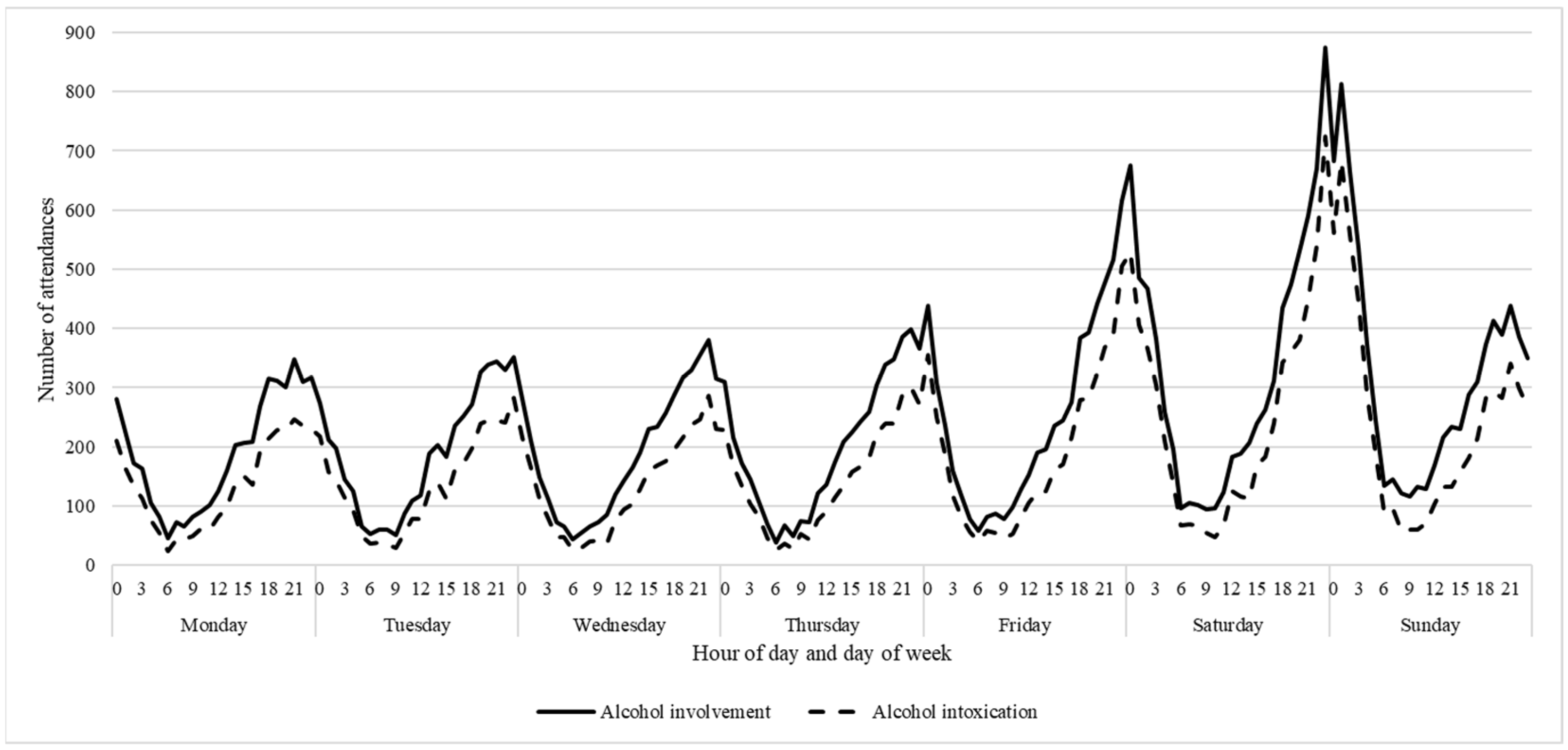
Description of Trends over the Week in Alcohol-Related Ambulance Attendance Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Alcohol Involvement
2.3. Design and Analysis
3. Results
Sensitivity Analysis
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Alcohol. 2021. Available online: https://www.who.int/health-topics/alcohol#tab=tab_1 (accessed on 26 May 2021).
