Development, Implementation and Evaluation of an Acute Care Physical Therapy ‘Float’ Placement during the COVID-19 Pandemic: A Case Report
Abstract
1. Introduction
2. Methods
2.1. Authors
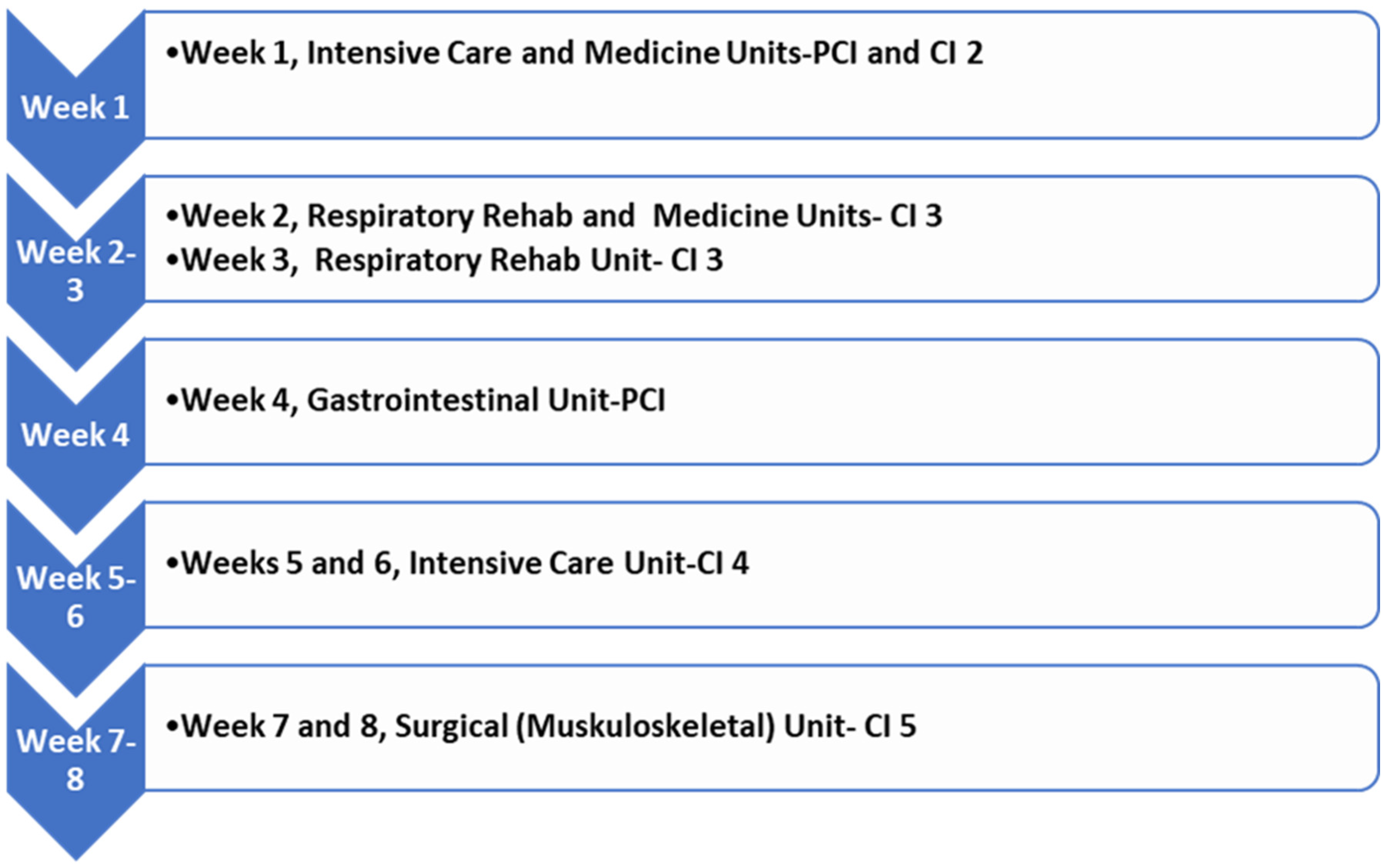
2.2. Placement Development
2.3. Measures
3. Results
- Theme 1. Clinical Instructor and Student Attributes
“...the student and Clinical Instructor have to be: Open minded, able to adapt and adjust, be open to delivering and receiving feedback openly and quickly.”—PCI
“Student would need to be flexible, adaptable. Would need to be comfortable seeing a wide variety of patients across various settings and use a variety of skill sets.”—CI 4
“Perhaps consider this model for an earlier placement where the benchmarks and expectations on the evaluations are not as high.”—CI 5
“Students need to prepare for each unit as they would for the start of a new placement and need to quickly adapt when moving across units. CIs need to be able to facilitate students’ learning and feedback quickly due to a short timeframe.”—Student
- Theme 2. Increased Feasibility
“This model gave me the opportunity to support a student placement, which would have been impossible in the traditional model.”—PCI
“The model makes it more feasible to offer a placement.”—CI 4
For this placement, it was “much more feasible to be able to commit to a shorter supervision period”.—CI 5
“In the future, I would offer supervision to a student in this model—especially being a first time CI it would be great to have a team of experienced CIs to share and assist the teaching.”—Student
- Theme 3. Varied Exposure
An expected opportunity was the... “Enhanced exposure to other hospital areas/experiences, enhanced exposure to different CIs and skill sets within PT scope (and) identification of common skills that are applied to all areas to broaden depth/scope of understanding of what it’s like to work in hospital”.—CI 3
“Student could be exposed to many settings/patient populations in one placement period.”—CI 4
“The key takeaway for me is that I’m really thankful to have the opportunity to practice all my acute care skills with supervision—being across so many units I got to learn and practice chest physio, suctioning, ventilators, oxygen titration, early mobilization, exercises and discharge planning. I think having the opportunity to practice everything you learn is fundamental to being a well-rounded clinician.”—Student
