Handgrip Strength Is Positively Associated with 24-hour Urine Creatine Concentration
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Hand Grip Strength Measurement
2.3. 24-h Urine Creatinine Collection and Measurement
2.4. Other Variables and Measurements
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abd Kahar, N.S.; Kuan, C.S.; Singh, D.K.; Mokhtar, S.A. Risk Factors Associated with Fragility Fracture Among Older Adults with Fragility Fracture: A Systematic Review. Mal. J. Med. Health Sci. 2022, 18, 318–326. [Google Scholar] [CrossRef]
- Bautmans, I.; Gorus, E.; Njemini, R.; Mets, T.; Njemini, R. Handgrip performance in relation to self-perceived fatigue, physical functioning and circulating IL-6 in elderly persons without inflammation. BMC Geriatr. 2007, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Au, I.L.Y.; Lau, N.Y.N.; Lee, S.K.W.; Tiu, K.L.; Lee, K.B.; Chan, A.C.M. Handgrip strength is associated with length of stay and functional outcomes at 1-year follow up in fragility hip fracture patients. J. Orthop. Trauma Rehabil. 2022, 29, 22104917221095255. [Google Scholar] [CrossRef]
- Kunutsor, S.K.; Seidu, S.; Voutilainen, A.; Blom, A.W.; Laukkanen, J.A. Handgrip strength—A risk indicator for future fractures in the general population: Findings from a prospective study and meta-analysis of 19 prospective cohort studies. Geroscience 2021, 43, 869–880. [Google Scholar] [CrossRef] [PubMed]
- Contreras-Bolívar, V.; Sánchez-Torralvo, F.J.; Ruiz-Vico, M.; González-Almendros, I.; Barrios, M.; Padín, S.; Alba, E.; Olveira, G. GLIM criteria using hand grip strength adequately predict six-month mortality in cancer inpatients. Nutrients 2019, 11, 2043. [Google Scholar] [CrossRef]
- Bahat, G.; Tufan, A.; Tufan, F.; Kilic, C.; Akpinar, T.S.; Kose, M.; Erten, N.; Karan, M.A.; Cruz-Jentoft, A.J. Cut-off points to identify sarcopenia according to European Working Group on Sarcopenia in Older People (EWGSOP) definition. Clin. Nutr. 2016, 35, 1557–1563. [Google Scholar] [CrossRef]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307. [Google Scholar] [CrossRef]
