Evaluation of a Community Hospital-Based Residencies’ Intimate Partner Violence Education by a Domestic Violence Shelter Expert
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population and Sample Size
2.3. Description of Educational Program and Assessment Tool
- How domestic and sexual violence impact the health of their patients
- Four best practice interventions with patients on the topic of domestic and sexual violence
- Why healthcare providers should discuss domestic and sexual violence with their patients
- Sharing the limits of their confidentiality with patients
- Universal education on domestic and sexual violence
- Best practices for handling disclosure of domestic and sexual violence from patients
- A supported referral for patients experiencing domestic or sexual violence
- Describe and demonstrate the use of harm reduction strategies with survivors of domestic and sexual violence
- Describe and demonstrate the use of targeted interventions with survivors of domestic and sexual violence
- Describe real-life interactions between survivors of domestic and sexual violence with healthcare providers
2.4. Outcome Measures and Statistical Analyses
3. Results
3.1. Background
3.2. Opinions
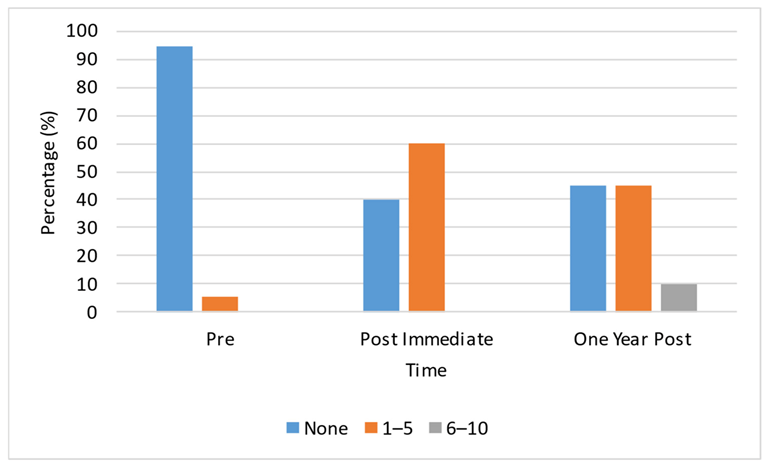
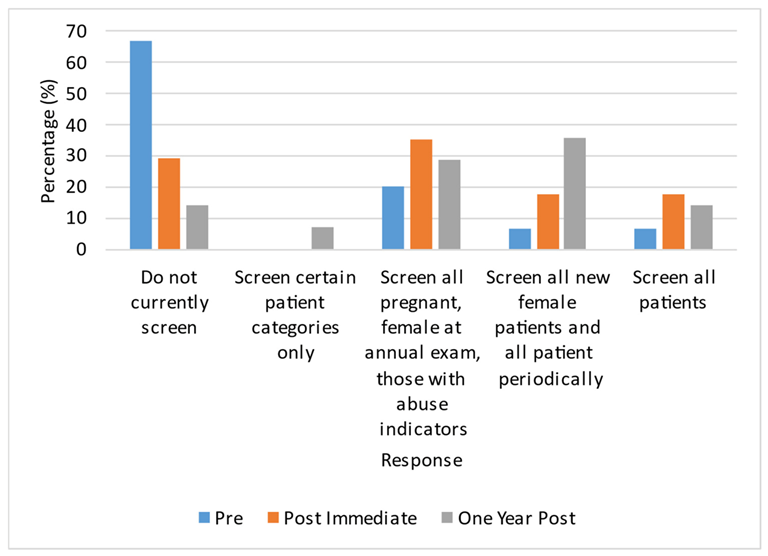
3.3. Practice Issues
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Violence Against Women. Available online: https://www.who.int/news-room/fact-sheets/detail/violence-against-women (accessed on 2 February 2023).
- Devries, K.M.; Mak, J.Y.; García-Moreno, C.; Petzold, M.; Child, J.C.; Falder, G.; Lim, S.; Bacchus, L.J.; Engell, R.E.; Rosenfeld, L.; et al. Global health. The global prevalence of intimate partner violence against women. Science 2013, 28, 1527–1528. [Google Scholar] [CrossRef] [PubMed]
- National Center for Injury Prevention and Control Centers for Disease Control and Prevention. Intimate Partner Violence Surveillance: Uniform Definitions and Recommended Data Elements. 2015, Version 2.0. Available online: https://stacks.cdc.gov/view/cdc/31292 (accessed on 2 February 2023).