“It’s great exposure to many units as mentioned above. Also, if one unit is not a student’s strength, it’s nice the student has the opportunity to practice in another unit to be more comfortable and demonstrate their strengths and skill.”—Student
- Theme 4. Central Communication and Resources
“I would consider a brief weekly meeting amongst all instructors working with the student and identify ways to streamline paperwork.”—CI 2
“Having 1 point contact for the placement organization and for the evaluation was key to the success of this model.”—CI 4
“Vital to have a point contact for the placement. Would not have been able to evaluate just based on 2 weeks, so it was important that there was one person that had oversight over the entire 8 week placement that did the evaluation.”—CI 5
“having a specific outline of what the student needs to review before the rotation to shorten onboarding of each unit [would be beneficial]…. [and] perhaps some sort of handoff between CIs—assist with transition between units and continue on the goals from the previous unit; the CI will also have more support between each other with this communication process.”—Student
- Theme 5. Organization
“I would, in the future, try to match the areas a bit better so that the 2 weeks were not such extreme changes in caseload and focus.”—CI 1
In the future placement organization should ‘consider a graduated approach to working with patients, from less medically complex to more medically complex’.—CI 2
“Suggest aligning the settings within the placement blocks to they are somewhat similar. This may help with carryover of skills.”—CI 5
“2 weeks is a good minimum time on a unit; 2.5 or 3 weeks would be great (0.5/1 week for intro, 1 week to practice, 1 week for mastery/independence).”—Student
- Theme 6. Managing Expectations
“The CIs need to identify realistic learning goals and patients for the student.”—CI 2
A potential barrier expected with this model was the “Reduced time not allowing for full development of student skill set and independence”.—CI 3
The clinical instructor “needs to be able to manage their expectations and goals and have these set early on”.—CI 5
“This was my first acute, inpatient placement, so I was nervous about not being quick enough to keep up with the expectations when moving unit to unit.”—Student
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Learning Goals
- (1)
- Be able to list the components of and perform a subjective assessment and understand how that subjective assessment is adapted based on unit by 2 October 2020.