- Donini, L.M.; Busetto, L.; Bischoff, S.C.; Cederholm, T.; Ballesteros-Pomar, M.D.; Batsis, J.A.; Bauer, J.M.; Boirie, Y.; Cruz-Jentoft, A.J.; Dicker, D.; et al. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO consensus statement. Obes. Facts 2022, 15, 321–335. [Google Scholar] [CrossRef]
- Murawiak, M.; Krzymińska-Siemaszko, R.; Kaluźniak-Szymanowska, A.; Lewandowicz, M.; Tobis, S.; Wieczorowska-Tobis, K.; Deskur-Śmielecka, E. Sarcopenia, Obesity, Sarcopenic Obesity and Risk of Poor Nutritional Status in Polish Community-Dwelling Older People Aged 60 Years and Over. Nutrients 2022, 14, 2889. [Google Scholar] [CrossRef]
- McPherson, R.A.; Matthew, R.P. Henry’s Clinical Diagnosis and Management by Laboratory Methods E-Book; Elsevier: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Heymsfield, S.B.; Arteaga, C.; McManus, C.; Smith, J.; Moffitt, S. Measurement of muscle mass in humans: Validity of the 24-hour urinary creatinine method. Am. J. Clin. Nutr. 1983, 37, 478–494. [Google Scholar] [CrossRef]
- Delanaye, P.; Cavalier, E.; Maillard, N.; Krzesinski, J.M.; Mariat, C.; Cristol, J.P.; Piéroni, L. Creatinine: Past and present. Ann. De Biol. Clin. 2010, 68, 5. [Google Scholar]
- Curcio, F.; Ferro, G.; Basile, C.; Liguori, I.; Parrella, P.; Pirozzi, F.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Tocchetti, C.G.; et al. Biomarkers in sarcopenia: A multifactorial approach. Exp. Gerontol. 2016, 85, 1–8. [Google Scholar] [CrossRef]
- Keller, U. Nutritional laboratory markers in malnutrition. J. Clin. Med. 2019, 8, 775. [Google Scholar] [CrossRef]
- Sallsten, G.; Lars, B. Variability of urinary creatinine in healthy individuals. Int. J. Environ. Res. Public Health 2021, 18, 3166. [Google Scholar] [CrossRef]
- Baxmann, A.C.; Ahmed, M.S.; Marques, N.C.; Menon, V.B.; Pereira, A.B.; Kirsztajn, G.M.; Heilberg, I.P. Influence of muscle mass and physical activity on serum and urinary creatinine and serum cystatin C. Clin. J. Am. Soc. Nephrol. 2008, 3, 348–354. [Google Scholar] [CrossRef]
