Longitudinal Process of Setting and Achieving Activity- and Participation-Level Goals in Home Rehabilitation in Japan: A Qualitative Study Using Trajectory Equifinality Modeling
Abstract
1. Introduction
- Clarify the process of occupational therapists’ assessment and intervention in achieving activity- and participation-level goals during home-based rehabilitation.
- Categorize the assessment and intervention processes occupational therapists utilize to achieve activity- and participation-level goals in home-based rehabilitation.
2. Materials and Methods
2.1. Study Design
2.2. Study Participants and Ethics
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Participants’ Characteristics and Home Rehabilitation
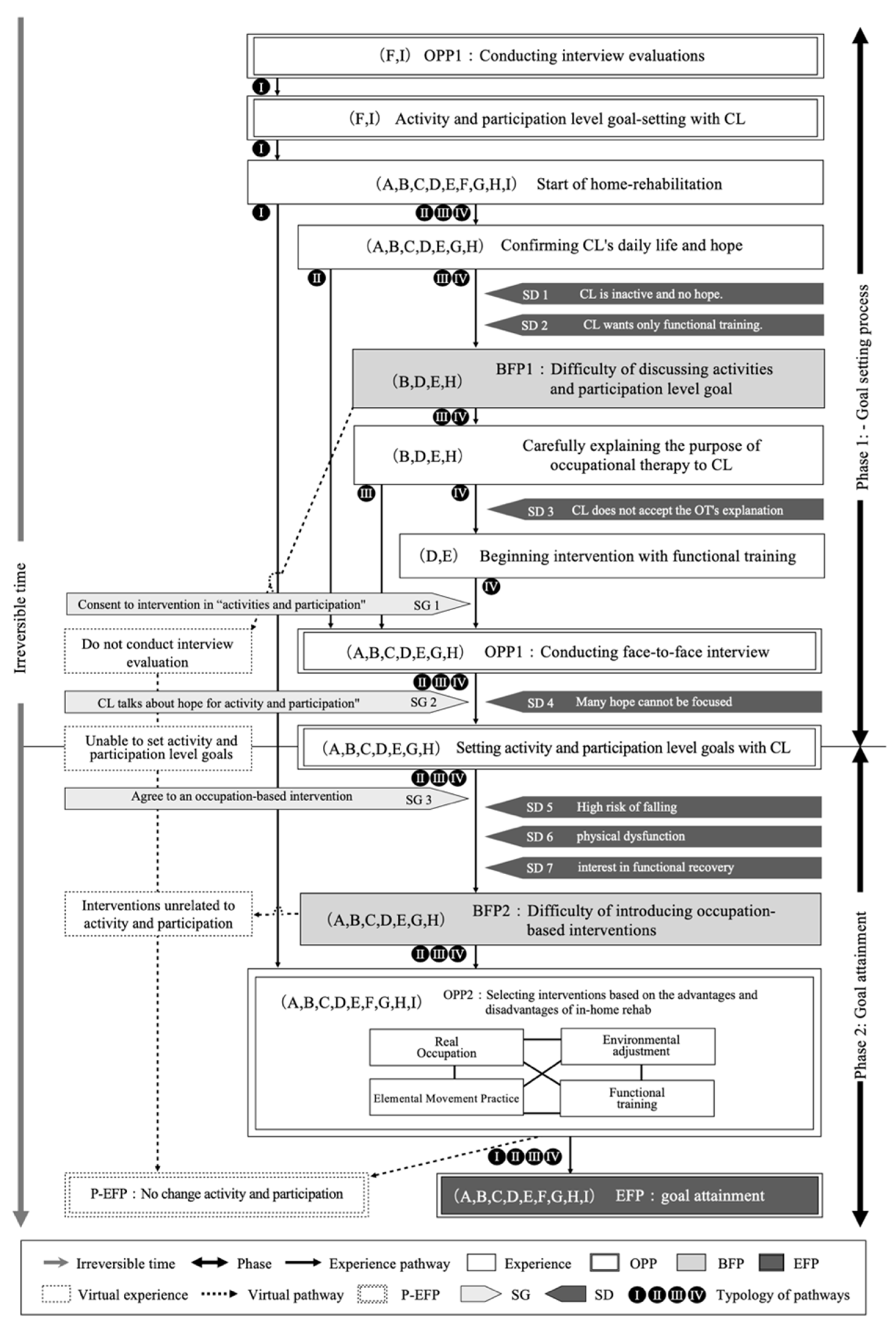
3.2. Definition of Items Using TEM Diagram
3.3. Classification of Time Phases
3.3.1. Phase 1: Goal-Setting Process
- Paternalistic explanations and persuasion are not effective.
