 45.00 | 41.47 | 43.02 | 0.40 | 41.07 | 47.16 | 42.41 | 0.64 | 30.60 | 39.79 | 52.74 | <0.0001 |
| Average | 19.71 | 27.07 | 28.09 | 31.63 | 32.27 | 33.38 | 24.66 | 26.37 | 27.50 | |||
| High | 35.29 | 31.47 | 28.89 | 27.29 | 20.56 | 24.21 | 44.74 | 33.84 | 19.77 | |||
| Marital status | ||||||||||||
| Not married or in union | 3.75 | 5.78 | 5.76 | 0.71 | 9.81 | 15.10 | 10.35 | 0.14 | 6.17 | 5.15 | 2.44 | 0.047 |
| Currently married or in union | 96.25 | 94.22 | 94.24 | 90.19 | 84.90 | 89.65 | 93.83 | 94.85 | 97.57 | |||
| Highest level of education | ||||||||||||
| None | 76.70 | 71.11 | 60.18 | 0.017 | 67.76 | 53.41 | 38.36 | <0.0001 | 74.70 | 49.33 | 33.65 | <0.0001 |
| Primary | 11.67 | 15.81 | 17.72 | 22.12 | 29.16 | 34.87 | 21.00 | 38.95 | 42.03 | |||
| Secondary or higher | 11.64 | 13.08 | 22.11 | 10.12 | 17.43 | 26.77 | 4.30 | 11.73 | 24.32 | |||
| Fertility intention | ||||||||||||
| Want no more | 10.88 | 10.95 | 10.81 | 0.72 | 10.28 | 15.96 | 16.15 | 0.27 | 21.62 | 28.26 | 20.18 | 0.01 |
| Wants more | 86.51 | 87.94 | 86.58 | 87.41 | 81.08 | 78.91 | 66.03 | 63.67 | 72.93 | |||
| Ambivalent | 2.61 | 1.11 | 2.61 | 2.30 | 2.96 | 4.95 | 12.34 | 8.07 | 6.90 | |||
| Received family planning counseling | ||||||||||||
| No | 52.07 | 49.11 | 53.18 | 0.63 | 78.13 | 63.67 | 56.19 | 0.002 | 77.11 | 66.62 | 60.99 | 0.017 |
| Yes | 47.93 | 50.89 | 46.82 | 21.87 | 36.33 | 43.81 | 22.89 | 33.38 | 39.01 | |||
| Exposure to family planning mass media | ||||||||||||
| Not exposed | 50.01 | 32.94 | 0.031 | 59.11 | 48.68 | 27.90 | <0.0001 | 70.44 | 62.69 | 54.75 | 0.004 | |
| Exposed | 49.99 | 67.06 | 64.93 | 40.89 | 51.32 | 72.10 | 29.57 | 37.31 | 45.25 | |||
| Household wealth index | ||||||||||||
| Lowest | 40.42 | 42.16 | 30.82 | 0.002 | 55.04 | 60.84 | 23.81 | <0.0001 | 54.38 | 51.27 | 27.58 | <0.0001 |
| Average | 34.82 | 39.75 | 34.38 | 20.49 | 15.83 | 23.75 | 24.13 | 23.44 | 16.32 | |||
| Highest | 24.76 | 18.09 | 34.80 | 24.47 | 23.34 | 52.44 | 21.49 | 25.29 | 56.10 | |||
| Place of residence | ||||||||||||
| Rural | 86.71 | 88.92 | 76.48 | <0.0001 | 55.36 | 52.00 | 28.55 | 0.001 | 88.47 | 85.77 | 66.21 | <0.0001 |
| Urban | 13.29 | 11.08 | 23.52 | 44.64 | 48.00 | 71.45 | 11.53 | 14.23 | 33.79 | |||
| Ghana | Kenya | Niger | ||||||||||
| Pre-contemplation | Con-templation | Post- action | p Value | Pre-contemplation | Con-templation | Post-Action | p Value | Pre-contemplation | Con-templation | Post-action | p Value | |
| Number of women (N) | 208 | 246 | 283 | 123 | 249 | 709 | 523 | 283 | 279 | |||
| All women (%) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||
| Pregnancy intention | ||||||||||||
| Intended | 63.73 | 52.66 | 50.93 | 0.03 | 56.65 | 44.26 | 59.13 | 0.006 | 90.28 | 90.17 | 90.85 | 0.87 |
| Mistimed | 23.60 | 25.46 | 29.73 | 29.95 | 39.22 | 32.50 | 8.98 | 9.74 | 8.28 | |||