- Oterdoom, L.H.; Gansevoort, R.T.; Schouten, J.P.; de Jong, P.E.; Gans, R.O.; Bakker, S.J. Urinary creatinine excretion, an indirect measure of muscle mass, is an independent predictor of cardiovascular disease and mortality in the general population. Atherosclerosis 2009, 207, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Poppe, E.S.; Polinder-Bos, H.A.; Huberts, M.; Vogels, S.; Ipema, K.J.; Gansevoort, R.T.; Westerhuis, R.; Bakker, S.J.; Gaillard, C.A.; Franssen, C.F. Creatinine synthesis rate and muscle strength and self-reported physical health in dialysis patients. Clin. Nutr. 2020, 39, 1600–1607. [Google Scholar] [CrossRef] [PubMed]
- Iacone, R.; D’Elia, L.; Guida, B.; Barbato, A.; Scanzano, C.; Strazzullo, P. Validation of daily urinary creatinine excretion measurement by muscle-creatinine equivalence. J. Clin. Lab. Anal. 2018, 32, e22407. [Google Scholar] [CrossRef]
- Riebe, D.; Ehrman, J.K.; Liguori, G.; Magal, M.; American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2018. [Google Scholar]
- Altankhuyag, I.; Byambaa, A.; Tuvshinjargal, A.; Bayarmunkh, A.; Jadamba, T.; Dagvajantsan, B.; Byambasukh, O. Association between hand-grip strength and risk of stroke among Mongolian adults: Results from a population-based study. Neurosci. Res. Notes 2021, 4 (Suppl. 3), 8–16. [Google Scholar] [CrossRef]
- Delanghe, J.R.; Marijn, M. Speeckaert. Creatinine determination according to Jaffe—What does it stand for? Nephrol. Dial. Transplant. Plus 2011, 4, 83–86. [Google Scholar]
- Bergland, A.; Langhammer, B. EU-Rapport Regarding Ageing, Disability and Physical Activity in Norway; Oslo University College: Oslo, Norway, 2005. [Google Scholar]
- Kuriyan, R.; Kurpad, A.V. Prediction of total body muscle mass from simple anthropometric measurements in young Indian males. Indian J. Med. Res. 2004, 119, 121. [Google Scholar] [PubMed]
- Kawasaki, T.; Uezono, K.; Itoh, K.; Ueno, M. Prediction of 24-hour urinary creatinine excretion from age, body weight and height of an individual and its application. Jpn. J. Public Health 1991, 38, 567–574. [Google Scholar]
- Ix, J.H.; de Boer, I.H.; Wassel, C.L.; Criqui, M.H.; Shlipak, M.G.; Whooley, M.A. Urinary creatinine excretion rate and mortality in persons with coronary artery disease: The Heart and Soul Study. Circulation 2010, 121, 1295–1303. [Google Scholar] [CrossRef] [PubMed]
