Sleep Patterns during the COVID-19 Lockdown in Spain
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Instruments
2.3. Procedure
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak, 18 March 2020; (WHO Reference Number: WHO/2019-nCoV/MentalHealth/2020.1); World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Boletín Oficial del Estado. Real Decreto 463/2020, de 14 de Marzo, Por el Que se Declara el Estado de Alarma Para la Gestión de la Situación de Crisis Sanitaria Ocasionada Por el COVID-19; Ministerio de la Presidencia, Relaciones con las Cortes y Memoria Democrática: Madrid, Spain, 2020. [Google Scholar]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarentine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Quevedo-Blasco, R.; Ruiz-Herrera, N.; Guillén-Riquelme, A. Análisis bibliométrico de las revistas españolas de psicología indexadas en el Emerging Source Citation Index (2018–2020). Pap. Psicól. 2021, 42, 170–176. [Google Scholar]
- Ramírez-Ortiz, J.; Fontecha-Hernández, J.; Escobar-Córdoba, F. Efectos del aislamiento social en el sueño durante la pandemia COVID-19. SciELO Prepints 2020, 801, 1–22. [Google Scholar]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impactof COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Tolsa, M.D.; Malas, O. COVID-19: Impacto Psicológico, Factores de Riesgo e Intervenciones Psicológicas en el Personal Sanitario. Una Revisión Sistemática. Rev. Iberoam. Psicol. Salud 2021, 12, 58–75. [Google Scholar]