- (2)
- Be able to list the components of and perform an objective assessment and understand how that objective assessment is adapted based on unit by 2 October 2020.
- (3)
- Able to set up patient room for mobility in all settings covered in placement with minimal to no cueing by 2 October 2020.
- (4)
- Able to understand and identify appropriate treatment goals and plan for at least six patients by 2 October 2020.
- (5)
- Able to identify an appropriate discharge destination and understand the discharge steps for patients across units.
Appendix B. Reflection Questions Provided to CIs and Student
- Given the unique placement model, did you have any expectations prior to the placement start? Please explain what these were.
- (6)
- Were there specific expectations you had of the student?
- (7)
- Were there specific expectations you have of the overall experience?
- (8)
- What potential barriers did you expect with this placement model?
- (9)
- What potential opportunities did you expect with this placement model?
- (10)
- Please describe the placement experience (a) week one (b) week two
- (11)
- Did your experience align with your expectations of this model?
- (12)
- What are some of your general reflections on this placement model and the overall experience?
- (13)
- What worked well with the organization and execution of the placement (1) for the student and (2) for the Clinical Instructor
- (14)
- What would you modify with the organization and execution of the placement to improve the overall experience (1) for the student and (2) for the Clinical Instructor?
- (15)
- Are there any specific qualities that you think a (1) student (2) Clinical Instructor should develop/possess to assist in the delivery and execution of this placement model?
- (16)
- Would you be involved in a placement model that is the same or similar to this in the future? Please expand on your response.
References
- World Confederation for Physical Therapy (WCPT). Education Policy Statement. 2019. Available online: https://world.physio/sites/default/files/2020-04/PS-2019-Education.pdf (accessed on 20 December 2022).
- World Confederation for Physical Therapy (WCPT). Physiotherapist Education Framework. 2021. Available online: https://world.physio/sites/default/files/2021-07/Physiotherapist-education-framework-FINAL.pdf (accessed on 20 December 2022).
- Canadian Council for Physiotherapy University Programs (CCPUP). National Physiotherapy Entry-to-Practice Curriculum Guidelines. 2019. Available online: https://peac-aepc.ca/pdfs/Resources/Competency%20Profiles/CCPUP%20Curriculum%20Guidelines%202019.pdf (accessed on 20 December 2022).
- Physiotherapy Education Accreditation Canada (PEAC). Accreditation Standards for Canadian Entry-to Practice Physiotherapy Education. 2020. Available online: https://peac-aepc.ca/pdfs/Accreditation/Accreditation%20Standards/Accreditation-Standards-for-Canadian-Entry-to-Practice-Physiotherapy-Education-Programs-(2020).pdf (accessed on 20 December 2022).