- Afsar, B.; Elsurer, R.; Guner, E.; Kirkpantur, A. Which anthropometric parameter is best related with urinary albumin excretion and creatinine clearance in type 2 diabetes: Body mass index, waist circumference, waist-to-hip ratio, or conicity index? J. Ren. Nutr. 2011, 21, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.M.; Gallagher, D.; Nelson, M.; Matthews, D.; Heymsfield, S.B. Total-body skeletal muscle mass: Evaluation of 24-h urinary creatinine excretion by computerized axial tomography. Am. J. Clin. Nutr. 1996, 63, 863–869. [Google Scholar] [CrossRef]
- van Hoeyweghen, R.J.; De Leeuw, I.H.; Vandewoude, M.F. Creatinine arm index as alternative for creatinine height index. Am. J. Clin. Nutr. 1992, 56, 611–615. [Google Scholar] [CrossRef]
- Blackburn, G.; Benotti, P.; Bistrian, B.; Bothe, A.; Maini, B.; Schlamm, H.; Smith, M. Nutritional Assessment and Treatment of Hospital Malnutrition. Transfus. Med. Hemoth. 1979, 6, 238–250. [Google Scholar] [CrossRef]
- Byambasukh, O.; Eisenga, M.F.; Gansevoort, R.T.; Bakker, S.J.; Corpeleijn, E. Body fat estimates from bioelectrical impedance equations in cardiovascular risk assessment: The PREVEND cohort study. Eur. J. Prev. Cardiol. 2019, 26, 905–916. [Google Scholar] [CrossRef]
- Walser, M. Creatinine excretion as a measure of protein nutrition in adults of varying age. J. Parenter. Enter. Nutr. 1987, 11, S73–S78. [Google Scholar] [CrossRef]
- Oosterwijk, M.M.; Braber, N.; Bakker, S.J.; Laverman, G.D. Urinary creatinine excretion is an indicator of physical performance and function. J. Cachexia Sarcopenia Muscle 2022, 13, 1431. [Google Scholar] [CrossRef]
- Neubert, A.; Remer, T. The impact of dietary protein intake on urinary creatinine excretion in a healthy pediatric population. J. Pediatr. 1998, 133, 655–659. [Google Scholar] [CrossRef] [PubMed]
- Kesteloot, H.; Joossens, J.V. Relationship between dietary protein intake and serum urea, uric acid and creatinine, and 24-hour urinary creatinine excretion: The BIRNH Study. J. Am. Coll. Nutr. 1993, 12, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Byambasukh, O.; Bayarmunkh, A.; Byambaa, A.; Tuvshinjargal, A.; Bor, D.; Ganbaatar, U.; Dagvajantsan, B.; Jadamba, T. The Contributions of Food Groups to the Daily Caloric Intake in Mongolian Population: A Mon-Timeline Study. Nutrients 2021, 13, 4062. [Google Scholar] [CrossRef] [PubMed]
