Exploratory Factor Analysis of a French Adapted Version of the Substance Abuse Attitude Survey among Medical Students in Belgium
Abstract
1. Introduction
2. Materials and Methods
2.1. Questionnaire
2.2. Data Collection
2.3. Statistical Methodology
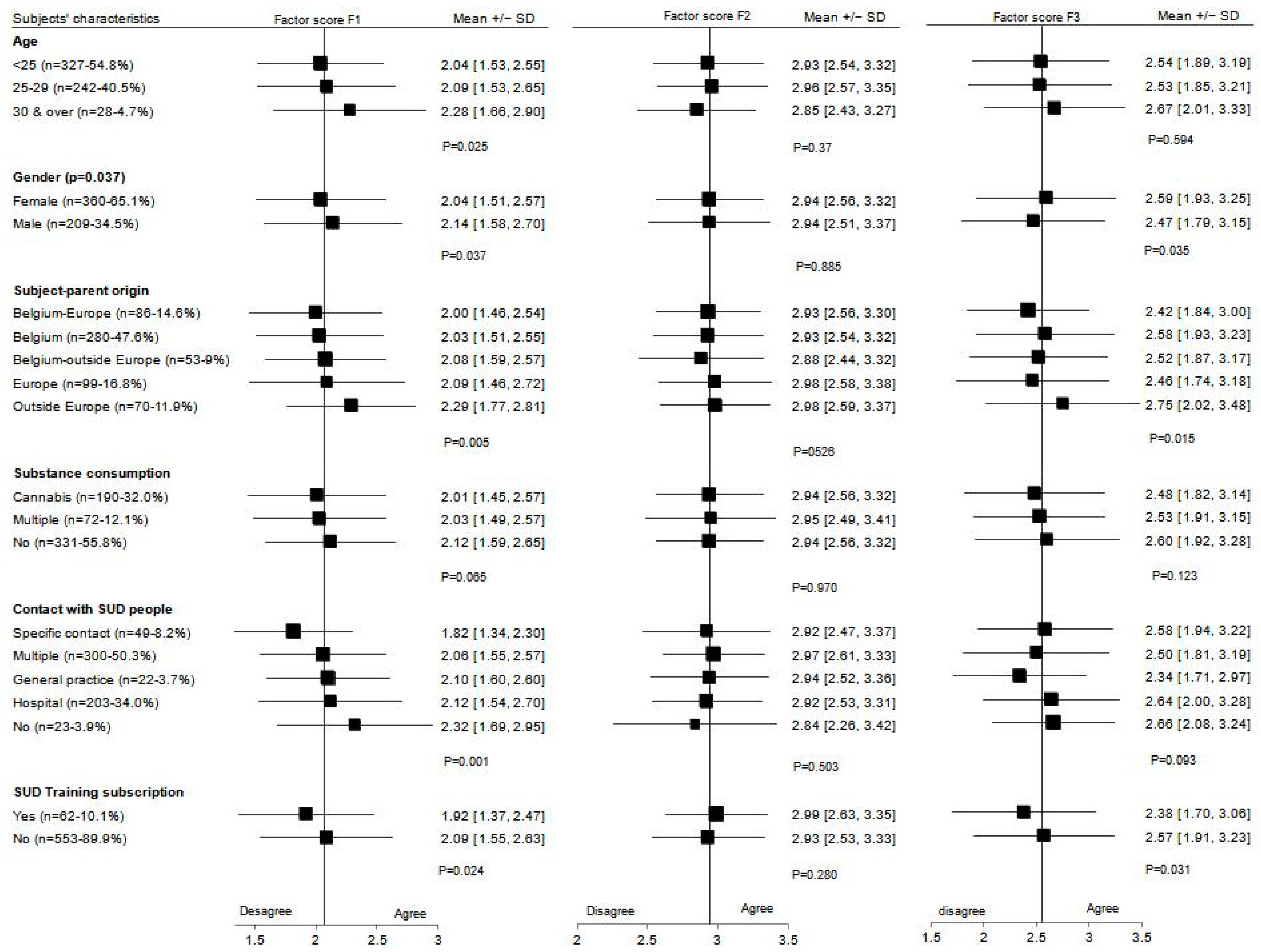
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Indicate your degree of agreement or disagreement by circling the appropriate choice to the right of each statement. There are no right or wrong answers | Strongly disagree…1 | Disagree…2 | Undecided…3 | Agree…4 | Strongly agree…5 |
| 1. Drug addiction is associated with a weak will | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 2. A drug-dependent person cannot be helped until he/she has hit rock bottom | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 3. Heroin is so addictive that no one can really recover once he/she becomes an addict | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 4. Drug abusers should only be treated by specialists in that field | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 5. Smoking leads to marijuana use, which in turn leads to hard drugs | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 6. Daily use of one marijuana cigarette is not necessarily harmful | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 7. Urine drug screening can be an important part of drug abuse treatment | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 8. A physician who has been addicted to narcotics should not be allowed to practice medicine again | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 9. A drug-addicted person who has relapsed several times probably cannot be treated | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 10. Long-term outpatient treatment is necessary for the treatment of drug addiction | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 11. Paramedical professionals (psychologists, nurses, social workers…) can provide effective treatment for drug abusers | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 12. Paraprofessional counselors (trained volunteers, previous drug users) can provide effective treatment for drugs abusers | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 13. Once a person becomes drug-free through treatment, he can never become a social user | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 14. Drug addiction is a treatable illness | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 15. Group therapy is very important in the treatment of drug addiction | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 16. A hospital is the best place to treat a drug addict | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 17. Most drug-dependent persons are unpleasant to work with as patients | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 18. Pregnant women who use drugs should be punished | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 19. Coercive pressure, such as threat or punishment, is useful in getting resistant patients to accept treatment | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 20. Alcoholism is associated with a weak will | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 21. An alcohol- or