- Smith, P.M.; Corso, L.N.; Cobb, N. The perennial struggle to find clinical placement opportunities: A Canadian national survey. Nurse Educ. Today 2010, 30, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Rodger, S.; Webb, G.; Devitt, L.; Gilbert, J.; Wrightson, P.; McMeeken, J. Clinical Education and Practice Placements in the Allied Health Professions: An International Perspective. J. Allied Health 2008, 37, 53–62. [Google Scholar] [PubMed]
- Davies, R.; Hanna, E.; Cott, C. “They put you on your toes”: Physical Therapists’ Perceived Benefits from and Barriers to Supervising Students in the Clinical Setting. Physiother. Can. 2011, 63, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.; Manns, P.; Beaupre, L. To Supervise or Not to Supervise a Physical Therapist Student: A National Survey of Canadian Physical Therapists. J. Phys. Ther. Educ. 2015, 29, 58–67. [Google Scholar] [CrossRef]
- Hall, M.; Poth, C.; Manns, P.; Beaupre, L. An Exploration of Canadian Physiotherapists’ Decisions about Whether to Supervise Physiotherapy Students: Results from a National Survey. Physiother. Can. 2016, 68, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Blakely, C.; Rigg, J.; Joynson, K.; Oldfield, S. Supervision models in a 2:1 acute care placement. Br. J. Occup. Ther. 2009, 72, 515–517. [Google Scholar] [CrossRef]
- Ladyshewsky, R.K. Enhancing Service Productivity in Acute Care Inpatient Settings Using a Collaborative Clinical Education Model. Phys. Ther. 1995, 75, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Mori, B.; Coleman, J.; Knott, K.; Newman, K.; O’Connor, A. Designing, Implementing, and Evaluating a Practice Tutor Internship Model during an Acute Care Clinical Internship. Physiother. Can. 2020, 72, 177–191. [Google Scholar] [CrossRef] [PubMed]
- Vassos, S.; Harms, L.; Rose, D. The Value of Mixing It Up: Student Experiences of a Multi-Modal Approach to Supervision on Placement. Br. J. Soc. Work 2019, 49, 1274–1295. [Google Scholar] [CrossRef]
- Sen-Crowe, B.; Sutherland, M.; McKenney, M.; Elkbuli, A. A Closer Look Into Global Hospital Beds Capacity and Resource Shortages during the COVID-19 Pandemic. J. Surg. Res. 2021, 260, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Bennett, R. Clinical education: Perceived abilities/qualities of clinical educators and team supervision of students. Physiotherapy 2003, 89, 432–440. [Google Scholar] [CrossRef]
- Lekkas, P.; Larsen, T.; Kumar, S.; Grimmer, K.; Nyland, L.; Chipchase, L.; Jull, G.; Buttrum, P.; Carr, L.; Finch, J. No model of clinical education for physiotherapy students is superior to another: A systematic review. Aust. J. Physiother. 2007, 53, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.; Sendelbach, S.; Missal, B.; Fliss, J.; Gaillard, P. Staffing patterns of scheduled unit staff nurses vs. float pool nurses: A pilot study. Medsurg. Nurs. 2012, 21, 27–32, 39. [Google Scholar] [PubMed]
- World Health Organization (WHO). WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 20 December 2022).
- Mori, B.; Norman, K.E.; Brooks, D.; Herold, J.; Beaton, D.E. Evidence of reliability, validity, and practicality for the Canadian Physiotherapy Assessment of Clinical Performance. Physiother. Can. 2016, 68, 156–169. [Google Scholar] [CrossRef] [PubMed]
- Thorne, S.; Kirkham, S.R.; MacDonald-Emes, J. Interpretive description: A noncategorical qualitative alternative for developing nursing knowledge. Res. Nurs. Health 1997, 20, 169–177. [Google Scholar] [CrossRef]
- Thorne, S.; Kirkham, S.R.; O’Flynn-Magee, K. The analytic challenge in interpretive description. Int. J. Qual. Methods 2004, 3, 1–11. [Google Scholar] [CrossRef]
- Thorne, S. Interpretive Description: Qualitative Research for Applied Practice; Routledge: Oxfordshire, UK, 2016. [Google Scholar]
- Olsen, N.R.; Bradley, P.; Lomborg, K.; Nortvedt, M.W. Evidence based practice in clinical physiotherapy education: A qualitative interpretive description. BMC Med. Educ. 2013, 13, 52. [Google Scholar] [CrossRef] [PubMed]
- Candela, A.G. Exploring the function of member checking. Qual. Rep. 2019, 24, 619–628. [Google Scholar] [CrossRef]
| Phase | Tip | Consideration |
|---|---|---|
| Organization of Placement (1–5) | 1. We recommend the site plan the placement early and include a minimum of two consecutive weeks for each rotation if possible. | Attempt to include CIs that work in similar units to allow transfer of skills from one rotation to the next and consider complexities of units and patient trajectory through the site. |