| Unwanted | 12.68 | 21.88 | 19.34 | 13.40 | 16.52 | 8.37 | 0.75 | 0.10 | 0.88 | |||
| Age, years | ||||||||||||
| 15–24 | 23.03 | 28.08 | 30.93 | 0.14 | 33.12 | 47.48 | 36.00 | <0.0001 | 39.18 | 35.64 | 39.93 | 0.88 |
| 24–34 | 49.46 | 52.27 | 47.82 | 38.43 | 41.03 | 51.02 | 41.25 | 46.50 | 42.64 | |||
| 35–49 | 27.51 | 19.65 | 21.25 | 28.45 | 11.49 | 12.98 | 19.57 | 17.86 | 17.43 | |||
| Parity | ||||||||||||
| Low | 57.51 | 53.11 | 51.37 | 0.73 | 44.95 | 61.90 | 56.74 | <0.0001 | 33.99 | 36.19 | 44.35 | 0.33 |
| Average | 27.15 | 28.48 | 28.47 | 15.58 | 21.23 | 31.38 | 29.46 | 25.33 | 25.69 | |||
| High | 15.34 | 18.11 | 20.16 | 39.47 | 16.86 | 11.87 | 36.55 | 38.48 | 29.96 | |||
| Marital status | ||||||||||||
| Not married or in union | 13.09 | 16.24 | 6.03 | 0.003 | 23.99 | 29.74 | 12.30 | <0.0001 | 4.10 | 3.44 | 1.75 | 0.49 |
| Currently married or in union | 86.91 | 83.76 | 93.97 | 76.00 | 70.26 | 87.70 | 95.90 | 96.56 | 98.25 | |||
| Highest level of education | ||||||||||||
| None | 23.25 | 20.26 | 19.00 | 0.23 | 26.62 | 8.23 | 1.69 | <0.0001 | 79.39 | 66.76 | 60.81 | <0.0001 |
| Primary | 15.30 | 23.57 | 19.37 | 56.74 | 54.53 | 44.08 | 14.34 | 22.07 | 18.46 | |||
| Secondary or higher | 61.45 | 56.17 | 61.63 | 16.64 | 37.24 | 54.23 | 6.27 | 11.17 | 20.73 | |||
| Fertility intention | ||||||||||||
| Want no more | 25.43 | 23.84 | 26.60 | 0.15 | 28.20 | 32.96 | 32.41 | 0.936 | 3.44 | 4.63 | 4.28 | 0.73 |
| Wants more | 67.65 | 74.01 | 69.42 | 66.65 | 61.00 | 62.14 | 94.08 | 91.52 | 94.01 | |||
| Undecided | 6.93 | 2.14 | 3.99 | 6.15 | 6.03 | 5.46 | 2.49 | 3.85 | 1.74 | |||
| Received family planning counseling | ||||||||||||
| No | 69.72 | 56.70 | 49.23 | 0.0003 | 60.62 | 47.54 | 50.32 | 0.203 | 73.29 | 66.7325 | 56.09 | 0.0019 |
| Yes | 30.28 | 43.31 | 50.77 | 39.38 | 52.46 | 49.68 | 26.71 | 33.2675 | 43.92 | |||
| Exposure to family planning mass media | ||||||||||||
| Not exposed | 25.36 | 29.51 | 18.22 | 0.017 | 21,04 | 9.20 | 4.29 | <0.0001 | 50.68 | 45.86 | 51.41 | 0.72 |
| Exposed | 74.64 | 70.49 | 81.78 | 78.96 | 90.80 | 95.71 | 49.32 | 54.14 | 48.59 | |||
| Household wealth index | ||||||||||||
| Lowest | 42.56 | 57.50 | 44.86 | 0.018 | 65.58 | 47.44 | 42.39 | 0.0013 | 35.3048 | 32.43 | 16.09 | <0.0001 |
| Average | 25.78 | 18.44 | 19.23 | 15.13 | 21.81 | 18.27 | 40.1511 | 29.85 | 31.57 | |||
| Highest | 31.67 | 24.05 | 35.91 | 19.27 | 30.76 | 39.34 | 24.5441 | 37.73 | 52.35 | |||
| Place of residence | ||||||||||||
| Rural | 47.18 | 66.82 | 57.47 | 0.011 | 85.26 | 68.39 | 65.89 | 0.0004 | 90.4424 | 86.71 | 68.70 | <0.0001 |
| Urban | 52.82 | 33.18 | 42.53 | 14.74 | 31.61 | 34.11 | 9.5576 | 13.30 | 31.30 | |||
| Nigeria | Uganda | |||||||||||
| Pre-contemplation | Contemplation | Post-action | p Value | Pre-contemplation | Contemplation | Post-action | p Value | |||||
| Number of women (N) | 862 | 973 | 664 | 142 | 560 | 492 | ||||||