- Camacho-Cardenosa, A.; Camacho-Cardenosa, M.; Merellano-Navarro, E.; Trapé, A.A.; Brazo-Sayavera, J. Influencia de la actividad física realizada durante el confinamiento en la pandemia del COVID-19 sobre el estado psicológico de adultos: Un protocolo de estudio. Rev. Española Salud Pública 2020, 94, e1–e9. [Google Scholar]
- Galea, S.; Merchant, R.M.; Lurie, N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef]
- Gao, C.; Schullin, M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: Integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020, 73, 1–10. [Google Scholar] [CrossRef]
- Morin, C.M.; Carrier, J.; Bastien, C.; Goldbout, R. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can. J. Public Health 2020, 111, 654–657. [Google Scholar] [CrossRef]
- Odriozola-González, P.; Planchuelo-Gómez, A.; Irurtia, M.J.; De Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020, 209, 113108. [Google Scholar] [CrossRef]
- Sher, L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020, 70, 124. [Google Scholar] [CrossRef] [PubMed]
- Trakada, A.; Nikolaidis, P.T.; Andrade, M.D.S.; Puccinelli, P.J.; Economou, N.-T.; Steiropoulos, P.; Knechtle, B.; Trakada, G. Sleep during “lockdown” in the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9094. [Google Scholar] [CrossRef] [PubMed]
- Curcio, G.G.; Tempesta, D.; Scarlata, S.; Marzano, C.; Moroni, F.; Rossini, P.M.; Ferrara, M.; De Gennaro, L. Validity of the Italian versión of the Pittsburgh Sleep Quality Index (PSQI). Neurol. Sci. 2013, 34, 511–519. