Fatigue on Waking, Insomnia, and Workplace Relationship Problems May Help to Detect Suicidal Ideation among New Middle-Aged Primary Care Patients: A 6-Month Prospective Study in Japan
Abstract
1. Introduction
2. Materials and Methods
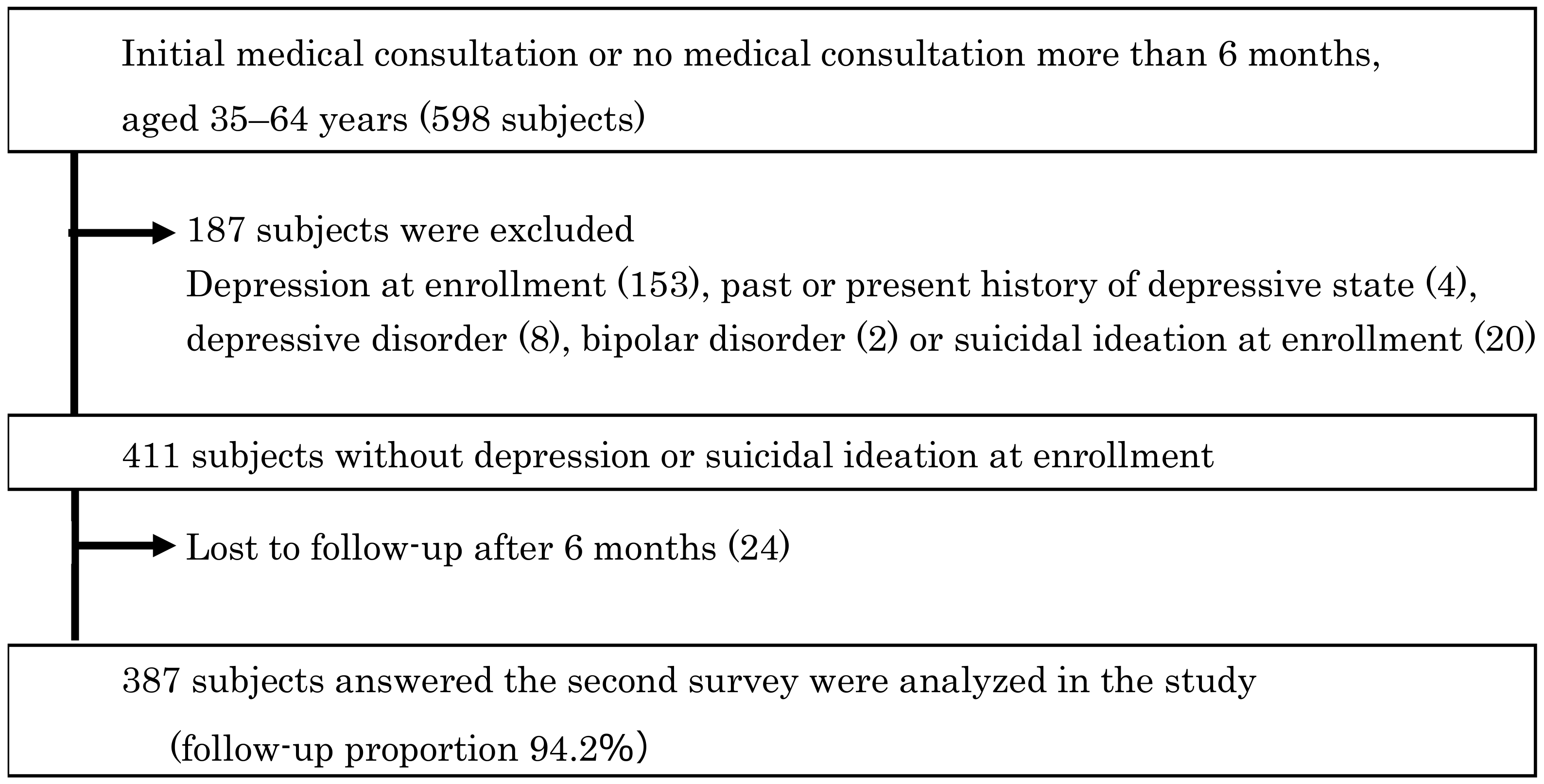
2.1. Study Subjects
2.2. Information Collection
2.3. Definition of Poor Sleep and Fatigue on Waking
2.4. Case Definition
2.5. Data Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blumenthal, D.; Causino, N.; Chang, Y.C.; Culpepper, L.; Marder, W.; Saglam, D.; Stafford, R.; Starfield, B. The duration of ambulatory visits to physicians. J. Fam. Pract. 1999, 48, 264–271. [Google Scholar] [PubMed]
- Goldsmith, S.K.; Pellmar, T.C.; Kleinman, A.M.; Bunney, W.E. (Eds.) Reducing Suicide: A National Imperative; The National Academic Press: Washington, DC, USA, 2002; pp. 339–342. [Google Scholar]
- Ministry of Health, Labour and Welfare of Japan. Patient’s Behavior Survey 2020. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/jyuryo/20/index.html (accessed on 14 February 2023). (In Japanese).
- Kekka no Gaiyo (Summary of Results), Ministry of Health, Labour and Welfare of Japan. Patient’s Behavior Survey 2020. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/jyuryo/20/dl/kekka-gaiyo.pdf (accessed on 14 February 2023). (In Japanese).