- National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. The National Intimate Partner and Sexual Violence Survey: 2016/2017 Report on Intimate Partner Violence. 2022. Available online: https://www.cdc.gov/violenceprevention/pdf/nisvs/NISVSReportonIPV_2022.pdf (accessed on 23 February 2023).
- Campbell, J.C. Health consequences of intimate partner violence. Lancet 2002, 359, 1331–1336. [Google Scholar] [CrossRef] [PubMed]
- Radtke, K.M.; Ruf, H.; Gunter, K. Transgenerational impact of intimate partner violence on methylation in the promoter of the glucocorticoid receptor. Transl. Psychiatry 2011, 1, e21. [Google Scholar] [CrossRef] [PubMed]
- Waalen, J.; Goodwin, M.M.; Spitz, A.M.; Petersen, R.; Saltzman, L.E. Screening for intimate partner violence by health care providers. Barriers and interventions. Am. J. Prev. Med. 2000, 19, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Williamson, K.J.; Coonrod, D.V.; Bay, R.C. Screening for domestic violence: Practice patterns, knowledge and attitudes of physicians in Arizona. South Med. J. 2004, 97, 1049–1054. [Google Scholar] [CrossRef] [PubMed]
- Carlson, M.; Kamimura, A.; Al-Obaydi, S.; Trinh, H.N.; Franchek-Roa, K. Background and clinical knowledge of intimate partner violence: A study of primary care residents and medical students at a United States medical school. Health Equity 2017, 1, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Ghaith, S.; Voleti, S.S.; Ginsberg, Z.; Marks, L.A.; Files, J.A.; Kling, J.M. A scoping review of published intimate partner violence curricula for medical trainees. J. Womens Health 2022, 11, 1596–1613. [Google Scholar] [CrossRef] [PubMed]
- Insetta, E.R.; Christmas, C. A novel intimate partner violence curriculum for internal medicine residents: Development, implementation, and evaluation. MedEdPORTAL. 2020, 16, 10905. [Google Scholar] [CrossRef] [PubMed]
- EDUCATE Investigators. Assessing readiness to manage intimate partner violence 12 months after completion of an educational program in fracture clinics: A pretest-posttest study. CMAJ Open 2020, 8, E731–E736. [Google Scholar] [CrossRef] [PubMed]
- EDUCATE Investigators. Novel educational program improves readiness to manage intimate partner violence within the fracture clinic: A pretest-posttest study. CMAJ Open 2018, 6, E628–E636. [Google Scholar] [CrossRef] [PubMed]
- Madden, K.; Sprague, S.; Petrisor, B.A.; Farrokhyar, F.; Ghert, M.A.; Kirmani, M.; Bhandari, M. Orthopedic trainees retain knowledge after a partner abuse course: An education study. Clin. Orthop. Relat. Res. 2015, 473, 2415–2422. [Google Scholar] [CrossRef] [PubMed]
- Papadakaki, M.; Petridou, E.; Kogevinas, M.; Lionis, C. Measuring the effectiveness of an intensive IPV training program offered to Greek general practitioners and residents of general practice. BMC Med. Educ. 2013, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Short, L.M.; Alpert, E.; Harris Jr, J.M.; Surprenant, Z.J. A tool for measuring physician readiness to manage intimate partner violence. Am J Prev Med 2006, 30, 173–180. [Google Scholar] [CrossRef] [PubMed]
- CUES: An Evidence-Based Intervention. Available online: https://ipvhealth.org/health-professionals/educate-providers/ (accessed on 27 January 2023).
- Futures Without Violence. Health. Available online: https://www.futureswithoutviolence.org/health/ (accessed on 21 February 2023).