| All women (%) | 100 | 100 | 100 | 100 | 100 | 100 | ||||||
| Pregnancy intention | ||||||||||||
| Intended | 82.15 | 72.66 | 71.23 | 0.0009 | 63.34 | 47.60 | 58.05 | 0.013 | ||||
| Mistimed | 12.94 | 22.09 | 19.64 | 27.64 | 36.33 | 28.65 | ||||||
| Unwanted | 4.90 | 5.25 | 9.13 | 9.02 | 16.08 | 13.31 | ||||||
| Age, years | ||||||||||||
| 15–24 | 32.75 | 25.38 | 16.26 | <0.0001 | 38.56 | 37.72 | 41.05 | 0.18 | ||||
| 24–34 | 44.47 | 52.59 | 58.46 | 39.01 | 43.62 | 45.65 | ||||||
| 35–49 | 22.78 | 22.03 | 25.28 | 22.43 | 18.66 | 13.30 | ||||||
| Parity | ||||||||||||
| Low | 38.70 | 44.66 | 43.27 | 0.0064 | 39.37 | 36.91 | 44.03 | 0.014 | ||||
| Average | 33.51 | 32.22 | 38.98 | 31.59 | 27.14 | 30.68 | ||||||
| High | 27.79 | 23.11 | 17.75 | 29.04 | 35.95 | 25.30 | ||||||
| Marital status | ||||||||||||
| Not married or in union | 5.21 | 4.97 | 3.49 | 0.398 | 17.52 | 16.66 | 10.45 | 0.035 | ||||
| Currently married or in union | 94.79 | 95.03 | 96.51 | 82.48 | 83.34 | 89.55 | ||||||
| Highest level of education | ||||||||||||
| None | 48.07 | 21.43 | 7.95 | <0.0001 | 21.12 | 11.36 | 5.41 | <0.0001 | ||||
| Primary | 20.20 | 22.33 | 10.30 | 53.33 | 64.33 | 57.01 | ||||||
| Secondary or higher | 31.74 | 56.25 | 81.76 | 25.55 | 24.31 | 37.58 | ||||||
| Fertility intention | ||||||||||||
| Want no more | 9.77 | 19.24 | 26.90 | 19.18 | 31.67 | 25.24 | 0.0098 | |||||
| Wants more | 73.45 | 71.11 | 65.85 | 74.34 | 64.86 | 72.74 | ||||||
| Undecided | 16.78 | 9.66 | 7.25 | 19.18 | 31.67 | 25.24 | ||||||
| Received family planning counseling | ||||||||||||
| No | 66.72 | 48.83 | 32.61 | <0.0001 | 55.38 | 42.50 | 48.47 | 0.027 | ||||
| Yes | 33.28 | 51.17 | 67.39 | 44.62 | 57.50 | 51.53 | ||||||
| Exposure to family planning mass media | ||||||||||||
| Not exposed | 45.34 | 30.44 | 16.03 | <0.0001 | 21.77 | 19.70 | 21.34 | 0.74 | ||||
| Exposed | 54.66 | 69.56 | 83.97 | 78.23 | 80.30 | 78.66 | ||||||
| Household wealth index | ||||||||||||
| Lowest | 72.14 | 56.02 | 26.17 | <0.0001 | 57.81 | 57.94 | 37.93 | <0.0001 | ||||
| Average | 11.83 | 14.32 | 17.61 | 18.94 | 18.77 | 24.49 | ||||||
| Highest | 16.04 | 29.66 | 56.22 | 23.25 | 23.30 | 37.58 | ||||||
| Place of residence | ||||||||||||
| Rural | 65.73 | 52.90 | 31.58 | <0.0001 | 84.00 | 83.62 | 81.88 | 0.82 | ||||
| Urban | 34.27 | 47.10 | 68.42 | 16.00 | 16.38 | 18.12 | ||||||
| Country | Contemplation vs. Precontemplation | Post-action vs. Precontemplation | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pregnancy Intentions | Crude OR | 95% CI | p Value | aOR | 95% CI | p Value | Crude OR | 95% CI | p Value | aOR | 95% CI | p Value | |
| Burkina Faso | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | |||||
| Mistimed | 2.40 | 1.10–5.24 | 0.028 | 2.12 | 0.92–4.91 | 0.078 | 2.78 | 1.29–5.79 | 0.0094 | 2.88 | 1.29–6.44 | 0.011 | |