- Paykel, E.S.; Myers, J.K.; Lindenthal, J.J.; Tanner, J. Suicidal feelings in the general population: A prevalence study. Br. J. Psychiatry J. Ment. Sci. 1974, 124, 460–469. [Google Scholar] [CrossRef] [PubMed]
- Crosby, A.E.; Cheltenham, M.P.; Sacks, J.J. Incidence of suicidal ideation and behavior in the United States, 1994. Suicide Life-Threat. Behav. 1999, 29, 131–140. [Google Scholar] [PubMed]
- Vassilas, C.A.; Morgan, H.G. General practitioners’ contact with victims of suicide. BMJ 1993, 307, 300–301. [Google Scholar] [CrossRef]
- Luoma, J.B.; Martin, C.E.; Pearson, J.L. Contact with mental health and primary care providers before suicide: A review of the evidence. Am. J. Psychiatry 2002, 159, 909–916. [Google Scholar] [CrossRef]
- Feldman, M.D.; Franks, P.; Duberstein, P.R.; Vannoy, S.; Epstein, R.; Kravitz, R.L. Let’s not talk about it: Suicide inquiry in primary care. Ann. Fam. Med. 2007, 5, 412–418. [Google Scholar] [CrossRef]
- Stoppe, G.; Sandholzer, H.; Huppertz, C.; Duwe, H.; Staedt, J. Family physicians and the risk of suicide in the depressed elderly. J. Affect. Disord. 1999, 54, 193–198. [Google Scholar] [CrossRef]
- Stoppe, G. Family physicians and their management of suicidal crisis: A qualitative interview study. Eur. Psychiatry 2008, 23 (Suppl. 2), S398–S399. [Google Scholar] [CrossRef]
- Kato, T.A.; Suzuki, Y.; Sato, R.; Fujisawa, D.; Uehara, K.; Hashimoto, N.; Sawayama, Y.; Hayashi, J.; Kanba, S.; Otsuka, K. Development of 2-hour suicide intervention program among medical residents: First pilot trial. Psychiatry Clin. Neurosci. 2010, 64, 531–540. [Google Scholar] [CrossRef]
- Harmer, B.; Lee, S.; Duong, T.H.; Saadabadi, A. Suicidal Ideation; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Busch, K.A.; Fawcett, J.; Jacobs, D.G. Clinical correlates of inpatient suicide. J. Clin. Psychiatry 2003, 64, 14–19. [Google Scholar] [CrossRef]
- Dueweke, A.R.; Bridges, A.J. Suicide interventions in primary care: A selective review of the evidence. Fam. Syst. Health 2018, 36, 289–302. [Google Scholar] [CrossRef]
- Morriss, R.; Gask, L.; Webb, R.; Dixon, C.; Appleby, L. The effects on suicide rates of an educational intervention for front-line health professionals with suicidal patients (the STORM Project). Psychol. Med. 2005, 35, 957–960. [Google Scholar] [CrossRef]
- Rutz, W.; Walinder, J.; Eberhard, G.; Holmberg, G.; von Knorring, A.L.; von Knorring, L.; Wistedt, B.; Aberg-Wistedt, A. An educational program on depressive disorders for general practitioners on Gotland: Background and evaluation. Acta Psychiatr. Scand. 1989, 79, 19–26. [Google Scholar] [CrossRef]
- Boudreaux, E.D.; Jaques, M.L.; Brady, K.M.; Matson, A.; Allen, M.H. The Patient Safety Screener: Validation of a brief suicide risk screener for emergency department settings. Arch. Suicide Res. 2017, 21, 52–61. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Vaze, A.; Rao, S. Clinical diagnosis of depression in primary care: A meta-analysis. Lancet 2009, 374, 609–619. [Google Scholar] [CrossRef]
- Fujieda, M.; Uchida, K.; Ikebe, S.; Kimura, A.; Kimura, M.; Watanabe, T.; Sakamoto, H.; Matsumoto, T.; Uchimura, N. Inquiring about insomnia may facilitate diagnosis of depression in the primary care setting. Psychiatry Clin. Neurosci. 2017, 71, 383–394. [Google Scholar] [CrossRef]
- Rihmer, Z.; Dome, P.; Gonda, X. The role of general practitioners in prevention of depression-related suicides. Neuropsychopharmacol. Hung. 2012, 14, 245–251. [Google Scholar]
- Sokero, T.P.; Melartin, T.K.; Rytsala, H.J.; Leskela, U.S.; Lestela-Mielonen, P.S.; Isometsa, E.T. Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J. Clin. Psychiatry 2003, 64, 1094–1100. [Google Scholar] [CrossRef]
- Rihmer, Z. Depression and Suicidal Behaviour. In International Handbook of Suicide Prevention; O’Connor RC, P.S., Gordon, J., Eds.; John Wiley & Sons, Ltd.: Oxford, UK, 2011; pp. 59–73. [Google Scholar]
- Douglas, G.; Jacobs, E. The Harvard Medical School Guide to Suicide Assessment and Intervention; Jossey-Bass: San Francsico, CA, USA, 1998; pp. 3–590. [Google Scholar]