| Findings | Total | 24-h Urine Creatinine Level | p-Value | ||
|---|---|---|---|---|---|
| T1 | T2 | T3 | |||
| Male (n) | 161 | 53 | 54 | 54 | |
| Age (years) | 42.5 ± 9.6 | 46.8 ± 10.8 | 41.1 ± 8.6 | 39.8 ± 7.8 | 0.002 |
| Height (cm) | 169.0 ± 8.2 | 168.1 ± 8.3 | 169.4 ± 7.5 | 169.6 ± 8.7 | 0.551 |
| Weight (kg) | 78.7 ± 14.1 | 77.9 ± 14.1 | 77.3 ± 14.2 | 80.9 ± 13.9 | 0.364 |
| BMI (kg/m2) | 28.9 ± 17.0 | 27.3 ± 3.4 | 27.0 ± 3.7 | 32.3 ± 28.7 | 0.144 |
| Systolic blood pressure (mmHg) | 114.5 ± 12.9 | 116.1 ± 11.7 | 115.4 ± 12.1 | 111.9 ± 13.4 | 0.401 |
| Muscle mass (kg) | 53.5 ± 38.3 | 50.0 ± 10.5 | 57.9 ± 65.1 | 52.5 ± 10.3 | 0.372 |
| Neck circumference (cm) | 39.2 ± 5.0 | 38.1 ± 4.0 | 39.8 ± 7.1 | 39.6 ± 3.0 | 0.054 |
| Waist circumference (cm) | 92.3 ± 10.9 | 92.0 ± 10.4 | 90.5 ± 11.7 | 94.5 ± 10.3 | 0.240 |
| Hip circumference (cm) | 100.3 ± 8.3 | 101.0 ± 8.1 | 100.0 ± 8.5 | 99.9 ± 8.5 | 0.741 |
| Upper arm circumference (cm) | 33.5 ± 25.9 | 31.2 ± 4.1 | 37.6 ± 4.2 | 31.6 ± 3.9 | 0.589 |
| Lower arm circumference (cm) | 23.5 ± 4.6 | 23.4 ± 4.5 | 23.5 ± 4.6 | 23.7 ± 4.7 | 0.839 |
| Tigh circumference (cm) | 54.7 ± 6.4 | 53.6 ± 6.1 | 54.6 ± 6.7 | 56.0 ± 6.3 | 0.108 |
| Hand grip strength (kg) | 43.7 ± 12.8 | 38.0 ± 14.1 | 45.6 ± 11.3 | 47.5 ± 11.1 | 0.002 |
| Meat intake (daily) | 98.1 (158) | 98.1 (52) | 96.3 (52) | 100.0 (54) | 0.363 |
| Fruit and vegetable intake (daily) | 5.0 (8) | 5.7 (3) | 1.9 (1) | 7.4 (4) | 0.398 |
| Regular physical activity (weekly) | 42.2 (68) | 41.5 (22) | 38.9 (21) | 46.3 (25) | 0.732 |
| Education (lower level) | 13.0 (21) | 11.3 (6) | 14.8 (8) | 13.0 (7) | 0.801 |
| Alcohol use (weekly) | 24.8 (40) | 35.8 (19) | 18.5 (10) | 20.4 (11) | 0.075 |
| Smokers | 55.3 (89) | 47.2 (25) | 53.7 (29) | 64.8 (35) | 0.178 |
| Female (n) | 149 | 49 | 50 | 50 | |
| Age (years) | 45.1 ± 9.4 | 49.8 ± 9.8 | 44.1 ± 8.6 | 41.6 ± 7.9 | <0.001 |
| Height (cm) | 164.6 ± 8.2 | 165.0 ± 8.3 | 164.0 ± 8.5 | 164.8 ± 7.9 | 0.790 |