| Unwanted | 0.43 | 0.08–2.46 | 0.34 | 0.59 | 0.09–3.99 | 0.58 | 1.03 | 0.18–5.83 | 0.98 | 1.36 | 0.22–8.56 | 0.74 | |
| Côte d’Ivoire | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | |||||
| Mistimed | 2.15 | 1.46–3.16 | 0.0002 | 1.95 | 1.20–3.18 | 0.0081 | 2.27 | 1.36–3.80 | 0.0023 | 2.57 | 1.34–4.92 | 0.0052 | |
| Unwanted | 4.46 | 0.69–28.70 | 0.11 | 4.94 | 0.65–37.23 | 0.12 | 3.16 | 0.37–27.08 | 0.29 | 7.97 | 0.48–13.15 | 0.15 | |
| Ethiopia | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | |||||
| Mistimed | 1.58 | 1.00–2.50 | 0.048 | 1.58 | 0.69–2.59 | 0.07 | 1.28 | 0.77–2.13 | 0.34 | 1.41 | 0.83–2.41 | 0.21 | |
| Unwanted | 3.04 | 1.40–6.60 | 0.005 | 2.69 | 1.15–6.31 | 0.023 | 1.03 | 0.39–2.72 | 0.96 | 1.15 | 0.42–3.17 | 0.79 | |
| Ghana | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | |||||
| Mistimed | 1.31 | 0.80–2.13 | 0.28 | 1.19 | 0.65–2.19 | 0.56 | 1.58 | 0.96–2.60 | 0.074 | 1.57 | 0.87–2.81 | 0.13 | |
| Unwanted | 2.09 | 1.09–3.97 | 0.025 | 1.69 | 0.85–3.38 | 0.13 | 1.91 | 1.04–3.52 | 0.039 | 1.79 | 0.89–3.59 | 0.09 | |
| Kenya | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | |||||
| Mistimed | 1.68 | 0.94–2.99 | 0.08 | 1.74 | 0.90–3.38 | 0.10 | 1.04 | 0.59–1.82 | 0.89 | 1.31 | 0.72–2.39 | 0.38 | |
| Unwanted | 1.58 | 0.72–3.47 | 0.26 | 1.49 | 0.55–4.07 | 0.43 | 0.59 | 0.28–1.27 | 0.18 | 0.77 | 0.32–1.88 | 0.57 | |
| Niger | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | |||||
| Mistimed | 1.09 | 0.45–2.61 | 0.85 | 1.07 | 0.42–2.77 | 0.88 | 0.92 | 0.47–1.80 | 0.80 | 1.03 | 0.49–2.15 | 0.93 | |
| Unwanted | 0.13 | 0.01–1.69 | 0.12 | 0.08 | 0.01–1.12 | 0.06 | 1.17 | 0.21–6.51 | 0.86 | 0.58 | 0.13–2.49 | 0.46 | |
| Nigeria | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | |||||
| Mistimed | 1.93 | 1.25–2.97 | 0.0029 | 1.97 | 1.25–3.17 | 0.0041 | 1.75 | 1.10–2.79 | 0.019 | 2.05 | 1.25–3.38 | 0.0049 | |
| Unwanted | 1.21 | 0.69–2.10 | 0.49 | 0.99 | 0.58–1.69 | 0.96 | 2.15 | 1.28–3.60 | 0.0037 | 2.19 | 1.19–4.04 | 0.012 | |
| Uganda | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | |||||
| Mistimed | 1.75 | 1.05–2.91 | 0.032 | 1.62 | 0.97–2.70 | 0.07 | 1.13 | 0.62–2.07 | 0.67 | 1.32 | 0.74–2.34 | 0.35 | |
| Unwanted | 2.37 | 1.21–4.65 | 0.012 | 1.94 | 0.88–4.27 | 0.10 | 1.61 | 0.76–3.41 | 0.21 | 1.89 | 0.74–4.81 | 0.18 | |
| Contemplation vs. Post-action | |||||||||||||
| Country | Pregnancy Intentions | Crude OR | 95% CI | p Value | aOR | 95% CI | p Value | ||||||
| Burkina Faso | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | |||||||||
| Mistimed | 0.87 | 0.53–1.42 | 0.56 | 0.74 | 0.44–1.25 | 0.26 | |||||||
| Unwanted | 0.42 | 0.08–2.28 | 0.31 | 0.43 | 0.07–2.68 | 0.36 | |||||||
| Côte d’Ivoire | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | |||||||||
| Mistimed | 0.95 | 0.64–1.40 | 0.79 | 0.76 | 0.47–1.22 | 0.26 | |||||||
| Unwanted | 1.41 | 0.44–4.52 | 0.56 | 0.62 | 0.11–3.66 | 0.59 | |||||||
