The Effect of COVID-19 Pandemic on Overall and Cause-Specific Mortality in Pavia, Northern Italy: Updated Estimates for the Year 2021
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- EpiCentro International Outbreak of Novel SARS-CoV-2 Coronavirus Infection. Available online: https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-international-outbreak (accessed on 12 April 2023).
- Naming the Coronavirus Disease (COVID-19) and the Virus That Causes It. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (accessed on 12 April 2023).
- Beaney, T.; Clarke, J.M.; Jain, V.; Golestaneh, A.K.; Lyons, G.; Salman, D.; Majeed, A. Excess Mortality: The Gold Standard in Measuring the Impact of COVID-19 Worldwide? J. R. Soc. Med. 2020, 113, 329–334. [Google Scholar] [CrossRef]
- Odone, A.; Delmonte, D.; Scognamiglio, T.; Signorelli, C. COVID-19 Deaths in Lombardy, Italy: Data in Context. Lancet Public Health 2020, 5, e310. [Google Scholar] [CrossRef]
- Amerio, A.; Aguglia, A.; Odone, A.; Gianfredi, V.; Serafini, G.; Signorelli, C.; Amore, M. Covid-19 Pandemic Impact on Mental Health of Vulnerable Populations. Acta Bio Medica Atenei Parm. 2020, 91, 95–96. [Google Scholar] [CrossRef]
- Vigezzi, G.P.; Bertuccio, P.; Amerio, A.; Bosetti, C.; Gori, D.; Cavalieri d’Oro, L.; Iacoviello, L.; Stuckler, D.; Zucchi, A.; Gallus, S.; et al. Older Adults’ Access to Care during the COVID-19 Pandemic: Results from the LOckdown and LifeSTyles (LOST) in Lombardia Project. Int. J. Environ. Res. Public Health 2022, 19, 11271. [Google Scholar] [CrossRef] [PubMed]
- Karlinsky, A.; Kobak, D. Tracking Excess Mortality across Countries during the COVID-19 Pandemic with the World Mortality Dataset. eLife 2021, 10, e69336. [Google Scholar] [CrossRef]
- Mannucci, P.M.; Nobili, A.; Tettamanti, M.; D’Avanzo, B.; Galbussera, A.A.; Remuzzi, G.; Fortino, I.; Leoni, O.; Harari, S. Impact of the Post-COVID-19 Condition on Health Care after the First Disease Wave in Lombardy. J. Intern. Med. 2022, 292, 450–462. [Google Scholar] [CrossRef]
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO Estimates of Excess Mortality Associated with the COVID-19 Pandemic. Nature 2022, 613, 130–137. [Google Scholar] [CrossRef]
- Grande, E.; Fedeli, U.; Pappagallo, M.; Crialesi, R.; Marchetti, S.; Minelli, G.; Iavarone, I.; Frova, L.; Onder, G.; Grippo, F. Variation in Cause-Specific Mortality Rates in Italy during the First Wave of the COVID-19 Pandemic: A Study Based on Nationwide Data. Int. J. Environ. Res. Public Health 2022, 19, 805. [Google Scholar] [CrossRef] [PubMed]
- Blangiardo, M.; Cameletti, M.; Pirani, M.; Corsetti, G.; Battaglini, M.; Baio, G. Estimating Weekly Excess Mortality at Sub-National Level in Italy during the COVID-19 Pandemic. PLoS ONE 2020, 15, e0240286. [Google Scholar] [CrossRef]
- Alicandro, G.; Remuzzi, G.; Centanni, S.; Gerli, A.; La Vecchia, C. Excess Total Mortality during the Covid-19 Pandemic in Italy: Updated Estimates Indicate Persistent Excess in Recent Months. Med. Lav. 2022, 113, e2022021. [Google Scholar] [CrossRef] [PubMed]
- Ceccarelli, E.; Dorrucci, M.; Minelli, G.; Jona Lasinio, G.; Prati, S.; Battaglini, M.; Corsetti, G.; Bella, A.; Boros, S.; Petrone, D.; et al. Assessing COVID-19-Related Excess Mortality Using Multiple Approaches—Italy, 2020–2021. Int. J. Environ. Res. Public Health 2022, 19, 16998. [Google Scholar] [CrossRef] [PubMed]
