Effects of Muscle Strength, Agility, and Fear of Falling on Risk of Falling in Older Adults
Abstract
1. Introduction
Current Study
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measurement Outcomes
2.4. Statistical Analyses
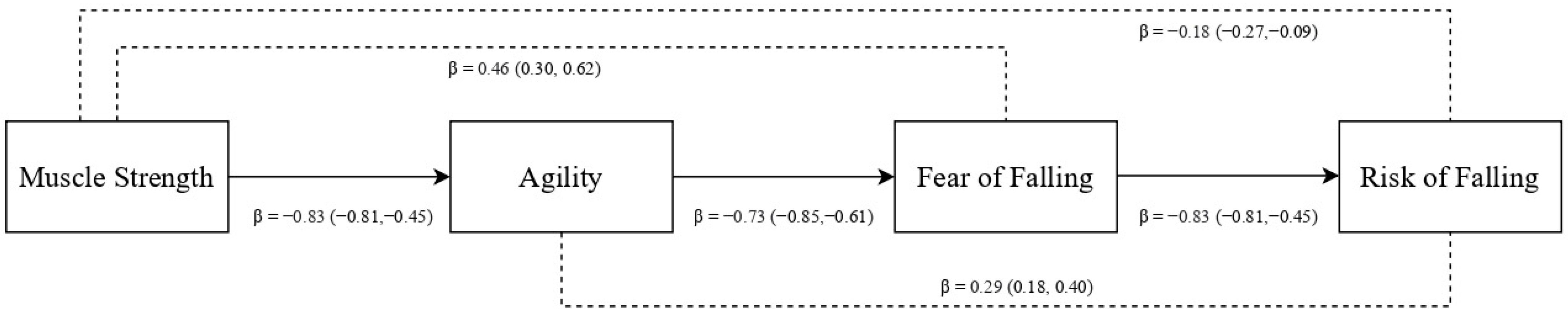
3. Results
4. Discussion
Limitations, Strengths, and Agenda for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ha, V.T.; Nguyen, T.N.; Nguyen, T.X.; Nguyen, H.; Nguyen, T.; Nguyen, A.T.; Pham, T.; Vu, H. Prevalence and factors associated with falls among older outpatients. Int. J. Environ. Res. Public Health 2021, 18, 4041. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef] [PubMed]
- O’Loughlin, J.L.; Robitaille, Y.; Boivin, J.F.; Suissa, S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am. J. Epidemiol. 1993, 137, 342–354. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.; Domingos, C.; Monteiro, D.; Morouço, P. A Review on aging, sarcopenia, falls, and resistance training in community-dwelling older adults. Int. J. Environ. Res. Public Health 2022, 19, 874. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Lamb, S.E.; Gates, S.; Cumming, R.G.; Rowe, B.H. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2009, 2, CD007146. [Google Scholar]
- Berry, S.D.; Miller, R.R. Falls: Epidemiology, pathophysiology, and relationship to fracture. Curr. Osteoporos. Rep. 2008, 6, 149–154. [Google Scholar] [CrossRef]
- Vellas, B.J.; Wayne, S.J.; Romero, L.; Baumgartner, R.N.; Rubenstein, L.Z.; Garry, P.J. One-leg balance is an important predictor of injurious falls in older persons. J. Am. Geriatr. Soc. 1997, 45, 735–738. [Google Scholar] [CrossRef]
- Monteiro, M.; Rodrigues, F.; Forte, P.; Carvalho, J. The influence of an eight-month multicomponent training program in elderly’s gait and bone mineral mass. BMC Health Serv. Res. 2018, 18, 684. [Google Scholar]
- Ambrose, A.F.; Cruz, L.; Paul, G. Falls and Fractures: A systematic approach to screening and prevention. Maturitas 2015, 82, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Brill, P.A.; Macera, C.A.; Davis, D.R.; Blair, S.N.; Gordon, N. Muscular strength and physical function. Med. Sci. Sports Exerc. 2000, 32, 412–416. [Google Scholar] [CrossRef]
- Rodrigues, F.; Amaro, N.; Matos, R.; Mendes, D.; Monteiro, D.; Morouço, P. The impact of an exercise intervention using low-cost equipment on functional fitness in the community-dwelling older adults: A pilot study. Front. Physiol. 2022, 13, 1039131. [Google Scholar] [CrossRef]
- Spidurso, W.W.; Francis, K.L.; MacRae, P.G. Physical Dimensions of Aging, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2005. [Google Scholar]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. European Working group on sarcopenia in older people. Sarcopenia: European consensus on definition and diagnosis: Report of the uropean working group on sarcopenia in older people. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Milanović, Z.; Pantelić, S.; Trajković, N.; Sporiš, G.; Kostić, R.; James, N. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin. Interv. Aging 2013, 8, 549–556. [Google Scholar] [CrossRef]
- Donath, L.; van Dieën, J.; Faude, O. Exercise-based fall prevention in the elderly: What about agility? Sports Med. 2016, 46, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Shimada, H.; Tiedemann, A.; Lord, S.R.; Suzukawa, M.; Makizako, H.; Kobayashi, K.; Suzuki, T. Physical factors underlying the association between lower walking performance and falls in older people: A structural equation model. Arch. Gerontol. Geriatr. 2011, 53, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Mendes de Leon, C.F.; Doucette, J.T.; Baker, D.I. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J. Gerontol. 1994, 49, M140–M147. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Branch, L.G.; Cummings, S.R.; Curb, J.D. Physical performance measures in aging research. J. Gerontol. 1989, 44, M141–M146. [Google Scholar] [CrossRef]
- Garbin, A.J.; Fisher, B.E. The interplay between fear of falling, balance performance, and future falls: Data From the national health and aging trends study. J. Geriatr. Phys. Ther. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Smith, H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist 2002, 42, 17–23. [Google Scholar] [CrossRef]
- Jørstad, E.C.; Hauer, K.; Becker, C.; Lamb, S.E.; on behalf of the ProFaNE Group. Measuring the psychological outcomes of falling: A systematic review. J. Am. Geriatr. Soc. 2005, 53, 501–510. [Google Scholar] [CrossRef]