- Griswold, M.G.; Fullman, N.; Hawley, C.; Arian, N.; Zimsen, S.R.M.; Tymeson, H.D.; Venkateswaran, V.; Tapp, A.D.; Forouzanfar, M.H.; Salama, J.S.; et al. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar] [CrossRef] [PubMed]
- Babor, T.F.; Casswell, S.; Graham, K.; Huckle, T.; Livingston, M.; Österberg, E.; Rehm, J.; Room, R.; Rossow, I.; Sornpaisarn, B. Alcohol: No Ordinary Commodity: RESEARCH and Public Policy; Oxford University Press: Oxford, UK, 2022. [Google Scholar]
- Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2019. 2020. Available online: https://www.aihw.gov.au/reports/illicit-use-of-drugs/national-drug-strategy-household-survey-2019/contents/summary (accessed on 26 May 2021).
- Coomber, K.; de Andrade, D.; Puljević, C.; Ferris, J.; Livingston, M.; Taylor, N.; Clough, A.; Miller, P.G. The impact of liquor legislation changes on police-recorded serious assault in Queensland, Australia. Drug Alcohol Rev. 2021, 40, 717–727. [Google Scholar] [CrossRef] [PubMed]
- Curtis, A.; Coomber, K.; Droste, N.; Hyder, S.; Palmer, D.; Miller, P.G. Effectiveness of community-based interventions for reducing alcohol-related harm in two metropolitan and two regional sites in Victoria, Australia. Drug Alcohol Rev. 2017, 36, 359–368. [Google Scholar] [CrossRef] [PubMed]
- De Andrade, D.; Coomber, K.; Livingston, M.; Taylor, N.; Moayeri, F.; Miller, P.G.; Ferris, J.; Puljević, C.; Mayshak, R.; Scott, D. The impact of late-night alcohol restrictions on ambulance call-outs in entertainment precincts. Drug Alcohol Rev. 2021, 40, 708–716. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.G.; Droste, N.; Baker, T.; Gervis, C. Last drinks: A study of rural emergency department data collection to identify and target community alcohol-related violence. Emerg. Med. Australas. 2015, 27, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Young, D.J.; Stockwell, T.; Cherpitel, C.J.; Ye, Y.; Macdonald, S.; Borges, G.; Giesbrecht, N. Emergency room injury presentations as an indicator of alcohol-related problems in the community: A multilevel analysis of an international study. J. Stud. Alcohol Drug 2004, 65, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Coghlan, S.; Sutherland, P.; Millsteed, M. Temporal Distribution of Crime in Victorian Night-Time Entertainment Precincts; Crime Statistics Agency: Melbourne, Australia, 2016.
- Nepal, S.; Kypri, K.; Attia, J.; Chikritzhs, T.; Miller, P.G. Indicators for estimating trends in alcohol-related assault: Evaluation using police data from Queensland, Australia. Inj. Prev. 2019, 25, 444–447. [Google Scholar] [CrossRef] [PubMed]
- Dietze, P.M.; McElwee, P.; Health, P.; Jonas, H.; Hanlin, K.; Cvetkovski, S. The Victorian Alcohol Statistics Handbook Volume 2: Alcohol-Related Serious Road Injury and Assault in Victoria 1992–1999; Turning Point Alcohol and Drug Centre: Melbourne, VI, Australia, 2001. [Google Scholar]
- Rumbold, G.; Malpass, A.; Lang, E.; Cvetkovski, S.; Kelly, W. An Evaluation of the Geelong Local Industry Accord: Final Report; Turning Point Alcohol and Drug Centre Inc.: Melbourne, Australia, 1998. [Google Scholar]
- Chikritzhs, T.; Stockwell, T.; Heale, P.; Dietze, P.; Webb, M. National Alcohol Indicators Project Technical Report No. 2: Trends in Alcohol-Related Road Injury in Australia, 1990–1997; National Drug Research Institute, Curtin University of Technology: Perth, Australia, 2000. [Google Scholar]