| Weight (kg) | 73.2 ± 12.9 | 75.4 ± 13.1 | 72.0 ± 12.2 | 72.4 ± 13.5 | 0.366 |
| BMI (kg/m2) | 26.9 ± 3.7 | 27.6 ± 3.6 | 26.8 ± 3.7 | 26.4 ± 3.7 | 0.227 |
| Systolic blood pressure (mmHg) | 117.5 ± 11.4 | 118.3 ± 9.9 | 116.1 ± 11.9 | 118.1 ± 10.9 | 0.401 |
| Muscle mass (kg) | 45.7 ± 9.5 | 46.8 ± 10.1 | 44.8 ± 8.5 | 45.7 ± 9.9 | 0.867 |
| Neck circumference (cm) | 36.7 ± 3.7 | 37.3 ± 3.2 | 36.4 ± 4.4 | 36.3 ± 3.3 | 0.331 |
| Waist circumference (cm) | 88.1 ± 12.0 | 91.2 ± 11.6 | 86.3 ± 11.5 | 87.0 ± 12.5 | 0.094 |
| Hip circumference (cm) | 99.2 ± 8.2 | 100.7 ± 7.6 | 98.1 ± 8.1 | 98.6 ± 8.8 | 0.231 |
| Upper arm circumference (cm) | 30.2 ± 3.6 | 30.7 ± 3.5 | 29.9 ± 4.0 | 30.1 ± 3.3 | 0.245 |
| Lower arm circumference (cm) | 23.6 ± 4.0 | 24.0 ± 3.7 | 23.7 ± 3.7 | 22.9 ± 4.6 | 0.322 |
| Tigh circumference (cm) | 53.1 ± 6.1 | 52.4 ± 6.2 | 53.6 ± 6.3 | 53.4 ± 5.7 | 0.503 |
| Hand grip strength (kg) | 33.0 ± 13.8 | 30.8 ± 14.8 | 29.9 ± 10.9 | 38.2 ± 13.9 | 0.009 |
| Meat intake (daily) | 98.0 (146) | 95.9 (47) | 98.0 (49) | 100.0 (50) | 0.352 |
| Fruit and vegetable intake (daily) | 4.0 (6) | 4.1 (2) | 6.0 (3) | 2.0 (1) | 0.596 |
| Regular physical activity (weekly) | 37.2 (55) | 30.6 (15) | 40.0 (20) | 40.8 (20) | 0.508 |
| Education (lower level) | 10.1 (15) | 8.2 (4) | 12.0 (6) | 10.0 (5) | 0.782 |
| Alcohol use (weekly) | 18.1 (27) | 22.4 (11) | 14.0 (7) | 18.0 (9) | 0.694 |
| Smokers | 38.9 (58) | 34.7 (17) | 40.0 (20) | 42.0 (21) | 0.744 |
| 24 hCER | Male | Female | ||
|---|---|---|---|---|
| r | p-Value | r | p-Value | |
| Age | −0.307 | <0.001 | −0.309 | <0.001 |
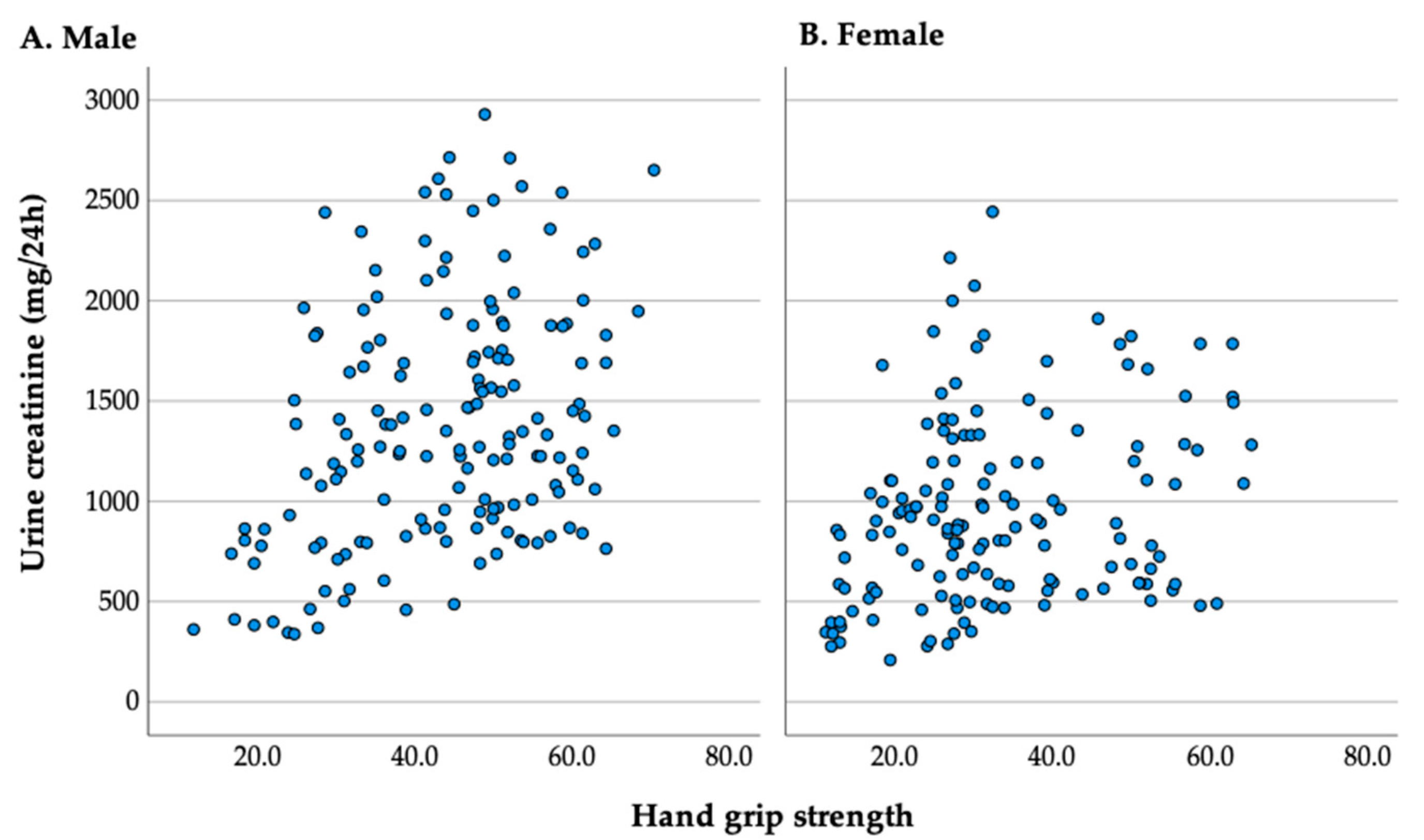
| HGS | 0.207 | 0.011 | 0.273 | 0.002 |
| BMI | 0.097 | 0.237 | −0.037 | 0.680 |
| Muscle mass | 0.018 | 0.831 | −0.016 | 0.857 |
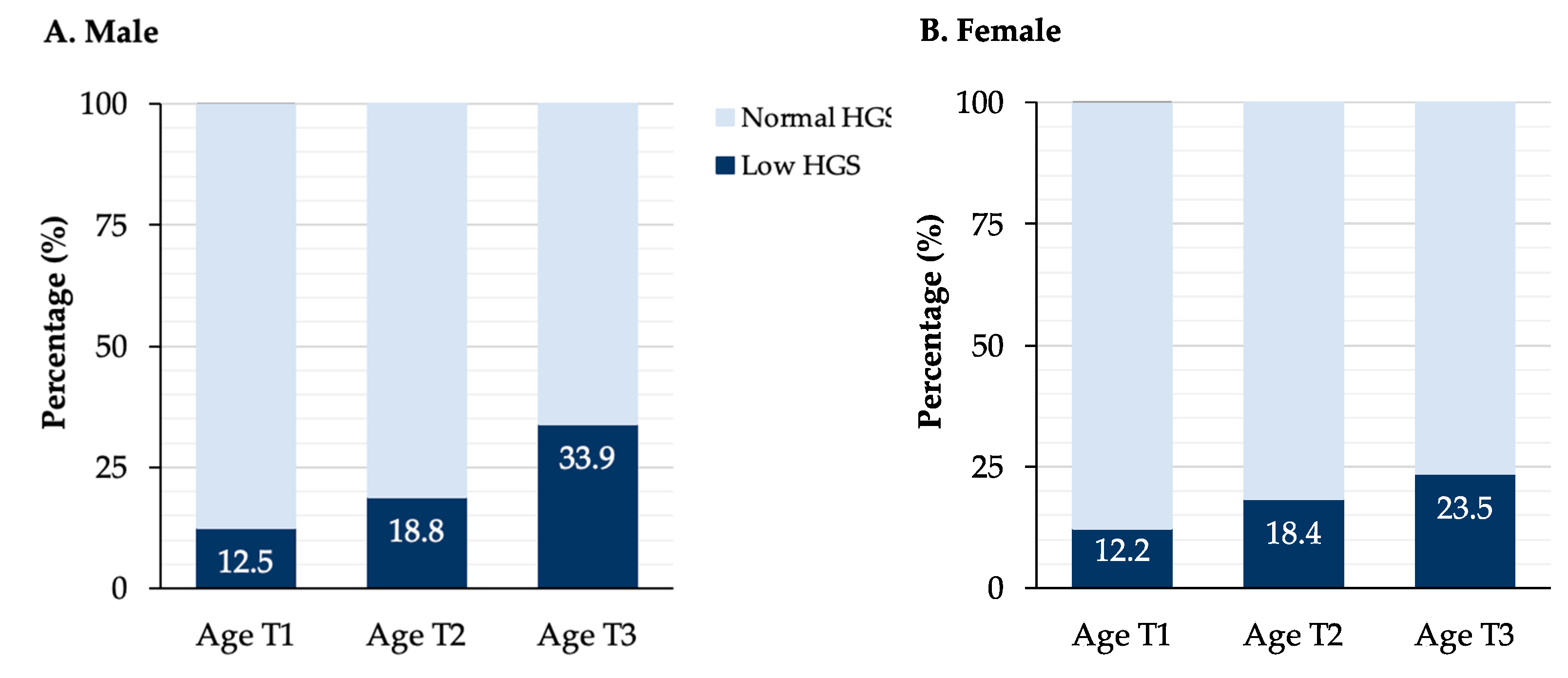
| Age Groups | Total | HGS Category | ||
|---|---|---|---|---|
| Normal | Low | p-Value | ||
| Male | ||||
| Age tertile 1 | 1556.0 ± 540.1 | 1574.0 ± 541.0 | 1434.1 ± 554.2 | 0.528 |
| Age tertile 2 | 1507.0 ± 649.0 | 1620.1 ± 589.2 | 1020.1 ± 705.3 | 0.011 |
| Age tertile 3 | 1115.1 ± 517.2 | 1297.1 ± 516.2 | 759.1 ± 288.3 | <0.001 |
| Total | 1387.1 ± 598.9 | 1506.2 ± 562.3 | 961.2 ± 534.1 | <0.001 |