- Konstantinoudis, G.; Cameletti, M.; Gómez-Rubio, V.; Gómez, I.L.; Pirani, M.; Baio, G.; Larrauri, A.; Riou, J.; Egger, M.; Vineis, P.; et al. Regional Excess Mortality during the 2020 COVID-19 Pandemic in Five European Countries. Nat. Commun. 2022, 13, 482. [Google Scholar] [CrossRef] [PubMed]
- Sanmarchi, F.; Golinelli, D.; Lenzi, J.; Esposito, F.; Capodici, A.; Reno, C.; Gibertoni, D. Exploring the Gap Between Excess Mortality and COVID-19 Deaths in 67 Countries. JAMA Netw. Open 2021, 4, e2117359. [Google Scholar] [CrossRef]
- Bilinski, A.; Emanuel, E.J. COVID-19 and Excess All-Cause Mortality in the US and 18 Comparison Countries. JAMA 2020, 324, 2100–2102. [Google Scholar] [CrossRef]
- Rossen, L.M.; Nørgaard, S.K.; Sutton, P.D.; Krause, T.G.; Ahmad, F.B.; Vestergaard, L.S.; Mølbak, K.; Anderson, R.N.; Nielsen, J. Excess All-Cause Mortality in the USA and Europe during the COVID-19 Pandemic, 2020 and 2021. Sci. Rep. 2022, 12, 18559. [Google Scholar] [CrossRef]
- Dorrucci, M.; Minelli, G.; Boros, S.; Manno, V.; Prati, S.; Battaglini, M.; Corsetti, G.; Andrianou, X.; Riccardo, F.; Fabiani, M.; et al. Excess Mortality in Italy During the COVID-19 Pandemic: Assessing the Differences Between the First and the Second Wave, Year 2020. Front. Public Health 2021, 9, 669209. [Google Scholar] [CrossRef]
- Odone, A.; Delmonte, D.; Gaetti, G.; Signorelli, C. Doubled Mortality Rate during the COVID-19 Pandemic in Italy: Quantifying What Is Not Captured by Surveillance. Public Health 2021, 190, 108–115. [Google Scholar] [CrossRef]
- Esper, F.P.; Adhikari, T.M.; Tu, Z.J.; Cheng, Y.W.; El-Haddad, K.; Farkas, D.H.; Bosler, D.; Rhoads, D.; Procop, G.W.; Ko, J.S.; et al. Alpha to Omicron: Disease Severity and Clinical Outcomes of Major SARS-CoV-2 Variants. J. Infect. Dis. 2022, 227, 344–352. [Google Scholar] [CrossRef]
- EpiCentro Monitoraggio Delle Varianti del Virus SARS-CoV-2 di Interesse in Sanità Pubblica in Italia. Available online: https://www.epicentro.iss.it/coronavirus/sars-cov-2-monitoraggio-varianti-rapporti-periodici (accessed on 27 December 2022).
- Maruotti, A.; Jona-Lasinio, G.; Divino, F.; Lovison, G.; Ciccozzi, M.; Farcomeni, A. Estimating COVID-19-Induced Excess Mortality in Lombardy, Italy. Aging Clin. Exp. Res. 2022, 34, 475–479. [Google Scholar] [CrossRef]
- Perotti, P.; Bertuccio, P.; Cacitti, S.; Deandrea, S.; Boschetti, L.; Dalle Carbonare, S.; Marguati, S.; Migliazza, S.; Porzio, E.; Riboli, S.; et al. Impact of the COVID-19 Pandemic on Total and Cause-Specific Mortality in Pavia, Northern Italy. Int. J. Environ. Res. Public Health 2022, 19, 6498. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.B.; Anderson, R.N. The Leading Causes of Death in the US for 2020. JAMA 2021, 325, 1829–1830. [Google Scholar] [CrossRef]
- International Guidelines for Certification and Classification (Coding) of COVID-19 as Cause of Death. Available online: https://www.who.int/publications/m/item/international-guidelines-for-certification-and-classification-(coding)-of-covid-19-as-cause-of-death (accessed on 4 April 2023).