- Decker, M.R.; Frattaroli, S.; McCaw, B.; Coker, A.L.; Miller, E.; Sharps, P.; Lane, W.G.; Mandal, M.; Hirsch, K.; Strobino, D.M.; et al. Transforming the healthcare response to intimate partner violence and taking best practices to scale. J. Womens Health 2012, 12, 1222–1229. [Google Scholar] [CrossRef] [PubMed]
- Dutton, M.A.; James, L.; Langhorne, A.; Kelley, M. Coordinated public health initiatives to address violence against women and adolescents. J. Womens Health 2015, 1, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Martin-Engel, L.; Allen, J.; Alencar, A.; Levin, S.; Udezi, V.O.; Pagels, P.; Eary, R.L. Improving readiness to manage intimate partner violence in family medicine clinics by collaboration with a community organization. PRiMER 2021, 5, 20. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.W.; Coonrood, D.V.; Brady, M.J. Medical student training in domestic violence: A comparison of students entering residency training in 1995 and 2001. Teach. Learn. Med. 2004, 16, 3–6. [Google Scholar] [CrossRef] [PubMed]
| Category | Time | p-Value | ||
|---|---|---|---|---|
| Pre | Post Immediate | Post One Year | ||
| Background | ||||
| Perceived preparation | 3.6333 (1.18) b | 5.6549 (0.76) a | 5.4402 (0.63) a | 0.0001 |
| Perceived knowledge | 3.52 (1.01) b | 5.75 (0.76) a | 5.37 (0.86) a | 0.0001 |
| Actual knowledge | ||||
| Total | 26.70 (4.40) b | 30.15 (2.80) a | 22.90 (2.65) c | 0.0001 |
| Opinions | ||||
| Preparation | 4.22 (0.98) | 5.16 (1.1) | 4.89 (1.09) | 0.058 |
| Legal Requirements | 3.76 (1.24) b | 5.32 (1.18) a | 5.11 (1.32) a | 0.0001 |
| Workplace issues | 4.02 (1.17) | 4.69 (0.98) | 4.53 (0.81) | 0.11 |
| Self-efficacy | 3.42 (0.76) b | 4.93 (1.11) a | 4.68 (0.69) a | 0.0001 |
| Alcohol/drugs | 4.33 (0.53) | 4.3 (0.74) | 4.18 (0.63) | 0.57 |
| Victim understanding | 4.97 (0.45) | 5.33 (0.94) | 5.06 (0.95) | 0.21 |
| Question | Time | p-Value | ||
|---|---|---|---|---|
| Pre | Post Immediate | Post One Year | ||
| a. Ask appropriate questions about IPV | 4.11 (1.73) b | 5.79 (0.79) a | 5.58 (0.84) a | 0.002 |
| b. Appropriately respond to disclosures of abuse | 4.37 (1.34) b | 5.84 (0.76) a | 5.47 (0.77) a | 0.001 |
| c. Identify IPV indicators based on patient history and physical examination | 4.42 (1.57) b | 5.95 (0.85) a | 5.63 (0.5) a | 0.0001 |
| d. Assess an IPV victim’s readiness to change | 4.11 (1.29) b | 5.68 (0.75) a | 5.53 (0.7) a | 0.0001 |
| e. Help an IPV victim assess his/her danger of lethality | 3.78 (1.59) b | 5.67 (0.97) a | 5.22 (0.73) a | 0.0001 |
| f. Conduct a safety assessment for the victim’s children | 3.63 (1.71) b | 5.32 (1.11) a | 4.95 (1.22) a | 0.002 |
| g. Help an IPV victim create a safety plan | 3.32 (1.8) c | 5.74 (0.99) a | 5.21 (1.13) b | 0.0001 |
| h. Document IPV history and physical examination findings in the patient’s chart | 3.83 (1.58) b | 5.89 (0.96) a | 5.83 (0.92) a | 0.0001 |
| i. Make appropriate referrals for IPV | 3.06 (1.43) b | 5.56 (1.15) a | 5.67 (1.03) a | 0.0001 |
| j-1. Fulfill state reporting requirements for IPV | 2.80 (1.67) b | 5.50 (1.19) a | 5.55 (1.1) a | 0.0001 |
| j-2. Fulfill state reporting requirements for Child abuse | 3.05 (2.01) b | 5.40 (1.19) a | 5.50 (1.1) a | 0.0001 |
| j-3. Fulfill state reporting requirements for Elder abuse | 3.05 (2.07) b | 5.58 (1.22) a | 5.47 (1.12) a | 0.0001 |
| Question | Time | p-Value | ||
|---|---|---|---|---|
| Pre | Post Immediate | Post One Year | ||