drug- dependent person cannot be helped until he/she has hit rock bottom | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 22. Alcohol addiction should only be treated by specialists in that field | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 23. An alcohol-dependent person who has relapsed several times probably cannot be treated | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 24. Alcoholism is a treatable illness | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 25. Group therapy is very important in the treatment of alcoholism | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 26. A hospital is the best place to treat an alcoholic | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 27. Lifelong abstinence is a necessary goal in the treatment of alcoholism | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 28. Most alcohol-dependent persons are unpleasant to work with as patients | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 29. Pregnant women who use alcohol should be punished | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
- What is your gender?
- ○
- Man
- ○
- Woman
- ○
- Other
- You are between:
- ○
- 20–24 yrs old
- ○
- 25–29 yrs old
- ○
- 30–34 yrs old
- ○
- 35–39 yrs old
- ○
- >40 yrs old
- What is your first choice of specialty? free answer
- During your work experience have you ever been in contact with people with illicit substance use disorder? (cannabis, cocaine, heroin, amphetamines…)? multiple answers are possible
- ○
- None
- ○
- Yes, in the emergency room
- ○
- Yes, in a hospital department
- ○
- Yes, during a specialist consultation
- ○
- Yes, in an addiction center
- ○
- Yes, in a GP consultation
- ○
- Other, please specify: ______________
- Have you ever taken any of these drugs?
- ○
- Yes
- ○
- Cannabis
- ○
- Cocaine (cocaine, crack)
- ○
- Other psychostimulants (amphetamine, methamphetamine, MDMA, mephedrone…)
- ○
- Hallucinogens (LSD, Ketamine, mushrooms…)
- ○
- Hypnotics, sedatives (GHB/GBL…)
- ○
- Opiates (heroin, methadone, buprenorphine, fentanyl, morphine…)
- ○
- Inhalants
- ○
- Other, please specify: ______________
- ○
- No
- Have you ever been in contact within your own environment with one or more problematic users of substances other than tobacco? several answers are possible
- ○
- No
- ○
- Yes
- ○
- Cannabis
- ○
- Cocaine (cocaine, crack)
- ○
- Other psychostimulants (amphetamine, methamphetamine, MDMA, mephedrone …)
- ○
- Hallucinogens (LSD, Ketamine, mushrooms…)
- ○
- Hypnotics, sedatives (GHB/GBL…)
- ○
- Opiates (heroin, methadone, buprenorphine, fentanyl, morphine…)
- ○
- Inhalants
- ○
- Other, please specify: ______________
- In general, would you say your health is:
- ○
- Excellent
- ○
- Very Good
- ○
- Good
- ○
- Fair
- ○
- Poor
- What is the highest level of your parents’ education?Father Mother
- ○
- Elementary school a. Elementary school
- ○
- Lower secondary education b. Lower secondary education
- ○
- Higher secondary education c. Higher secondary education
- ○
- High school d. High School
- ○
- University e. University
- ○
- None f. None
- ○
- Unknown g. Unknown
- If you are of foreign origin or if you have opted for Belgian nationality, can you indicate your nationality of origin?