- Scortichini, M.; Schneider Dos Santos, R.; De’ Donato, F.; De Sario, M.; Michelozzi, P.; Davoli, M.; Masselot, P.; Sera, F.; Gasparrini, A. Excess Mortality during the COVID-19 Outbreak in Italy: A Two-Stage Interrupted Time-Series Analysis. Int. J. Epidemiol. 2021, 49, 1909–1917. [Google Scholar] [CrossRef]
- Ioannidis, J.P.A.; Zonta, F.; Levitt, M. Estimates of COVID-19 Deaths in Mainland China after Abandoning Zero COVID Policy. Eur. J. Clin. Investig. 2023, 53, e13956. [Google Scholar] [CrossRef]
- Rapporto SDGs 2022. Informazioni Statistiche per l’Agenda 2030 in Italia. Available online: https://www.istat.it/it/archivio/275718 (accessed on 27 December 2022).
- Marziano, V.; Guzzetta, G.; Mammone, A.; Riccardo, F.; Poletti, P.; Trentini, F.; Manica, M.; Siddu, A.; Bella, A.; Stefanelli, P.; et al. The Effect of COVID-19 Vaccination in Italy and Perspectives for Living with the Virus. Nat. Commun. 2021, 12, 7272. [Google Scholar] [CrossRef]
- Italian Ministry of Health. Vaccinazione Anti-SARS-COV-2/COVID-19 Piano Strategico. Available online: https://www.trovanorme.salute.gov.it/norme/renderpdf.spring?seriegu=sg&datagu=24/03/2021&redaz=21A01802&artp=1&art=1&subart=1&subart1=10&vers=1&prog=001 (accessed on 20 December 2022).
- Signorelli, C.; Odone, A.; Gianfredi, V.; Balzarini, F.; Bucci, D.; Croci, R.; Gaetti, G.; Stirparo, G.; Guerra, R. Epidemiological Assessment of the First COVID-19 Epidemic Wave in Lombardy. A Systematic Review: First COVID-19 Epidemic Wave in Lombardy. Acta Biomed. Atenei Parm. 2021, 92, e2021462. [Google Scholar] [CrossRef]
- Alicandro, G.; Remuzzi, G.; Centanni, S.; Gerli, A.; La Vecchia, C. Excess Total Mortality in 2021 in Italy Was about One Third of That Observed in 2020. Med. Lav. 2021, 112, 414–421. [Google Scholar] [CrossRef]
- Characteristics of COVID-19 Patients Dying in Italy. Available online: https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-analysis-of-deaths (accessed on 31 December 2022).
- Ritchie, H.; Spooner, F.; Roser, M. Causes of Death. Our World Data. Available online: https://ourworldindata.org/causes-of-death (accessed on 27 December 2022).
- Italy: COVID Deaths by Age Group 2022. Available online: https://www.statista.com/statistics/1105061/coronavirus-deaths-by-age-group-in-italy/ (accessed on 27 December 2022).
- Silversmit, G.; Verdoodt, F.; Van Damme, N.; De Schutter, H.; Van Eycken, L. Excess Mortality in a Nationwide Cohort of Cancer Patients during the Initial Phase of the COVID-19 Pandemic in Belgium. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol. 2021, 30, 1615–1619. [Google Scholar] [CrossRef]
- I numeri del cancro in Italia. Available online: https://www.aiom.it/i-numeri-del-cancro-in-italia/ (accessed on 27 December 2022).