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef] [PubMed]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leitner, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2021, 268, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Castronovo, V.; Galbiati, A.; Marelli, S.; Brombin, C.; Cugnata, F.; Giarolli, L.; Anelli, M.M.; Rinaldi, F.; Ferini-Strambi, L. Validation study of the Italianversion of the Insomnia Severity Index (ISI). Neurol. Sci. 2016, 37, 1517–1524. [Google Scholar] [CrossRef]
- Natale, V.; Esposito, M.J.; Martoni, M.; Fabbri, M. Validity of the reduced version of the Morningness-Eveningness Questionnaire. Sleep Biol. Rhythm. 2006, 4, 72–74. [Google Scholar] [CrossRef]
- Kocevska, D.; Blanken, T.F.; Van Someren, E.J.; Rösler, L. Sleep quality during the COVID-19 pandemic: Not one size fits all. Sleep Med. 2020, 76, 86–88. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Bados, A.; Solanas, A.; Andrés, R. Psychometric properties of the Spanish version of depression, anxiety and stress scales (DASS). Psicothema 2005, 17, 679–683. [Google Scholar]
- Báguena, M.J.; Villarroya, E.; Beleña, A.; Roldán, C.; Reig, R. Propiedades psicométricas de la versión española de la Escala Revisada de Impacto del Estresor (EIE-R). Análisis Modif. Conducta 2001, 27, 581–604. [Google Scholar]
- Dal Santo, F.; González-Blanco, L.; Rodríguez-Revuelta, J.; Marina González, P.A.; Paniagua, G.; García-Álvarez, L.; Fuente-Tomás, L.; Sáiz, P.A.; García-Portillaa, M.P.; Bobes, J. Early impact of the COVID-19 out break on sleep in a large Spanish sample. Behav. Sleep Med. 2021, 20, 100–115. [Google Scholar] [CrossRef] [PubMed]