- Are one or both of your parents of a nationality other than Belgian, or have they ever been of a nationality other than Belgian?
- ○
- Yes
- ○
- No
| Indicate your degree of agreement or disagreement by circling the appropriate choice to the right of each statement. There are no right or wrong answers | Strongly Disagree…1 | Disagree…2 | Undecided…3 | Agree…4 | Strongly agree…5 |
| 1. Drug addiction is associated with a weak will | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 2. A drug-dependent person cannot be helped until he/she has hit rock bottom | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 3. Drug abusers should only be treated by specialists in that field | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 4. A physician who has been addicted to narcotics should not be allowed to practice medicine again | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 5. A drug-addicted person who has relapsed several times probably cannot be treated | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 6. Long-term outpatient treatment is necessary for the treatment of drug addiction | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 7. Paramedical professionals (psychologists, nurses, social workers…) can provide effective treatment for drug abusers | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 8. Paraprofessional counselors (trained volunteers, previous drug users) can provide effective treatment for drugs abusers | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 9. Drug addiction is a treatable illness | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 10. Group therapy is very important in the treatment of drug addiction | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 11. A hospital is the best place to treat a drug addict | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 12. Most drug-dependent persons are unpleasant to work with as patients | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 13. Pregnant women who use drugs should be punished | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 14. Coercive pressure, such as threat or punishment, is useful in getting resistant patients to accept treatment | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 15. Alcoholism is associated with a weak will | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 16. An alcohol-dependent person cannot be helped until he/she has hit rock bottom | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 17. Alcohol addiction should only be treated by specialists in that field | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 18. An alcohol-dependent person who has relapsed several times probably cannot be treated | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 19. Alcoholism is a treatable illness | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 20. Group therapy is very important in the treatment of alcoholism | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 21. A hospital is the best place to treat an alcoholic | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 22. Most alcohol-dependent persons are unpleasant to work with as patients | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 23. Pregnant women who use alcohol should be punished | Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
Appendix B. Additional Tables
| First factor analysis: |
| Heroin is so addictive that you cannot get off it once you become addicted. |
| Smoking a joint of marijuana every day leads in turn to hard drugs. |
| Smoking a marijuana joint every day is not necessarily bad for your health. |
| Urine drug testing can be an important part of management. |
| Once a person is no longer addicted to a drug, he or she can never again be a recreational user of that drug. |
| Second factor analysis: |
| Long-term abstinence is a necessary goal of alcohol treatment. |
| Variable | Stereotypes and Moralism | Optimism about Treatment | Specialized Treatment | ||||
|---|---|---|---|---|---|---|---|
| n (%) | Mean ± SD | p a | Mean ± SD | P a | Mean ± SD | p a | |
| Total | 615 (100) | 2.07 ± 0.55 | 2.94 ± 0.40 | 2.55 ± 0.67 | |||
| Maternal education level | 0.438 b | 0.684 | 0.460 | ||||
| Low | 48 (8.3) | 2.12 ± 0.53 | 2.96 ± 0.35 | 2.16 ± 0.64 | |||
| Medium | 110 (19.0) | 2.10 ± 0.60 | 2.92 ± 0.39 | 2.06 ± 0.54 | |||