- Semenzato, L.; Botton, J.; Drouin, J.; Cuenot, F.; Dray-Spira, R.; Weill, A.; Zureik, M. Chronic Diseases, Health Conditions and Risk of COVID-19-Related Hospitalization and in-Hospital Mortality during the First Wave of the Epidemic in France: A Cohort Study of 66 Million People. Lancet Reg. Health Eur. 2021, 8, 100158. [Google Scholar] [CrossRef]
- Mosconi, G.; Stival, C.; Lugo, A.; Signorelli, C.; Amerio, A.; Cavalieri d’Oro, L.; Iacoviello, L.; Stuckler, D.; Zucchi, A.; Odone, A.; et al. Determinants of SARS-CoV-2 Infection in the Older Adult Population: Data from the LOST in Lombardia Study. Vaccines 2022, 10, 989. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, M.; Elliott, J.; Chadeau-Hyam, M.; Riley, S.; Darzi, A.; Cooke, G.; Ward, H.; Elliott, P. Persistent COVID-19 Symptoms in a Community Study of 606,434 People in England. Nat. Commun. 2022, 13, 1957. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-Term Cardiovascular Outcomes of COVID-19. Nat. Med. 2022, 28, 583–590. [Google Scholar] [CrossRef] [PubMed]
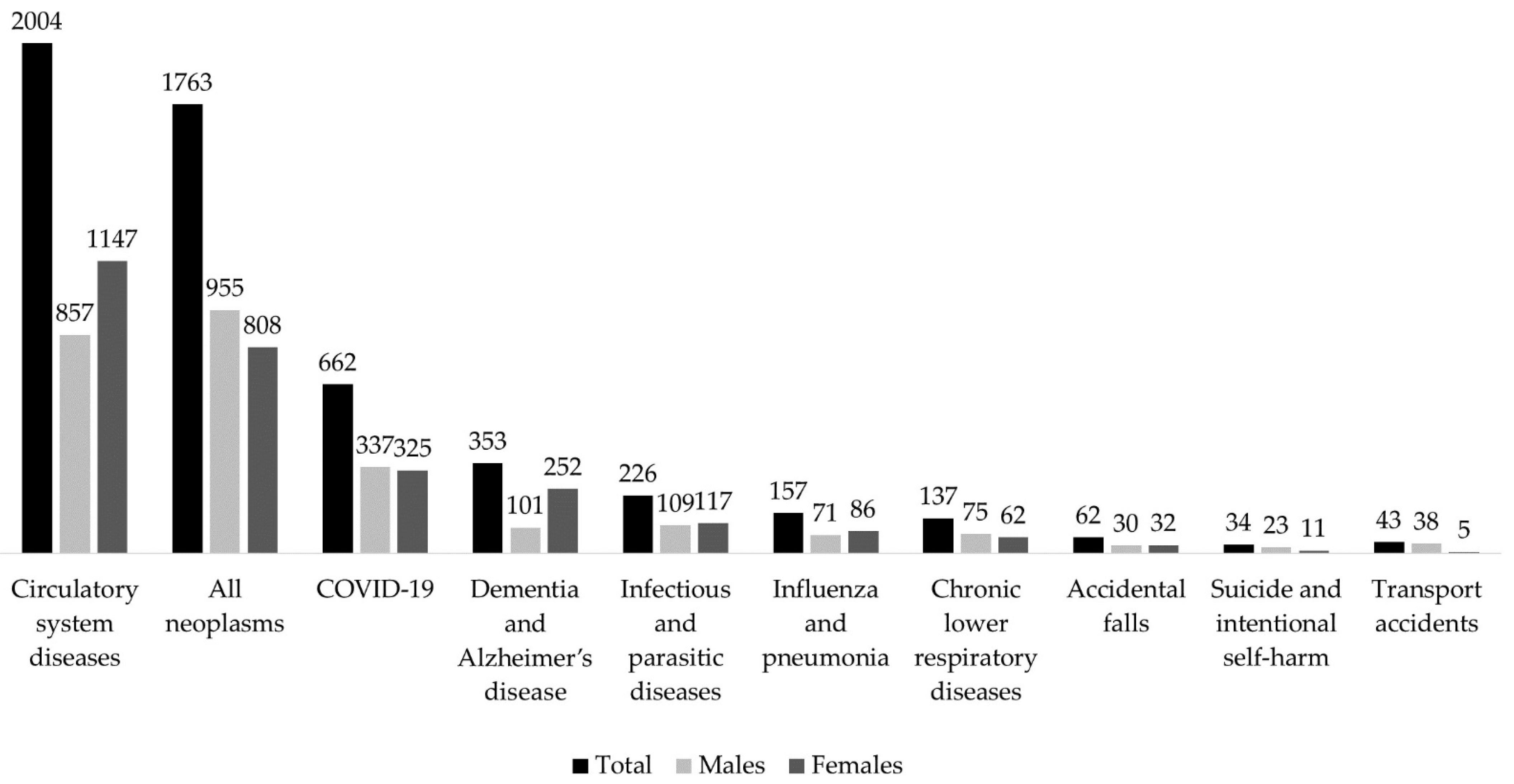
| 2015–2019 | 2021 | Rate Ratio (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| Group of Causes | Average Deaths | RMR | ASMR | Deaths | RMR | ASMR | |
| Total | |||||||
| All causes | 6653 | 1215.9 | 978.3 | 6836 | 1275.9 | 972.4 | 0.99 (0.96–1.03) |
| COVID-19 | - | - | - | 662 | 123.6 | 94.8 | - |
| Infectious and parasitic diseases (COVID-19 excluded) | 186 | 34.0 | 27.8 | 226 | 42.2 | 32.1 | 1.15 (0.95–1.40) |
| All neoplasms | 1926 | 352.1 | 300.9 | 1763 | 329.0 | 270.3 | 0.90 (0.84–0.96) |
| Diabetes mellitus | 173 | 31.7 | 25.5 | 157 | 29.3 | 21.5 | 0.85 (0.68–1.05) |
| Dementia and Alzheimer’s disease | 393 | 71.9 | 54.2 | 353 | 65.9 | 46.3 | 0.85 (0.74–0.99) |
| Circulatory system diseases | 2326 | 425.2 | 329.3 | 2004 | 374 | 272.6 | 0.83 (0.78–0.88) |
| Influenza and Pneumonia | 207 | 37.9 | 29.0 | 157 | 29.3 | 21.4 | 0.74 (0.60–0.91) |
| Chronic lower respiratory diseases | 181 | 25.6 | 18.9 | 137 | 33.2 | 26 | 0.73 (0.58–0.91) |
| Transport accidents | 32 | 5.9 | 5.7 | 43 | 8.0 | 7.7 | 1.33 (0.84–2.11) |