| Female | ||||
| Age tertile 1 | 1138.1 ± 566.4 | 1184.3 ± 562.9 | 805.3 ± 521.9 | 0.126 |
| Age tertile 2 | 1014.5 ± 436.1 | 1095.4 ± 424.4 | 653.2 ± 291.4 | 0.005 |
| Age tertile 3 | 739.4 ± 367.8 | 776.1 ± 385.1 | 619.4 ± 278.3 | 0.199 |
| Total | 960.1 ± 489.3 | 1024.2 ± 495.5 | 672.2 ± 341.7 | <0.001 |
| HGS | Unstandardized Beta Coefficient of 24 hCER | |||
|---|---|---|---|---|
| Male | Female | |||
| β (95% CI) | p-Value | β (95% CI) | p-Value | |
| Crude | 16.1 (9.3–22.9) | <0.001 | 8.6 (3.3–13.9) | 0.002 |
| Adjusted for age | 12.5 (5.3–19.6) | <0.001 | 8.1 (3.1–13.1) | 0.002 |
| Adjusted for age and education | 11.1 (3.9–18.1) | 0.002 | 8.2 (3.2–13.3) | 0.002 |
| Adjusted for age and BMI | 12.1 (5.1–19.0) | <0.001 | 8.2 (2.9–13.1) | 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ulambayar, E.; Bor, D.; Sukhbaatar, N.-E.; Usukhbayar, N.; Ganbold, U.; Byambasuren, O.; Enkhbayar, U.; Byambasukh, O. Handgrip Strength Is Positively Associated with 24-hour Urine Creatine Concentration. Int. J. Environ. Res. Public Health 2023, 20, 5191. https://doi.org/10.3390/ijerph20065191
Ulambayar E, Bor D, Sukhbaatar N-E, Usukhbayar N, Ganbold U, Byambasuren O, Enkhbayar U, Byambasukh O. Handgrip Strength Is Positively Associated with 24-hour Urine Creatine Concentration. International Journal of Environmental Research and Public Health. 2023; 20(6):5191. https://doi.org/10.3390/ijerph20065191
Chicago/Turabian StyleUlambayar, Enkhtuya, Delgermaa Bor, Nandin-Erdene Sukhbaatar, Narkhajid Usukhbayar, Uugantuya Ganbold, Odmaa Byambasuren, Uranbaigali Enkhbayar, and Oyuntugs Byambasukh. 2023. "Handgrip Strength Is Positively Associated with 24-hour Urine Creatine Concentration" International Journal of Environmental Research and Public Health 20, no. 6: 5191. https://doi.org/10.3390/ijerph20065191
APA StyleUlambayar, E., Bor, D., Sukhbaatar, N.-E., Usukhbayar, N., Ganbold, U., Byambasuren, O., Enkhbayar, U., & Byambasukh, O. (2023). Handgrip Strength Is Positively Associated with 24-hour Urine Creatine Concentration. International Journal of Environmental Research and Public Health, 20(6), 5191. https://doi.org/10.3390/ijerph20065191