- Building a trusting relationship with the client is a priority.
- Client-centered values are the basis for interaction.
- “The goal of occupational therapy is not for me to decide.”
- “Occupational therapy is more effective when the client participates actively.”
- “It is important for the occupational therapist to provide the client with opportunities to reflect on the current situation and to work together to identify challenges and expectations related to their level of activity and participation.”
3.3.2. Phase 2: Goal Attainment
| BFP | SD and SG Related to BFP | A Part of the Narrative Obtained from the Results |
|---|---|---|
| BFP1: Difficulty in having discussions focused on activities and participation | • SD1: CL is inactive with no hope • SD2: CL wants only functional training | • I did not think it would be effective to forcefully persuade clients to focus on the activity and participation level goal. • I thought that building a trusting relationship first was a higher priority. • In this situation, if communication and intervention are focused on activity and participation level, it would only lead to client distrust. • I thought creating an environment for clients to reflect and resolve issues together was important. |
| BFP2: Difficulty in having occupation-based interventions | • SG3: Agree to an occupation-based intervention • SD5: High risk of falling • SD6: Physical dysfunction • SD7: Interest in functional recovery | • I do not think the client’s reductionist approach can be changed by persuasion. • I think priority should be given to interventions to reduce the client’s risk of falling. • I think it is better to provide functional training and elemental movement exercises concurrently so that the client can participate in occupational therapy with conviction. |
- “The priority is an intervention aimed at risk reduction.”
- “When I visit a client’s home, I am the only staff member on-site; therefore, I need to consider various factors in determining interventions, including risk management, in addition to meeting activity and participation-level goals.”
- “Functional restoration training should be conducted concurrently to convince the client to participate in occupational therapy.”
- “The priority is to establish a trusting relationship. It was ineffective to forcefully persuade the client to focus on activity- and participation-level goals.”
- “Forcing communication and interventions to focus on activity and participation level would only lead to client distrust.”
- “I thought it was important to make a chance for clients to reflect and to resolve issues together.”
- Functional training and direct interventions at the activity and participation level are necessary to improve and maintain occupational performance.
- Occupational procedures and methods should be modified to make them safe and efficient.
3.4. Typification of Trajectories
3.4.1. Type I: Pathways with Shared Activity and Participation Goals before the Start of Home-Based Rehabilitation (Participants F and I)
3.4.2. Type II: Pathways with Shared Goals for Activity and Participation Levels in Initial Interview Evaluations (Participants A, C, and G)
3.4.3. Type III: Pathway with Activity and Participation Levels Goal Setting by Fully Explaining the Purpose of Home-Based Rehabilitation (Participants B and H)
3.4.4. Type IV: Pathways with Clients Who Did Not Understand the Purpose of Occupational Therapy Even after Explaining in Interviews (Participants D and E)
4. Discussion
4.1. Achieving Activity- and Participation-Level Goals
4.2. Categories of Assessment and Intervention Processes for Occupational Therapists to Achieve Activity- and Participation-Level Goals in Home Rehabilitation
4.3. Limitation and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rice, D.B.; McIntyre, A.; Mirkowski, M.; Janzen, S.; Viana, R.; Britt, E.; Teasell, R. Patient-centered goal setting in a hospital-based outpatient stroke rehabilitation center. PM R. 2017, 9, 856–865. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. Report of the Study Group on Rehabilitation of the Elderly in the Community. Available online: https://www.mhlw.go.jp/file/05-Shingikai-12301000-Roukenkyoku-Soumuka/0000081900.pdf (accessed on 15 March 2023). (In Japanese).