| Accidental falls | 66 | 12.0 | 9.4 | 62 | 11.6 | 8.3 | 0.88 (0.62–1.25) |
| Suicides and intentional self-harm | 43 | 6.4 | 5.9 | 34 | 6.4 | 5.9 | 0.78 (0.50–1.23) |
| Males | |||||||
| All causes | 3054 | 1146.0 | 974.7 | 3174 | 1210.2 | 958.1 | 0.99 (0.93–1.03) |
| COVID-19 | - | - | - | 337 | 128.5 | 101.2 | - |
| Infectious and parasitic diseases (COVID-19 excluded) | 88 | 33.0 | 28.1 | 109 | 41.6 | 32.5 | 1.16 (0.87–1.54) |
| All neoplasms | 1060 | 397.9 | 345.8 | 955 | 364.1 | 299.9 | 0.87 (0.80–0.95) |
| Diabetes mellitus | 80 | 30.0 | 25.5 | 66 | 25.2 | 19.5 | 0.76 (0.55–1.06) |
| Dementia and Alzheimer’s disease | 112 | 42.0 | 34.1 | 101 | 38.5 | 28.9 | 0.85 (0.65–1.11) |
| Circulatory system diseases | 953 | 357.6 | 298.2 | 857 | 326.8 | 250.4 | 0.84 (0.77–0.92) |
| Influenza and Pneumonia | 93 | 35.1 | 28.9 | 71 | 27.1 | 20.3 | 0.70 (0.51–0.96) |
| Chronic lower respiratory diseases | 97 | 36.5 | 29.8 | 75 | 28.6 | 21.4 | 0.72 (0.53–0.97) |
| Transport accidents | 26 | 9.6 | 9.4 | 38 | 14.5 | 13.6 | 1.45 (0.87–2.41) |
| Accidental falls | 29 | 11.0 | 9.2 | 30 | 11.4 | 8.7 | 0.95 (0.57–1.59) |
| Suicide and intentional self-harm | 33 | 12.5 | 11.8 | 23 | 8.8 | 8.1 | 0.68 (0.40–1.17) |
| Females | |||||||
| All causes | 3599 | 1282.3 | 983.1 | 3662 | 1338.8 | 977.5 | 0.99 (0.95–1.04) |
| COVID-19 | 0 | - | - | 325 | 118.8 | 87.5 | - |
| Infectious and parasitic diseases (COVID-19 excluded) | 98 | 35 | 27.7 | 117 | 42.8 | 31.4 | 1.14 (0.87–1.49) |
| All neoplasms | 866 | 308.6 | 259.1 | 808 | 295.4 | 239.4 | 0.92 (0.84–1.02) |
| Diabetes mellitus | 93 | 33.3 | 25.4 | 91 | 33.3 | 23.3 | 0.92 (0.69–1.23) |
| Dementia and Alzheimer’s disease | 282 | 100.3 | 72.7 | 252 | 92.1 | 62.3 | 0.86 (0.72–1.02) |
| Circulatory system diseases | 1373 | 489.4 | 358.5 | 1147 | 419.3 | 291.8 | 0.81 (0.75–0.88) |
| Influenza and Pneumonia | 114 | 40.6 | 29.4 | 86 | 31.4 | 22.5 | 0.76 (0.58–1.02) |
| Chronic lower respiratory diseases | 84 | 30.0 | 22.8 | 62 | 22.7 | 16.4 | 0.72 (0.52–1.01) |
| Transport accidents | 6 | 2.3 | 2.2 | 5 | 1.8 | 1.8 | 0.79 (0.24–2.58) |
| Accidental falls | 37 | 13.2 | 9.8 | 32 | 11.7 | 7.8 | 0.80 (0.50–1.30) |