| How much do you feel you now know about: a. Your legal reporting requirements for IPV | 2.95 (1.47) b | 5.58 (0.69) a | 5.26 (1.37) a | 0.0001 |
| How much do you feel you now know about a. Your legal reporting requirements for Child abuse | 3.58 (1.87) b | 5.79 (0.92) a | 5.42 (1.35) a | 0.0001 |
| How much do you feel you now know about a. Your legal reporting requirements for Elder abuse | 3.53 (1.84) b | 5.84 (0.96) a | 5.37 (1.46) a | 0.0004 |
| b. Signs or symptoms of IPV | 4.10 (1.37) b | 5.75 (0.79) a | 5.50 (1.00) a | 0.0001 |
| c. How to document IPV in a patient’s chart | 3.15 (1.09) b | 5.70 a (0.8) | 5.40 a (0.99) | 0.0001 |
| d. Referral sources for IPV victims | 3.05 (1.18) b | 5.74 (0.99) a | 5.53 (1.17) a | 0.0001 |
| e. Perpetrators of IPV | 3.16 (1.34) b | 5.63 (1.07) a | 5.21 (1.18) a | 0.0001 |
| f. Relationship between IPV and pregnancy | 3.25 (1.45) b | 5.65 (1.04) a | 5.15 (1.09) a | 0.0001 |
| g. Recognizing the childhood effects of witnessing IPV | 3.32 (1.67) b | 5.37 (1.07) a | 5.21 (1.08) a | 0.0002 |
| h. What questions to ask to identify IPV | 3.79 (1.36) b | 5.84 (1.01) a | 5.63 (1.01) a | 0.0001 |
| i. Why a victim might not disclose IPV | 4.05 (1.54) b | 6.00 (1.03) a | 5.55 (0.89) a | 0.0001 |
| j. Your role in detecting IPV | 4.05 (1.51) b | 6.16 (0.96) a | 5.58 (0.9) a | 0.0001 |
| k. What to say and not say in IPV situations with a patient | 3.85 (1.46) b | 5.90 (0.97) a | 5.55 (1.05) a | 0.0001 |
| l. Determining danger for a patient experiencing IPV | 3.55 (1.39) b | 5.85 (0.81) a | 5.35 (0.99) a | 0.0001 |
| m. Developing a safety plan with an IPV victim | 3.28 (1.49) c | 5.67 (0.84) a | 4.94 (0.87) b | 0.0001 |
| n. The stages an IPV victim experiences in understanding and changing his/her situation | 3.53 (1.39) b | 5.53 (0.96) a | 5.37 (0.83) a | 0.0001 |
| Questions | Time | ||
|---|---|---|---|
| Pre | Post Immediate | Post One Year | |
| What is the strongest single risk factor for becoming a victim of intimate partner violence? | 20 | 40. | 25 |
| Alcohol consumption is the greatest single predictor of the likelihood of IPV. | 100 | 100 | 35 |
| There are no good reasons not to leave an abusive relationship | 100 | 100 | 30 |
| Reasons for concern about IPV should not be included in a patient’s chart if s/he does not disclose the violence | 100 | 100 | 55 |
| When asking patients about IPV, physicians should use the words “abused” or “battered.” | 100 | 100 | 90 |
| Being supportive of a patient’s choice to remain in a violent relationship would condone the abuse. | 100 | 100 | 65 |
| Victims of IPV are able to make appropriate choices about how to handle their situation. | 100 | 100 | 55 |
| Healthcare providers should not pressure patients to acknowledge that they are living in an abusive relationship | 100 | 100 | 90 |
| Victims of IPV are at greater risk of injury when they leave the relationship. | 100 | 100 | 65 |
| Strangulation injuries are rare in cases of IPV. | 100 | 100 | 80 |
| Allowing partners or friends to be present during a patient’s history and physical exam ensures the safety of an IPV victim. | 100 | 100 | 100 |
| Which one of the following is generally true about batterers? | 85 | 85 | 100 |
| Which of the following are warning signs that a patient may have been abused by his/her partner—Chronic unexplained pain | 90 | 100 | 95 |