| High | 421 (72.7) | 2.06 ± 0.52 | 2.95 ± 0.40 | 2.06 ± 0.52 | |||
| SUD in the entourage | 0.958 | 0.561 | 0.638 | ||||
| No | 222 (37.8) | 2.09 ± 0.54 | 2.92 ± 0.40 | 2.58 ± 0.69 | |||
| Alcohol | 83 (14.1) | 2.08 ± 0.50 | 2.99 ± 0.39 | 2.56 ± 0.61 | |||
| Cannabis | 41 (7.0) | 2.04 ± 0.50 | 2.91 ± 0.35 | 2.65 ± 0.57 | |||
| Alcohol–cannabis | 95 (16.2) | 2.05 ± 0.52 | 2.91 ± 0.38 | 2.49 ± 0.59 | |||
| Other drugs | 147 (25.0) | 2.09 ± 0.61 | 2.96 ± 0.41 | 2.52 ± 0.73 | |||
| Health perception | 0.617 | 0.466 | 0.310 | ||||
| Excellent | 111 (27.7) | 2.02 ± 0.53 | 2.97 ± 0.47 | 2.60 ± 0.70 | |||
| Very good | 191 (47.6) | 2.07 ± 0.55 | 2.93 ± 0.38 | 2.61 ± 0.63 | |||
| Good–satisfactory | 99 (24.7) | 2.01 ± 0.52 | 2.99 ± 0.36 | 2.49 ± 0.71 | |||
| Choice of medical specialty | 0.752 | 0.384 | 0.103 | ||||
| General Practice | 159 (25.9) | 2.08 ± 0.50 | 2.96 ± 0.38 | 2.44 ± 0.65 | |||
| Internal medicine | 78 (12.7) | 2.05 ± 0.60 | 2.94 ± 0.38 | 2.54 ± 0.68 | |||
| Pediatrics | 41 (6.7) | 2.06 ± 0.52 | 2.92 ± 0.36 | 2.59 ± 0.68 | |||
| Gynecology | 41 (6.7) | 1.96 ± 0.53 | 3.02 ± 0.36 | 2.46 ± 0.63 | |||
| Other | 296 (48.1) | 2.08 ± 0.56 | 2.91 ± 0.42 | 2.61 ± 0.67 |
Appendix C. Additional Figures
References
- Watson, H.; MacLaren, W.; Kerr, S. Staff attitudes towards working with drug users: Development of the Drug Problems Perceptions Questionnaire. Addiction 2007, 102, 206–215. [Google Scholar] [CrossRef]
- Richardson, G.B.; Smith, R.; Lowe, L.; Acquavita, S.P. Structure and longitudinal invariance of the Short Alcohol and Alcohol Problems Perception Questionnaire. J. Subst. Abus. Treat. 2020, 115, 108041. [Google Scholar] [CrossRef]
- Luty, J.; Fekadu, D.; Umoh, O.; Gallagher, J. Validation of a short instrument to measure stigmatised attitudes towards mental illness. Psychiatr. Bull. 2006, 30, 257–260. [Google Scholar] [CrossRef]
- Schaler, J.A. The Addiction Belief Scale. Int. J. Addict. 1995, 30, 117–134. [Google Scholar] [CrossRef]
- Humphreys, K.; Greenbaum, M.A.; Noke, J.M.; Finney, J.W. Reliability, validity, and normative data for a short version of the Understanding of Alcoholism Scale. Psychol. Addict. Behav. 1996, 10, 38–44. [Google Scholar] [CrossRef]
- Lindberg, M.; Vergara, C.; Wild-Wesley, R.; Gruman, C. Physicians-in-training Attitudes Toward Caring for and Working with Patients with Alcohol and Drug Abuse Diagnoses. South. Med. J. 2006, 99, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Cernasev, A.; Kline, K.M.; Barenie, R.E.; Hohmeier, K.C.; Stewart, S.; Forrest-Bank, S.S. Healthcare Professional Students’ Perspectives on Substance Use Disorders and Stigma: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 2776. [Google Scholar] [CrossRef]
- Chappel, J.N.; Veach, T.L.; Krug, R.S. The substance abuse attitude survey: An instrument for measuring attitudes. J. Stud. Alcohol 1985, 46, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Chappel, J.N.; Veach, T.L. Effect of a course on students’ attitudes toward substance abuse and its treatment. J. Med. Educ. 1987, 62, 394–400. [Google Scholar] [CrossRef]
- Jenkins, S.J.; Fisher, G.L.; Applegate, R.L. Factor Analysis of the Substance Abuse Attitude Survey with College Undergraduates. Psychol. Rep. 1990, 66, 331–336. [Google Scholar] [CrossRef]
- Pinikahana, J.; Happell, B.; Carta, B. Mental health professionals’ attitudes to drugs and substance abuse. Nurs. Health Sci. 2002, 4, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Puskar, K.; Gotham, H.J.; Terhorst, L.; Hagle, H.; Mitchell, A.M.; Braxter, B.; Fioravanti, M.; Kane, I.; Mpa, K.S.T.; Woomer, G.R.; et al. Effects of Screening, Brief Intervention, and Referral to Treatment (SBIRT) Education and Training on Nursing Students’ Attitudes Toward Working with Patients Who Use Alcohol and Drugs. Subst. Abus. 2013, 34, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Muzyk, A.; Mullan, P.; Andolsek, K.M.; DeRouin, A.; Smothers, Z.P.; Sanders, C.; Holmer, S. An Interprofessional Substance Use Disorder Course to Improve Students’ Educational Outcomes and Patients’ Treatment Decisions. Acad. Med. 2019, 94, 1792–1799. [Google Scholar] [CrossRef] [PubMed]
- Brief Substance Atittude Survey. Available online: https://medicine.yale.edu/sbirt/curriculum/modules/medicine/brief_substance_abuse_attitude_survey_100733_284_13474_v1.pdf (accessed on 29 December 2022).