- Sokero, T.P.; Melartin, T.K.; Rytsala, H.J.; Leskela, U.S.; Lestela-Mielonen, P.S.; Isometsa, E.T. Prospective study of risk factors for attempted suicide among patients with DSM-IV major depressive disorder. Br. J. Psychiatry J. Ment. Sci. 2005, 186, 314–318. [Google Scholar] [CrossRef]
- Riihimäki, K.; Vuorilehto, M.; Melartin, T.; Haukka, J.; Isometsa, E. Incidence and predictors of suicide attempts among primary-care patients with depressive disorders: A 5-year prospective study. Psychol. Med. 2014, 44, 291–302. [Google Scholar] [CrossRef]
- Malik, S.; Kanwar, A.; Sim, L.A.; Prokop, L.J.; Wang, Z.; Benkhadra, K.; Murad, M.H. The association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses: A systematic review and meta-analysis. Syst. Rev. 2014, 3, 18. [Google Scholar] [CrossRef] [PubMed]
- Pigeon, W.R.; Pinquart, M.; Conner, K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J. Clin. Psychiatry 2012, 73, e1160–e1167. [Google Scholar] [CrossRef] [PubMed]
- Kodaka, M.; Matsumoto, T.; Katsumata, Y.; Akazawa, M.; Tachimori, H.; Kawakami, N.; Eguchi, N.; Shirakawa, N.; Takeshima, T. Suicide risk among individuals with sleep disturbances in Japan: A case-control psychological autopsy study. Sleep Med. 2014, 15, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Bishop, T.M.; Walsh, P.G.; Ashrafioun, L.; Lavigne, J.E.; Pigeon, W.R. Sleep, suicide behaviors, and the protective role of sleep medicine. Sleep Med. 2020, 66, 264–270. [Google Scholar] [CrossRef]
- Yoshimasu, K.; Sugahara, H.; Akamine, M.; Kondo, T.; Fujisawa, K.; Tokunaga, S.; Kiyohara, C.; Miyashita, K.; Kubo, C. Sleep disorders and suicidal ideation in Japanese patients visiting a psychosomatic clinic in a university hospital. Sleep Biol. Rhythm. 2006, 4, 137–143. [Google Scholar] [CrossRef]
- Heisel, M.J.; Duberstein, P.R.; Lyness, J.M.; Feldman, M.D. Screening for suicide ideation among older primary care patients. J. Am. Board Fam. Med. 2010, 23, 260–269. [Google Scholar] [CrossRef]
- Kinoshita, Y.; Itani, O.; Otsuka, Y.; Matsumoto, Y.; Nakagome, S.; Osaki, Y.; Higuchi, S.; Maki, J.; Kanda, H.; Kaneita, Y. A nationwide cross-sectional study of difficulty waking up for school among adolescents. Sleep 2021, 44, zsab157. [Google Scholar] [CrossRef]
- Nakai, H.; Yamaguchi, N. Kangonotameno Seishinigaku (Psychiatry for Nursing); Igaku-Shoin: Tokyo, Japan, 2006; pp. 167–170. (In Japanese) [Google Scholar]
- Inoue, A.; Kawakami, N. Interpersonal conflict and depression among Japanese workers with high or low socioeconomic status: Findings from the Japan Work Stress and Health Cohort Study. Soc. Sci. Med. 2010, 71, 173–180. [Google Scholar] [CrossRef]
- General Affairs Division, Social Welfare and War Victims’ Relief Bureau, Ministry of Health, Labour and Welfare in Japan; Community Safety Planning Division, Community Safety Bureau, National Police Agency in Japan. Heiseisanjunen Chuniokeru Jisatsunojokyo (Suicide in Japan). 2018. Available online: https://www.npa.go.jp/safetylife/seianki/jisatsu/H30/H30_jisatunojoukyou.pdf (accessed on 12 March 2023). (In Japanese).
- Office for Policy of Suicide Prevention, Ministry of Health, Labour and Welfare in Japan; Community Safety Planning Division, Community Safety Bureau, National Police Agency in Japan. Reiwagannen Chuniokeru Jisatsunojokyo (Suicide in Japan in 2019). Available online: https://www.npa.go.jp/safetylife/seianki/jisatsu/R02/R01_jisatuno_joukyou.pdf (accessed on 12 March 2023). (In Japanese).
- Office for Policy of Suicide Prevention, Ministry of Health, Labour and Welfare in Japan; Community Safety Planning Division, Community Safety Bureau, National Police Agency in Japan. Reiwaninen Chuniokeru Jisatsunojokyo (Suicide in Japan in 2020). Available online: https://www.npa.go.jp/safetylife/seianki/jisatsu/R03/R02_jisatuno_joukyou.pdf (accessed on 12 March 2023). (In Japanese).
- Office for Policy of Suicide Prevention, Ministry of Health, Labour and Welfare in Japan; Community Safety Planning Division, Community Safety Bureau, National Police Agency in Japan. Reiwasannen Chuniokeru Jisatsunojokyo (Suicide in Japan in 2021). Available online: https://www.npa.go.jp/safetylife/seianki/jisatsu/R04/R3jisatsunojoukyou.pdf (accessed on 12 March 2023). (In Japanese).