- Coomber, K.; Curtis, A.; Vandenberg, B.; Miller, P.G.; Heilbronn, C.; Matthews, S.; Smith, K.; Wilson, J.; Moayeri, F.; Mayshak, R. Aggression and violence at ambulance attendances where alcohol, illicit and/or pharmaceutical drugs were recorded: A 5-year study of ambulance records in Victoria, Australia. Drug Alcohol Depend. 2019, 205, 107685. [Google Scholar] [CrossRef] [PubMed]
- Lubman, D.I.; Matthews, S.; Heilbronn, C.; Killian, J.J.; Ogeil, R.P.; Lloyd, B.; Witt, K.; Crossin, R.; Smith, K.; Bosley, E. The National Ambulance Surveillance System: A novel method for monitoring acute alcohol, illicit and pharmaceutical drug related-harms using coded Australian ambulance clinical records. PLoS ONE 2020, 15, e0228316. [Google Scholar] [CrossRef] [PubMed]
- Masho, S.W.; Bishop, D.L.; Edmonds, T.; Farrell, A.D. Using surveillance data to inform community action: The effect of alcohol sale restrictions on intentional injury-related ambulance pickups. Prev. Sci. 2014, 15, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Quigg, Z.; McGee, C.; Hughes, K.; Russell, S.; Bellis, M.A. Violence-related ambulance call-outs in the North West of England: A cross-sectional analysis of nature, extent and relationships to temporal, celebratory and sporting events. Emerg. Med. J. 2017, 34, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, A.; Strang, L.; Stepanek, M.; Giacomantonio, C.; Boyle, A. Using Ambulance Data for Violence Prevention; RAND Corporation: Cambridge, UK, 2017. [Google Scholar]
- Coomber, K.; Miller, P.G.; Livingston, M.; Xantidis, L. Larger regional and rural areas in Victoria, Australia, experience more alcohol-related injury presentations at emergency departments. J. Rural Health 2013, 29, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.G.; Coomber, K.; Staiger, P.; Zinkiewicz, L.; Toumbourou, J.W. Review of rural and regional alcohol research in Australia. Aust. J. Rural Health 2010, 18, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Denson, T.F.; Aviles, F.E.; Pollock, V.E.; Earleywine, M.; Vasquez, E.A.; Miller, N. The effects of alcohol and the salience of aggressive cues on triggered displaced aggression. Aggress. Behav. 2008, 34, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Denson, T.F.; Blundell, K.A.; Schofield, T.P.; Schira, M.M.; Krämer, U.M. The neural correlates of alcohol-related aggression. Cogn. Affect. Behav. Neurosci. 2018, 18, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Mason, R.; Roberts, A.; Spaight, R.; Shaw, D.; Whitley, G.A.; Hogue, T.E.; Siriwardena, A.N.; Rogers, J.; Law, G.R. Ambulance attendance for substance and/or alcohol use in a pandemic: Interrupted time series analysis of incidents. Drug Alcohol Rev. 2022, 41, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, R.; La Cecilia, O.; Boari, B.; Steliu, J.; Michelini, V.; Carli, P.; Zanotti, C.; Bigoni, M.; Gallerani, M. Circadian pattern of emergency calls: Implications for ED organization. Am. J. Emerg. Med. 2002, 20, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.; Coomber, K.; Ferris, J.; Burn, M.; Vakidis, T.; Livingston, M.; Droste, N.; Taylor, N.; Puljević, C.; de Andrade, D.; et al. QUeensland Alcohol-Related Violence and Night Time Economy Monitoring (QUANTEM): Final Report; Deakin University: Geelong, Australia, 2019. [Google Scholar]
| Season | Summer | Autumn | Winter | Spring | ||||
| Fri 6:00 p.m. to Sat 3:59 a.m. | Fri 6:00 p.m. to 3:59 a.m. | Fri 6:00 p.m. to Sun 3:59 a.m. | Fri 6:00 p.m. to Sat 3:59 a.m. | |||||
| Sat 6:00 p.m. to Sun 4:59 a.m. | Sat 5:00 p.m. to Sun 4:59 a.m. | Sat 5:00 p.m. to Sun 4:59 a.m. | Sat 6:00 p.m. to Sun 4:59 a.m. | |||||