- Richelle, L.; Dramaix-Wilmet, M.; Roland, M.; Kacenelenbogen, N. Factors influencing medical students’ attitudes towards substance use during pregnancy. BMC Med. Educ. 2022, 22, 335. [Google Scholar] [CrossRef]
- Hoffman, A. The support of drug users by general practitioners. 15 years after… Santé conjugué n°46. Fédérations des Maisons Médicales. 2008, 46, 8–10. [Google Scholar]
- Ketterer, F.; Symons, L.; Lambrechts, M.-C.; Mairiaux, P.; Godderis, L.; Peremans, L.; Remmen, R.; Vanmeerbeek, M. What factors determine Belgian general practitioners’ approaches to detecting and managing substance abuse? A qualitative study based on the I-Change Model. BMC Fam. Pract. 2014, 15, 119. [Google Scholar] [CrossRef]
- Gorsuch, R.L. Exploratory Factor Analysis: Its Role in Item Analysis. J. Pers. Assess. 1997, 68, 532–560. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Allyn and Bacon: New York, NY, USA, 2007. [Google Scholar]
- Bloom, B.S.; Engelhart, M.D.; Furst, E.J.; Hill, W.H.; Krathwohl, D.R. Taxonomy of Educational Objectives: The Classification of Educational Goals. In Handbook 1: Cognitive Domain; Bloom, B.S., Ed.; David McKay: New York, NY, USA, 1956. [Google Scholar]
- Anderson, L.W.; Krathwohl, D.R.; Airasian, P.W.; Cruikshank, K.A.; Mayer, R.E.; Pintrich, P.R.; Raths, J.; Wittrock, M.C. A Taxonomy for Learning, Teaching, and Assessing: A Revision of Bloom’s Taxonomy of Educational Objectives (Complete edition); Anderson, L.W., Krathwohl, D.R., Eds.; Longman: New York, NY, USA, 2001. [Google Scholar]
- ULB Gender Report. Available online: https://www.ulb.be/fr/egalite-des-genres/dernier-rapport-genre-disponible-rapport-2020-2021 (accessed on 29 December 2022).