- Goldner, E.M.; Jones, W.; Fang, M.L. Access to and waiting time for psychiatrist services in a Canadian urban area: A study in real time. Can. J. Psychiatry 2011, 56, 474–480. [Google Scholar] [CrossRef]
- Clement, S.; Schauman, O.; Graham, T.; Maggioni, F.; Evans-Lacko, S.; Bezborodovs, N.; Morgan, C.; Rusch, N.; Brown, J.S.; Thornicroft, G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2015, 45, 11–27. [Google Scholar] [CrossRef]
- Kubota, Y.; Uchida, K.; Matsumoto, T. Depression awareness and suicide prevention in mental clinic: Community network of primary care doctor and psychiatrist in Fuji City Medical Association. Jpn. J. Psychiatr. Treat. 2015, 30, 449–455. (In Japanese) [Google Scholar]
- Japan Medical Association Mental Health Committee. Depression and suicide countermeasures in Japan. JMA J. 2013, 56, 129–142. [Google Scholar]
- Doi, Y.; Minowa, M.; Uchiyama, M.; Okawa, M.; Kim, K.; Shibui, K.; Kamei, Y. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000, 97, 165–172. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Fukuda, K. Ippanrinshoui ni yakudatu shinri test, SDS-yokuutsusei no sokutei. [Psychological test useful for general physicians, SDS-measurement of depression]. Yamagata J. Med. 1967, 1, 36–42. (In Japanese) [Google Scholar]
- Fukuda, K.; Kobayashi, S. A study on a self-rating depression scale. Psychiatr. Neurol. Jpn. Seishin Shinkeigaku Zasshi 1973, 75, 673–679. (In Japanese) [Google Scholar]
- Zung, W.W. How normal is depression? Psychosomatics 1972, 13, 174–178. [Google Scholar] [CrossRef]
- Biggs, J.T.; Wylie, L.T.; Ziegler, V.E. Validity of the Zung Self-rating Depression Scale. Br. J. Psychiatry J. Ment. Sci. 1978, 132, 381–385. [Google Scholar] [CrossRef]
- Yokoyama, K.; Araki, S.; Kawakami, N.; Tkakeshita, T. Production of the Japanese edition of profile of mood states (POMS): Assessment of reliability and validity. Jpn. J. Public Health Nihon Koshu Eisei Zasshi 1990, 37, 913–918. (In Japanese) [Google Scholar]
- Yokoyama, K.; Araki, S. Nihon Ban POMS Tebiki [Manual for the Japanese Edition of Profile of Mood States]; Kaneko Shobo: Tokyo, Japan, 2010; pp. 1–30. (In Japanese) [Google Scholar]
- Spreen, O.; Strauss, E. Adaptive Behavior and Personality. In A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary, 2nd ed.; Oxford University Press: New York, NY, USA, 1998; pp. 599–659. [Google Scholar]
- SAS Institute Inc. The CORR Procedure. Available online: https://documentation.sas.com/doc/en/pgmsascdc/9.4_3.5/procstat/procstat_corr_examples09.htm (accessed on 12 March 2023).
- Takegami, M.; Suzukamo, Y.; Wakita, T.; Noguchi, H.; Chin, K.; Kadotani, H.; Inoue, Y.; Oka, Y.; Nakamura, T.; Green, J.; et al. Development of a Japanese version of the Epworth Sleepiness Scale (JESS) based on item response theory. Sleep Med. 2009, 10, 556–565. [Google Scholar] [CrossRef]
- Johns, M.W. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 1992, 15, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Zung, W.W. A self-rating depression scale. Arch. Gen. Psychiatry 1965, 12, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Simel, D.L.; Samsa, G.P.; Matchar, D.B. Likelihood ratios with confidence: Sample size estimation for diagnostic test studies. J. Clin. Epidemiol. 1991, 44, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, R.H.; Fletcher, S.W.; Fletcher, G.S. Clinical Epidemiology: The Essentials, 5th ed.; Wolters Kluwer/Lippincott Williams & Wilkins: Baltimore, MD, USA, 2014; pp. 93–151. [Google Scholar]
- Higuchi, S. Conversion Table for Alcohol Beverages Distributed at Training Course for Tobacco and Alcohol Control Held by Ministry of Health, Labour and Welfare in 2010. Available online: https://www.mhlw.go.jp/topics/tobacco/houkoku/dl/100222i.pdf (accessed on 14 February 2023). (In Japanese).