- Maestro-González, A.; Sánchez-Zaballos, M.; Mosteiro-Díaz, M.P.; Zuazua-Rico, D. Quality of sleep among social media users during the lockdown period due to COVID-19 in Spain. Sleep Med. 2021, 80, 210–215. [Google Scholar] [CrossRef]
- Benítez, I.; Roure, N.; Pinilla, L.; Sapiña-Beltran, E.; Buysse, D.J.; Barbé, F.; de Batlle, J. Validation of the satisfaction, alertness, timing, efficiency and Duration (SATED) questionnaire for sleep health measurement. Ann. Am. Thorac. Soc. 2020, 17, 338–343. [Google Scholar] [CrossRef]
- Johns, M.W. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 1992, 15, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Targa, A.D.; Benítez, I.D.; Moncusí-Moix, A.; Arguimbau, M.; de Batlle, J.; Dalmases, M.; Barbé, F. Decrease in sleep quality during COVID-19 outbreak. Sleep Breath. 2021, 25, 1055–1061. [Google Scholar] [CrossRef]
- Magalhães, P.; Pereira, B.; Oliveira, A.; Santos, D.; Núñez, J.C.; Rosário, P. The Mediator Role of Routines on the Relationship between General Procrastination, Academic Procrastination and Perceived Importance of Sleep and Bedtime Procrastination. Int. J. Environ. Res. Public Health 2021, 18, 7796. [Google Scholar] [CrossRef]
- Buela-Casal, G. Clasificación y evaluación del insomnio. Análisis Modif. Conducta 1992, 18, 561–574. [Google Scholar]
- Buela-Casal, G.; Díaz-Román, A.; Sánchez Gómez, A.I. Evaluación y Tratamiento de los Trastornos del Sueño; Síntesis: Madrid, Spain, 2020. [Google Scholar]