- Maitra, K.K.; Erway, F. Perception of client-centered practice in occupational therapists and their clients. Am. J. Occup. Ther. 2006, 60, 298–310. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.; Levack, W.; McPherson, K.M.; Dean, S.G.; Reed, K.; Weatherall, M.; Taylor, W.J. Survival, momentum, and things that make me “me”: Patients’ perceptions of goal setting after stroke. Disabil. Rehabil. 2014, 36, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, T.; Tomori, K.; Nagayama, H.; Okita, Y. The occupational experience helps to express the clients’ occupational needs in goal setting: A retrospective study in subacute care setting. Occup. Ther. Health Care. 2022, 36, 408–421. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, Y. TEA Theory—Learn the Fundamentals of the Trajectory Equifinality Approach. Shinyosya (In Japanese). 2015. [Google Scholar]
- Yasuda, Y. TEA Practice—Utilizing the trajectory equifinality approach. Shinyosya (In Japanese). 2015. [Google Scholar]
- Sato, T.; Hidaka, T.; Fukuda, M. Depicting the dynamics of living the life: The trajectory equifinality model. In Dynamic Process Methodology in the Social and Developmental Sciences; Springer: New York, NY, USA, 2009; pp. 217–240. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, A.; Yasuda, Y.; Sato, T. A method for analyzing with Trajectoyr equifinality model. Hum. Sci. Press Res. Ritsumeikan 2012, 25, 95–107 (In Japanese). (In Japanese) [Google Scholar]
- Palmadottir, G. Client perspectives on occupational therapy in rehabilitation services. Scand. J. Occup. Ther. 2003, 10, 157–166. [Google Scholar] [CrossRef]
- Rebeiro, K.L. Client perspectives on occupational therapy practice: Are we truly client-centred? Can. J. Occup. Ther. 2000, 67, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.J.; Chang, W.P.; Chang, M.C. Occupational therapy interventions to improve Activities of Daily Living for community-dwelling older adults: A systematic review. Am. J. Occup. Ther. 2018, 72, 7204190060p1–7204190060p11. [Google Scholar] [CrossRef] [PubMed]
- Chisholm, D.; Dolhi, C.D.; Schreiber, J. Occupational Therapy Intervention Resource Manual: A Guide for Occupation Based-Practice; Cengage Learning: Boston, MA, USA, 2003. [Google Scholar]
- Schut, H.A.; Stam, H.J. Goals in rehabilitation teamwork. Disabil. Rehabil. 1994, 16, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Duff, J.; Evans, M.J.; Kennedy, P. Goal planning: A retrospective audit of rehabilitation process and outcome. Clin. Rehabil. 2004, 18, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Turner-Stokes, L.; Rose, H.; Ashford, S.A.; Singer, B. Patient engagement and satisfaction with goal planning: Impact on outcome from rehabilitation. Int. J. Ther. Rehabil. 2015, 22, 210–216. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare in Japan; Social Security Council Subcommittee on Classification of Long-Term Care Benefits. Available online: https://www.mhlw.go.jp/file/05-Shingikai-12601000-Seisakutoukatsukan-Sanjikanshitsu_Shakaihoshoutantou/0000167233.pdf (accessed on 20 March 2023).