- Hamashima, N. Clinical Studies by Multivariate Analysis; The University of Nagoya Press: Nagoya, Japan, 2000; pp. 23–33. (In Japanese) [Google Scholar]
- Holma, K.M.; Melartin, T.K.; Haukka, J.; Holma, I.A.; Sokero, T.P.; Isometsa, E.T. Incidence and predictors of suicide attempts in DSM-IV major depressive disorder: A five-year prospective study. Am. J. Psychiatry 2010, 167, 801–808. [Google Scholar] [CrossRef]
- Brown, G.K.; Beck, A.T.; Steer, R.A.; Grisham, J.R. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. J. Consult. Clin. Psychol. 2000, 68, 371–377. [Google Scholar] [CrossRef]
- Suominen, K.; Isometsa, E.; Suokas, J.; Haukka, J.; Achte, K.; Lonnqvist, J. Completed suicide after a suicide attempt: A 37-year follow-up study. Am. J. Psychiatry 2004, 161, 562–563. [Google Scholar] [CrossRef]
- Barraclough, B.; Bunch, J.; Nelson, B.; Sainsbury, P. A hundred cases of suicide: Clinical aspects. Br. J. Psychiatry J. Ment. Sci. 1974, 125, 355–373. [Google Scholar] [CrossRef]
- Chynoweth, R.; Tonge, J.I.; Armstrong, J. Suicide in Brisbane: A retrospective psychosocial study. Aust. N. Z. J. Psychiatry 1980, 14, 37–45. [Google Scholar] [CrossRef]
- Skapinakis, P.; Rai, D.; Anagnostopoulos, F.; Harrison, S.; Araya, R.; Lewis, G. Sleep disturbances and depressive symptoms: An investigation of their longitudinal association in a representative sample of the UK general population. Psychol. Med. 2013, 43, 329–339. [Google Scholar] [CrossRef]
- Owusu, J.T.; Doty, S.B.; Adjaye-Gbewonyo, D.; Bass, J.K.; Wilcox, H.C.; Gallo, J.J.; Spira, A.P. Association of sleep characteristics with suicidal ideation and suicide attempt among adults aged 50 and older with depressive symptoms in low- and middle-income countries. Sleep Health 2020, 6, 92–99. [Google Scholar] [CrossRef]
- Rothman, K.J. Epidemiology. An Introduction, 2nd ed.; Oxford University Press: New York, NY, USA, 2012; pp. 1–253. [Google Scholar]
- Silva, I.d.S. Cancer Epidemiology: Principles and Methods; International Agency for Research on Cancer: Lyon, France, 1999; pp. 1–425. [Google Scholar]
- Duggan, C.F.; Sham, P.; Lee, A.S.; Murray, R.M. Can future suicidal behaviour in depressed patients be predicted? J. Affect. Disord. 1991, 22, 111–118. [Google Scholar] [CrossRef]
- Mezuk, B.; Eaton, W.W.; Albrecht, S.; Golden, S.H. Depression and type 2 diabetes over the lifespan: A meta-analysis. Diabetes Care 2008, 31, 2383–2390. [Google Scholar] [CrossRef]
- Rudisch, B.; Nemeroff, C.B. Epidemiology of comorbid coronary artery disease and depression. Biol. Psychiatry 2003, 54, 227–240. [Google Scholar] [CrossRef]
- Hackett, M.L.; Anderson, C.S. Predictors of depression after stroke: A systematic review of observational studies. Stroke A J. Cereb. Circ. 2005, 36, 2296–2301. [Google Scholar] [CrossRef]
- Almeida, O.P.; Draper, B.; Snowdon, J.; Lautenschlager, N.T.; Pirkis, J.; Byrne, G.; Sim, M.; Stocks, N.; Flicker, L.; Pfaff, J.J. Factors associated with suicidal thoughts in a large community study of older adults. Br. J. Psychiatry J. Ment. Sci. 2012, 201, 466–472. [Google Scholar] [CrossRef]
- Kleiman, E.M.; Liu, R.T. Social support as a protective factor in suicide: Findings from two nationally representative samples. J. Affect. Disord. 2013, 150, 540–545. [Google Scholar] [CrossRef]
- Szanto, K.; Dombrovski, A.Y.; Sahakian, B.J.; Mulsant, B.H.; Houck, P.R.; Reynolds, C.F., 3rd; Clark, L. Social emotion recognition, social functioning, and attempted suicide in late-life depression. Am. J. Geriatr. Psychiatry 2012, 20, 257–265. [Google Scholar] [CrossRef]
- De Silva, M.J.; Cooper, S.; Li, H.L.; Lund, C.; Patel, V. Effect of psychosocial interventions on social functioning in depression and schizophrenia: Meta-analysis. Br. J. Psychiatry 2013, 202, 253–260. [Google Scholar] [CrossRef]
- Nemoto, T.; Fujii, C.; Miura, U.; Chino, B.; Kobayashi, H.; Yamazawa, R.; Murakami, M.; Kashima, H.; Mizuno, M. Reliability and validity of the Social Functioning Scale Japanese version (SFS-J). JPN Bull. Soc. Psychiatr. 2008, 17, 188–195. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Publishing: Washington, DC, USA, 2013; pp. 155–188. [Google Scholar]
- Tsuang, M.T.; Tohen, M.; Jones, P.B. Textbook of Psychiatric Epidemiology, 3rd ed.; John Wiley & Sons: Chichester, UK, 2011; pp. 1–8. [Google Scholar]
- Heeringen, K.V. Understanding Suicidal Behaviour: The Suicidal Process Approach Research, Treatment and Prevention; John Wiley & Sons Ltd.: Chichester, UK, 2001; pp. 4–14. [Google Scholar]
- Kessler, R.C.; Borges, G.; Walters, E.E. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch. Gen. Psychiatry 1999, 56, 617–626. [Google Scholar] [CrossRef]
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef] [PubMed]
- Amagliani, G.; Baldelli, G.; Italiano, P.; Frisina, P.; Schiavano, G.F.; Brandi, G.; De Santi, M. Effect of COVID-19 isolation measures on physical activity of children and their parents, and role of the family environment: A cross-sectional study. Ann. Ig. Med. Prev. Comunità 2023, 35, 159–177. [Google Scholar]
- Organisation for Economic Co-Operation and Development (OECD). COVID-19 Pandemic Underlines Need to Strengthen Resilience of Health Systems, Says OECD. Available online: https://www.oecd.org/newsroom/covid-19-pandemic-underlines-need-to-strengthen-resilience-of-health-systems-says-oecd.htm (accessed on 26 March 2023).