- Buela-Casal, G.; Guillén-Riquelme, A. Trastornos del sueño. Manual de Psicopatología, 3rd ed.; Belloch, E.A., Sandín, B., Ramos, F., Eds.; McGraw-Hill Interamericana de España S.L.: Madrid, Spain, 2020; Volume I, pp. 541–555. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing (Version 4.1.3) [Computer Software]; R Core Foundation: Vienna, Austria, 2022. [Google Scholar]
- Zhao, X.; Lan, M.; Li, H.; Yang, J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: A moderated mediation model. Sleep Med. 2021, 77, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Conte, F.; De Rosa, O.; Rescott, M.L.; Arabia, T.P.; D’Onofrio, P.; Lustro, A.; Malloggi, S.; Molinaro, D.; Spagnoli, P.; Giganti, F.; et al. High sleep fragmentation parallels poor subjective sleep quality during the third wave of the COVID-19 pandemic: An actigraphic study. J. Sleep Res. 2022, 31, e13519. [Google Scholar] [CrossRef] [PubMed]
- Paiva, T.; Reis, C.; Feliciano, A.; Canas-Simião, H.; Machado, M.; Gaspar, T.; Tomé, G.; Branquinho, C.; Silva, M.; Ramiro, L.; et al. Sleep and awakening quality during COVID-19 confinement: Complexity and relevance for health and behavior. Int. J. Environ. Res. Public Health 2021, 18, 3506. [Google Scholar] [CrossRef] [PubMed]
- Scarpelli, S.; Alfonsi, V.; Mangiaruga, A.; Musetti, A.; Quattropani, M.C.; Lenzo, V.; Freda, M.F.; Lemmo, D.; Vegni, E.; Borghi, L.; et al. Pandemic nightmares: Effects on dream activity of the COVID-19 lockdown in Italy. J. Sleep Res. 2021, 30, e13300. [Google Scholar] [CrossRef] [PubMed]
- Amigo Vázquez, I. Manual de Psicología de la Salud, 4th ed.; Pirámide: Madrid, Spain, 2020. [Google Scholar]