| 2. We recommend the site provide information related to placement organization including timing of rotations and units to the university program. Ideally, this information is made available to the student in advance of the placement match. | Helps program to understand placement organization and student to self-identify required qualities to maximize success on placement and prepare for the types of clinical settings. | |
| 3. We recommend the site designate roles for supervision including the role of the PCI. | Identify one primary clinical instructor to act as a point contact and oversee evaluations and all communication for the student, program and all supervising CIs. | |
| 4. Following student assignment, we recommend the PCI and student identify overarching goals that can be applied to all rotations. | Identification of common learning goals across units will assist in evaluation of the clinical placement. | |
| 5. We recommend the CIs prepare an outline for each rotation and suggest resources that will assist the student with onboarding. | Planning an outline for each rotation allows the student to prepare for placement and content that will be covered. | |
| Execution of Placement (6–10) | 6. We recommend the PCI and student review and modify overarching goals and the CI and student review the placement outline at the beginning of each rotation. | Allows revisions to be made to the overall placement goals and learning objectives within each rotation based on caseload and potential learning opportunities. |
| 7. We recommend the CI include one to two days of orientation at the beginning of each rotation. | Orientation to a unit and unit-specific protocols and caseload allows the student and CI to acclimate to learning environment, personalities, and associated processes. | |
| 8. We recommend the PCI, CIs and student ensure communication and planning opportunities for frequent and timely feedback at the beginning of each placement rotation. | Assists in managing expectations and review of overarching goals. Providing and receiving timely feedback is important when placement rotations are shorter in duration than a typical placement. | |
| 9. We recommend the PCI, CIs and student plan transition meetings between placement rotations with opportunities to provide feedback. | Allows CIs and students to review skills that have been covered/developed in each placement rotation and areas that require growth. | |
| 10. We recommend the PCI and CI plan communications to ensure evaluations are informed by supervising CIs. | Ensures evaluations are reflective of all CI feedback.Program can support to ensure that all CIs are aware of expected benchmarks for the respective placement period. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhir, J.; Connell, A.; McCaughan, M.; Hatzoglou, D.; Ajami, D.; Fursman, A.; Wojkowski, S.; Kho, M.E. Development, Implementation and Evaluation of an Acute Care Physical Therapy ‘Float’ Placement during the COVID-19 Pandemic: A Case Report. Int. J. Environ. Res. Public Health 2023, 20, 6038. https://doi.org/10.3390/ijerph20116038
Dhir J, Connell A, McCaughan M, Hatzoglou D, Ajami D, Fursman A, Wojkowski S, Kho ME. Development, Implementation and Evaluation of an Acute Care Physical Therapy ‘Float’ Placement during the COVID-19 Pandemic: A Case Report. International Journal of Environmental Research and Public Health. 2023; 20(11):6038. https://doi.org/10.3390/ijerph20116038
Chicago/Turabian StyleDhir, Jasdeep, Amy Connell, Magda McCaughan, Diana Hatzoglou, Daana Ajami, Andrea Fursman, Sarah Wojkowski, and Michelle E. Kho. 2023. "Development, Implementation and Evaluation of an Acute Care Physical Therapy ‘Float’ Placement during the COVID-19 Pandemic: A Case Report" International Journal of Environmental Research and Public Health 20, no. 11: 6038. https://doi.org/10.3390/ijerph20116038
APA StyleDhir, J., Connell, A., McCaughan, M., Hatzoglou, D., Ajami, D., Fursman, A., Wojkowski, S., & Kho, M. E. (2023). Development, Implementation and Evaluation of an Acute Care Physical Therapy ‘Float’ Placement during the COVID-19 Pandemic: A Case Report. International Journal of Environmental Research and Public Health, 20(11), 6038. https://doi.org/10.3390/ijerph20116038