| Subjects with DSI | Subjects without DSI | Crude | Model 1 † | Model 2 ‡ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n = 13) | (n = 374) | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |||
| n (%) | n (%) | |||||||||
| Sex | ||||||||||
| Male | 6 | (46.2) | 182 | (48.7) | 1.00 | 1.00 | 1.00 | |||
| Female | 7 | (53.9) | 192 | (51.3) | 1.11 (0.37–3.35) | 0.859 | 2.43 (0.46–12.9) | 0.296 | 2.64 (0.46–15.1) | 0.277 |
| Age (median, range) | 52.0 (40.0–64.3) 48.9 (35.1–64.4) | |||||||||
| 35–44 (years) | 3 | (23.1) | 145 | (38.8) | 1.00 | 1.00 | 1.00 | |||
| 45–54 | 8 | (61.5) | 120 | (32.1) | 3.22 (0.84–12.4) | 0.089 | 5.64 (0.96–33.3) | 0.056 | 4.19 (0.70–25.3) | 0.118 |
| 55–64 | 2 | (15.4) | 109 | (29.1) | 0.89 (0.15–5.40) | 0.896 | 2.52 (0.28–23.0) | 0.414 | 1.20 (0.14–10.3) | 0.867 |
| (p for trend 0.933) | (p for trend 0.288) | (p for trend 0.810) | ||||||||
| Regular exercise | ||||||||||
| Less than once per month | 12 | (92.3) | 244 | (65.2) | 1.00 | 1.00 | 1.00 | |||
| Once or more per month | 1 | (7.7) | 130 | (34.8) | 0.16 (0.02–1.22) | 0.076 | 0.17 (0.02–1.76) | 0.136 | 0.19 (0.02–1.82) | 0.148 |
| Problems involving care of an ill or elderly family member during the previous 6 months | ||||||||||
| No | 10 | (76.9) | 345 | (92.3) | 1.00 | 1.00 | 1.00 | |||
| Yes | 3 | (23.1) | 29 | (7.8) | 3.57 (0.93–13.7) | 0.064 | 4.44 (0.76–25.9) | 0.098 | 5.61 (0.88–35.6) | 0.067 |
| Death of a family member during the previous 6 months | ||||||||||
| No | 11 | (84.6) | 361 | (96.5) | 1.00 | 1.00 | 1.00 | |||
| Yes | 2 | (15.4) | 13 | (3.5) | 5.05 (1.01–25.1) | 0.048 | 3.23 (0.38–27.8) | 0.286 | 3.07 (0.35–26.8) | 0.310 |
| Relationship problems in the workplace | ||||||||||
| No | 7 | (53.9) | 324 | (86.6) | 1.00 | 1.00 | 1.00 | |||
| Yes | 6 | (46.2) | 50 | (13.4) | 5.56 (1.79–17.2) | 0.003 | 4.24 (1.00–17.9) | 0.049 | 4.84 (1.14–20.6) | 0.033 |
| Cigarette smoking | ||||||||||
| Never or former | 6 | (46.2) | 286 | (76.5) | 1.00 | 1.00 | 1.00 | |||
| Current | 7 | (53.9) | 88 | (23.5) | 3.79 (1.24–11.6) | 0.019 | 7.48 (1.27–44.2) | 0.027 | 3.42 (0.65–17.9) | 0.146 |
| History of psychiatric disorder excluding dementia in parent(s) or child (children) | ||||||||||
| None | 10 | (76.9) | 350 | (93.6) | 1.00 | 1.00 | 1.00 | |||
| Parent(s) or child (children) with psychiatric illness(es) | 3 | (23.1) | 24 | (6.4) | 4.38 (1.13–17.0) | 0.033 | 4.94 (0.85–28.6) | 0.074 | 3.03 (0.45–20.2) | 0.253 |
| Educational background | ||||||||||
| Junior high school | 1 | (7.7) | 15 | (4.0) | 1.74 (0.20–15.1) | 0.614 | 1.01 (0.03–31.2) | 0.998 | 1.61 (0.06–42.0) | 0.776 |
| High school | 7 | (53.9) | 183 | (48.9) | 1.00 | 1.00 | 1.00 | |||
| Technical school, junior college, or higher vocational school | 2 | (15.4) | 88 | (23.5) | 0.59 (0.12–2.92) | 0.522 | 0.34 (0.04–2.59) | 0.296 | 0.24 (0.02–2.32) | 0.216 |
| University or graduate school | 3 | (23.1) | 88 | (23.5) | 0.89 (0.23–3.53) | 0.870 | 0.93 (0.15–5.84) | 0.941 | 0.77 (0.12–4.72) | 0.773 |
| Mean alcohol consumption per day | ||||||||||
| non-drinker | 2 | (15.4) | 147 | (39.3) | 1.00 | 1.00 | 1.00 | |||
| ≤34 (g) | 10 | (76.9) | 186 | (49.7) | 3.95 (0.85–18.3) | 0.079 | 4.71 (0.77–28.7) | 0.093 | 4.74 (0.71–31.8) | 0.109 |
| >34 | 1 | (7.7) | 41 | (11.0) | 1.79 (0.16–20.3) | 0.637 | 3.50 (0.17–70.3) | 0.413 | 3.51 (0.18–67.4) | 0.406 |
| (p for trend 0.261) | (p for trend 0.169) | (p for trend 0.209) | ||||||||
| Feeling of isolation from other family members (visual analogue scale) | ||||||||||
| <10.0 (mm) | 7 | (53.9) | 302 | (80.8) | 1.00 | 1.00 | 1.00 | |||