- Burgess, A.; Oates, K.; Goulston, K. Role modelling in medical education: The importance of teaching skills. Clin. Teach. 2016, 13, 134–137. [Google Scholar] [CrossRef]
- Cruess, S.R.; Cruess, R.L.; Steinert, Y. Role modelling—Making the most of a powerful teaching strategy. BMJ 2008, 336, 718–721. [Google Scholar] [CrossRef]
- Kidd, J.D.; Smith, J.L.; Hu, M.-C.; Turrigiano, E.M.; Bisaga, A.; Nunes, E.V.; Levin, F.R. Medical Student Attitudes Toward Substance Use Disorders Before and After a Skills-Based Screening, Brief Intervention, and Referral to Treatment (SBIRT) Curriculum. Adv. Med. Educ. Pract. 2020, 11, 455–461. [Google Scholar] [CrossRef]
- Sarikhani, Y.; Shojaei, P.; Rafiee, M.; Delavari, S. Analyzing the interaction of main components of hidden curriculum in medical education using interpretive structural modeling method. BMC Med. Educ. 2020, 20, 176. [Google Scholar] [CrossRef] [PubMed]
- van Boekel, L.C.; Brouwers, E.P.; van Weeghel, J.; Garretsen, H.F. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug Alcohol Depend. 2013, 131, 23–35. [Google Scholar] [CrossRef]
- Garpenhag, L.; Dahlman, D. Perceived healthcare stigma among patients in opioid substitution treatment: A qualitative study. Subst. Abus. Treat. Prev. Policy 2021, 16, 81. [Google Scholar] [CrossRef] [PubMed]
- Muncan, B.; Walters, S.M.; Ezell, J.; Ompad, D.C. “They look at us like junkies”: Influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduct. J. 2020, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Goodyear, K.; Chavanne, D. Sociodemographic Characteristics and the Stigmatization of Prescription Opioid Addiction. J. Addict. Med. 2020, 14, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Rowe, T.A.; Jacapraro, J.S.; Rastegar, D.A. Entry into primary care-based buprenorphine treatment is associated with identification and treatment of other chronic medical problems. Addict. Sci. Clin. Pract. 2012, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Buresh, M.; Stern, R.; Rastegar, D. Treatment of opioid use disorder in primary care. BMJ 2021, 373, n784. [Google Scholar] [CrossRef]
- Rombouts, S.A.; Conigrave, J.H.; Saitz, R.; Louie, E.; Haber, P.; Morley, K.C. Evidence based models of care for the treatment of alcohol use disorder in primary health care settings: A systematic review. BMC Fam. Pract. 2020, 21, 260. [Google Scholar] [CrossRef]
- Mahood, S.C. Medical education: Beware the hidden curriculum. Can. Fam. Physician 2011, 57, 983–985. [Google Scholar]
- Livingston, J.D.; Milne, T.; Fang, M.L.; Amari, E. The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction 2012, 107, 39–50. [Google Scholar] [CrossRef]
- Wood, E.; Samet, J.H.; Volkow, N.D. Physician Education in Addiction Medicine. JAMA 2013, 310, 1673–1674. [Google Scholar] [CrossRef] [PubMed]
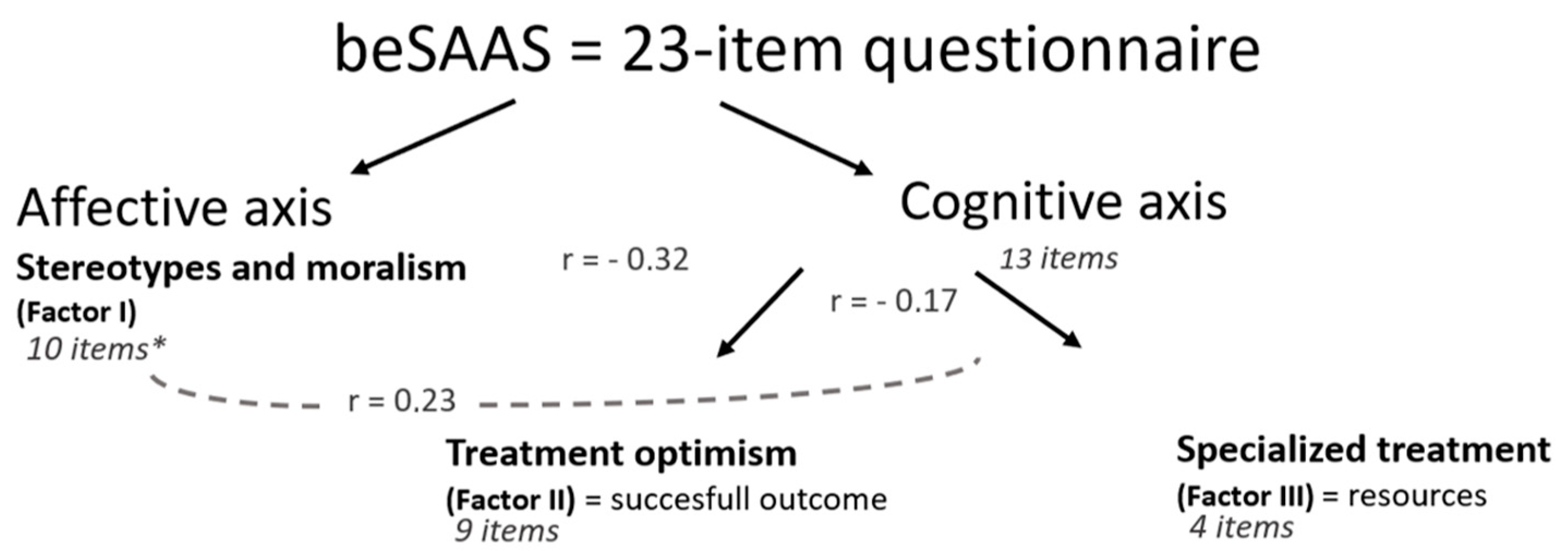
| Items | Factor I: Stereotypes and Moralism | Factor II: Treatment Optimism | Factor III: Specialized Treatment |
|---|---|---|---|
| Factor Loadings | |||
| Drug addiction is associated with a weak will | 0.60 | ||
| A drug-dependent person cannot be helped until he/she has hit rock bottom | 0.39 | ||
| Drug abusers should only be treated by specialists in that field | 0.44 | ||