| Region | Metropolitan | Regional | ||||||
| Fri 6:00 p.m. to Sat 3:59 a.m. | Fri 6:00 p.m. to Sat 3:59 a.m. | |||||||
| Sat 5:00 p.m. to Sun 4:59 a.m. | Sat 6:00 p.m. to Sun 4:59 a.m. | |||||||
| Gender | Males | Females | ||||||
| Fri 6:00 p.m. to Sat 3:59 a.m. | Fri 6:00 p.m. to Sat 4:59 a.m. | |||||||
| Sat 6:00 p.m. to Sun 4:59 a.m. | Sat 6:00 p.m. to Sun 4:59 a.m. | |||||||
| Age | 18–24 years | 25–29 years | 30–39 years | 40–49 years | 50–59 years | 60+ years | ||
| Fri 9:00 p.m. to Sat 5:59 a.m. | Fri 7:00 p.m. to Sat 5:59 a.m. | Fri 6:00 p.m. to Sat 3:59 a.m. | Fri 6:00 p.m. to Sat 2:59 a.m. | Fri 5:00 p.m. to Sat 0:59 a.m. | Fri 6:00 p.m. to Sat 0:59 a.m. | |||
| Sat 7:00 p.m. to Sun 7:59 a.m. | Sat 6:00 p.m. to Sun 5:59 a.m. | Sat 6:00 p.m. to Sun 4:49 a.m. | Sat 5:00 p.m. to Sun 3:59 a.m. | Sat 6:00 p.m. to Sun 2:59 a.m. | Sat 5:00 p.m. to Sun 1:59 a.m. | |||
| Season | Summer | Autumn | Winter | Spring | ||||
| Fri 6:00 p.m. to 2:59 a.m. | Fri 6:00 p.m. to 3:59 a.m. | Fri 6:00 p.m. to Sun 3:59 a.m. | Fri 5:00 p.m. to Sat 4:59 a.m. | |||||
| Sat 6:00 p.m. to Sun 4:59 a.m. | Sat 5:00 p.m. to Sun 4:59 a.m. | Sat 5:00 p.m. to Sun 4:59 a.m. | Sat 6:00 p.m. to Sun 4:59 a.m. | |||||
| Region | Metropolitan | Regional | ||||||
| Fri 6:00 p.m. to Sat 3:59 a.m. | Fri 6:00 p.m. to Sat 3:59 a.m. | |||||||
| Sat 5:00 p.m. to Sun 4:49 a.m. | Sat 6:00 p.m. to Sun 4:59 a.m. | |||||||
| Gender | Males | Females | ||||||
| Fri 6:00 p.m. to Sat 3:59 a.m. | Fri 6:00 p.m. to Sat 3:59 a.m. | |||||||
| Sat 5:00 p.m. to Sun 4:49 a.m. | Sat 6:00 p.m. to Sun 4:59 a.m. | |||||||
| Age | 18–24 years | 25–29 years | 30–39 years | 40–49 years | 50–59 years | 60+ years | ||
| Fri 9:00 p.m. to Sat 5:59 a.m. | Fri 7:00 p.m. to Sat 4:49 a.m. | Fri 6:00 p.m. to Sat 3:59 a.m. | Fri 6:00 p.m. to Sat 2:59 a.m. | Fri 5:00 p.m. to Sat 0:59 a.m. | Fri 6:00 p.m. to Sat 0:59 a.m. | |||
| Sat 7:00 p.m. to Sun 6:59 a.m. | Sat 5:00 p.m. to Sun 5:59 a.m. | Sat 6:00 p.m. to Sun 5:59 a.m. | Sat 5:00 p.m. to Sun 3:59 a.m. | Sat 6:00 p.m. to Sun 2:59 a.m. | Sat 5:00 p.m. to 11:59 p.m. | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coomber, K.; Miller, P.G.; Killian, J.J.; Ogeil, R.P.; Beard, N.; Lubman, D.I.; Baldwin, R.; Smith, K.; Scott, D. Description of Trends over the Week in Alcohol-Related Ambulance Attendance Data. Int. J. Environ. Res. Public Health 2023, 20, 5583. https://doi.org/10.3390/ijerph20085583
Coomber K, Miller PG, Killian JJ, Ogeil RP, Beard N, Lubman DI, Baldwin R, Smith K, Scott D. Description of Trends over the Week in Alcohol-Related Ambulance Attendance Data. International Journal of Environmental Research and Public Health. 2023; 20(8):5583. https://doi.org/10.3390/ijerph20085583
Chicago/Turabian StyleCoomber, Kerri, Peter G. Miller, Jessica J. Killian, Rowan P. Ogeil, Naomi Beard, Dan I. Lubman, Ryan Baldwin, Karen Smith, and Debbie Scott. 2023. "Description of Trends over the Week in Alcohol-Related Ambulance Attendance Data" International Journal of Environmental Research and Public Health 20, no. 8: 5583. https://doi.org/10.3390/ijerph20085583
APA StyleCoomber, K., Miller, P. G., Killian, J. J., Ogeil, R. P., Beard, N., Lubman, D. I., Baldwin, R., Smith, K., & Scott, D. (2023). Description of Trends over the Week in Alcohol-Related Ambulance Attendance Data. International Journal of Environmental Research and Public Health, 20(8), 5583. https://doi.org/10.3390/ijerph20085583