| Ethiopia | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | |||||||||
| Mistimed | 1.24 | 0.81–1.89 | 0.33 | 1.12 | 0.72–1.74 | 0.61 | |||||||
| Unwanted | 2.97 | 1.64–5.38 | 0.0004 | 2.34 | 1.20–4.58 | 0.0125 | |||||||
| Ghana | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | |||||||||
| Mistimed | 0.83 | 0.56–1.22 | 0.34 | 0.76 | 0.48–1.20 | 0.24 | |||||||
| Unwanted | 1.09 | 0.73–1.64 | 0.66 | 0.95 | 0.56–1.60 | 0.84 | |||||||
| Kenya | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | |||||||||
| Mistimed | 1.61 | 1.13–2.31 | 0.0092 | 1.33 | 0.90–1.97 | 0.15 | |||||||
| Unwanted | 2.64 | 1.40–4.96 | 0.0029 | 1.93 | 0.92–4.07 | 0.08 | |||||||
| Niger | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | |||||||||
| Mistimed | 1.19 | 0.44–3.21 | 0.74 | 1.04 | 0.37–2.94 | 0.94 | |||||||
| Unwanted | 0.11 | 0.01–1.08 | 0.06 | 0.14 | 0.01–1.83 | 0.13 | |||||||
| Nigeria | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | |||||||||
| Mistimed | 1.10 | 0.78–1.56 | 0.58 | 0.97 | 0.68–1.37 | 0.85 | |||||||
| Unwanted | 0.56 | 0.28–1.12 | 0.101 | 0.45 | 0.22–0.94 | 0.034 | |||||||
| Uganda | |||||||||||||
| Intended | 1.00 | Referent | 1.00 | Referent | |||||||||
| Mistimed | 1.55 | 1.12–2.13 | 0.0085 | 1.23 | 0.91–1.65 | 0.17 | |||||||
| Unwanted | 1.47 | 0.93–2.32 | 0.09 | 1.03 | 0.62–1.69 | 0.92 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ujah, O.I.; Olagbuji, B.N.; Ogbu, C.E.; Ujah, I.A.O.; Kirby, R.S. Pregnancy Desirability and Motivational Readiness for Postpartum Contraceptive Use: Findings from Population-Based Surveys in Eight Sub-Saharan African Countries. Int. J. Environ. Res. Public Health 2024, 21, 53. https://doi.org/10.3390/ijerph21010053
Ujah OI, Olagbuji BN, Ogbu CE, Ujah IAO, Kirby RS. Pregnancy Desirability and Motivational Readiness for Postpartum Contraceptive Use: Findings from Population-Based Surveys in Eight Sub-Saharan African Countries. International Journal of Environmental Research and Public Health. 2024; 21(1):53. https://doi.org/10.3390/ijerph21010053
Chicago/Turabian StyleUjah, Otobo I., Biodun N. Olagbuji, Chukwuemeka E. Ogbu, Innocent A. O. Ujah, and Russell S. Kirby. 2024. "Pregnancy Desirability and Motivational Readiness for Postpartum Contraceptive Use: Findings from Population-Based Surveys in Eight Sub-Saharan African Countries" International Journal of Environmental Research and Public Health 21, no. 1: 53. https://doi.org/10.3390/ijerph21010053
APA StyleUjah, O. I., Olagbuji, B. N., Ogbu, C. E., Ujah, I. A. O., & Kirby, R. S. (2024). Pregnancy Desirability and Motivational Readiness for Postpartum Contraceptive Use: Findings from Population-Based Surveys in Eight Sub-Saharan African Countries. International Journal of Environmental Research and Public Health, 21(1), 53. https://doi.org/10.3390/ijerph21010053