- Arbesman, M.; Mosley, L.J. Systematic review of occupation- and activity-based health management and maintenance interventions for community-dwelling older adults. Am. J. Occup. Ther. 2012, 66, 277–283. [Google Scholar] [CrossRef] [PubMed]
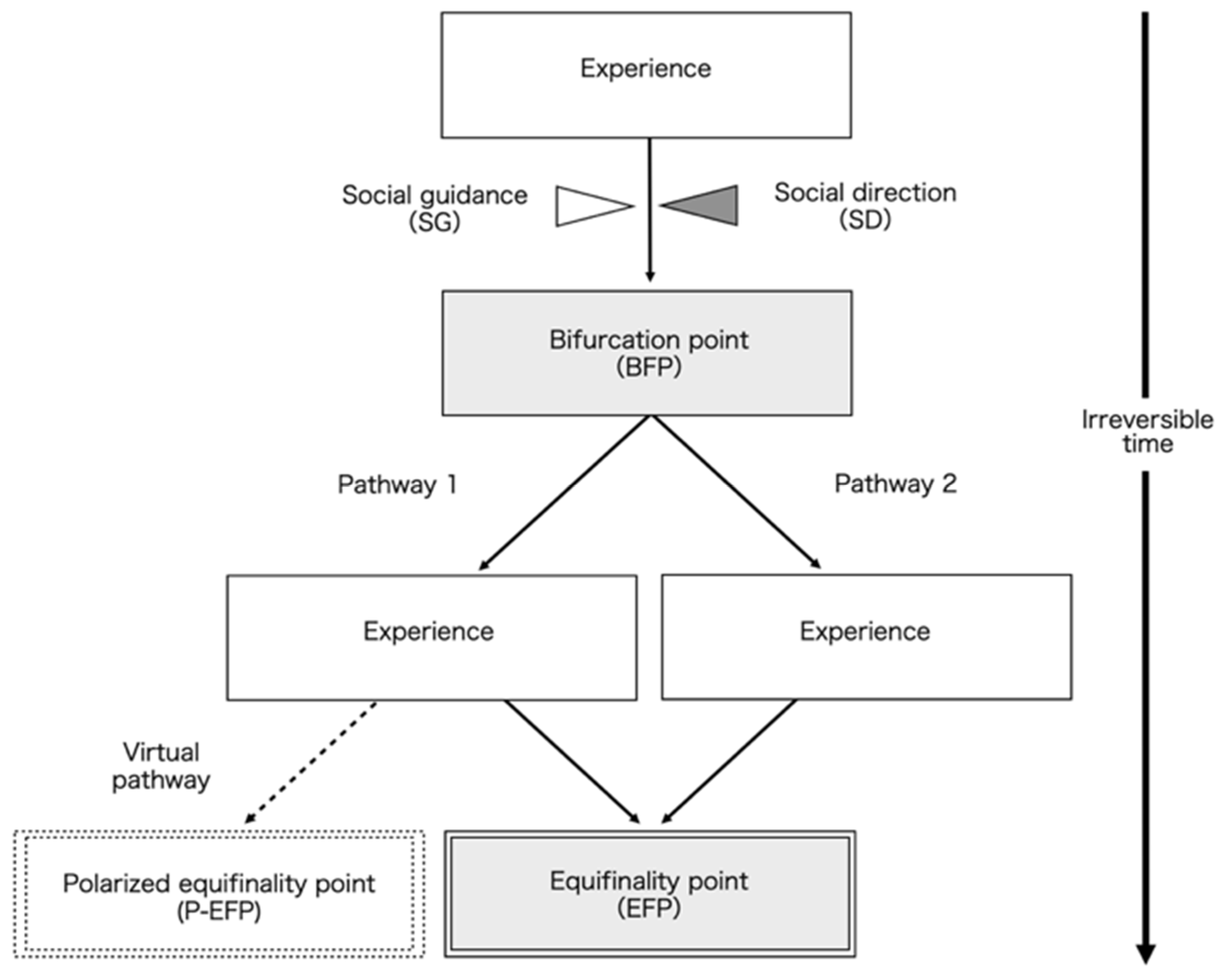
| Major Concepts | Definition | Implications for This Study |
|---|---|---|
| Irreversible Time | TEM incorporates the concept of time, but as an ongoing, qualitatively irreversible state rather than a concrete length of time reduced to units | − |
| EFP (Equifinality Point) | The situation that the study participants are in | Goal attainment |
| P-EFP (Polarized Equifinality Point) | The situation at the polar opposite of the equifinality point | No change in activity and participation |
| BFP (Bifurcation Point) | A situation at a certain experience that allows a choice between several optional trajectories | BFP-1: Difficulty in having discussions focused on activities and participation BFP-2: Difficulty in performing occupation-based interventions |
| OPP (Obligatory Passage Point) | A point that many people necessarily pass through | OPP-1: Conducting interview evaluations OPP-2: Selecting interventions based on the advantages and disadvantages of home-visit rehabilitation |
| SG (Social Guidance) | Environmental factors that attempt to move the individuals toward the equifinality point and their underlying social pressures | Environmental influences that are conducive to goal setting and goal attainment |
| SD (Social Direction) | Environmental factors that attempt to move the individuals away from the equifinality point and their underlying social pressures | Influences from the environment that act as inhibitors to goal setting and goal attainment |
| Main Questions | Subtopics |
|---|---|
| 1. What experience pathway did you follow before setting the activity- and participation-level goals? | − What is the goal? − How did you determine the goals? − What were some of the barriers to goal setting? − What did you do to overcome the barriers? − What kind of clinical judgment is the device based on? − What changes have resulted from this device? |
| 2. What experience pathway did you follow after setting a goal for activity and participation levels until achieving that goal? | − What barriers have you encountered in the process of achieving the goal? − What did you do to overcome the barriers? − What kind of clinical judgment is the device based on? − What changes have resulted from this device? |
| Information | A | B | C | D | E | F | G | H | I | |
|---|---|---|---|---|---|---|---|---|---|---|
| Occupational therapist | Number of interviews (times) | 3 | 3 | 4 | 3 | 2 | 3 | 3 | 3 | 3 |
| Total interview time | 110 min | 190 min | 150 min | 120 min | 90 min | 150 min | 110 min | 110 min | 120 min | |
| Sex | male | female | female | male | female | male | female | male | male | |