| Which of the following are warning signs that a patient may have been abused by his/her partner?—Anxiety | 90 | 100 | 100 |
| Which of the following are warning signs that a patient may have been abused by his/her partner?—Frequent injuries | 100 | 100 | 100 |
| Which of the following are warning signs that a patient may have been abused by his/her partner?—Depression | 90 | 100 | 95 |
| Which of the following are reasons an IPV victim may not be able to leave a violent relationship?—Fear of retribution | 100 | 95 | 95 |
| Which of the following are reasons an IPV victim may not be able to leave a violent relationship?—Financial dependence on the perpetrator | 95 | 100 | 100 |
| Which of the following are reasons an IPV victim may not be able to leave a violent relationship?—Religious beliefs | 85 | 100 | 100 |
| Which of the following are reasons an IPV victim may not be able to leave a violent relationship?—Children’s needs | 95 | 100 | 100 |
| Which of the following are reasons an IPV victim may not be able to leave a violent relationship?—Love for one’s partner | 90 | 100 | 100 |
| Which of the following are reasons an IPV victim may not be able to leave a violent relationship?—Isolation | 90 | 100 | 95 |
| Which of the following are the most appropriate ways to ask about IPV?—“Has your partner ever hurt or threatened you?” | 90 | 85 | 80 |
| Which of the following are the most appropriate ways to ask about IPV?—“Has your partner ever hit or hurt you?” | 50 | 65 | 50 |
| Which of the following is/are generally true?—There are common, non-injury presentations of abused patients | 90 | 95 | 80 |
| Which of the following is/are generally true?—There are behavioral patterns in couples that may indicate IPV | 95 | 90 | 100 |
| Which of the following is/are generally true?—Specific areas of the body are most often targeted in IPV cases | 70 | 65 | 85 |
| Which of the following is/are generally true?—There are common injury patterns associated with IPV | 85 | 75 | 90 |
| Which of the following is/are generally true?—Injuries in different stages of recovery may indicate abuse | 90 | 95 | 80 |
| Please label the following descriptions of the behaviors and feelings of patients with a history of IPV with the appropriate stage of change.—Begins making plans for leaving the abusive partner | 89.5 | 89.5 | 100 |
| Please label the following descriptions of the behaviors and feelings of patients with a history of IPV with the appropriate stage of change.—Denies there’s a problem | 94.7 | 10 | 80 |
| Please label the following descriptions of the behaviors and feelings of patients with a history of IPV with the appropriate stage of change.—Begins thinking the abuse is not their own fault | 89.5 | 94.7 | 80 |
| Please label the following descriptions of the behaviors and feelings of patients with a history of IPV with the appropriate stage of change.—Continues changing behaviors | 68.4 | 94.7 | 85 |
| Please label the following descriptions of the behaviors and feelings of patients with a history of IPV with the appropriate stage of change.—Obtains order(s) for protection | 68.4 | 89.5 | 80 |
| Questions | Pre | Post Immediate | Post One Year | p-Value |
|---|---|---|---|---|
| Legal Requirements | ||||
| I am aware of legal requirements in this state regarding reporting of suspected cases of: (a) IPV | 3.42 (1.5) b | 5.32 (1.34) a | 5.11 (1.37) a | 0.0001 |