- Carneiro-Barrera, A.; Amaro-Gahete, F.J.; Acosta, F.M.; Ruiz, J.R. Body composition impact on sleep in young adults: The mediating role of sedentariness, physical activity, and diet. J. Clin. Med. 2020, 9, 1560. [Google Scholar] [CrossRef]
- Mochón-Benguigui, S.; Carneiro-Barrera, A.; Castillo, M.J.; Amaro-Gahete, F.J. Role of physical activity and fitness on sleep in sedentary middle aged adults: The FIT AGEING study. Sci. Rep. 2021, 11, 539. [Google Scholar] [CrossRef] [PubMed]
- Villaécija, J.; Luque, B.; Martínez, S.; Castillo-Mayén, R.; Cuadrado, E.; Domínguez-Escribano, M.; Tabernero, C. Perceived social support and healthy eating self-efficacy on the well-beingof children and adolescents. Rev. Iberoam. Psicol. Salud 2022, 13, 56–72. [Google Scholar]
- Sandín, B.; Valiente, R.M.; García-Escalera, J.; Chorot, P. Impacto psicológico de la pandemia de COVID-19: Efectos negativos y positivos en población española asociados al periodo de confinamiento nacional. J. Psychopathol. Clin. Psychol. 2020, 25, 1–22. [Google Scholar] [CrossRef]
- López-Núñez, M.I.; Díaz-Morales, J.F.; Aparicio-García, M.E. Individual differences, personality, social, family and work variables on mental health during COVID-19 outbreak in Spain. Pers. Individ. Differ. 2021, 172, 110562. [Google Scholar] [CrossRef]
- Oksanen, A.; Miller, B.L.; Savolainen, I.; Sirola, A.; Demant, J.; Kaakinen, M.; Zych, I. Social media and access to drugs online: A nationwide study in the United states and Spain among adolescents and young adults. Eur. J. Psychol. Appl. Legal Context 2021, 13, 29–36. [Google Scholar] [CrossRef]