| Age (years) | 38 | 26 | 29 | 37 | 29 | 27 | 28 | 32 | 36 | |
| Clinical experience in OT (years) | 14 | 4 | 7 | 14 | 4 | 5 | 6 | 9 | 13 | |
| Experience in home rehab | 4 years | 6 months | 1 month | 1 month | 2 years | 1 year | 1 month | 3 years | 5 years | |
| Pathway in TEM | Type II | Type III | Type II | Type IV | Type IV | Type I | Type II | Type III | Type I | |
| Client | Diagnosis | Spiral cord injury | Stroke | Cervical spondylosis | Rheumatoid arthritis | Stroke | GBS | Stroke | Lumbar spondylosis | Femoral fracture |
| Level of basic ADL | Partial assistance | Partial assistance | Partial assistance | Partial assistance | Partial assistance | Partial assistance | Independent | Independent | Independent | |
| Goal | Gardening | Work | Wash hair | Cooking | Meet to friends | Take a shower | Mobilize outdoors | Mobilize outdoors | Cooking | |
| Frequency of home rehab | 2/week | 1/week | 2/week | 1/week | 1/week | 3/week | 1/week | 1/week | 2/week | |
| When is set a goal from starting OT? | After 1 week | At the start | After 2 weeks | After 2 months | After 5 months | At the start | After 2 weeks | After 5 months | After 6 months | |
| When did the goal achirve? | After 1 month | After 8 months | After 3 months | After 5 months | After 3.5 years | After 1 year | After 6 month | After 2 months | After 6 months | |
| After goal achievement | Continue | End | Continue | Continue | Continue | End | End | Continue | End | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saito, Y.; Tomori, K.; Sawada, T.; Ohno, K. Longitudinal Process of Setting and Achieving Activity- and Participation-Level Goals in Home Rehabilitation in Japan: A Qualitative Study Using Trajectory Equifinality Modeling. Int. J. Environ. Res. Public Health 2023, 20, 5746. https://doi.org/10.3390/ijerph20095746
Saito Y, Tomori K, Sawada T, Ohno K. Longitudinal Process of Setting and Achieving Activity- and Participation-Level Goals in Home Rehabilitation in Japan: A Qualitative Study Using Trajectory Equifinality Modeling. International Journal of Environmental Research and Public Health. 2023; 20(9):5746. https://doi.org/10.3390/ijerph20095746
Chicago/Turabian StyleSaito, Yuki, Kounosuke Tomori, Tatsunori Sawada, and Kanta Ohno. 2023. "Longitudinal Process of Setting and Achieving Activity- and Participation-Level Goals in Home Rehabilitation in Japan: A Qualitative Study Using Trajectory Equifinality Modeling" International Journal of Environmental Research and Public Health 20, no. 9: 5746. https://doi.org/10.3390/ijerph20095746
APA StyleSaito, Y., Tomori, K., Sawada, T., & Ohno, K. (2023). Longitudinal Process of Setting and Achieving Activity- and Participation-Level Goals in Home Rehabilitation in Japan: A Qualitative Study Using Trajectory Equifinality Modeling. International Journal of Environmental Research and Public Health, 20(9), 5746. https://doi.org/10.3390/ijerph20095746