| I am aware of legal requirements in this state regarding reporting of suspected cases of: (b) child abuse | 3.95 (1.75) b | 5.37 (1.34) a | 5.16 (1.34) a | 0.002 |
| I am aware of legal requirements in this state regarding reporting of suspected cases of: (c) elder abuse | 3.89 (1.73) b | 5.37 (1.34) a | 5.21 (1.32) a | 0.008 |
| I comply with the Joint Commission standards that require assessment for IPV. | 3.78 (1.11) b | 5.22 (1.26) a | 4.94 (1.51) a | 0.006 |
| Self Efficacy | ||||
| I ask all new patients about abuse in their relationships. | 2.45 (1.28) b | 4.05 (1.57) a | 3.70 (1.26) a | 0.0003 |
| I am capable of identifying IPV without asking my patient about it. ** | 4.47 (1.07) b | 3.47 (1.22) a | 3.7 (1.08) a | 0.005 |
| I feel comfortable discussing IPV with my patients. | 3.95 (1.27) b | 5.58 (1.07) a | 5.37 (1.01) a | 0.0003 |
| I am able to gather the necessary information to identify IPV as the underlying cause of patient illnesses (e.g., depression, migraines). | 3.79 (1.13) b | 5.21 (1.03) a | 5.00 (1.00) a | 0.0001 |
| I can match therapeutic interventions to an IPV patient’s readiness to change. | 4.11 (0.74) b | 5.11 (1.33) a | 4.63 (1.26) ab | 0.025 |
| I can recognize victims of IPV by the way they behave. ** | 4.11 (1.41) | 3.53 (1.02) | 3.79 (0.85) | 0.176 |
| Item | Time | p Value | ||
|---|---|---|---|---|
| Pre | Post Immediate | Post One Year | ||
| a. Injuries | 1.77 (0.73) b | 3.46 (0.97) a | 3.15 (0.80) a | 0.0001 |
| b. Chronic pelvic pain | 1.20 (0.42) b | 3.00 (1.41) a | 2.70 (0.82) a | 0.0001 |
| c. Irritable bowel syndrome | 1.33 (0.49) b | 2.33 (1.07) a | 2.08 (0.51) a | 0.004 |
| d. Headaches | 1.25 (0.45) b | 2.33 (1.07) a | 2.25 (0.45) a | 0.001 |
| e. Depression/Anxiety | 1.77 (0.83) b | 2.92 (1.55) a | 3.38 (1.04) a | 0.0001 |
| f. Hypertension | 1.23 (0.44) b | 1.38 (0.51) b | 1.85 (0.69) a | 0.032 |
| g. Eating disorders | 1.56 (0.73) b | 2.78 (1.20) a | 2.89 (1.27) a | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takov, V.; Harnden, A.; Rummel, K.; Burnell, M.; McMann, S.; Wargel, C.E.; Seelbach, C.; McQuiston, J.; Brannan, G.D. Evaluation of a Community Hospital-Based Residencies’ Intimate Partner Violence Education by a Domestic Violence Shelter Expert. Int. J. Environ. Res. Public Health 2023, 20, 5685. https://doi.org/10.3390/ijerph20095685
Takov V, Harnden A, Rummel K, Burnell M, McMann S, Wargel CE, Seelbach C, McQuiston J, Brannan GD. Evaluation of a Community Hospital-Based Residencies’ Intimate Partner Violence Education by a Domestic Violence Shelter Expert. International Journal of Environmental Research and Public Health. 2023; 20(9):5685. https://doi.org/10.3390/ijerph20095685
Chicago/Turabian StyleTakov, Veronica, Ashley Harnden, Kegan Rummel, Mariah Burnell, Shannon McMann, Carmen E. Wargel, Corie Seelbach, James McQuiston, and Grace D. Brannan. 2023. "Evaluation of a Community Hospital-Based Residencies’ Intimate Partner Violence Education by a Domestic Violence Shelter Expert" International Journal of Environmental Research and Public Health 20, no. 9: 5685. https://doi.org/10.3390/ijerph20095685
APA StyleTakov, V., Harnden, A., Rummel, K., Burnell, M., McMann, S., Wargel, C. E., Seelbach, C., McQuiston, J., & Brannan, G. D. (2023). Evaluation of a Community Hospital-Based Residencies’ Intimate Partner Violence Education by a Domestic Violence Shelter Expert. International Journal of Environmental Research and Public Health, 20(9), 5685. https://doi.org/10.3390/ijerph20095685