- Quevedo-Blasco, R.; Díaz-Román, A.; Quevedo-Blasco, V.J. Associations between Sleep, Depression, and Cognitive Performance in Adolescence. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 501–511. [Google Scholar] [CrossRef]
- Sierra, J.C.; Sánchez, A.I.; Quevedo-Blasco, R. Evaluación Psicológica: Técnicas y Aplicaciones, 5th ed.; Editorial Técnica AVICAM: Granada, Spain, 2023. [Google Scholar]
| Variable | Sex | Total Sample | ||
|---|---|---|---|---|
| χ2 (DF) | p | χ2 (DF) | p | |
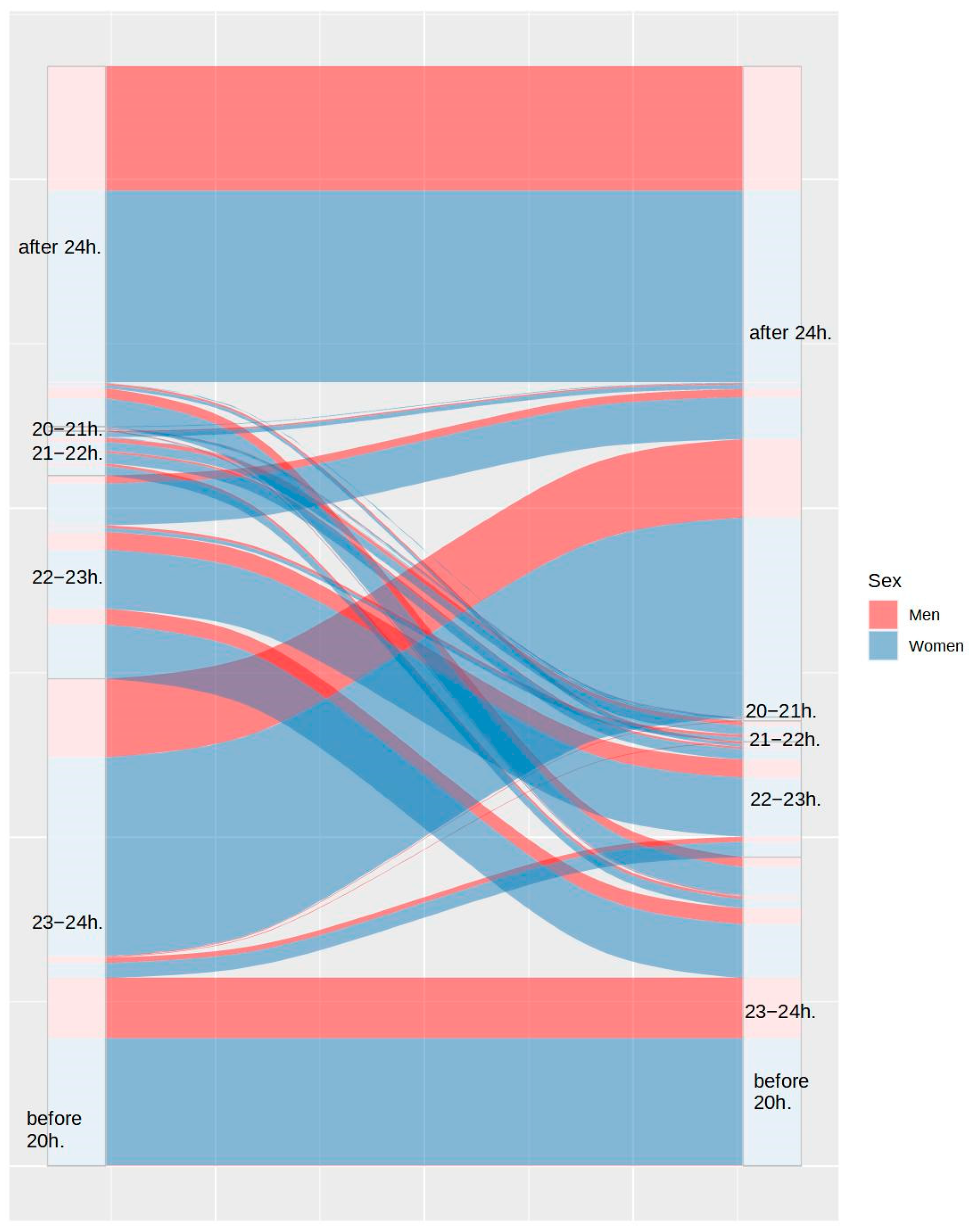
| Bedtime pre-lockdown | 29.4 (5) | <0.001 | 2902 (25) | <0.001 |
| Bedtime lockdown | 9.08 (5) | 0.106 | ||
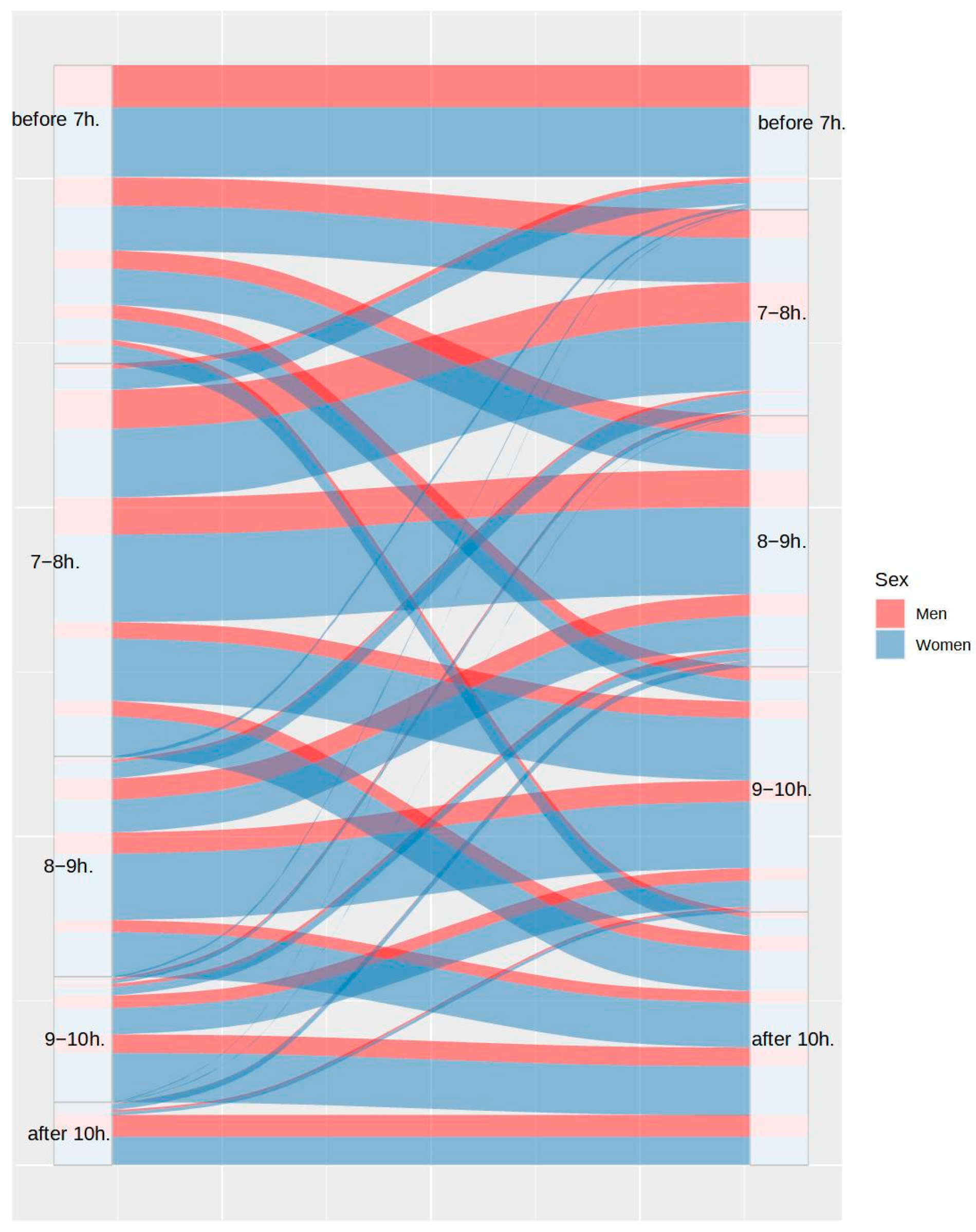
| Wake up time pre-lockdown | 14.86 (4) | 0.005 | 785 (16) | <0.001 |
| Wake up time lockdown | 6.74 (4) | 0.15 | ||
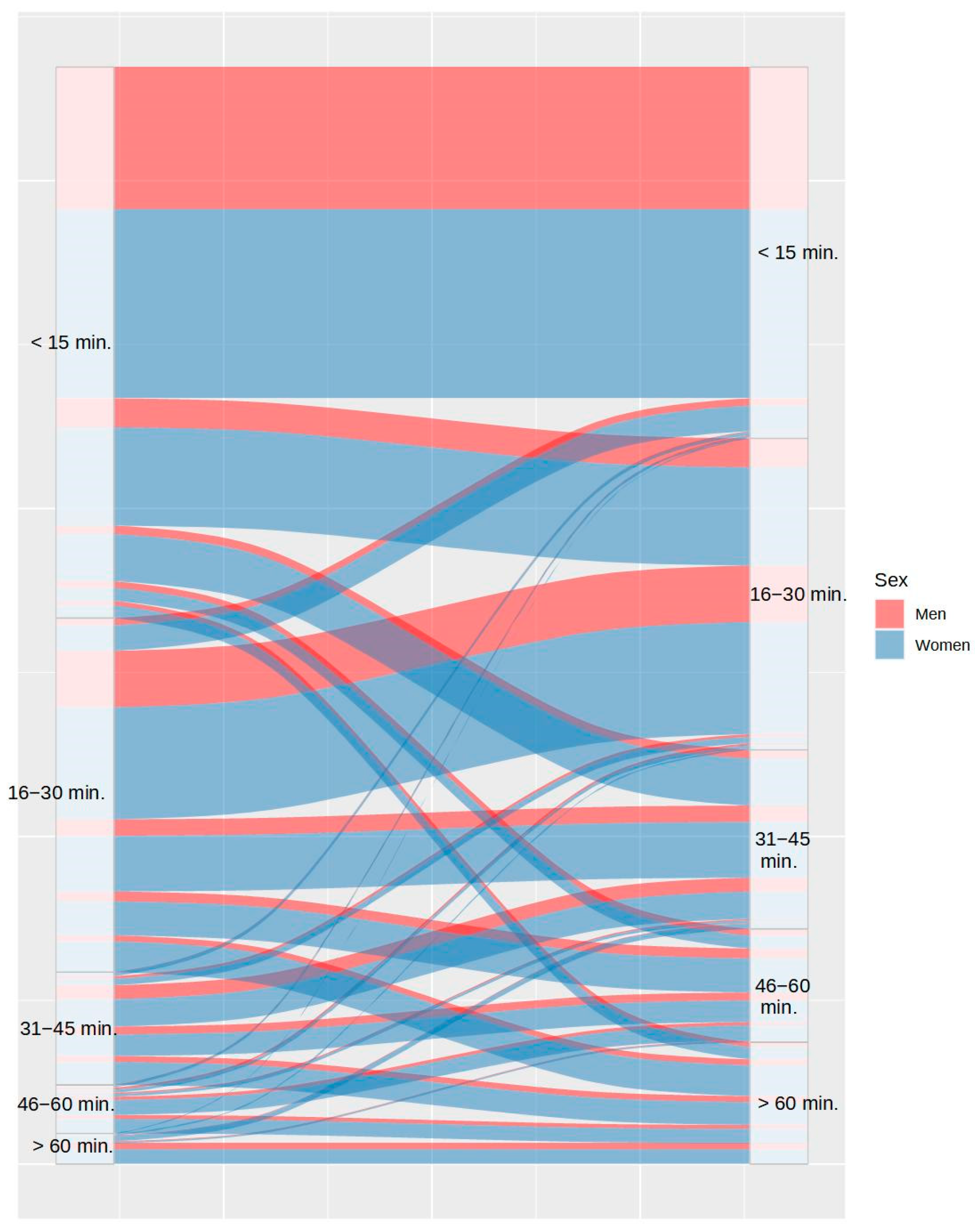
| Time to fall asleep pre-lockdown | 13.14 (4) | 0.011 | 941 (16) | <0.001 |
| Time to fall asleep lockdown | 44.58 (4) | <0.001 | ||
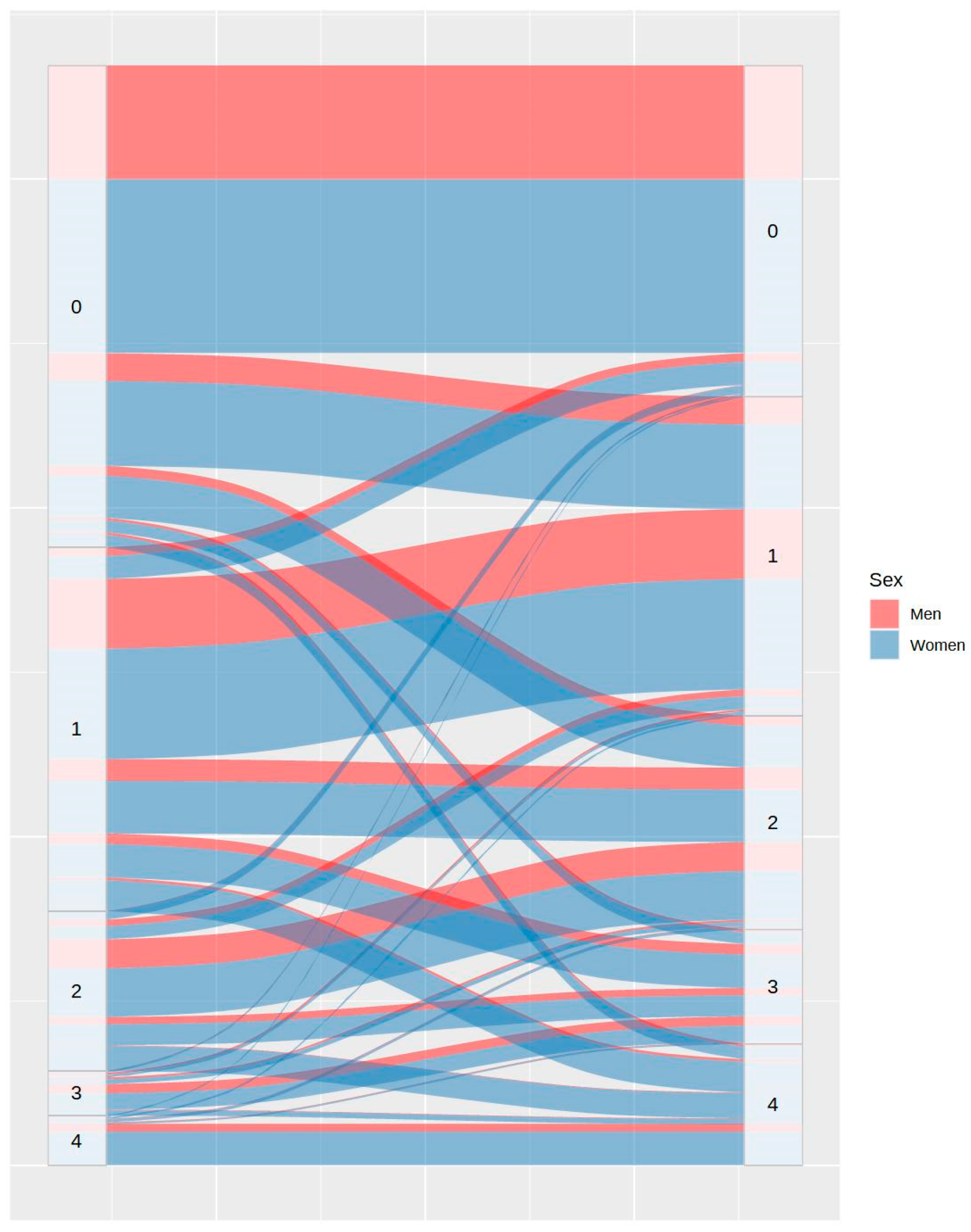
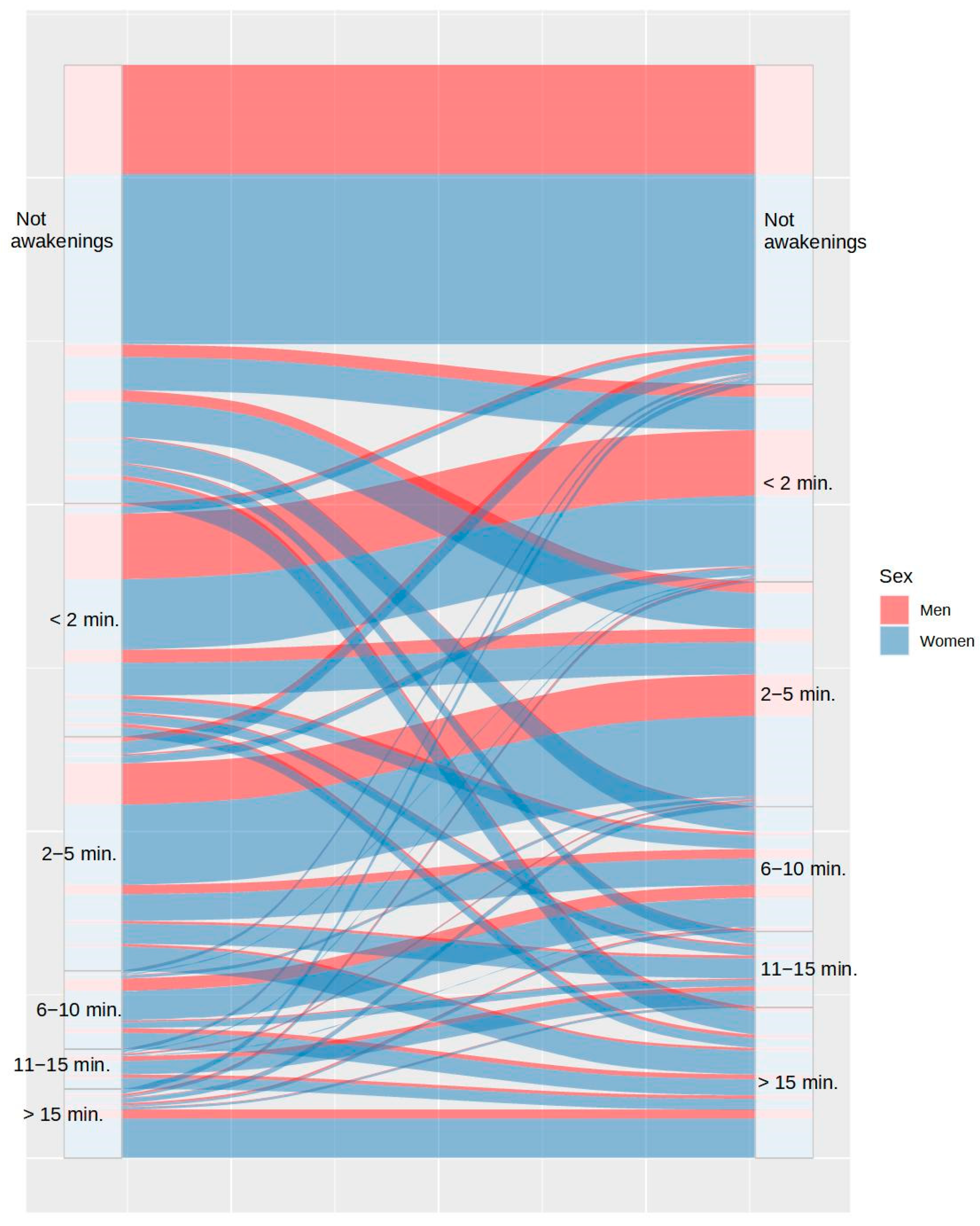
| Awakening number pre-lockdown | 7.76 (4) | 0.1 | 1261 (16) | <0.001 |
| Awakening number lockdown | 44.42 (4) | <0.001 | ||
| Awakening duration pre-lockdown | 21.5 (5) | <0.001 | 1810 (25) | <0.001 |
| Awakening duration lockdown | 60.68 (5) | <0.001 | ||
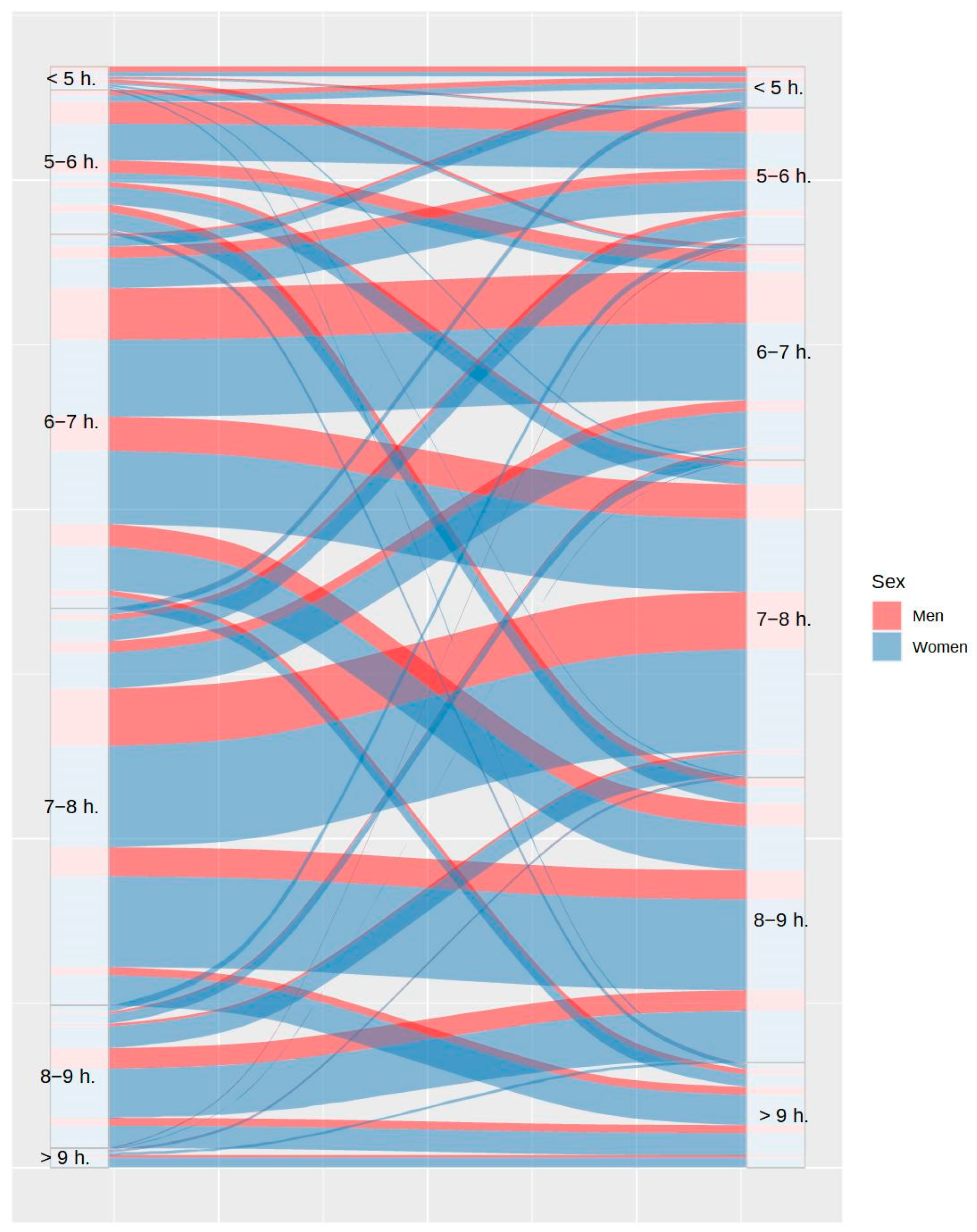
| Total sleep time pre-lockdown | 18.34 (5) | 0.003 | 721 (25) | <0.001 |
| Total sleep time lockdown | 13.14 (5) | 0.022 | ||