| 10.0–19.9 | 2 | (15.4) | 25 | (6.7) | 3.45 (0.68–17.5) | 0.135 | 2.92 (0.33–25.7) | 0.335 | 3.35 (0.42–26.5) | 0.252 |
| ≥20.0 | 4 | (30.8) | 47 | (12.6) | 3.67 (1.04–13.0) | 0.044 | 1.91 (0.36–10.1) | 0.447 | 2.98 (0.54–16.4) | 0.210 |
| (p for trend 0.030) | (p for trend 0.320) | (p for trend 0.145) | ||||||||
| Fatigue on waking | ||||||||||
| Less than once per month | 3 | (23.1) | 240 | (64.2) | 1.00 | 1.00 | ||||
| Once or more per month but less than once per week | 4 | (30.8) | 43 | (11.5) | 7.44 (1.61–34.4) | 0.010 | 7.90 (1.06–58.7) | 0.043 | ||
| Once or more per week | 6 | (46.2) | 91 | (24.3) | 5.28 (1.29–21.5) | 0.021 | 6.79 (1.02–45.1) | 0.048 | ||
| (p for trend 0.015) | (p for trend 0.051) | |||||||||
| Global score on Pittsburgh Sleep Quality Index | ||||||||||
| ≤5 | 4 | (30.8) | 259 | (69.3) | 1.00 | 1.00 | ||||
| 6 | 2 | (15.4) | 47 | (12.6) | 2.76 (0.49–15.5) | 0.250 | 2.15 (0.28–16.5) | 0.463 | ||
| 7–9 | 5 | (38.5) | 58 | (15.5) | 5.58 (1.45–21.4) | 0.012 | 3.22 (0.56–18.7) | 0.193 | ||
| ≥10 | 2 | (15.4) | 10 | (2.7) | 13.0 (2.12–79.2) | 0.006 | 8.19 (1.05–63.8) | 0.045 | ||
| (p for trend 0.001) | (p for trend 0.038) | |||||||||
| Condition | Sensitivity (%) (95% CI) | Specificity (%) (95% CI) | Positive Predictive Value (%) (95% CI) | Negative Predictive Value (%) (95% CI) | Positive Likelihood Ratio (95% CI) | Negative Likelihood Ratio (95% CI) | DSI/Number of Subjects with Condition (s) |
|---|---|---|---|---|---|---|---|
| Relationship problems in the workplace, Pittsburgh Sleep Quality Index score ≥ 10, and fatigue on waking once or more per week (RPW, PS10, and FWW) | 15.4 | 100 | 100 | 97.1 | ∞ | 0.846 | 2/2 |
| (1.9–45.5) | (99.0–100) | (15.8–100) | (95.0–98.6) | (0.671–1.067) | |||
| Relationship problems in the workplace and Pittsburgh Sleep Quality Index score ≥ 10 (RPW and PS10) | 15.4 | 99.7 | 66.7 | 97.1 | 57.54 | 0.848 | 2/3 |
| (1.9–45.5) | (98.5–99.99) | (9.4–99.2) | (94.9–98.6) | (5.565–594.9) | (0.673–1.070) | ||
| Relationship problems in the workplace, Pittsburgh Sleep Quality Index score ≥ 6, and fatigue on waking once or more per month (RPW, PS6, and FWM) | 38.5 | 96.8 | 29.4 | 97.8 | 11.99 | 0.636 | 5/17 |
| (13.9–68.4) | (94.5–98.3) | (10.3–56.0) | (95.8–99.1) | (4.949–29.04) | (0.414–0.978) | ||
| Relationship problems in the workplace and Pittsburgh Sleep Quality Index score ≥ 6 (RPW and PS6) | 46.2 | 94.4 | 22.2 | 98.1 | 8.220 | 0.570 | 6/27 |
| (19.2–74.9) | (91.5–96.5) | (8.6–42.3) | (96.0–99.2) | (4.004–16.88) | (0.345–0.944) | ||
| Relationship problems in the workplace and fatigue on waking once or more per week (RPW and FWW) | 38.5 | 95.2 | 21.7 | 97.8 | 7.991 | 0.646 | 5/23 |
| (13.9–68.4) | (92.5–97.1) | (7.5–43.7) | (95.7–99.1) | (3.512–18.18) | (0.420–0.994) | ||
| Pittsburgh Sleep Quality Index score ≥ 10 (PS10) | 15.4 | 97.3 | 16.7 | 97.1 | 5.754 | 0.869 | 2/12 |
| (1.9–45.5) | (95.1–98.7) | (2.1–48.4) | (94.8–98.5) | (1.399–23.66) | (0.689–1.097) | ||
| Relationship problems in the workplace and fatigue on waking once or more per month (RPW and FWM) | 38.5 | 93.3 | 16.7 | 97.8 | 5.754 | 0.659 | 5/30 |
| (13.9–68.4) | (90.3–95.6) | (5.6–34.7) | (95.6–99.0) | (2.624–12.62) | (0.429–1.014) | ||
| Relationship problems in the workplace (RPW) | 46.2 | 86.6 | 10.7 | 97.9 | 3.452 | 0.622 | 6/56 |
| (19.2–74.9) | (82.8–89.9) | (4.0–21.9) | (95.7–99.2) | (1.818–6.556) | (0.375–1.030) | ||
| Relationship problems in the workplace or Pittsburgh Sleep Quality Index score ≥ 10 (RPW or PS10) | 46.2 | 84.2 | 9.2 | 97.8 | 2.926 | 0.639 | 6/65 |
| (19.2–74.9) | (80.1–87.8) | (3.5–19.0) | (95.6–99.1) | (1.555–5.505) | (0.386–1.060) | ||