- Forte, P.; Pinto Barbosa, T.; Morais, J.; Monteiro, A. The effect of a six-month multicomponent training in elderly’s body composition and functional fitness—A before-after analysis. Motricidade 2021, 17, 34–41. [Google Scholar]
- Monteiro, A.M.; Forte, P.; Carvalho, J.; Barbosa, T.M.; Morais, J.E. Relationship between fear of falling and balance factors in healthy elderly women: A confirmatory analysis. J. Women Aging 2021, 33, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.; Jones, J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Health 1992, 83, 7–11. [Google Scholar]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef]
- Muthén, L.; Muthén, B. Mplus User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2010. [Google Scholar]
- Hair, J.; Black, W.; Babin, B.; Anderson, R. Multivariate Data Analysis, 8th ed.; Pearson Educational, Inc.: London, UK, 2019. [Google Scholar]
- Williams, J.; Mackinnon, D. Resampling and distribution of the product methods for testing indirect effects in complex models. Struct. Equ. Model. 2008, 15, 23–51. [Google Scholar] [CrossRef]
- Rodrigues, F.; Jacinto, M.; Figueiredo, N.; Monteiro, A.M.; Forte, P. Effects of a 24-Week Low-Cost Multicomponent Exercise Program on Health-Related Functional Fitness in the Community-Dwelling Aged and Older Adults. Medicina 2023, 59, 371. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar]
- Langhammer, B.; Bergland, A.; Rydwik, E. The importance of physical activity exercise among older people. Biomed. Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef]
- Lin, Y.H.; Chen, Y.C.; Tseng, Y.C.; Tsai, S.T.; Tseng, Y.H. Physical activity and successful aging among middle-aged and older adults: A systematic review and meta-analysis of cohort studies. Aging 2020, 12, 7704–7716. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, A.M.; Forte, P.; Carvalho, J. The effect of three different training programs in elderly women’s isokinetic strength. Motricidade 2020, 16, 84–93. [Google Scholar]
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. Task Force on Global Guidelines for Falls in Older Adults. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef]
- Wang, Q.X.; Ye, Z.M.; Wu, W.J.; Zhang, Y.; Wang, C.L.; Zheng, H.G. Association of Fear of Falling with Cognition and Physical Function in Community-Dwelling Older Adults. Nurs. Res. 2022, 71, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Tavares, G.M.S.; Pacheco, B.P.; Gottlieb, M.G.V.; Müller, D.V.K.; Santos, G.M. Interaction between cognitive status, fear of falling, and balance in elderly persons. Clinics 2020, 26, e1612. [Google Scholar] [CrossRef] [PubMed]
- Hadjistavropoulos, T.; Carleton, R.N.; Delbaere, K.; Barden, J.; Zwakhalen, S.; Fitzgerald, B.; Ghandehari, O.O.; Hadjistavropoulos, H. The relationship of fear of falling and balance confidence with balance and dual tasking performance. Psychol. Aging 2012, 27, 1–13. [Google Scholar] [CrossRef] [PubMed]
| Variables | Unit | Range | M | SD | S | K | 1. | 2. | 3. | 4. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Chair Stand Test | Repetitions | 11–35 | 20.90 | 5.82 | 0.51 | −0.11 | 1 | |||
| 2. Timed Up-and-Go Test | Seconds | 3.29–7.10 | 4.65 | 0.81 | 0.94 | 0.86 | −0.68 ** | 1 | ||
| 3. Berg Balance Scale | Points | 41–52 | 47.32 | 2.97 | −0.59 | −0.38 | 0.23 | −0.42 ** | 1 | |
| 4. Falls Efficacy Scale | Points | 16–29 | 19.89 | 3.66 | 0.87 | −0.20 | −0.23 | 0.36 ** | −0.40 ** | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, F.; Monteiro, A.M.; Forte, P.; Morouço, P. Effects of Muscle Strength, Agility, and Fear of Falling on Risk of Falling in Older Adults. Int. J. Environ. Res. Public Health 2023, 20, 4945. https://doi.org/10.3390/ijerph20064945
Rodrigues F, Monteiro AM, Forte P, Morouço P. Effects of Muscle Strength, Agility, and Fear of Falling on Risk of Falling in Older Adults. International Journal of Environmental Research and Public Health. 2023; 20(6):4945. https://doi.org/10.3390/ijerph20064945
Chicago/Turabian StyleRodrigues, Filipe, António M. Monteiro, Pedro Forte, and Pedro Morouço. 2023. "Effects of Muscle Strength, Agility, and Fear of Falling on Risk of Falling in Older Adults" International Journal of Environmental Research and Public Health 20, no. 6: 4945. https://doi.org/10.3390/ijerph20064945
APA StyleRodrigues, F., Monteiro, A. M., Forte, P., & Morouço, P. (2023). Effects of Muscle Strength, Agility, and Fear of Falling on Risk of Falling in Older Adults. International Journal of Environmental Research and Public Health, 20(6), 4945. https://doi.org/10.3390/ijerph20064945