| Suicide and intentional self-harm | 10 | 3.5 | 3.3 | 11 | 4.0 | 3.6 | 1.10 (0.46–2.62) |
| Observed Deaths | Expected 1 Deaths | Excess Deaths (95% C.I.) | % Excess Deaths (95% C.I.) | |
|---|---|---|---|---|
| All causes | ||||
| Total | ||||
| All ages | 6836 | 6436 | 400 (253–546) | 6.2 (3.9–8.5) |
| 25–64 | 639 | 614 | 25 (3–46) | 4.1 (0.5–7.5) |
| 65–79 | 1609 | 1493 | 116 (74–157) | 7.8 (5.0–10.5) |
| 80+ | 4565 | 4309 | 256 (154–357) | 5.9 (3.6–8.3) |
| Males | ||||
| All ages | 3174 | 2960 | 214 (112–315) | 7.2 (3.8–10.6) |
| 25–64 | 414 | 389 | 25 (7–42) | 6.4 (1.8–10.8) |
| 65–79 | 983 | 894 | 89 (54–123) | 10.0 (6.0–13.8) |
| 80+ | 1762 | 1664 | 98 (38–157) | 5.9 (2.3–9.4) |
| Females | ||||
| All ages | 3662 | 3476 | 186 (77–294) | 5.4 (2.2–8.5) |
| 25–64 | 225 | 224 | 1 (−11–13) | 0.4 (−4.9–5.8) |
| 65–79 | 626 | 598 | 28 (4–51) | 4.7 (0.7–8.5) |
| 80+ | 2803 | 2645 | 158 (74–241) | 6.0 (2.8–9.1) |
| Observed Deaths | Expected 1 Deaths | Excess Deaths (95% C.I.) | % Excess Deaths (95% C.I.) | |
|---|---|---|---|---|
| All neoplasms | ||||
| Total | ||||
| All ages | 1763 | 1761 | 2 (−109–113) | 0.1 (−6.2–6.4) |
| 25–64 | 298 | 279 | 19 (−1–39) | 6.8 (−0.4–14.0) |
| 65–79 | 631 | 678 | −47 (−92–−1) | −6.9 (−13.6–−0.1) |
| 80+ | 830 | 794 | 36 (−15–87) | 4.5 (−1.9–11.0) |
| Males | ||||
| All ages | 955 | 983 | −28 (−106–50) | −2.8 (−10.8–5.1) |
| 25–64 | 165 | 156 | 9 (−6–24) | 5.8 (−3.8–15.4) |
| 65–79 | 385 | 412 | −27 (−62–8) | −6.6 (−15.0–1.9) |
| 80+ | 402 | 410 | −8 (−42–26) | −2.0 (−10.2–6.3) |
| Females | ||||
| All ages | 808 | 778 | 30 (−29–89) | 3.9 (−3.7–11.4) |
| 25–64 | 133 | 123 | 10 (−1–21) | 8.1 (−0.8–17.1) |
| 65–79 | 246 | 266 | −20 (−41–1) | −7.5 (−15.4–0.4) |
| 80+ | 428 | 383 | 45 (14–75) | 11.7 (3.7–19.6) |
| Circulatory system diseases | ||||
| Total | ||||
| All ages | 2004 | 2135 | −131 (−211–−50) | −6.1 (−9.9–−2.3) |
| 25–64 | 108 | 92 | 16 (8–23) | 17.4 (8.7–25.0) |
| 65–79 | 360 | 350 | 10 (−6–26) | 2.9 (−1.7–7.4) |
| 80+ | 1536 | 1688 | −152 (−216–−87) | −9.0 (−12.8–−5.2) |
| Males | ||||
| All ages | 857 | 874 | −17 (−69–35) | −1.9 (−7.9–4.0) |