| Sleepiness pre-lockdown | 23.51 (4) | <0.001 | 569 (16) | <0.001 |
| Sleepiness lockdown | 19.1 (4) | <0.001 | ||
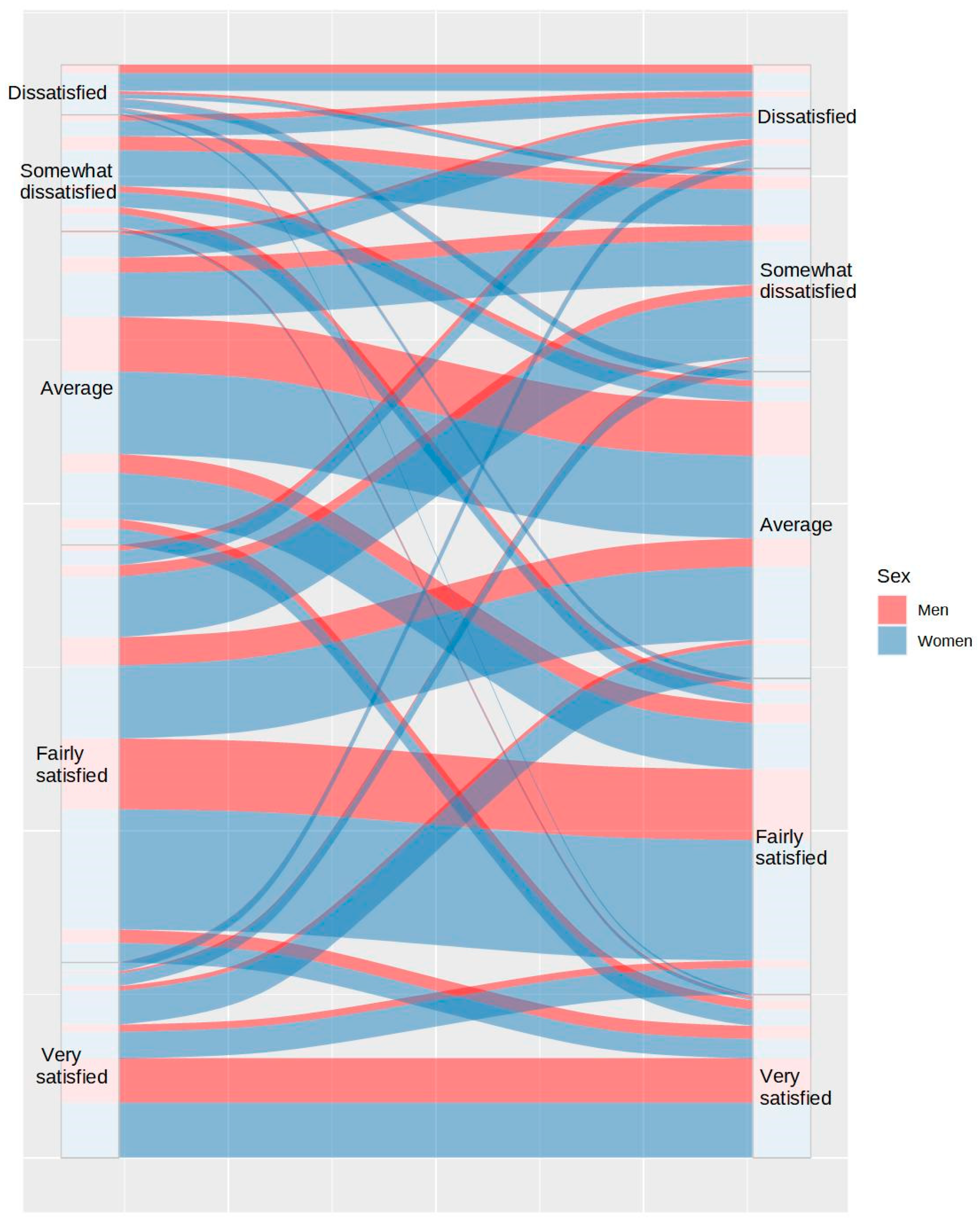
| Sleep satisfaction pre-lockdown | 1.85 (4) | 0.763 | 748 (20) | <0.001 |
| Sleep satisfaction lockdown | 31.86 (5) | <0.001 | ||
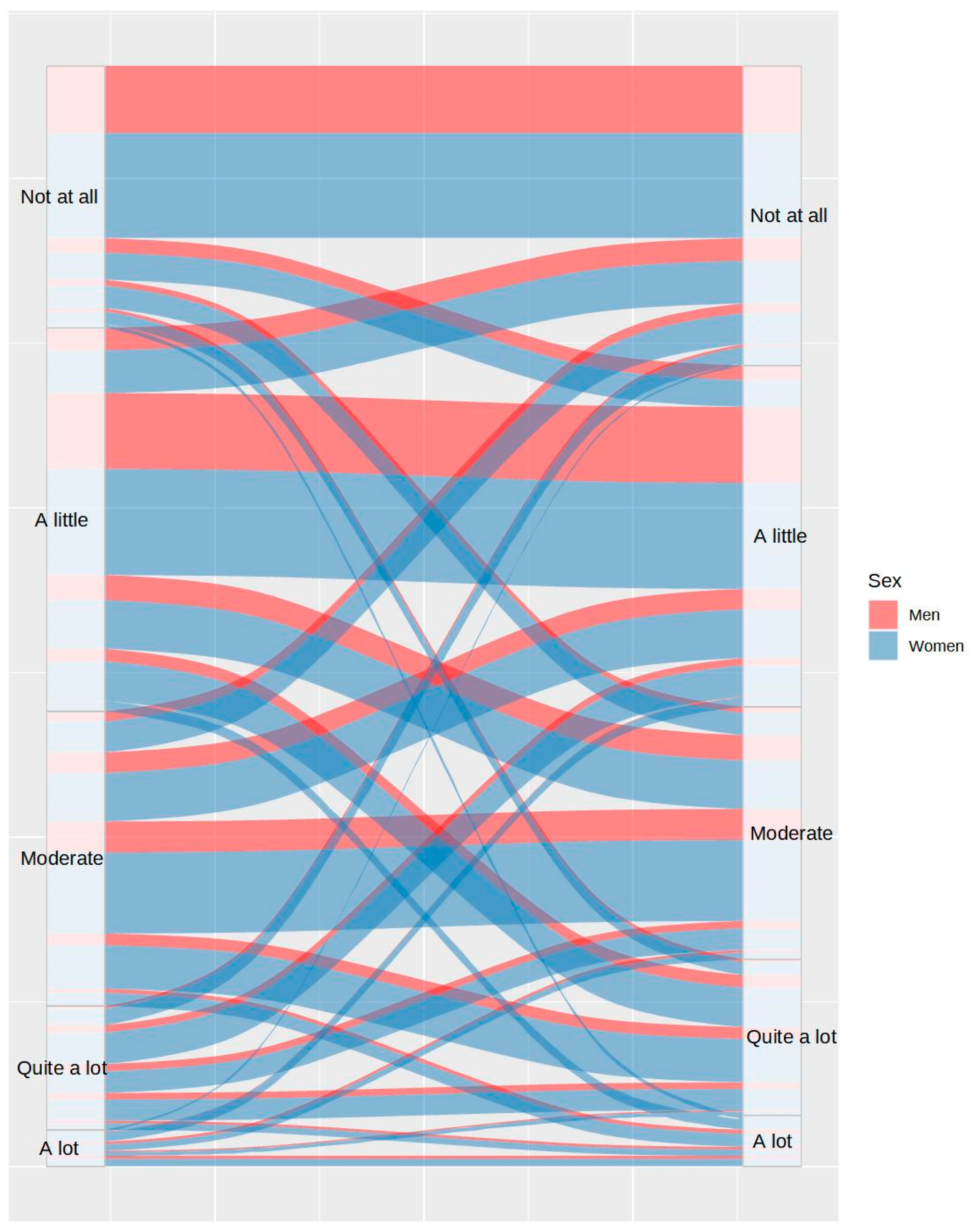
| Tiredness pre-lockdown | 28.48 (4) | <0.001 | 596.42 (16) | <0.001 |
| Tiredness lockdown | 51.25 (4) | <0.001 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz-Herrera, N.; Díaz-Román, A.; Guillén-Riquelme, A.; Quevedo-Blasco, R. Sleep Patterns during the COVID-19 Lockdown in Spain. Int. J. Environ. Res. Public Health 2023, 20, 4841. https://doi.org/10.3390/ijerph20064841
Ruiz-Herrera N, Díaz-Román A, Guillén-Riquelme A, Quevedo-Blasco R. Sleep Patterns during the COVID-19 Lockdown in Spain. International Journal of Environmental Research and Public Health. 2023; 20(6):4841. https://doi.org/10.3390/ijerph20064841
Chicago/Turabian StyleRuiz-Herrera, Noelia, Amparo Díaz-Román, Alejandro Guillén-Riquelme, and Raúl Quevedo-Blasco. 2023. "Sleep Patterns during the COVID-19 Lockdown in Spain" International Journal of Environmental Research and Public Health 20, no. 6: 4841. https://doi.org/10.3390/ijerph20064841
APA StyleRuiz-Herrera, N., Díaz-Román, A., Guillén-Riquelme, A., & Quevedo-Blasco, R. (2023). Sleep Patterns during the COVID-19 Lockdown in Spain. International Journal of Environmental Research and Public Health, 20(6), 4841. https://doi.org/10.3390/ijerph20064841