| Pittsburgh Sleep Quality Index score ≥ 6 (PS6) | 69.2 | 69.3 | 7.3 | 98.5 | 2.252 | 0.444 | 9/124 |
| (38.6–90.9) | (64.3–73.9) | (3.4–13.3) | (96.2–99.6) | (1.520–3.336) | (0.196–1.007) | ||
| Fatigue on waking once or more per month (FWM) | 76.9 | 64.2 | 6.9 | 98.8 | 2.147 | 0.360 | 10/144 |
| (46.2–95.0) | (59.1–69.0) | (3.4–12.4) | (96.4–99.7) | (1.548–2.978) | (0.133–0.973) | ||
| Relationship problems in the workplace or fatigue on waking once or more per month (RPW or FWM) | 84.6 | 57.5 | 6.5 | 99.1 | 1.990 | 0.268 | 11/170 |
| (54.6–98.1) | (52.3–62.6) | (3.3–11.3) | (96.7–99.9) | (1.535–2.581) | (0.075–0.960) | ||
| Fatigue on waking once or more per week (FWW) | 46.2 | 75.7 | 6.2 | 97.6 | 1.897 | 0.712 | 6/97 |
| (19.2–74.9) | (71.0–79.9) | (2.3–13.0) | (95.1–99.0) | (1.027–3.504) | (0.429–1.181) | ||
| Relationship problems in the workplace or Pittsburgh Sleep Quality Index score ≥ 6 (RPW or PQ6) | 69.2 | 61.5 | 5.9 | 98.3 | 1.798 | 0.500 | 9/153 |
| (38.6–90.9) | (56.4–66.5) | (2.7–10.9) | (95.7–99.5) | (1.224–2.641) | (0.221–1.135) | ||
| Relationship problems in the workplace, Pittsburgh Sleep Quality Index score ≥ 6, or fatigue on waking once or more per month (RPW, PS6, or FWM) | 92.3 | 44.9 | 5.5 | 99.4 | 1.676 | 0.171 | 12/218 |
| (64.0–99.8) | (39.8–50.1) | (2.9–9.4) | (96.8–99.99) | (1.397–2.010) | (0.026–1.130) | ||
| Relationship problems in the workplace or fatigue on waking once or more per week (RPW or FWW) | 53.9 | 67.1 | 5.4 | 97.7 | 1.637 | 0.688 | 7/130 |
| (25.1–80.8) | (62.1–71.9) | (2.2–10.8) | (95.0–99.1) | (0.970–2.764) | (0.381–1.242) | ||
| Relationship problems in the workplace, Pittsburgh Sleep Quality Index score ≥ 10, or fatigue on waking once or more per week (RPW, PQ10, or FWW) | 53.9 | 65.0 | 5.1 | 97.6 | 1.537 | 0.710 | 7/138 |
| (25.1–80.8) | (59.9–69.8) | (2.1–10.2) | (94.8–99.1) | (0.912–2.591) | (0.393–1.284) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujieda, M.; Uchida, K.; Ikebe, S.; Kimura, A.; Kimura, M.; Watanabe, T.; Sakamoto, H.; Matsumoto, T.; Uchimura, N. Fatigue on Waking, Insomnia, and Workplace Relationship Problems May Help to Detect Suicidal Ideation among New Middle-Aged Primary Care Patients: A 6-Month Prospective Study in Japan. Int. J. Environ. Res. Public Health 2023, 20, 5547. https://doi.org/10.3390/ijerph20085547
Fujieda M, Uchida K, Ikebe S, Kimura A, Kimura M, Watanabe T, Sakamoto H, Matsumoto T, Uchimura N. Fatigue on Waking, Insomnia, and Workplace Relationship Problems May Help to Detect Suicidal Ideation among New Middle-Aged Primary Care Patients: A 6-Month Prospective Study in Japan. International Journal of Environmental Research and Public Health. 2023; 20(8):5547. https://doi.org/10.3390/ijerph20085547
Chicago/Turabian StyleFujieda, Megumi, Katsuhisa Uchida, Shinichiro Ikebe, Akihiro Kimura, Masashi Kimura, Toshiaki Watanabe, Hisako Sakamoto, Teruaki Matsumoto, and Naohisa Uchimura. 2023. "Fatigue on Waking, Insomnia, and Workplace Relationship Problems May Help to Detect Suicidal Ideation among New Middle-Aged Primary Care Patients: A 6-Month Prospective Study in Japan" International Journal of Environmental Research and Public Health 20, no. 8: 5547. https://doi.org/10.3390/ijerph20085547
APA StyleFujieda, M., Uchida, K., Ikebe, S., Kimura, A., Kimura, M., Watanabe, T., Sakamoto, H., Matsumoto, T., & Uchimura, N. (2023). Fatigue on Waking, Insomnia, and Workplace Relationship Problems May Help to Detect Suicidal Ideation among New Middle-Aged Primary Care Patients: A 6-Month Prospective Study in Japan. International Journal of Environmental Research and Public Health, 20(8), 5547. https://doi.org/10.3390/ijerph20085547