| 25–64 | 84 | 73 | 11 (4–17) | 15.1 (5.5–23.3) |
| 65–79 | 220 | 214 | 6 (−8–20) | 2.8 (−3.7–9.3) |
| 80+ | 553 | 584 | −31 (−67–5) | −5.3 (−11.5–0.9) |
| Females | ||||
| All ages | 1147 | 1261 | −114 (−176–−51) | −9.0 (−14.0–−4.0) |
| 25–64 | 24 | 19 | 5 (2–7) | 26.3 (10.5–36.8) |
| 65–79 | 140 | 136 | 4 (−5–13) | 2.9 (−3.7–9.6) |
| 80+ | 983 | 1103 | −120 (−175–−64) | −10.9 (−15.9–−5.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertuccio, P.; Perotti, P.; Mosconi, G.; Dalle Carbonare, S.; Manzoni, F.; Boschetti, L.; Marguati, S.; Paraluppi, P.; Blandi, L.; Gentile, L.; et al. The Effect of COVID-19 Pandemic on Overall and Cause-Specific Mortality in Pavia, Northern Italy: Updated Estimates for the Year 2021. Int. J. Environ. Res. Public Health 2023, 20, 5529. https://doi.org/10.3390/ijerph20085529
Bertuccio P, Perotti P, Mosconi G, Dalle Carbonare S, Manzoni F, Boschetti L, Marguati S, Paraluppi P, Blandi L, Gentile L, et al. The Effect of COVID-19 Pandemic on Overall and Cause-Specific Mortality in Pavia, Northern Italy: Updated Estimates for the Year 2021. International Journal of Environmental Research and Public Health. 2023; 20(8):5529. https://doi.org/10.3390/ijerph20085529
Chicago/Turabian StyleBertuccio, Paola, Pietro Perotti, Giansanto Mosconi, Simona Dalle Carbonare, Federica Manzoni, Lorenza Boschetti, Stefano Marguati, Paolo Paraluppi, Lorenzo Blandi, Leandro Gentile, and et al. 2023. "The Effect of COVID-19 Pandemic on Overall and Cause-Specific Mortality in Pavia, Northern Italy: Updated Estimates for the Year 2021" International Journal of Environmental Research and Public Health 20, no. 8: 5529. https://doi.org/10.3390/ijerph20085529
APA StyleBertuccio, P., Perotti, P., Mosconi, G., Dalle Carbonare, S., Manzoni, F., Boschetti, L., Marguati, S., Paraluppi, P., Blandi, L., Gentile, L., Gaeta, M., Cecconami, L., & Odone, A. (2023). The Effect of COVID-19 Pandemic on Overall and Cause-Specific Mortality in Pavia, Northern Italy: Updated Estimates for the Year 2021. International Journal of Environmental Research and Public Health, 20(8), 5529. https://doi.org/10.3390/ijerph20085529