| A physician who has been addicted to narcotics should not be allowed to practice medicine again | 0.36 | ||
| A drug-addicted person who has relapsed several times probably cannot be treated | −0.37 | ||
| Long-term outpatient treatment is necessary for the treatment of drug addiction | 0.30 | ||
| Paramedical professionals (psychologists, nurses, social workers…) can provide effective treatment for drug abusers | 0.43 | ||
| Paraprofessional counselors (trained volunteers, previous drug users) can provide effective treatment for drugs abusers | 0.40 | ||
| Drug addiction is a treatable illness | 0.46 | ||
| Group therapy is very important in the treatment of drug addiction | 0.53 | ||
| A hospital is the best place to treat a drug addict | 0.51 | ||
| Most drug-dependent persons are unpleasant to work with as patients | 0.38 | ||
| Pregnant women who use drugs should be punished | 0.76 | ||
| Coercive pressure, such as threat or punishment, is useful in getting resistant patients to accept treatment | 0.48 | ||
| Alcoholism is associated with a weak will | 0.65 | ||
| An alcohol- dependent person cannot be helped until he/she has hit rock bottom | 0.44 | ||
| Alcohol should only be treated by specialists in that field | 0.53 | ||
| An alcohol-dependent person who has relapsed several times probably cannot be treated | −0.45 | ||
| Alcoholism is a treatable illness | 0.53 | ||
| Group therapy is very important in the treatment of alcoholism | 0.61 | ||
| A hospital is the best place to treat an alcoholic | 0.56 | ||
| Most alcohol-dependent persons are unpleasant to work with as patients | 0.42 | ||
| Pregnant women who use alcohol should be punished | 0.76 | ||
| Eigenvalues | 4.0 | 1.7 | 1.3 |
| Cronbach’s alpha | 0.80 | 0.70 | 0.59 |
| % of variance explained | 40.3 | 17.1 | 12.6 |
| % of total variance explained: 70.0 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Richelle, L.; Dramaix-Wilmet, M.; Kacenelenbogen, N.; Kornreich, C. Exploratory Factor Analysis of a French Adapted Version of the Substance Abuse Attitude Survey among Medical Students in Belgium. Int. J. Environ. Res. Public Health 2023, 20, 5356. https://doi.org/10.3390/ijerph20075356
Richelle L, Dramaix-Wilmet M, Kacenelenbogen N, Kornreich C. Exploratory Factor Analysis of a French Adapted Version of the Substance Abuse Attitude Survey among Medical Students in Belgium. International Journal of Environmental Research and Public Health. 2023; 20(7):5356. https://doi.org/10.3390/ijerph20075356
Chicago/Turabian StyleRichelle, Lou, Michèle Dramaix-Wilmet, Nadine Kacenelenbogen, and Charles Kornreich. 2023. "Exploratory Factor Analysis of a French Adapted Version of the Substance Abuse Attitude Survey among Medical Students in Belgium" International Journal of Environmental Research and Public Health 20, no. 7: 5356. https://doi.org/10.3390/ijerph20075356
APA StyleRichelle, L., Dramaix-Wilmet, M., Kacenelenbogen, N., & Kornreich, C. (2023). Exploratory Factor Analysis of a French Adapted Version of the Substance Abuse Attitude Survey among Medical Students in Belgium. International Journal of Environmental Research and Public Health, 20(7), 5356. https://doi.org/10.3390/ijerph20075356






